Abstract
One-fifth of cancer deaths are associated with obesity. Because the molecular mechanisms by which obesity affects the progression of ovarian cancer (OC) are poorly understood, we investigated if obesity could promote the progression of OC cells using the postmenopausal ob/ob mouse model and peritoneal dissemination of mouse ID8 OC cells. Compared to lean mice, obese mice had earlier OC occurrence, greater metastasis throughout the peritoneal cavity, a trend toward shorter survival, and higher circulating glucose and proinflammatory chemokine CXCL1 levels. Ascites in obese mice had higher levels of macrophages (Mφ) and chemokines including CCL2, CXCL12, CXCL13, G-CSF and M-CSF. Omental tumor tissues in obese mice had more adipocytes than lean mice. Our data suggest that obesity may accelerate the peritoneal dissemination of OC through higher production of pro-inflammatory chemokines and Mφ recruitment.
Keywords: Obesity, Macrophages, Chemokines, Ascites, Ovarian cancer
INTRODUCTION
The prevalence of obesity is rapidly and globally increasing (1). Obesity reduces human life expectancy and increases risks of multiple malignancies (2,3). In 2018, approximately 22,240 new cases and 14,070 deaths from ovarian cancer (OC) are expected in the United States (4). Despite OC being the 5th leading cause of cancer deaths among U.S. women and frequent spread through the peritoneal cavity rather than blood vessels (5), how obesity influences the progression of OC is not fully understood. Epidemiological evidence indicates controversial results between obesity and OC survival: both a positive relationship (6,7,8,9) and no relationship (10,11,12) have been reported. Despite this controversy, obesity appears as a risk factor for OC (13,14,15) and leads to poorer quality-of-life outcomes in patients with OC (16,17,18). Interestingly, obesity in early adulthood is linked with higher mortality in OC (12,19,20). Obesity induces chronic inflammation which can lead to adverse health conditions such as cardiovascular disease, diabetes and some cancers. Obesity-associated inflammatory mediators may modify the tumor microenvironment, leading to cancer progression (21,22). Adipose tissues release growth factors and cytokines such as adiponectin, leptin, TNF-α, IL-6 and IL-8/CXCL8 (23). Chronic inflammation has been shown to involve a chemokine network that influences the migration and invasion of cancer cells (24,25), which support the tumor microenvironment for cancer progression by increasing inflammatory burden. We found that obesity could launch an inflammatory burden for OC progression via CXCR2-mediated signaling. OC cells produce high levels of CXCR2-specific chemokines such as CXCL1-3 and 8 (26,27) in a NF-κB-dependent manner (28,29). Furthermore, CXCR2-mediated signaling could be a central adipocyte-driven chemokine network (30), linking obesity and OC. Our recent study shows that CXCR2 is a negative regulator of p21 via Akt-mediated Mdm2 in OC, contributing to OC proliferation (31). High-grade serous ovarian cancer (HGSOC), the most common OC subtype, has highly mutated p53 tumor suppressor protein (up to 96%) (32). CXCR2-deriven progression of OC further enhances CXCR2-specific chemokines by potentiating NF-κB via epidermal growth factor receptor-transactivated Akt signaling (33). Functional restoration of p53 repressed CXCR2-specific chemokines CXCL1-3 and 8 in p53 mutant (p53m) OC cells (26). Our recent study indicates that CXCR2 associates with poor overall survival in p53m HGSOC (34), suggesting an involvement of CXCR2 in the high mortality of HGSOC compared to other OC subtypes. These facts indicate that obesity-induced chronic inflammation may enhance the inflammatory burden in OC followed by a high mortality via the accelerated progression of OC.
Because the relationship between obesity and OC survival remains controversial, we investigated if obesity could promote the progression of OC cells using the postmenopausal obese mouse model and the peritoneal dissemination of mouse ID8 OC cells, focusing on immune cell profile and cytokine signature in OC-induced ascites.
MATERIALS AND METHODS
Generation of stable ID8 luciferase (ID8Luc) OC cell line and culture
ID8Luc cells were generated from parental ID8 OC cells as described previously (35). Cells were cultured at 37°C in a water-saturated atmosphere of 95% air and 5% CO2 with DMEM containing penicillin/streptomycin (each 100 U/ml) and 4% FBS. All liquid culture media were acquired from Invitrogen (Grand Island, NY, USA).
Mouse peritoneal syngeneic model
Mouse peritoneal syngeneic model was performed under guidelines approved by the Institutional Animal Care and Use Committee at Meharry Medical College and the National Institutes of Health (NIH) guide for the Care and Use of Laboratory Animals. Wild-type (WT, C57BL/6J) and ob/ob mice (OB, B6.V-Lepob/J) were obtained from Jackson Laboratory (Bar Harbor, ME, USA). The mice were maintained in a specific pathogen free animal housing facility at 22°C±2°C and 40%–60% humidity under a 12:12 light: dark cycle. Nine-week old female mice were ovariectomized (OVX) for the peritoneal dissemination model of postmenopausal obesity and the OVX mice were maintained on a standard diet throughout the experimental period. ID8Luc OC cells (3×106 cells/mouse in a volume of 0.2 ml PBS) were injected intraperitoneally into WT and OB mice after complete recovery from OVX procedure and confirmation of weight gain. Bioluminescence imaging were monitored weekly for tumor growth. Briefly, mice anesthetized with 3% isoflurane were administered D-Luciferin (Cayman Chemical, Ann Arbor, MI, USA) intraperitoneally at 125 mg/kg, 5 min before acquisition of the image. Mice were then placed in the chamber of an In-Vivo MS FX PRO optical imaging system (Carestream, Rochester, NY, USA), and photons were collected for a period of 1 min. The luminescent intensity of the region of interest were quantified using Molecular Imaging software (Carestream). We monitored body weight and terminated the mice upon irreversible accumulation of ascites (up to 8–10 ml). Mice were monitored 3 times weekly to assess animal health such as hunched posture, lethargy and inactivity, impaired ambulation, shallow or labored breathing, hair coat condition and change in the body weight. In particular, mice showing clinical signs of ascites fluid production with constant increase of body weight and changes in appearance and activity were observed daily. When 20% increase in the body weight, extensive ascites accumulation or sluggish activity were observed, animals were terminated for humane reasons. Particularly, solid tumors from the diaphragm, omentum and pelvic sites were investigated for spreading index followed by histological examination using H&E staining. The survival time of the mice were compared between WT and OB mice with ID8Luc OC cells.
ELISA
CXCL1 levels in ascites and serum were measured by murine KC (CXCL1) ELISA kit (900-K127; PeproTech, Rocky Hill, NJ, USA) according to the manufacturer's instructions. The optical density of each well was determined using a microplate reader set to 405 nm with wavelength correction at 570 nm. Glucose levels in ascites and serum were measured by Glucose Colorimetric Assay Kit (Cayman Chemical). The optical density of each well was determined using a microplate reader at 514 nm wavelength.
