Abstract
The incidence and mortality rates of lung cancer, the leading cause of cancer death in China, have significantly increased in recent years, and present geographic and gender differences as a result of diversity in lifestyles and socioeconomic development. A series of attribute risk analyses have shown that factors such as smoking, air pollution, and occupational factors are all related to lung cancer. Behavioral intervention, such as smoking cessation and screening, could effectively reduce lung cancer incidence and mortality.
Keywords: China, epidemiology, lung cancer, prevention, risk factor
Introduction
Lung cancer is a multi‐step and multi‐factorial disease, has a variety of histological subtypes, and is the most fatal cancer worldwide. The etiology of lung cancer is not yet clear. Smoking and air pollution are two significant risk factors. Other risk factors, such as occupational exposure (e.g. asbestos), also play a significant role in the development of lung cancer. In China, lung cancer incidence in both men and women has increased rapidly in recent years, imposing a great threat to human health. Thus, it is critical to determine the epidemiological distribution of lung cancer in order to provide basic information for cancer prevention and control and ultimately, to reduce incidence and mortality.
Global epidemiology of lung cancer
It is estimated that 2.09 million new cases of lung cancer occurred globally in 2018, ranking first among all cancer types. In some developed countries, such as Austria and Germany, lung cancer is one of the most common cancers.1 In the United States, however, lung cancer incidence has decreased, particularly in recent years, partly as a result of effective tobacco control and a series of health education and promotion measures.2 Interestingly, although Africa has a high smoking prevalence, lung cancer incidence is relatively low in both genders, which may be related to low life expectancy.3 In terms of gender differences, lung cancer is more prevalent in men, both in worldwide and in most regions.
As for mortality, lung cancer is currently the leading cause of cancer death, accounting for nearly 20% of all cancer deaths. Lung cancer mortality in China is relatively high compared to most countries.1 It is projected that lung cancer mortality in China may increase by approximately 40% between 2015 and 2030.4
Epidemiology and current trends in China
Cancer incidence
According to Chen et al., nearly 3 804 000 (2 114 000 men, 1 690 000 women) new cancer cases were diagnosed in 2014, which is the equivalent of more than 10 422 cases diagnosed each day.5 The overall crude and age‐standardized incidence rates by Chinese standard population (ASIRC) for all cancers combined were 278.07/100000 and 190.63/100000, respectively.5 The incidence rate is higher in men than in women.
Cancer incidence rates usually vary distinctly by region as a result of lifestyle diversity or environment. In 2014, the ASIRC for all cancers combined was higher in urban areas (196.58/100000 vs. rural 182.64/100000).5 The age‐standardized incidence rate (ASIR) for all cancers combined was highest in South China, followed by Northeast and East China, with Southwest China having the lowest incidence rate.6
Cancer mortality
An estimated 2 296 000 cancer deaths occurred in 2014, corresponding to almost 6 290 deaths on average per day.5 The crude and age‐standardized mortality rates by Chinese standard population (ASMRC) for cancers combined were 167.89 per 100 000 and 106.98 per 100 000, respectively.5 The number of new cases and the ASMRC were both higher in men than in women.
Similar to the incidence rates, the age‐standardized mortality rate (ASMR) for all cancers combined also showed geographic diversity. The ASMRC was higher in rural areas in both men and women. East China had the highest cancer mortality rate followed by Northeast and Central China. The lowest rate occurred in North China.6
Cancer survival
Chen et al. reported that approximately 36.9% of cancer patients could survive over five years after diagnosis.7 Women have a higher survival rate (47.3% vs. men 29.3%). The survival rate in urban areas was 10% higher than in rural areas.7 Central and East China had similar survival rates (41.0% vs. 40.3%, respectively), with Southwest China showing the lowest survival rate (24.9%),7 which may be related to economic development. Zeng et al. conducted an analysis of 17 population‐based registries and found that survival had increased from 30.9% in 2003–2005 to 40.5% in 2012–2015.8
Trends in cancer incidence and mortality
For all cancers combined, the ASIR in men remained generally stable over the period 2000–2011, while a significant upward trend was observed in women. Different incidence patterns by gender may reflect different risk factors to exposure. In contrast to incidence, the ASMR decreased in both genders, as a result of population aging and changes in the cancer spectrum.7
Epidemiology of lung cancer in China
Lung cancer incidence rates in 2014
Based on data from 339 cancer registries, the ASIR of lung cancer was 36.71 per 100 000.5 The rates in men and women were 49.94 per 100 000 and 23.89 per 100 000, respectively. The number of new cases in urban areas was 457 000, 1.4 times higher than that in rural areas. The ASIR in urban areas was similar to that in rural areas, but was twice as high in men as in women.
