Abstract
Background.
Despite significant attention to resuscitation care by hospitals, national data on trends in the incidence and survival of patients with in-hospital cardiac arrest (IHCA) are limited.
Objective.
To determine trends and hospital-level variation in the incidence and outcomes associated with IHCA. In exploratory analyses, we evaluated the relationship between hospital-level IHCA incidence and outcomes with general hospital-wide quality improvement activities.
Design, Setting, and Participants.
Retrospective cohort study of 2,205,123 hospitalizations at 101 Veterans Health Administration (VHA) hospitals between 2008 and 2012.
Main Outcomes.
Risk- and reliability-adjusted hospital-level IHCA incidence and survival to hospital discharge.
Results.
A total of 8,821 (0.40%) IHCA occurred between 2008 and 2012, with no significant change in risk-adjusted incidence over this time (p=0.77). Hospital-level IHCA incidence varied substantially across facilities, with a median hospital incidence of 4.0 per 1000 hospitalizations and a range from 1.4 to 11.8 per 1000 hospitalizations. Overall, survival to discharge after IHCA was 31.2%. Risk-adjusted odds of survival increased over the study period (2012 vs 2008, OR: 1.49, 95% CI: 1.27, 1.75) but survival varied substantially across facilities from 20.3% to 45.4%. General hospital quality improvement activities were inconsistently associated with IHCA incidence and survival.
Conclusions.
Within the VHA, the incidence and outcomes of IHCA showed important trends over time but varied substantially across hospitals with no consistent link to general hospital quality improvement activities. Identification of specific resuscitation practices at hospitals with low incidence and high survival of IHCA may guide further improvements for in-hospital resuscitation.
Keywords: Cardiac arrest, resuscitation, hospital, quality of care
More than 200,000 patients suffer in-hospital cardiac arrest (IHCA) each year in the United States and fewer than 1 in 4 survives to hospital discharge.1,2 Significant resources are dedicated to this high-risk condition, with estimates exceeding $300 million nationally to equip, train, and accredit providers and hospitals in resuscitation care.3,4 This attention to resuscitation care may be contributing to improvements in IHCA survival. For example, survival of IHCA has improved at select hospitals participating in an IHCA quality-improvement registry sponsored by the American Heart Association.2,5 However, it is unknown whether this contemporary trend in IHCA survival is occurring more broadly, consistent with widespread adoption of efforts to improve resuscitation care.
Prior studies also have demonstrated significant hospital-level variation in the incidence and in-hospital outcomes of IHCA.6–8 Although suggestive of variation in the quality of resuscitation care that impacts patient outcomes, these studies have included a diverse set of hospitals and patient populations that may contribute to variation in outcomes. The Veterans Health Administration (VHA) offers a unique opportunity to evaluate facility-level IHCA incidence and survival over time within similar care delivery and patient population settings. Additionally, data on the commitment to general quality improvement activities at individual VA hospitals9 affords an opportunity to explore the association between these activities and the hospital-level incidence and outcomes of IHCA. Understanding this relationship may inform how hospitals address quality shortcomings that contribute to higher incidence and worse outcomes of IHCA.
Using VHA national data, we determined system-wide trends and hospital-level variation in the incidence and outcomes after IHCA. By understanding hospital-level variation in the incidence and outcomes for IHCA, as well as their relationship with general quality improvement activities at hospitals, our study can guide future efforts to optimize IHCA care.
METHODS
Study Setting and Patient Population
We identified all Veterans hospitalized at VHA hospitals nationally between 2008 and 2012 from the VA Inpatient Evaluation Center (IPEC) data. Based on prior work,10 we identified patients in this cohort suffering IHCA using International Classification of Diseases, Ninth Revision (ICD-9-CM) procedure and diagnosis codes for IHCA: 99.60 (cardiopulmonary resuscitation, not otherwise specified) and 99.63 (closed chest massage), as well as diagnosis code 427.5 (cardiac arrest). In the very rare instances that a patient suffers an IHCA during distinct hospitalizations, each hospitalization with IHCA was included in the analysis, with appropriate adjustment for non-independence of observations via robust standard errors.
This study was approved by the Ann Arbor VA Institutional Review Board. This study was funded by the Department of Veterans Affairs, Health Services Research & Development, IIR 13–079. The authors are solely responsible for the design and conduct of this study, all study analyses, the drafting and editing of the paper and its final contents.