FACS
Immune cell profiles in ascites were evaluated by FACS with the following specific antibodies for leukocyte subtypes: PerCP-Cy™ 5.5 Rat Anti-Mouse CD335 [NKp46] for NK cells; Alexa Fluor® 647 Rat Anti-Mouse F4/80 for macrophages (Mφ); PE Rat Anti-Mouse CD4 for CD4 T cells; and APC Rat Anti-Mouse CD8a for CD8 T cells (BD Biosciences, San Jose, CA, USA).
Proteomic array for cytokine signatures
Cytokine signatures in ascites were evaluated using Proteome Profiler Mouse Cytokine Array (ARY006; R&D Systems, Minneapolis, MN, USA).
PCR array and quantitative RT-PCR
PCR array for customized mouse chemokines (CAMP10242) was obtained from Qiagen (Frederick, MD, USA). After isolating total RNA from tumor samples and eliminating genomic DNA, the RT reaction was performed at 42°C for 15 min followed by 94°C for 5 min. A real-time PCR for chemokines was performed according to manufacturer's instructions using a Bio-Rad CFX96 (Hercules, CA, USA) and the following 2-step cycling program: 1 cycle at 95°C for 10 min, and 40 cycles at 95°C for 15 s and at 60°C for 1 min. Data analysis was performed based on a Data Analysis Center (https://www.qiagen.com/us/shop/genes-and-pathways/data-analysis-center-overview-page/) provided by Qiagen.
Adipogenesis
The mouse fibroblast cell line 3T3-L1 (CL-173) was purchased from the American Type Culture Collection. Cells were cultured in DMEM with 10% calf serum (Invitrogen) at 37°C in a water-saturated atmosphere of 95% air and 5% CO2, avoiding situations in which the cells became too confluent (>70%) before the initiation of differentiation. Differentiation was performed as described previously (30). Undifferentiated and differentiated cells were washed with sterile Dulbecco's phosphate-buffered saline and cultured for an additional 48 h in complete DMEM media followed by centrifuged conditioned media (CM) collection and storage at −80°C for future use.
Cell proliferation
Cell proliferation assay was performed using the cleavage of MTT to a colored product as described previously (31).
Cell migration
ID8 cells (2×105 cells/ml in serum-free DMEM with 1% BSA) to be used for a migration assay were seeded in the 24-well Transwell cell culture insert (VWR Corp., Radnor, PA, USA). The bottom chamber contained 0.5 ml DMEM supplemented with 10% FBS as a chemoattractant. Cells were treated as indicated in Results and then incubated for 24 h. The cells that remained inside the insert were removed with a cotton swab; migrating cells on the filter were fixed with 3.7% formaldehyde and stained with 0.1% crystal violet followed by washing of the cells with PBS. The number of migrating cells was counted under the microscope (×400) using 5 randomly chosen fields.
Statistics
Data were expressed as mean±standard error and analyzed by the paired Student's t-test to detect statistical significance (p<0.05).
RESULTS AND DISCUSSION
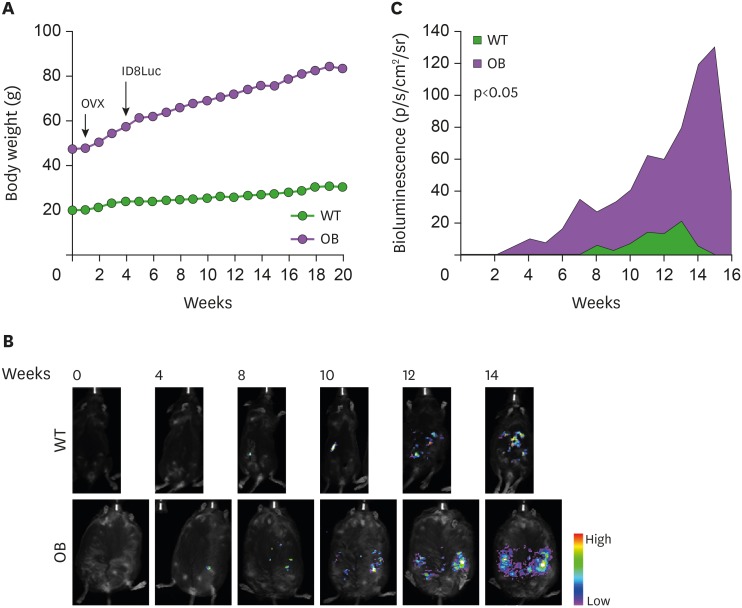
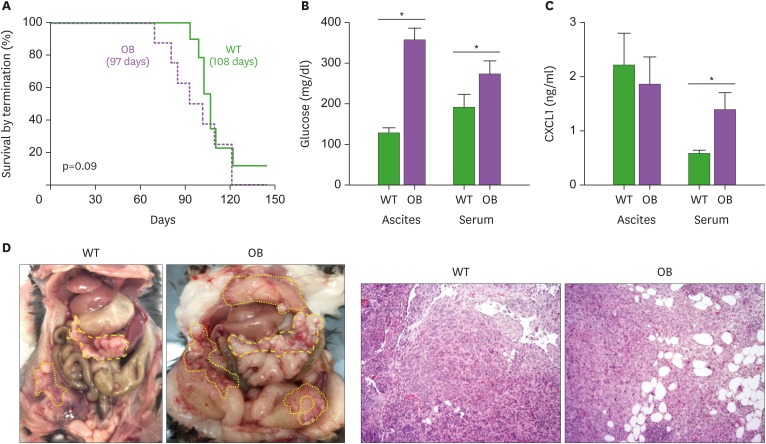
Older women have higher rates of diagnosis and death from OC (36) and activation of estrogen receptor prevents fat accumulation (37). Because ovariectomy eliminates the protection of female mice from gaining body weight (38), we used OVX WT and OB mice on standard diets to reflect a postmenopausal status. In agreement with another study (39), obese mice gained 2-fold more body weight than WT mice (Fig. 1A). The OB mouse is leptin-deficient, resulting in obesity via hyperphagia despite a standard diet (40). We generated ID8Luc cells from parental mouse ovarian surface epithelial ID8 OC cells using stable transfection. Bioluminescence imaging revealed that tumors in obese mice were detected at earlier time points and were more widely spread metastasis of OC cells in the peritoneal cavity than lean mice (Fig. 1B). Bioluminescence intensity showed statistical significance in obese mice throughout the whole experimental period compared to lean mice (Fig. 1C). Other studies using the K18-gT121+/−; p53fl/fl; Brca1fl/fl (KpB) mice for serous epithelial OC model revealed that mice fed with a high-fat diet had larger tumor volume and heavier tumor weight than mice fed with a low-fat diet (41,42), supporting our results showing more widespread metastasis of OC in the peritoneal cavity (Fig. 1B and C). Compared to lean mice (109 days), obese mice showed a shorter survival trend (97 days) following termination due to ascitic fluid accumulation as defined by humane endpoints (Fig. 2A). Ascitic fluid accumulation was easily detected in lean mice, while it was difficult to observe in obese mice due to a larger body size. This fact might have caused survival in obese mice to be overestimated. Obese mice had higher levels of glucose in both ascites and serum than lean mice (Fig. 2B), consistent with increased levels of blood glucose in mice fed with a high-fat diet (42). Obese mice had higher serum levels of CXCL1 but similar levels in ascites (Fig. 2C). Higher serum levels of CXCL1 indicate a systemic inflammatory burden in obese mice, which may promote cancer progression as suggested by our previous studies (26,33,35). Similarly, increased serum CXCL1 and CXCL5 were associated with increased obesity in db/db mice (43). In addition, CXCL1 is required for obesity-dependent tumor adipose stromal cell recruitment, vascularization and tumor growth promotion (44). Obese mice had more tumor burden in the peritoneal cavity, showing the wider peritoneal dissemination of ID8Luc cells, compared to lean mice (Fig. 2D). These results are consistent with other report showing enhanced intraperitoneal tumor burden in overweight or obese mice (39). Furthermore, histological evaluation revealed that omental tumor tissues in obese mice had more adipocytes (Fig. 2D).