Lung cancer mortality rates in 2014
According to Chen et al., the ASMR for lung cancer over all cancer registries was 28.49 per 100 000.5 The rates in men and women were 40.30 per 100 000 and 17.13 per 100 000, respectively. The crude and age‐standardized mortality rates for lung cancer in urban areas were 48.79 per 100 000 and 28.24 per 100 000, respectively, and in rural areas were 42.17 per 100 000 and 28.77 per 100 000, respectively. There was a vast difference in mortality, with the ASMR in men more than double the rate in women.
Lung cancer survival
Although the survival rates for all cancers have improved in recent years, lung cancer survival remains at a relatively low level. In 2012–2015, the lung cancer survival rate in men was 16.8%, which is 62.5% worse than in thyroid cancer, which has the highest survival rate. The survival rate in women was 25.1% in 2012–2015, which is classified as low survival.
Age‐specific incidence and mortality
Incidence and mortality in men and women increases with age. Data from 72 local population‐based cancer registries indicates that there has been a dramatic increase in lung cancer incidence and mortality in the population aged > 60 years.7 Moreover, incidence and mortality in men has increased more rapidly than in women among different age groups.
Trends in lung cancer incidence and mortality
Zhang et al. showed that crude incidence rates in both genders increased sharply from 2000 to 2014; however, the ASIR increased slightly in men (annual percentage change [APC]: 0.4%) and decreased in women (APC: −0.2%).9 The incidence gap between men and women has narrowed over this period (Fig 1). With APCs of 2.7% and 2.1% in men and women, respectively, a significant upward trend in ASIR was observed in rural areas compared to urban areas. Invariably, the crude and age‐standardized incidence rates were consistently higher in men than in women over the 14‐year period.9
Figure 1.
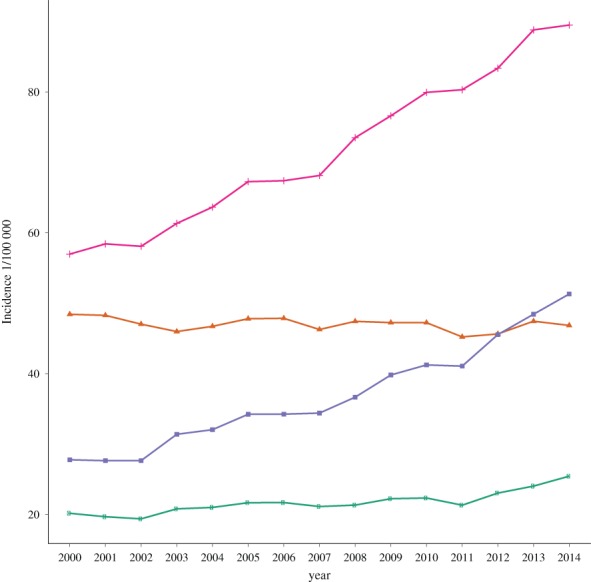
Changing trends in lung cancer incidence and age‐standardized incidence rates by Chinese standard population (ASIRC) by gender in cancer registries in 2000–2014. ( ) ASIRC in females, (
) ASIRC in females, ( ) ASIRC in males, (
) ASIRC in males, ( ) Female incidence and (
) Female incidence and ( ) Male incidence.
) Male incidence.
Zhou et al. observed an increased trend in the lung cancer mortality rate from 30.18% in 2004 to 36.10% in 2010.10 Wang et al. reported a similar trend and found gender and geographic differences in the mortality rate.11 The ASIR increased dramatically in rural residents from 1987 to 2014, with APCs in men and women of 2.58% and 2.54%, respectively.11 But the trends were disparate for urban residents, with APCs of −0.23% and 0.74% in men and women, respectively.