Survival to Discharge
Survival to discharge was determined from the VA Information Resource Center Vital Status File, which compiles data from the Beneficiary Identification Records Locator Subsystem Death file, VA Medicare Vital Status File, and the Social Security Administration Death Master File. This method has been shown to be highly accurate at determining death and survival to discharge.11
Hospital-wide Quality Improvement Activities Survey Instrument
To explore the association between general quality improvement activities at individual VA hospitals and the hospital-level incidence and outcomes of IHCA, we used data collected on hospital-wide quality improvement activities from a prior cross-sectional, descriptive study.9
In this prior study, the Chief of Medicine at each hospital was surveyed about quality improvement activities. Details on the survey development, administration, scoring, and the identification of dimensions of quality improvement activities represented by the survey instrument have been previously described.9 Briefly, the survey included 27 questions primarily derived from the Quality Improvement Activities Survey. Using multi-trait scaling analysis, four dimensions were derived from the survey that focused on: infrastructure, prevention, information gathering, and goal alignment/quality commitment. Components of these dimensions and scoring by the instrument are provided in Supplemental Table 1. In each case, a higher score meant higher levels of reported activities.
Statistical Analysis
General Approach
We used hierarchical logistic regression models with patients nested in hospitals to assess risk- and reliability-adjusted rates of IHCA incidence and survival to discharge. Analyses were conducted using Stata software version 14 (StataCorp, College Station, TX), SAS version 9.4 (SAS Institute Inc, Cary,NC), and R version 3.3.0 (The R Foundation for Statistical Computing).
Risk Adjustment
We used a severity of illness score to account for differences in case-mix that may confound temporal and hospital-level relationships for IHCA incidence and survival. The severity of illness score included age, race, sex, admission diagnosis category, 29 Elixhauser comorbid conditions,12 and 11 lab values drawn within 24 hours of admission.13,14 The Elixhauser comorbidities serve as a standardized method for measuring patient comorbidity based on diagnosis codes found in administrative data.12 As in past work, we used a logistic multivariate adaptive regression spline (MARS), a nonparametric spline-and-knot-based form of regression that models the functional forms of covariates, as well as nonlinearities and higher-level interactions of the covariates.15 This allowed us to use a flexible nonlinear structure in accounting for the severity of illness score. In the determination of risk-adjusted IHCA incidence, our dataset was too large to allow estimation from the MARS model for all 5 years of the cohort. Instead, we fit a MARS model to a random sample of 10,000 hospitalizations from the cohort and then repeated this process a total of five times. We used the mean predicted probability from these five models for each hospitalization as that hospitalization’s risk score. In modeling temporal trends, time was aggregated to calendar year and treated as a continuous variable.
Reliability Adjustment
Small numbers of IHCA events at some hospitals may lead to instability in the estimate incidence and survival outcomes at that hospital. We used reliability adjustment with empirical Bayes prediction methods to provide better estimates of incidence and survival outcomes for hospitals with few IHCA events.15
Hospital-Level Variation after Risk- and Reliability-Adjustment
We quantified hospital-level variation in IHCA incidence and survival using the intra-class correlation coefficient (ICC) and median odds ratios (MOR) calculated from the hierarchical logistic regression models. The MOR is a function of the between-hospital variance estimates as determined from the hierarchical models and can be interpreted as the odds that 2 patients with identical patient-level covariates from separate, randomly chosen hospitals will experience the outcome of interest.
Hospital Quality Improvement Activities and IHCA Incidence and Survival
To determine the association between hospital quality improvement activities and the incidence and survival outcomes of IHCA, covariates for the dimensions of infrastructure, prevention, information gathering, and goal alignment/quality as measured by the survey instrument were subsequently added to the hierarchical logistic regression models. We applied the same methodology employed in the initial study of hospital quality improvement activities in ascertaining hospital-level measures for these dimensions and did not reweight for specific activities that may more closely align with in-hospital cardiac arrest (e.g. rapid response teams).9 In secondary analyses, we assessed the relationship between the presence or absence of rapid response teams at a hospital and hospital-level incidence and survival outcomes of in-hospital cardiac arrest.