Figure 1. The peritoneal dissemination of OC in postmenopausal obese mouse model. (A) Body weight in WT (n=9) and OB (n=8) female mice. OVX WT and OB mice were fed with standard diets and generated mouse ID8Luc OC cells were injected intraperitoneally. (B) The tumor burden imaging in the peritoneal cavity of ID8Luc cell bearing mice measured by bioluminescence imaging. Representative pictures obtained from 9 WT and 8 OB mice. (C) Bioluminescence intensity in in the peritoneal cavity of ID8Luc cell bearing mice.
Figure 2. Parameters of the peritoneal dissemination of OC in postmenopausal obese mouse model. (A) Survival rate between WT (n=9) and OB (n=8) mice in the peritoneal dissemination model of OC cells. (B) Glucose levels in ascites and serum between WT and OB mice by ELISA. (C) CXCL1 levels in ascites and serum between WT and OB mice by ELISA. (D) Tumor burden and omental tumor tissues in the peritoneal cavity of ID8Luc cell bearing mice. Bold and thin yellow dots indicate the omental OC burden and the peritoneal OC dissemination, respectively. Representative pictures obtained from 9 WT and 8 OB mice.
*p<0.05.
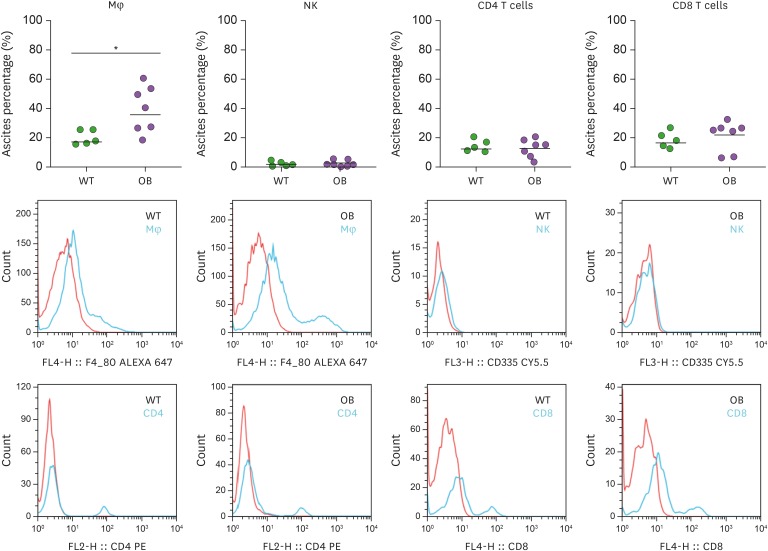
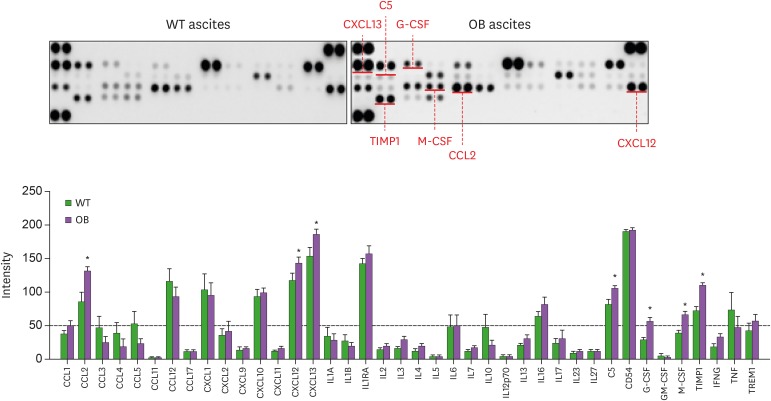
We investigated immune cell profiles in ascites produced by OC. Ascites in obese mice showed higher levels of Mφ, but similar levels of NK, CD4 T and CD8 T cells compared to lean mice (Fig. 3). Multiple lines indicate that tumor-associated Mφ (TAMs) play an important role in progression of OC: TAMs constitute over 50% of cells in malignant ascites (45); CD163+ TAMs infiltration was associated with poor prognosis of OC (46,47); high level of TAMs was associated with metastasis and advance of patients with OC (48); coculture of TAMs and SKOV3 OC cells increased the invasion ability of SKOV3 cells (48); M1-Mφ CM increased the metastatic potential, such as migration and invasion, in OC cells (49); and blocking Mφ function in mice with ID8 OC cells using a CSF-1 receptor kinase inhibitor (GW2580) reduced infiltration of M2-Mφ and decreased ascites volume (50). Based on these facts, obesity-promoted Mφ infiltration in ascites may accelerate OC progression followed by high mortality. Furthermore, we investigated chemokine and cytokine signatures in ascites from obese and lean mice. Ascites in obese mice expressed higher levels of CCL2, CXCL12, CXCL13, complement component 5 (C5), G-CSF, M-CSF, and tissue inhibitors of metalloproteinase-1 (TIMP1) compared to those in lean mice (Fig. 4). Obesity is known to promote breast cancer by CCL2-mediated Mφ recruitment (51). Mφ accumulation in adipose tissue induced by a high-fat diet were reduced in CCL2 knockout (KO) mice compared to WT mice (52). Circulating levels of CCL2 were elevated in human obese subjects (53). These results may support obesity-derived CCL2-mediated Mφ recruitment in ascites produced by OC.
Figure 3. FACS analysis for immune cell profiles in the ascites of ID8Luc OC cell bearing WT (n=5) and OB (n=7) mice.
*p<0.05.
Figure 4. Chemokine and cytokine signatures in the ascites of ID8Luc OC cell bearing WT (n=5) and OB (n=7) mice by proteomic analysis.
*p<0.05.