Risk factors and primary prevention
Smoking
Of the 315 million smokers in China, about 28% are aged ≥ 15 years. China is the largest producer and consumer of tobacco.12 Cancer and chronic respiratory disease are both associated with tobacco use. According to related epidemiologic data, tobacco use is one of the most significant risk factors accelerating the growing lung cancer epidemic.13 An estimated 75.04% of lung cancer deaths in men and 18.35% in women are attributable to tobacco use,14 indicating a clear association between the extent of smoking and cancer.15
Given the high smoking rate and psychological and financial burdens, the Chinese government launched a national strategy, Health China 2030, which aims to reduce the prevalence of smoking to < 20%.16 Measures such as increasing the cost and taxation on tobacco and assigning smoke‐free locations have led to a significant decrease in the smoking rate, from 30.2% to 26.9% over 2000–2015 (Fig 2). Based on World Health Organization data, in spite of the obvious drop in smoking prevalence, the actual number of smokers in China increased from 310 to 315 million over the same period.12 Thus, taking population growth and aging into account, more work needs to be done to cut down lung cancer incidence by reducing the rate of smoking.
Figure 2.
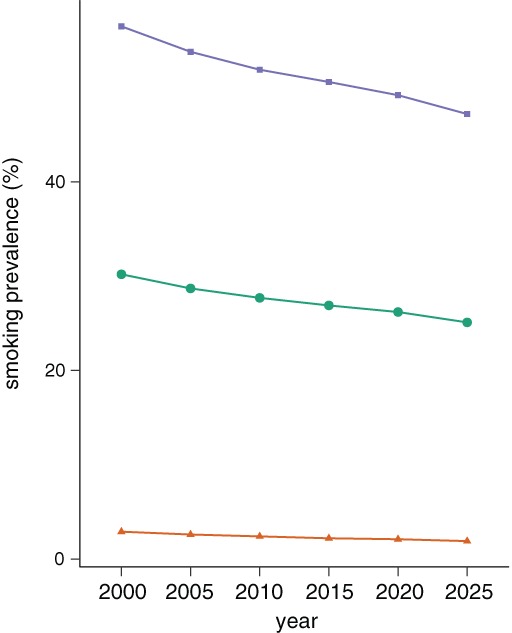
Trends in smoking prevalence among people aged ≥ 15 years, 2000–2025, not age‐standardized. The data was from World Health Organization. ( ) All, (
) All, ( ) Females, and (
) Females, and ( ) Males.
) Males.
Air pollution
As a result of the acceleration of urbanization and industrial progress, the side effects of air pollution are becoming increasingly severe. Air pollution has recently been classified as the primary carcinogen.17 In 2017, the Ministry of Ecology and Environment of the People's Republic of China reported air quality statistics in 338 urban areas. The air quality in 239 (70.7%) areas had reached a hazardous level. Degradation of air quality has been confirmed to have severe side effects on human health.
Fine particulate matter (PM) with a diameter of < 2.5 μm suspended in the atmosphere is the chief component of atmospheric pollution. A PM2.5 level can result in the stimulation of factors that can seriously interfere with gas exchange.18 Long‐term exposure to high level PM2.5 could increase the risk of lung cancer.19, 20, 21 Fu et al. found a positive association between PM2.5 and mortality, with R‐values of 0.464.22 Smokers seem to be more vulnerable.23 An American report clarified the correlation between exposure to ambient PM2.5 and life expectancy. For each 10 μg/m decrease in the concentration of fine PM2.5, life expectancy increases approximately 0.61 ± 0.20/year.24 Therefore, it is urgent to manage air quality now.
Occupational exposure
The International Agency for Research on Cancer has classified occupational exposure as a group 1 lung carcinogen.25 The main occupational factors include asbestos and dust.26, 27, 28 A case–control study conducted by De Matteis et al. reported that occupational exposure to asbestos, even at low levels, contributed to the risk of developing lung cancer, with population attributable fractions of 18.1%.29 Silica and Ni–Cr showed similar results. For this reason, it is vitally important for policy‐makers and environmental administrators to conduct health surveillance at the workplace.