RESULTS
Patient and Hospital Characteristics
There were 2,735,383 hospitalizations at 132 hospitals in VA between 2008 and 2012. Of these, 2,205,123 (80.6%) hospitalizations were at 101 (76.5%) hospitals that were linked to the Chief of Medicine survey. These linked hospitalizations formed the analytic cohort for this analysis. There were 8,821 IHCA at these 101 hospitals during the period (Figure 1). Hospitals that could be linked to the survey had neither different incidence (p=0.782) of IHCA nor different hospital survival (p=0.182) than those hospitals that could not be linked. Characteristics of all hospitalizations (Table 1a), hospitalizations resulting in an IHCA (Table 1b), and of included hospitals (Table 2) are shown and are typical of VA patients. At hospitalization, patients’ mean age was 65.4 years overall, and 95% were male and 72% were white. At hospitalization, patients had a mean of 2.3 Elixhauser comorbidities and a predicted risk of death of 2.2%. Among patients who had an IHCA, the mean age at hospitalization was 69.3 years with a mean of 2.8 Elixhauser comorbidities. Of the studied hospitals, 48 (48%) were level 1 (full service) hospitals with ICUs.
Figure 1.
Identification of Study Cohort
Table 2.
Characteristics of Hospitals
| Hospitals | 101 (100%) |
|---|---|
| Teaching Hospital, N (%) | 48 (48%) |
| ICU levels, N (%) | |
| 1 | 40 (41%) |
| 2 | 15 (15%) |
| 3 | 29 (30%) |
| 4 | 13 (13%) |
| Region, N (%) | |
| Midwest | 24 (24%) |
| Northeast | 15 (15%) |
| South | 40 (40%) |
| West | 22 (22%) |
| COM Survey, mean ± SD | |
| Information Gathering | 2.3 ± 0.79 |
| Infrastructure | 2.3 ± 0.81 |
| Prevention | 3.4 ± 0.62 |
| Goal Alignment/Quality Improvement | 3.4 ± 0.91 |
Trends in IHCA Incidence and Survival to Discharge
The overall unadjusted incidence of IHCA was 4.0 per 1000 hospitalizations and the unadjusted survival of IHCA was 31.2%. There was no significant change in risk-adjusted decline in IHCA incidence between 2008 and 2012, with an odds ratio of 0.99 (95% CI: 0.90, 1.08) for an incident IHCA in 2012 relative to 2008 (p=0.77). Unadjusted survival to discharge for all IHCA patients was 34.0% in 2012, up from 26.2% in 2008. Risk-adjusted survival increased over time, with odds of survival to discharge increasing by nearly 50% between 2012 versus 2008 (OR: 1.49, 95% CI: 1.27, 1.75)
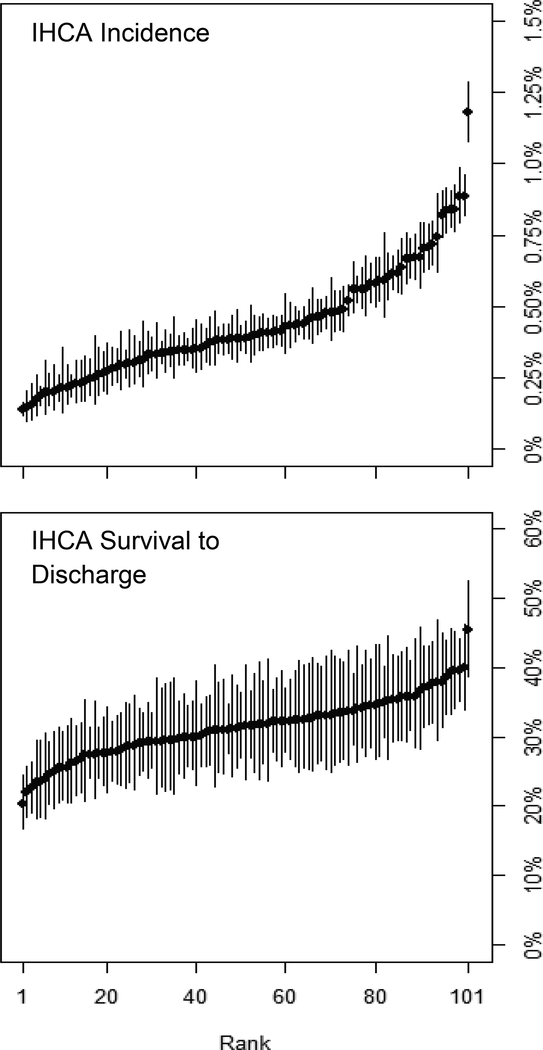
IHCA Incidence and Survival to Discharge Across Hospitals
The median hospital incidence of IHCA was 4.0 per 1000 hospitalizations and ranged from 1.4 per 1000 hospitalizations to 11.8 per 1000 hospitalizations after risk- and reliability-adjustment (Figure 2, top panel). After adjustment for severity-of-illness and reliability of these hospital-level estimates, significant variation persisted in the hospital-level incidence of IHCA (ICC=0.065). The MOR for IHCA incidence was 1.58, reflecting the odds of IHCA incidence at a randomly selected hospital that was 58% higher than another randomly selected hospital for a patient with the same covariates.