Diet-induced obese mice demonstrated a robust increase of CXCL12 expression in white adipose tissues, recruiting Mφ (54). CXCL12-induced adipose tissue Mφ chemotaxis was mediated by CXCR7 in obesity but not leanness (55). CXCL12-CXCR4/CXCR7 signaling axis might drive Myc-induced prostate cancer in obese mice (56). CXCL12 protein was found to be up-regulated during differentiation of THP-1 monocytes (57). Polarized CD163+ TAMs were associated with increased CXCL12 expression in gastric cancer (58). These results also may support obesity-derived CXCL12-mediated Mφ recruitment in ascites produced by OC. We found previously that the dominant chemokine in adipocytes was CXCL13 during adipogenesis in 3T3-L1 cells (30), being consistent with a high level of CXCL13 in mature adipocytes (59). Monocyte-like and mature Mφ were found to produce CXCL13 in inflammatory lesions (60). These facts suggest that CXCL13 in ascites of OC may be potentiated by obesity and Mφ accumulation. Although expression levels of C5 are similar in adipocytes from lean and obese subjects (61), obese dogs with obesity-related metabolic dysfunction show increased C5 protein levels (62). So far roles of C5 in obesity and OC are poorly understood.
Although Mφ may promote colon cancer growth via a GM-CSF/heparin-binding epidermal growth factor-like growth factor paracrine loop that is enhanced by CXCL12 (63), ascites from OC have low levels of GM-CSF (Fig. 4). G-CSF treatment reduced body weight and increased energy expenditure in a diabetic rat model (64). On the other hand, M-CSF KO mice showed reduced body weight and monocytes in blood and spleen but no change in neutrophils compared to WT mice (65). The small intestinal lamina propria of G-CSF receptor KO mice harbored reduced numbers of Mφ compared to those of WT mice, but levels of neutrophil-like cells were similar between these mice (66). These results indicate that G-CSF in ascites of OC may be potentiated by Mφ accumulation rather than obesity. In high-fat diet-fed mice, mature adipocyte-induced CCL2 and M-CSF increase M2-Mφ in melanoma tumors (67). M-CSF enhanced OC tumorigenesis and metastasis (68). High-fat feeding increased Mφ infiltration into adipose tissues and serum levels of M-CSF and TIMP1 in BALB/c mice (69). On the other hand, there was no change in the expression of M-CSF in the adipose tissue from obese mice and only a minor change in Mφ infiltration (70). Mφ recruitment was reduced in the uterus of osteopetrotic mutant mice lacking M-CSF (71). Elevated Mφ infiltration into omental fat was observable in lean women and exaggerated by obesity, being paralleled by CCL2 and M-CSF mRNA levels (72). These results support obesity-derived M-CSF-mediated Mφ recruitment in ascites produced by OC. TIMP1 KO mice with high-fat diet had a lower body weight and less subcutaneous and gonadal fat mass compared to WT mice (73). TIMP1 was highly secreted by omental adipose tissue in human obesity (74) and circulating levels of TIMP1 were higher in obese women than in lean women (75). These results indicate that TIMP1 in ascites of OC may be potentiated by obesity rather than Mφ accumulation.
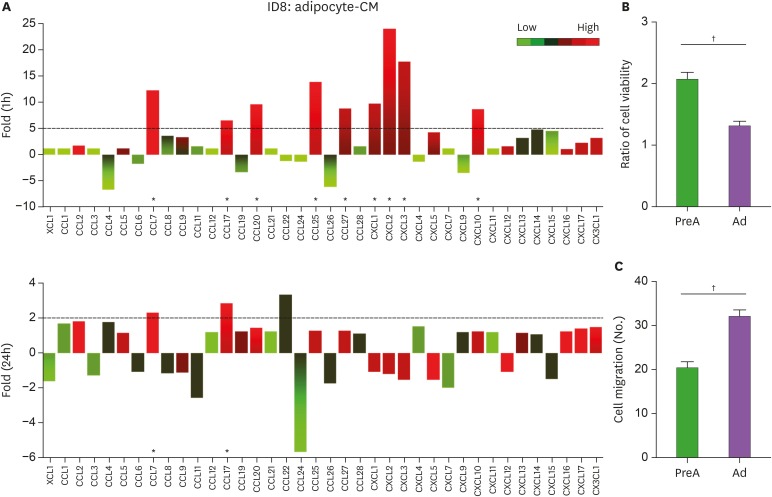
We compared chemokine signatures and functional roles between preadipocyte and adipocyte CM-treated ID8 OC cells. A short-term treatment (1 h) of adipocyte-CM in ID8 OC cells showed above 5-fold induction in CCL7, CCL17, CCL20, CCL25, CCL27, CXCL1, CXCL2, CXCL3 and CXCL10 compared to preadipocyte-CM (Fig. 5A). Dominant chemokines (above 15-fold) induced by adipocyte-CM were CXCL2 and CXCL3 (Fig. 5A). Long-term treatment (24 h) with adipocyte-CM diminished chemokines induced by short-term treatment, although maintaining above 2-fold induction in CCL7 and CCL17 (Fig. 5A). High-fat diet fed mice bearing prostate tumors showed higher levels of CXCL1 and CXCL2 expression compared to low-fat fed mice (76). CXCL1 is required for the obesity-dependent tumor adipose stromal cell recruitment, vascularization and tumor growth promotion in prostate cancer (44). OC cell lines expressed highly CXCL1-3 and 8 (35), while ovarian tumor tissues expressed highly CCL20 (35) and CXCL10 (34). The differential chemokine signatures between adipocyte-CM on ID8 cells and ascites from obese mice with ID8 OC cells may be due to tumor heterogeneity including cancer cells, adipocytes, stromal cells and immune cells. Interestingly, adipocyte-CM prefers cell migration to viability compared to preadipocyte-CM in ID8 OC cells (Fig. 5A and B). Adipocyte-CM increased the proliferation and migration of ID8 cells compared to basal media not preadipocyte-CM (77). In B16F1 melanoma and E0771 breast cancer cells, adipocyte-CM supported cell proliferation and migration compared to basal media not preadipocyte-CM (78). In RM1 prostate cancer cells, adipocyte-CM increased cell proliferation but had no effect on migration compared to preadipocyte-CM (79). MCF7 and MDA-MB-231 breast cancer cells showed higher migration in a cancer-associated adipocyte-CM than in normal breast adipocyte-CM but no change in cell proliferation (80). In LNCaP prostate cancer cells, periprostatic explants CM enhanced cell motility but inhibited proliferation compared to stromal-vascular fraction CM (81). Despite cancer type-specific effects of adipocyte-CM on cancer cells, generally it looks like to enhance cell migration and somewhat proliferation in obesity-related cancer.
Figure 5. Chemokine signatures and functional roles in preadipocyte- and adipocyte-CM treated ID8 OC cells. (A) Chemokine signatures in preadipocyte- and adipocyte-CM treated ID8 OC cells using PCR array containing complementary sequences for human chemokine genes. Expression levels of chemokines were defined as absent (light green), low (green area) and high (red area) on average threshold cycles. (B) Cell viability in preadipocyte- (PreA) and adipocyte-CM (Ad) treated ID8 OC cells n=3). (C) Cell migration in preadipocyte- (PreA) and adipocyte-CM (Ad) treated ID8 OC cells (n=3).
*Chemokines with >5 (1 h treatment) and >2 (24 h treatment)-fold increase were recognized as the major differences between preadipocyte- and adipocyte-CM; †p<0.05.