Lung cancer screening
The development of low dose helical computed tomography (LDCT) has made screening in high‐risk populations easier and has led to the establishment of free screening programs in some regions. Thanks to widespread screening programs, significant reductions in lung cancer incidence and mortality have been reported.30, 31
Low‐dose helical computed tomography, a new advanced technology, is more effective than previous methods for diagnosing early stage lung cancer and, subsequently, reducing mortality.32 It not only reduces radiation exposure by adjusting related scanner parameters but also uses different algorithms to acquire better diagnostic image quality.33 The American Cancer Society has recommended that people aged 55–74 should undergo LDCT screening annually and has published criteria to determine the population at high risk.34 However, early detection rates vary as a result of differences in equipment and skill, thus greater focus on these factors would lead to improved detection rates. Nevertheless, the cancer burden in China has been alleviated by the introduction of screening.
Conclusions
Two phenomena warrant discussion after exploring the many studies related to lung cancer. One is that lung cancer may overtake breast cancer as the leading cause of cancer death in women. The other is that the lung cancer risk is highest in people aged > 60 years. Combined clinical data may help us to better interpret why lung cancer incidence has increased in these populations.
Although China has implemented a series of policies to benefit peasants, including free screening, the proportion of lung cancer in poor areas remains dominant. People located in rural areas, particularly those in remote mountainous regions, may not be aware of the exact meaning of screening or methods of cancer prevention. Consequently, the most urgent task at present is to launch a series of nationwide screening programs based on the conditions in China, with greater effort made to mobilize the population to prevent cancer in rural areas that have a relative shortage of resources.
Disclosure
No authors report any conflict of interest.
References
- 1. Ferlay J, Ervik M, Lam F, Colombet M, Mery L, Piñeros M, Znaor A, Soerjomataram I, Bray F (2018). Global Cancer Observatory: Cancer Today. Lyon, France: International Agency for Research on Cancer. [Cited 5 Nov 18.] Available from URL: https://gco.iarc.fr/today
- 2. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin 2018; 68: 7–30. [DOI] [PubMed] [Google Scholar]
- 3. McIntyre A, Ganti AK. Lung cancer‐A global perspective. J Surg Oncol 2017; 115: 550–4. [DOI] [PubMed] [Google Scholar]
- 4. Martin‐Sanchez JC, Lunet N, Gonzalez‐Marron A et al Projections in Breast and Lung Cancer Mortality among Women: A Bayesian Analysis of 52 Countries Worldwide. Cancer Res 2018; 78: 4436–42. [DOI] [PubMed] [Google Scholar]
- 5. WQ C, H L, KX S et al Report of cancer incidence and mortality in China. Chin J Oncol 2014; 2018: 5–13. [DOI] [PubMed] [Google Scholar]
- 6. Chen W, Sun K, Zheng R et al Cancer incidence and mortality in China, 2014. Chin J Cancer Res 2018; 30: 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chen W, Zheng R, Baade PD et al Cancer statistics in China, 2015. CA Cancer J Clin 2016; 66: 115–32. [DOI] [PubMed] [Google Scholar]
- 8. Zeng H, Chen W, Zheng R et al Changing cancer survival in China during 2003–15: a pooled analysis of 17 population‐based cancer registries. Lancet Glob Health 2018; 6: e555––67 (In Chinese.). [DOI] [PubMed] [Google Scholar]
- 9. Zhang SW, Zheng RS, Yang ZX et al [Trend analysis on incidence and age at diagnosis for lung cancer in cancer registration areas of China, 2000‐2014]. Zhonghua Yu Fang Yi Xue Za Zhi 2018; 52: 579–85 (In Chinese.). [DOI] [PubMed] [Google Scholar]
- 10. QU R, Zhou B. Analysis of the Distribution and Trend of Lung Cancer Mortality in China between 2004 and 2010. Chinese Journal of Health Statistics 2014; 31: 932–5. [Google Scholar]
- 11. Wang L, Yu C, Zhang Z et al Trend in lung cancer mortality among residents in China:1987‐2014. Chinese Journal of Public Health 2017; 33: 42–6. [Google Scholar]
- 12. World Health Organization . WHO Report on the Global Tobacco Epidemic. 2017. [Cited 5 Nov 18.] Available from URL: http://www.who.int/tobacco/global_report/2017/en/