Figure 2.
Risk- and Reliability-Adjusted Hospital Differences in IHCA Incidence (Top Panel) and Survival (Lower Panel). Confidence intervals are presented such that hospitals with non-overlapping confidence intervals have statistically significant (at p<0.05) differences in their rates of IHCA.
The hospital-level median survival to discharge of IHCA was 31.5% and ranged from 20.3% to 45.4% after risk- and reliability-adjustment (ICC=0.26) (Figure 2, bottom panel). The MOR for survival of IHCA was 1.33—meaning that holding all else constant, a patient with an IHCA at two randomly selected hospitals will have a median 33% difference in odds of survival.
Hospital-wide Quality Improvement Activities and IHCA
Hospitals with a higher measure of quality improvement activities related to infrastructure had lower odds of IHCA incidence (Table 3). In contrast, hospitals with a higher measure of quality improvement activities related to information gathering were associated with a higher incidence of IHCA. None of the quality improvement activities were associated with IHCA survival to discharge. In secondary analyses, the presence of a rapid response team at a hospital was not associated with the hospital-level incidence or survival outcomes of IHCA (Table 3).
Table 3.
Association Between Hospital Level Quality Improvement Activities and Risk- and Reliability Adjusted IHCA Incidence and Survival.
| Quality Improvement Activity | IHCA Incidence | IHCA Survival | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p-value | OR | 95% CI | p-value | |
| Information-Gathering Activities | 1.26 | 1.03, 1.53 | 0.02 | 0.96 | 0.82, 1.13 | 0.65 |
| Infrastructure Activities | 0.76 | 0.64, 0.91 | 0.002 | 1.07 | 0.93, 1.24 | 0.35 |
| Prevention Activities | 1.10 | 0.87, 1.39 | 0.43 | 0.98 | 0.84, 1.13 | 0.76 |
| Goal Alignment | 0.95 | 0.85, 1.06 | 0.35 | 1.08 | 0.98, 1.20 | 0.12 |
| Rapid Response Team | 1.12 | 0.55, 2.30 | 0.75 | 0.74 | 0.44, 1.25 | 0.26 |
DISCUSSION
In this large, national, retrospective cohort of hospitalizations within the VA healthcare system, we determined temporal trends and hospital-level variation in the incidence and outcomes of IHCA. Between 2008 and 2012, the risk-adjusted incidence of IHCA remained stable in the VA. Over the same time period, there was a significant increase in the risk-adjusted odds of survival with IHCA increasing by 49%. However, risk-adjusted incidence and survival of IHCA varied significantly across hospitals. This variation was clinically significant as evidenced by a median odds ratio that differed by more than 30% between two randomly selected hospitals treating an identical patient. These findings suggest opportunities for hospitals to identify care delivery strategies associated with better patient outcomes.
A prior study of hospitals participating in a national quality improvement registry for in-hospital resuscitation demonstrated IHCA survival has improved in the past decade.2 However, it was unclear from this study if similar trends in survival of IHCA were occurring more broadly across hospitals due to the select nature of these hospitals that all participated in a national quality improvement program aimed at resuscitation care. In fact, a study of Medicare beneficiaries found no temporal trend in survival rates of IHCA.10 Our study from the VHA, the largest integrated health care system in the United States with over 100 hospitals for inpatient care, is consistent with improving survival of IHCA.
Little is known about temporal trends of IHCA incidence. One prior study demonstrated a temporal decline in the incidence of IHCA occurring in intensive care unit settings.16 Similar studies of overall trends in the incidence of IHCA are lacking. In the present study, we observed no significant change in IHCA incidence between 2008 and 2012, which suggests that improvements in risk-adjusted survival for IHCA is not likely due to increased rates of do-not-resuscitate (DNR) orders (in which case we would expect lower rates of IHCA incidence over time). This ability to link assessments of incidence and survival in the same analysis is a particular strength of our approach. Although encouraging, further study is needed to determine the components of care delivery that may both decrease IHCA incidence and improve IHCA case survival rates.