Based on our findings and other studies, obesity may accelerate the peritoneal dissemination of OC through systemically higher production of proinflammatory chemokines and increased Mφ recruitment in ascites.
ACKNOWLEDGMENTS
This research was supported, in whole or in part, by National Institutes of Health (NIH) as the following grants: R01ES024756 (E.L.), NIAID SC1AI089073 (D.S.), NCI SC1CA200519 (D.S.), and U54CA163069 (D.S., A.B., M.M.W.). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of NIH. In addition, the authors gratefully acknowledge the members and supporters of the Vanderbilt Ovarian Cancer Alliance.
Abbreviations
- C5
complement component 5
- CM
conditioned media
- HGSOC
high-grade serous ovarian cancer
- ID8Luc
ID8 luciferase
- KO
knockout
- Mφ
macrophages
- NIH
National Institutes of Health
- OB
ob/ob
- OC
ovarian cancer
- OVX
ovariectomized
- p53m
p53 mutant
- TAMs
tumor-associated Mφ
- TIMP1
tissue inhibitors of metalloproteinase-1
- WT
wild-type
Footnotes
Conflict of Interest: The authors declare no potential conflicts of interest.
- Conceptualization: Lee ES, Beeghly-Fadiel A, Whalen MM, Son DS.
- Data curation: Ignacio RM, Wilson AJ, Beeghly-Fadiel A, Whalen MM, Son DS.
- Formal analysis: Ignacio RM, Lee ES, Wilson AJ, Beeghly-Fadiel A, Whalen MM, Son DS.
- Funding acquisition: Lee ES, Beeghly-Fadiel A, Whalen MM, Son DS.
- Investigation: Ignacio RM, Lee ES, Wilson AJ, Beeghly-Fadiel A, Son DS.
- Methodology: Ignacio RM, Whalen MM, Son DS.
- Supervision: Son DS.
- Validation: Ignacio RM, Whalen MM, Son DS.
- Visualization: Son DS.
- Writing - original draft: Son DS.
- Writing - review & editing: Lee ES, Wilson AJ, Beeghly-Fadiel A, Whalen MM, Son DS.
References
- 1.Arroyo-Johnson C, Mincey KD. Obesity epidemiology worldwide. Gastroenterol Clin North Am. 2016;45:571–579. doi: 10.1016/j.gtc.2016.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 2003;348:1625–1638. doi: 10.1056/NEJMoa021423. [DOI] [PubMed] [Google Scholar]
- 3.Smith KB, Smith MS. Obesity statistics. Prim Care. 2016;43:121–135. doi: 10.1016/j.pop.2015.10.001. [DOI] [PubMed] [Google Scholar]
- 4.Torre LA, Trabert B, DeSantis CE, Miller KD, Samimi G, Runowicz CD, Gaudet MM, Jemal A, Siegel RL. Ovarian cancer statistics, 2018. CA Cancer J Clin. 2018;68:284–296. doi: 10.3322/caac.21456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yeung TL, Leung CS, Yip KP, Au Yeung CL, Wong ST, Mok SC. Cellular and molecular processes in ovarian cancer metastasis. A review in the theme: cell and molecular processes in cancer metastasis. Am J Physiol Cell Physiol. 2015;309:C444–C456. doi: 10.1152/ajpcell.00188.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pavelka JC, Brown RS, Karlan BY, Cass I, Leuchter RS, Lagasse LD, Li AJ. Effect of obesity on survival in epithelial ovarian cancer. Cancer. 2006;107:1520–1524. doi: 10.1002/cncr.22194. [DOI] [PubMed] [Google Scholar]
- 7.Diaz ES, Karlan BY, Li AJ. Obesity-associated adipokines correlate with survival in epithelial ovarian cancer. Gynecol Oncol. 2013;129:353–357. doi: 10.1016/j.ygyno.2013.02.006. [DOI] [PubMed] [Google Scholar]
- 8.Protani MM, Nagle CM, Webb PM. Obesity and ovarian cancer survival: a systematic review and meta-analysis. Cancer Prev Res (Phila) 2012;5:901–910. doi: 10.1158/1940-6207.CAPR-12-0048. [DOI] [PubMed] [Google Scholar]
- 9.Farrow DC, Weiss NS, Lyon JL, Daling JR. Association of obesity and ovarian cancer in a case-control study. Am J Epidemiol. 1989;129:1300–1304. doi: 10.1093/oxfordjournals.aje.a115249. [DOI] [PubMed] [Google Scholar]
- 10.Matthews KS, Straughn JM, Jr, Kemper MK, Hoskins KE, Wang W, Rocconi RP. The effect of obesity on survival in patients with ovarian cancer. Gynecol Oncol. 2009;112:389–393. doi: 10.1016/j.ygyno.2008.10.016. [DOI] [PubMed] [Google Scholar]
- 11.Skírnisdóttir I, Sorbe B. Prognostic impact of body mass index and effect of overweight and obesity on surgical and adjuvant treatment in early-stage epithelial ovarian cancer. Int J Gynecol Cancer. 2008;18:345–351. doi: 10.1111/j.1525-1438.2007.01013.x. [DOI] [PubMed] [Google Scholar]
- 12.Fairfield KM, Willett WC, Rosner BA, Manson JE, Speizer FE, Hankinson SE. Obesity, weight gain, and ovarian cancer. Obstet Gynecol. 2002;100:288–296. doi: 10.1016/s0029-7844(02)02053-7. [DOI] [PubMed] [Google Scholar]
- 13.Poorolajal J, Jenabi E, Masoumi SZ. Body mass index effects on risk of ovarian cancer: a meta- analysis. Asian Pac J Cancer Prev. 2014;15:7665–7671. doi: 10.7314/apjcp.2014.15.18.7665. [DOI] [PubMed] [Google Scholar]
- 14.Schildkraut JM, Alberg AJ, Bandera EV, Barnholtz-Sloan J, Bondy M, Cote ML, Funkhouser E, Peters E, Schwartz AG, Terry P, et al. A multi-center population-based case-control study of ovarian cancer in African-American women: the African American Cancer Epidemiology Study (AACES) BMC Cancer. 2014;14:688. doi: 10.1186/1471-2407-14-688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wu MM, Chen HC, Chen CL, You SL, Cheng WF, Chen CA, Lee TC, Chen CJ. A prospective study of gynecological cancer risk in relation to adiposity factors: cumulative incidence and association with plasma adipokine levels. PLoS One. 2014;9:e104630. doi: 10.1371/journal.pone.0104630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Smits A, Lopes A, Das N, Bekkers R, Galaal K. Quality of life in ovarian cancer survivors: the influence of obesity. Int J Gynecol Cancer. 2015;25:616–621. doi: 10.1097/IGC.0000000000000388. [DOI] [PubMed] [Google Scholar]
- 17.Kumar A, Bakkum-Gamez JN, Weaver AL, McGree ME, Cliby WA. Impact of obesity on surgical and oncologic outcomes in ovarian cancer. Gynecol Oncol. 2014;135:19–24. doi: 10.1016/j.ygyno.2014.07.103. [DOI] [PubMed] [Google Scholar]