- 13. Chen W, Zhang S, Zou X. Evaluation on the incidence, mortality and tendency of lung cancer in China. Thorac Cancer 2010; 1: 35–40. [DOI] [PubMed] [Google Scholar]
- 14. Wang JB, Fan YG, Jiang Y et al Attributable causes of lung cancer incidence and mortality in China. Thorac Cancer 2011; 2: 156–63. [DOI] [PubMed] [Google Scholar]
- 15. Lee PN, Forey BA, Coombs KJ. Systematic review with meta‐analysis of the epidemiological evidence in the 1900s relating smoking to lung cancer. BMC Cancer 2012; 12: 385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Goodchild M, Zheng R. Tobacco control and Healthy China 2030. Tob Control 2018; 1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hamra GB, Guha N, Cohen A et al Outdoor particulate matter exposure and lung cancer: A systematic review and meta‐analysis. Environ Health Perspect 2014; 122: 906–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wei H, Liang F, Cheng W et al The mechanisms for lung cancer risk of PM2.5 : Induction of epithelial‐mesenchymal transition and cancer stem cell properties in human non‐small cell lung cancer cells. Environ Toxicol 2017; 32: 2341–51. [DOI] [PubMed] [Google Scholar]
- 19. Berger RE, Ramaswami R, Solomon CG et al Air pollution still kills. New Engl J Med 2017; 376: 2591–2. [DOI] [PubMed] [Google Scholar]
- 20. Brauer M, Amann M, Burnett RT et al Exposure assessment for estimation of the global burden of disease attributable to outdoor air pollution. Environ Sci Technol 2012; 46: 652–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Chen G, Wan X, Yang G, Zou X. Traffic‐related air pollution and lung cancer: A meta‐analysis. Thorac Cancer 2015; 6: 307–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Fu J, Jiang D, Lin G, Liu K, Wang Q. An ecological analysis of PM2.5 concentrations and lung cancer mortality rates in China. BMJ Open 2015; 5: e009452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kotaki K, Senjyu H, Tanaka T et al Tobacco use among designated air pollution victims and its association with lung function and respiratory symptoms: a retrospective cross‐sectional study. BMJ Open 2014; 4: e005393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Pope CA, Ezzati M, Dockery DW. Fine‐particulate air pollution and life expectancy in the United States. New Eng J Med 2009; 360: 376–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Field RW, Withers BL. Occupational and environmental causes of lung cancer. Clin Chest Med 2012; 33: 681–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Poinen‐Rughooputh S, Rughooputh MS, Guo Y, Rong Y, Chen W. Occupational exposure to silica dust and risk of lung cancer: an updated meta‐analysis of epidemiological studies. BMC Public Health 2016; 16: 1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. McCormack V, Peto J, Byrnes G, Straif K, Boffetta P. Estimating the asbestos‐related lung cancer burden from mesothelioma mortality. Br J Cancer 2012; 106: 575–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Järvholm B, Åström E. The risk of lung cancer after cessation of asbestos exposure in construction workers using pleural malignant mesothelioma as a marker of exposure. J Occup Environ Med 2014; 56: 1297–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. De Matteis S, Consonni D, Lubin JH et al Impact of occupational carcinogens on lung cancer risk in a general population. Int J Epidemiol 2012; 41: 711–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Church TR, Black WC, Aberle DR et al Results of initial low‐dose computed tomographic screening for lung cancer. N Engl J Med 2013; 368: 1980–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Nanavaty P, Alvarez MS, Alberts WM. Lung cancer screening: advantages, controversies, and applications. Cancer Control: J Moffitt Cancer Center 2014; 21: 9–14. [DOI] [PubMed] [Google Scholar]
- 32. Aberle DR, Adams AM, Berg CD et al Reduced lung‐cancer mortality with low‐dose computed tomographic screening. New Eng J Med 2011; 365: 395–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Munden RF, Godoy MC. Lung cancer screening: state of the art. J Surg Oncol 2013; 108: 270–4. [DOI] [PubMed] [Google Scholar]
- 34. Smith RA, Andrews KS, Brooks D et al Cancer screening in the United States, 2018: A review of current American Cancer Society guidelines and current issues in cancer screening. CA Cancer J Clin 2018; 68: 297–316. [DOI] [PubMed] [Google Scholar]