Although these overall trends suggest improvements in the treatment of IHCA, we observed significant hospital-level variation in the incidence and survival outcomes of IHCA that are consistent with prior studies.6,8,17 General aspects of quality improvement have been shown to contribute to variation in hospital performance for other clinical conditions. For example, a prior study of hospital-performance in acute myocardial infarction care found high-performing hospitals were defined by an organizational culture that supported efforts to improve care.18 However, in the present study, general measures of hospital quality improvement activities were poorly correlated with IHCA incidence and outcomes.
The lack of relationship between general measures of quality improvement and hospital rates and outcomes of IHCA suggests the need for more granular and IHCA-specific quality improvement activities. Studies have begun to identify aspects of the care delivery structure (i.e., nurse staffing ratios19), culture,19 and process (e.g., rapid defibrillation,20 achievement of IHCA process measures,21 duration of attempted resuscitation22), that contribute to high-performing hospitals for IHCA. The lack of association between hospital rapid response teams and incidence and survival outcomes of cardiac arrest is not unexpected in light of the mixed results of prior studies.17,23,24 Additional study is needed to further inform consistent aspects of high-quality IHCA care and define approaches to apply these findings in quality improvement activities for the achievement of lower incidence and better survival of IHCA.
The study should be considered in light of the following limitations. First, patients with IHCA were identified from administrative codes that have been applied in prior studies.10 However, this approach may be less specific than studies using clinical data to identify IHCA and may contribute to the higher IHCA survival rates in the present study as compared with prior studies of IHCA.2 Furthermore, there is potential for misclassification of out-of-hospital arrests or non-arrests by ICD-9 codes. Separately, in chart review of 67 study patients, we determined the positive-predictive value of ICD codes for in-hospital cardiac arrest in the VA is high (76%) and similar to that of other conditions.25,26 Second, although our approach to risk-adjustment was robust given the flexibility of the MARS model and the large number of covariates for adjustment, we lacked clinical details at the time of cardiac arrest (e.g., arrest rhythm, time to chest compressions, time to defibrillation, time of arrest, rapid response team activation) and residual confounding cannot be excluded in this observational analysis. Furthermore, our study lacks details on the timing of arrest, which could inform aspects of utilization (length of stay, diagnostic and therapeutic procedures) and care (on- vs off-hours arrest outcomes). These are areas for future study. Third, not all hospitals participated in the quality of care survey, which limits the generalizability and raises concern for differential participation. However, IHCA incidence and survival outcomes were similar across participating and non-participating hospitals. Finally, as do not resuscitate (DNR) orders are not captured in national VA data, we cannot exclude the potential for differential use of DNR orders over the period of study which could contribute to differential patient selection and IHCA survival over time. The stability of incidence rates of IHCA over time somewhat discounts this concern. Further study is needed to understand the implications of DNR use on measures of the incidence and outcomes of IHCA, which could have changed over time.
In conclusion, trends in the incidence and survival of IHCA have improved in the VA. However, large hospital-level variation in the incidence and survival of IHCA are suggestive of important variation in the quality of care delivery related to in-hospital resuscitation. General measures of quality improvement activities did not correlate well with IHCA and outcomes. Identification of specific quality improvement activities associated with low incidence and high survival of IHCA may guide further improvements in in-hospital resuscitation.
Supplementary Material
Table 1.