- 18.Doll KM, Kalinowski AK, Snavely AC, Irwin DE, Bensen JT, Bae-Jump VL, Kim KH, Van Le L, Clarke-Pearson DL, Gehrig PA. Obesity is associated with worse quality of life in women with gynecologic malignancies: an opportunity to improve patient-centered outcomes. Cancer. 2015;121:395–402. doi: 10.1002/cncr.29061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Olsen CM, Green AC, Whiteman DC, Sadeghi S, Kolahdooz F, Webb PM. Obesity and the risk of epithelial ovarian cancer: a systematic review and meta-analysis. Eur J Cancer. 2007;43:690–709. doi: 10.1016/j.ejca.2006.11.010. [DOI] [PubMed] [Google Scholar]
- 20.Yang HS, Yoon C, Myung SK, Park SM. Effect of obesity on survival of women with epithelial ovarian cancer: a systematic review and meta-analysis of observational studies. Int J Gynecol Cancer. 2011;21:1525–1532. doi: 10.1097/IGC.0b013e31822eb5f8. [DOI] [PubMed] [Google Scholar]
- 21.Hursting SD, Digiovanni J, Dannenberg AJ, Azrad M, Leroith D, Demark-Wahnefried W, Kakarala M, Brodie A, Berger NA. Obesity, energy balance, and cancer: new opportunities for prevention. Cancer Prev Res (Phila) 2012;5:1260–1272. doi: 10.1158/1940-6207.CAPR-12-0140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sundaram S, Johnson AR, Makowski L. Obesity, metabolism and the microenvironment: Links to cancer. J Carcinog. 2013;12:19. doi: 10.4103/1477-3163.119606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rondinone CM. Adipocyte-derived hormones, cytokines, and mediators. Endocrine. 2006;29:81–90. doi: 10.1385/endo:29:1:81. [DOI] [PubMed] [Google Scholar]
- 24.Balkwill FR. The chemokine system and cancer. J Pathol. 2012;226:148–157. doi: 10.1002/path.3029. [DOI] [PubMed] [Google Scholar]
- 25.Mantovani A, Savino B, Locati M, Zammataro L, Allavena P, Bonecchi R. The chemokine system in cancer biology and therapy. Cytokine Growth Factor Rev. 2010;21:27–39. doi: 10.1016/j.cytogfr.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 26.Son DS, Kabir SM, Dong YL, Lee E, Adunyah SE. Inhibitory effect of tumor suppressor p53 on proinflammatory chemokine expression in ovarian cancer cells by reducing proteasomal degradation of IκB. PLoS One. 2012;7:e51116. doi: 10.1371/journal.pone.0051116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Son DS, Kabir SM, Dong Y, Lee E, Adunyah SE. Characteristics of chemokine signatures elicited by EGF and TNF in ovarian cancer cells. J Inflamm (Lond) 2013;10:25. doi: 10.1186/1476-9255-10-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Son DS, Parl AK, Rice VM, Khabele D. Keratinocyte chemoattractant (KC)/human growth-regulated oncogene (GRO) chemokines and pro-inflammatory chemokine networks in mouse and human ovarian epithelial cancer cells. Cancer Biol Ther. 2007;6:1302–1312. doi: 10.4161/cbt.6.8.4506. [DOI] [PubMed] [Google Scholar]
- 29.Son DS, Roby KF. Interleukin-1alpha-induced chemokines in mouse granulosa cells: impact on keratinocyte chemoattractant chemokine, a CXC subfamily. Mol Endocrinol. 2006;20:2999–3013. doi: 10.1210/me.2006-0001. [DOI] [PubMed] [Google Scholar]
- 30.Kabir SM, Lee ES, Son DS. Chemokine network during adipogenesis in 3T3-L1 cells: Differential response between growth and proinflammatory factor in preadipocytes vs. adipocytes. Adipocyte. 2014;3:97–106. doi: 10.4161/adip.28110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ignacio RM, Dong YL, Kabir SM, Choi H, Lee ES, Wilson AJ, Beeghly-Fadiel A, Whalen MM, Son DS. CXCR2 is a negative regulator of p21 in p53-dependent and independent manner via Akt-mediated Mdm2 in ovarian cancer. Oncotarget. 2018;9:9751–9765. doi: 10.18632/oncotarget.24231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cancer Genome Atlas Research Network. Integrated genomic analyses of ovarian carcinoma. Nature. 2011;474:609–615. doi: 10.1038/nature10166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dong YL, Kabir SM, Lee ES, Son DS. CXCR2-driven ovarian cancer progression involves upregulation of proinflammatory chemokines by potentiating NF-κB activation via EGFR-transactivated Akt signaling. PLoS One. 2013;8:e83789. doi: 10.1371/journal.pone.0083789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ignacio RM, Lee ES, Wilson AJ, Beeghly-Fadiel A, Whalen MM, Son DS. Chemokine network and overall survival in TP53 wild-type and mutant ovarian cancer. Immune Netw. 2018;18:e29. doi: 10.4110/in.2018.18.e29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ignacio RM, Kabir SM, Lee ES, Adunyah SE, Son DS. NF-κB-mediated CCL20 reigns dominantly in CXCR2-driven ovarian cancer progression. PLoS One. 2016;11:e0164189. doi: 10.1371/journal.pone.0164189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Harper EI, Sheedy EF, Stack MS. With great age comes great metastatic ability: ovarian cancer and the appeal of the aging peritoneal microenvironment. Cancers (Basel) 2018;10:E230. doi: 10.3390/cancers10070230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Arao Y, Hamilton KJ, Lierz SL, Korach KS. N-terminal transactivation function, AF-1, of estrogen receptor alpha controls obesity through enhancement of energy expenditure. Mol Metab. 2018;18:68–78. doi: 10.1016/j.molmet.2018.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hong J, Stubbins RE, Smith RR, Harvey AE, Núñez NP. Differential susceptibility to obesity between male, female and ovariectomized female mice. Nutr J. 2009;8:11. doi: 10.1186/1475-2891-8-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liu Y, Metzinger MN, Lewellen KA, Cripps SN, Carey KD, Harper EI, Shi Z, Tarwater L, Grisoli A, Lee E, et al. Obesity contributes to ovarian cancer metastatic success through increased lipogenesis, enhanced vascularity, and decreased infiltration of M1 macrophages. Cancer Res. 2015;75:5046–5057. doi: 10.1158/0008-5472.CAN-15-0706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ingalls AM, Dickie MM, Snell GD. Obese, a new mutation in the house mouse. J Hered. 1950;41:317–318. doi: 10.1093/oxfordjournals.jhered.a106073. [DOI] [PubMed] [Google Scholar]