Characteristics of Hospitalizations and IHCA Hospitalizations, 2008–2012, including selected Elixhauser comorbidities and lab values
| Characteristics | All Hospitalizations N=2,205,123 | IHCA Hospitalizations N=8,821 (0.4% of all hospitalizations) |
|---|---|---|
| Age, years ± SD | 65.4 ± 13.02 | 69.3 ± 11.59 |
| Gender, N (%) | ||
| Male | 2,102,220 (95%) | 8,627 (98%) |
| Female | 102,903 (5%) | 194 (2%) |
| Race, N (%) | ||
| White/Caucasian | 1,589,885 (72%) | 6,055 (69%) |
| Black/African American | 369,867 (17%) | 1,815 (21%) |
| Unknown | 211,722 (10%) | 825 (9%) |
| Other | 33,649 (2%) | 126 (1%) |
| Comorbidities, total ± SD | 2.3 ± 1.65 | 2.8 ± 1.60 |
| Congestive Heart Failure | 257,492 (12%) | 1,828 (21%) |
| Hypertension | 946,077 (43%) | 2,888 (33%) |
| Diabetes, complicated | 120,116 (5%) | 581 (7%) |
| Diabetes, uncomplicated | 554,529 (25%) | 2,041 (23%) |
| Renal Failure | 305,206 (14%) | 2,089 (24%) |
| Chronic Pulmonary Disease | 407,320 (18%) | 1,760 (20%) |
| Select Lab Values on Admission | ||
| Albumin | 3.8±0.7 | 3.3±0.9 |
| White blood cell count | 9.4±21.1 | 12.0±13.8 |
| Glomerular filtration rate | 75.6±39.3 | 59.2±41.8 |
| Hematocrit | 37.9±6.6 | 35.4±7.2 |
| Admission Source, N (%) | ||
| VA Emergency Department | 1,110,833 (50%) | 4,338 (49%) |
| VA Outpatient Clinic | 987,093 (45%) | 3,587 (41%) |
| Other | 107,197 (5%) | 896 (10%) |
| Survive to Discharge, N (%) | 2,156,933 (98%) | 2,750 (31%) |
Acknowledgments
FUNDING
This study was funded by the Department of Veterans Affairs, Health Services Research & Development, IIR 13–079. Drs. Chan and Nallamothu are supported by funding (R01HL123980) from the National Heart Lung and Blood Institute.
Footnotes
Disclaimer: The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
REFERENCES
- 1.Merchant RM, Yang L, Becker LB, et al. Incidence of treated cardiac arrest in hospitalized patients in the United States. Crit Care Med. 2011;39(11):2401–2406. doi: 10.1097/CCM.0b013e3182257459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Girotra S, Nallamothu BK, Spertus JA, et al. Trends in survival after in-hospital cardiac arrest. N Engl J Med. 2012;367(20):1912–1920. doi: 10.1056/NEJMoa1109148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gage H, Kenward G, Hodgetts TJ, Castle N, Ineson N, Shaikh L. Health system costs of in-hospital cardiac arrest. Resuscitation. 2002;54(2):139–146. [DOI] [PubMed] [Google Scholar]
- 4.Paniagua D, Lopez-Jimenez F, Londoño JC, Mangione CM, Fleischmann K, Lamas GA. Outcome and cost-effectiveness of cardiopulmonary resuscitation after in-hospital cardiac arrest in octogenarians. Cardiology. 2002;97(1):6–11. doi:47412. [DOI] [PubMed] [Google Scholar]
- 5.Bradley SM, Huszti E, Warren SA, Merchant RM, Sayre MR, Nichol G. Duration of hospital participation in Get With the Guidelines-Resuscitation and survival of in-hospital cardiac arrest. Resuscitation. 2012;83(11):1349–1357. doi: 10.1016/j.resuscitation.2012.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Merchant RM, Yang L, Becker LB, et al. Variability in case-mix adjusted in-hospital cardiac arrest rates. Med Care. 2012;50(2):124–130. doi: 10.1097/MLR.0b013e31822d5d17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Merchant RM, Berg RA, Yang L, et al. Hospital variation in survival after in-hospital cardiac arrest. J Am Heart Assoc. 2014;3(1):e000400. doi: 10.1161/JAHA.113.000400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Girotra S, Cram P, Spertus JA, et al. Hospital variation in survival trends for in-hospital cardiac arrest. J Am Heart Assoc. 2014;3(3):e000871. doi: 10.1161/JAHA.114.000871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Restuccia JD, Mohr D, Meterko M, Stolzmann K, Kaboli P. The association of hospital characteristics and quality improvement activities in inpatient medical services. J Gen Intern Med. 2014;29(5):715–722. doi: 10.1007/s11606-013-2759-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ehlenbach WJ, Barnato AE, Curtis JR, et al. Epidemiologic study of in-hospital cardiopulmonary resuscitation in the elderly. N Engl J Med. 2009;361(1):22–31. doi: 10.1056/NEJMoa0810245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sohn M-W, Arnold N, Maynard C, Hynes DM. Accuracy and completeness of mortality data in the Department of Veterans Affairs. Popul Health Metr. 2006;4:2. doi: 10.1186/1478-7954-4-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. [DOI] [PubMed] [Google Scholar]