- 41.Han J, Wysham WZ, Zhong Y, Guo H, Zhang L, Malloy KM, Dickens HK, Huh G, Lee D, Makowski L, et al. Increased efficacy of metformin corresponds to differential metabolic effects in the ovarian tumors from obese versus lean mice. Oncotarget. 2017;8:110965–110982. doi: 10.18632/oncotarget.20754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Makowski L, Zhou C, Zhong Y, Kuan PF, Fan C, Sampey BP, Difurio M, Bae-Jump VL. Obesity increases tumor aggressiveness in a genetically engineered mouse model of serous ovarian cancer. Gynecol Oncol. 2014;133:90–97. doi: 10.1016/j.ygyno.2013.12.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nunemaker CS, Chung HG, Verrilli GM, Corbin KL, Upadhye A, Sharma PR. Increased serum CXCL1 and CXCL5 are linked to obesity, hyperglycemia, and impaired islet function. J Endocrinol. 2014;222:267–276. doi: 10.1530/JOE-14-0126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhang T, Tseng C, Zhang Y, Sirin O, Corn PG, Li-Ning-Tapia EM, Troncoso P, Davis J, Pettaway C, Ward J, et al. CXCL1 mediates obesity-associated adipose stromal cell trafficking and function in the tumour microenvironment. Nat Commun. 2016;7:11674. doi: 10.1038/ncomms11674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gupta V, Yull F, Khabele D. Bipolar tumor-associated macrophages in ovarian cancer as targets for therapy. Cancers (Basel) 2018;10:E366. doi: 10.3390/cancers10100366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yuan X, Zhang J, Li D, Mao Y, Mo F, Du W, Ma X. Prognostic significance of tumor-associated macrophages in ovarian cancer: a meta-analysis. Gynecol Oncol. 2017;147:181–187. doi: 10.1016/j.ygyno.2017.07.007. [DOI] [PubMed] [Google Scholar]
- 47.Lan C, Huang X, Lin S, Huang H, Cai Q, Wan T, Lu J, Liu J. Expression of M2-polarized macrophages is associated with poor prognosis for advanced epithelial ovarian cancer. Technol Cancer Res Treat. 2013;12:259–267. doi: 10.7785/tcrt.2012.500312. [DOI] [PubMed] [Google Scholar]
- 48.Ke X, Zhang S, Wu M, Lou J, Zhang J, Xu T, Huang L, Huang P, Wang F, Pan S. Tumor-associated macrophages promote invasion via Toll-like receptors signaling in patients with ovarian cancer. Int Immunopharmacol. 2016;40:184–195. doi: 10.1016/j.intimp.2016.08.029. [DOI] [PubMed] [Google Scholar]
- 49.Cho U, Kim B, Kim S, Han Y, Song YS. Pro-inflammatory M1 macrophage enhances metastatic potential of ovarian cancer cells through NF-κB activation. Mol Carcinog. 2018;57:235–242. doi: 10.1002/mc.22750. [DOI] [PubMed] [Google Scholar]
- 50.Moughon DL, He H, Schokrpur S, Jiang ZK, Yaqoob M, David J, Lin C, Iruela-Arispe ML, Dorigo O, Wu L. Macrophage blockade using CSF1R inhibitors reverses the vascular leakage underlying malignant ascites in late-stage epithelial ovarian cancer. Cancer Res. 2015;75:4742–4752. doi: 10.1158/0008-5472.CAN-14-3373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Arendt LM, McCready J, Keller PJ, Baker DD, Naber SP, Seewaldt V, Kuperwasser C. Obesity promotes breast cancer by CCL2-mediated macrophage recruitment and angiogenesis. Cancer Res. 2013;73:6080–6093. doi: 10.1158/0008-5472.CAN-13-0926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kanda H, Tateya S, Tamori Y, Kotani K, Hiasa K, Kitazawa R, Kitazawa S, Miyachi H, Maeda S, Egashira K, et al. MCP-1 contributes to macrophage infiltration into adipose tissue, insulin resistance, and hepatic steatosis in obesity. J Clin Invest. 2006;116:1494–1505. doi: 10.1172/JCI26498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kim CS, Park HS, Kawada T, Kim JH, Lim D, Hubbard NE, Kwon BS, Erickson KL, Yu R. Circulating levels of MCP-1 and IL-8 are elevated in human obese subjects and associated with obesity-related parameters. Int J Obes. 2006;30:1347–1355. doi: 10.1038/sj.ijo.0803259. [DOI] [PubMed] [Google Scholar]
- 54.Kim D, Kim J, Yoon JH, Ghim J, Yea K, Song P, Park S, Lee A, Hong CP, Jang MS, et al. CXCL12 secreted from adipose tissue recruits macrophages and induces insulin resistance in mice. Diabetologia. 2014;57:1456–1465. doi: 10.1007/s00125-014-3237-5. [DOI] [PubMed] [Google Scholar]
- 55.Peng H, Zhang H, Zhu H. Blocking CXCR7-mediated adipose tissue macrophages chemotaxis attenuates insulin resistance and inflammation in obesity. Biochem Biophys Res Commun. 2016;479:649–655. doi: 10.1016/j.bbrc.2016.09.158. [DOI] [PubMed] [Google Scholar]
- 56.Saha A, Ahn S, Blando J, Su F, Kolonin MG, DiGiovanni J. Proinflammatory CXCL12-CXCR4/CXCR7 signaling axis drives Myc-induced prostate cancer in obese mice. Cancer Res. 2017;77:5158–5168. doi: 10.1158/0008-5472.CAN-17-0284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yu L, Yu L, Pham Q, Wang TT. Transcriptional and translational-uncoupling in regulation of the CXCL12 and its receptors CXCR4, 7 in THP-1 monocytes and macrophages. Immun Inflamm Dis. 2018;6:106–116. doi: 10.1002/iid3.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Park JY, Sung JY, Lee J, Park YK, Kim YW, Kim GY, Won KY, Lim SJ. Polarized CD163+ tumor-associated macrophages are associated with increased angiogenesis and CXCL12 expression in gastric cancer. Clin Res Hepatol Gastroenterol. 2016;40:357–365. doi: 10.1016/j.clinre.2015.09.005. [DOI] [PubMed] [Google Scholar]
- 59.Kusuyama J, Komorizono A, Bandow K, Ohnishi T, Matsuguchi T. CXCL3 positively regulates adipogenic differentiation. J Lipid Res. 2016;57:1806–1820. doi: 10.1194/jlr.M067207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Carlsen HS, Baekkevold ES, Morton HC, Haraldsen G, Brandtzaeg P. Monocyte-like and mature macrophages produce CXCL13 (B cell-attracting chemokine 1) in inflammatory lesions with lymphoid neogenesis. Blood. 2004;104:3021–3027. doi: 10.1182/blood-2004-02-0701. [DOI] [PubMed] [Google Scholar]
- 61.Kaye S, Lokki AI, Hanttu A, Nissilä E, Heinonen S, Hakkarainen A, Lundbom J, Lundbom N, Saarinen L, Tynninen O, et al. Upregulation of early and downregulation of terminal pathway complement genes in subcutaneous adipose tissue and adipocytes in acquired obesity. Front Immunol. 2017;8:545. doi: 10.3389/fimmu.2017.00545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Tvarijonaviciute A, Ceron JJ, de Torre C, Ljubić BB, Holden SL, Queau Y, Morris PJ, Pastor J, German AJ. Obese dogs with and without obesity-related metabolic dysfunction - a proteomic approach. BMC Vet Res. 2016;12:211. doi: 10.1186/s12917-016-0839-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rigo A, Gottardi M, Zamò A, Mauri P, Bonifacio M, Krampera M, Damiani E, Pizzolo G, Vinante F. Macrophages may promote cancer growth via a GM-CSF/HB-EGF paracrine loop that is enhanced by CXCL12. Mol Cancer. 2010;9:273. doi: 10.1186/1476-4598-9-273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lee Y, Song YS, Fang CH, So BI, Park JY, Joo HW, Park IH, Shen GY, Shin JH, Kim H, et al. Anti-obesity effects of granulocyte-colony stimulating factor in Otsuka-Long-Evans-Tokushima fatty rats. PLoS One. 2014;9:e105603. doi: 10.1371/journal.pone.0105603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hibbs ML, Quilici C, Kountouri N, Seymour JF, Armes JE, Burgess AW, Dunn AR. Mice lacking three myeloid colony-stimulating factors (G-CSF, GM-CSF, and M-CSF) still produce macrophages and granulocytes and mount an inflammatory response in a sterile model of peritonitis. J Immunol. 2007;178:6435–6443. doi: 10.4049/jimmunol.178.10.6435. [DOI] [PubMed] [Google Scholar]
- 66.Meshkibaf S, Gower MW, Dekaban GA, Kim SO. G-CSF preferentially supports the generation of gut-homing Gr-1high macrophages in M-CSF-treated bone marrow cells. J Leukoc Biol. 2014;96:549–561. doi: 10.1189/jlb.1A0314-172R. [DOI] [PubMed] [Google Scholar]
- 67.Jung JI, Cho HJ, Jung YJ, Kwon SH, Her S, Choi SS, Shin SH, Lee KW, Park JH. High-fat diet-induced obesity increases lymphangiogenesis and lymph node metastasis in the B16F10 melanoma allograft model: roles of adipocytes and M2-macrophages. Int J Cancer. 2015;136:258–270. doi: 10.1002/ijc.28983. [DOI] [PubMed] [Google Scholar]
- 68.Toy EP, Azodi M, Folk NL, Zito CM, Zeiss CJ, Chambers SK. Enhanced ovarian cancer tumorigenesis and metastasis by the macrophage colony-stimulating factor. Neoplasia. 2009;11:136–144. doi: 10.1593/neo.81150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kim EJ, Choi MR, Park H, Kim M, Hong JE, Lee JY, Chun HS, Lee KW, Yoon Park JH. Dietary fat increases solid tumor growth and metastasis of 4T1 murine mammary carcinoma cells and mortality in obesity-resistant BALB/c mice. Breast Cancer Res. 2011;13:R78. doi: 10.1186/bcr2927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sugita S, Kamei Y, Oka J, Suganami T, Ogawa Y. Macrophage-colony stimulating factor in obese adipose tissue: studies with heterozygous op/+ mice. Obesity (Silver Spring) 2007;15:1988–1995. doi: 10.1038/oby.2007.237. [DOI] [PubMed] [Google Scholar]
- 71.Shimada-Hiratsuka M, Naito M, Kaizu C, Shuying J, Hasegawa G, Shultz LD. Defective macrophage recruitment and clearance of apoptotic cells in the uterus of osteopetrotic mutant mice lacking macrophage colony-stimulating factor (M-CSF) J Submicrosc Cytol Pathol. 2000;32:297–307. [PubMed] [Google Scholar]
- 72.Harman-Boehm I, Blüher M, Redel H, Sion-Vardy N, Ovadia S, Avinoach E, Shai I, Klöting N, Stumvoll M, Bashan N, et al. Macrophage infiltration into omental versus subcutaneous fat across different populations: effect of regional adiposity and the comorbidities of obesity. J Clin Endocrinol Metab. 2007;92:2240–2247. doi: 10.1210/jc.2006-1811. [DOI] [PubMed] [Google Scholar]
- 73.Lijnen HR, Demeulemeester D, Van Hoef B, Collen D, Maquoi E. Deficiency of tissue inhibitor of matrix metalloproteinase-1 (TIMP-1) impairs nutritionally induced obesity in mice. Thromb Haemost. 2003;89:249–255. [PubMed] [Google Scholar]
- 74.Maury E, Ehala-Aleksejev K, Guiot Y, Detry R, Vandenhooft A, Brichard SM. Adipokines oversecreted by omental adipose tissue in human obesity. Am J Physiol Endocrinol Metab. 2007;293:E656–E665. doi: 10.1152/ajpendo.00127.2007. [DOI] [PubMed] [Google Scholar]
- 75.Maury E, Brichard SM, Pataky Z, Carpentier A, Golay A, Bobbioni-Harsch E. Effect of obesity on growth-related oncogene factor-alpha, thrombopoietin, and tissue inhibitor metalloproteinase-1 serum levels. Obesity (Silver Spring) 2010;18:1503–1509. doi: 10.1038/oby.2009.464. [DOI] [PubMed] [Google Scholar]
- 76.Hardaway AL, Herroon MK, Rajagurubandara E, Podgorski I. Marrow adipocyte-derived CXCL1 and CXCL2 contribute to osteolysis in metastatic prostate cancer. Clin Exp Metastasis. 2015;32:353–368. doi: 10.1007/s10585-015-9714-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Tebbe C, Chhina J, Dar SA, Sarigiannis K, Giri S, Munkarah AR, Rattan R. Metformin limits the adipocyte tumor-promoting effect on ovarian cancer. Oncotarget. 2014;5:4746–4764. doi: 10.18632/oncotarget.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Xiong Y, Russell DL, McDonald LT, Cowart LA, LaRue AC. Hematopoietic stem cell-derived adipocytes promote tumor growth and cancer cell migration. Int J Cancer Res Mol Mech. 2017;3 doi: 10.16966/2381-3318.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Moreira Â, Pereira SS, Costa M, Morais T, Pinto A, Fernandes R, Monteiro MP. Adipocyte secreted factors enhance aggressiveness of prostate carcinoma cells. PLoS One. 2015;10:e0123217. doi: 10.1371/journal.pone.0123217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Fujisaki K, Fujimoto H, Sangai T, Nagashima T, Sakakibara M, Shiina N, Kuroda M, Aoyagi Y, Miyazaki M. Cancer-mediated adipose reversion promotes cancer cell migration via IL-6 and MCP-1. Breast Cancer Res Treat. 2015;150:255–263. doi: 10.1007/s10549-015-3318-2. [DOI] [PubMed] [Google Scholar]
- 81.Ribeiro R, Monteiro C, Cunha V, Oliveira MJ, Freitas M, Fraga A, Príncipe P, Lobato C, Lobo F, Morais A, et al. Human periprostatic adipose tissue promotes prostate cancer aggressiveness in vitro. J Exp Clin Cancer Res. 2012;31:32. doi: 10.1186/1756-9966-31-32. [DOI] [PMC free article] [PubMed] [Google Scholar]