- 13.Render ML, Deddens J, Freyberg R, et al. Veterans Affairs intensive care unit risk adjustment model: validation, updating, recalibration. Crit Care Med. 2008;36(4):1031–1042. doi: 10.1097/CCM.0b013e318169f290. [DOI] [PubMed] [Google Scholar]
- 14.Render ML, Kim HM, Welsh DE, et al. Automated intensive care unit risk adjustment: results from a National Veterans Affairs study. Crit Care Med. 2003;31(6):1638–1646. doi: 10.1097/01.CCM.0000055372.08235.09. [DOI] [PubMed] [Google Scholar]
- 15.Prescott HC, Kepreos KM, Wiitala WL, Iwashyna TJ. Temporal Changes in the Influence of Hospitals and Regional Healthcare Networks on Severe Sepsis Mortality. Crit Care Med. 2015;43(7):1368–1374. doi: 10.1097/CCM.0000000000000970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Efendijev I, Raj R, Reinikainen M, Hoppu S, Skrifvars MB. Temporal trends in cardiac arrest incidence and outcome in Finnish intensive care units from 2003 to 2013. Intensive Care Med. 2014;40(12):1853–1861. doi: 10.1007/s00134-014-3509-z. [DOI] [PubMed] [Google Scholar]
- 17.Fennessy G, Hilton A, Radford S, Bellomo R, Jones D. The epidemiology of in-hospital cardiac arrests in Australia and New Zealand. Intern Med J. 2016;46(10):1172–1181. doi: 10.1111/imj.13039. [DOI] [PubMed] [Google Scholar]
- 18.Curry LA, Spatz E, Cherlin E, et al. What distinguishes top-performing hospitals in acute myocardial infarction mortality rates? A qualitative study. Ann Intern Med. 2011;154(6):384–390. doi: 10.7326/0003-4819-154-6-201103150-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McHugh MD, Rochman MF, Sloane DM, et al. Better Nurse Staffing and Nurse Work Environments Associated With Increased Survival of In-Hospital Cardiac Arrest Patients. Med Care. 2016;54(1):74–80. doi: 10.1097/MLR.0000000000000456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chan PS, Nichol G, Krumholz HM, Spertus JA, Nallamothu BK, American Heart Association National Registry of Cardiopulmonary Resuscitation (NRCPR) Investigators. Hospital variation in time to defibrillation after in-hospital cardiac arrest. Arch Intern Med. 2009;169(14):1265–1273. doi: 10.1001/archinternmed.2009.196. [DOI] [PubMed] [Google Scholar]
- 21.Anderson ML, Nichol G, Dai D, et al. Association Between Hospital Process Composite Performance and Patient Outcomes After In-Hospital Cardiac Arrest Care. JAMA Cardiol. 2016;1(1):37–45. doi: 10.1001/jamacardio.2015.0275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goldberger ZD, Chan PS, Berg RA, et al. Duration of resuscitation efforts and survival after in-hospital cardiac arrest: an observational study. Lancet Lond Engl. 2012;380(9852):1473–1481. doi: 10.1016/S0140-6736(12)60862-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chan PS, Khalid A, Longmore LS, Berg RA, Kosiborod M, Spertus JA. Hospital-wide code rates and mortality before and after implementation of a rapid response team. JAMA. 2008;300(21):2506–2513. doi: 10.1001/jama.2008.715. [DOI] [PubMed] [Google Scholar]
- 24.Chan PS, Jain R, Nallmothu BK, Berg RA, Sasson C. Rapid Response Teams: A Systematic Review and Meta-analysis. Arch Intern Med. 2010;170(1):18–26. doi: 10.1001/archinternmed.2009.424. [DOI] [PubMed] [Google Scholar]
- 25.McCormick N, Lacaille D, Bhole V, Avina-Zubieta JA. Validity of heart failure diagnoses in administrative databases: a systematic review and meta-analysis. PloS One. 2014;9(8):e104519. doi: 10.1371/journal.pone.0104519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McCormick N, Bhole V, Lacaille D, Avina-Zubieta JA. Validity of Diagnostic Codes for Acute Stroke in Administrative Databases: A Systematic Review. PloS One. 2015;10(8):e0135834. doi: 10.1371/journal.pone.0135834. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.