Abstract
Background:
Anaphylaxis is an acute, systemic allergic reaction that can be life threatening, and with an increasing incidence and costs associated with hospitalization and intensive care.
Objective:
To assess the risk factors for hospitalization by comparing pediatric and adult patients.
Methods:
We performed a retrospective chart review for patients with anaphylactic reactions who presented to the Albany Medical Center emergency department between 2005 and 2012.
Results:
We identified 267 anaphylactic reactions in 258 patients (143 adults). Of those, 128 (48%) were not coded as anaphylaxis despite fulfilling diagnostic criteria. Foods were the most common trigger both in adults and children. Factors associated with increased odds of hospitalization (intensive care unit [ICU] and hospital floor combined) included a severity score of 3 in both children (odds ratio [OR] 41.86 [95% confidence interval {CI}, 2.9–602.48], p = 0.006) and adults (OR 32.52 [95% CI, 6.28–168.35], p < 0.001), and those who received multiple doses of epinephrine in children (OR 15.36 [95% CI, 1.9–121.4], p = 0.009) and adults (OR 11.49 [95% CI, 3.08–44.13], p < 0.001). Patient characteristics associated with ICU admission in children and adults combined included Medicare and/or Medicaid insurance (OR 4.96 [95% CI, 1.14–21.67], p = 0.023), cutaneous symptoms (OR 0.19 [95% CI, 0.04–0.79], p = 0.23), and cardiovascular symptoms (OR 5.8 [95% CI, 1.16–28.87], p = 0.032).
Conclusion:
Anaphylaxis remains underrecognized and improperly treated in the emergency department. Severity of symptoms and receiving multiple doses of epinephrine were associated with hospitalization in both children and adults. Medicare and/or Medicaid insurance, and cardiovascular or cutaneous symptoms were characteristics associated with ICU admission in our cohort.
Keywords: Anaphylaxis, food allergy, epinephrine, insurance, drug allergy, allergic reaction, urticaria, emergency, insect allergy, hospitalization
Anaphylaxis is a life-threatening allergic reaction that is frequently seen in emergency departments (ED). Previous studies reported an increasing incidence in anaphylaxis.1–5 Symptoms may present rapidly and can be followed by airway compromise, respiratory distress, hemodynamic instability, and, potentially, death.6,7 Potential allergic triggers that cause anaphylaxis include food, medications, latex, and insect stings.1,8 Early recognition and rapid treatment are cornerstones of therapy for anaphylaxis and are often life saving. A lack of recognition and delayed treatment of anaphylaxis may lead to disastrous and fatal outcomes. Therefore, identification of causative factors, avoidance of triggers, recognition of typical and atypical symptoms, and rapid treatment remain the backbone of optimal care for patients with anaphylaxis.
In the United States, foods, including peanuts, tree nuts, and seafood, remain a major contributor of allergic reactions and anaphylaxis.9 Medication-induced anaphylaxis, common in the adult population, has led to increased hospitalizations and mortality rates over the past decade.10 With increasing incidences and costs associated with hospitalization and intensive care, we sought to assess the risk factors for hospitalization in both pediatric and adult populations in an upstate New York ED. This may offer an opportunity for improvement in care in at-risk groups and in cost reduction.
METHODS
Patient Selection
We reviewed the electronic records of children and adults with anaphylaxis who presented to the Albany Medical Center ED. The ED is a level 1 tertiary center, with an annual census of >70,000 patients and services an urban, suburban, and rural population that encompasses >20 counties in three different states and consists of distinct adult and pediatric zones but not a separate pediatric ED. Medical records of patients from September 1, 2005, through March 21, 2012, were reviewed and divided into two groups: adults and children (ages ≤21 years). Charts were reviewed for International Classification of Diseases, Ninth Revision codes,11 including “adverse food reaction, not elsewhere classified” (995.7); “allergic urticaria” (708.0); “allergy unspecified, not elsewhere classified” (995.3); “anaphylaxis” (995.0); “anaphylactic reaction due to food (995.6), peanuts (995.61), tree nuts and seeds (995.64), vaccinations (999.42), crustaceans (995.62), fish (995.65), food additives (995.66), fruits and vegetables (995.63); “cholinergic urticaria” (708.5); “dermatographic urticaria” (708.3); “drug allergy” (995.27); “idiopathic urticaria” (708.1); “unspecified urticaria” (708.9); “urticaria other” (708.8); and “urticaria due to cold and heat” (708.2).
Even if the diagnostic code for anaphylaxis was not used, patients who met the Second Symposium criteria8 were included in the study. Demographics, type of insurance, area of residence (urban, suburban, rural), mode of transportation, atopic history, chief concerns, suspected triggers, time from exposure to onset of symptoms, symptoms, physical examination findings, medications administered, response to treatment, and disposition were recorded and analyzed. This study was approved by the internal review board of the Albany Medical Center, Albany, New York.
Definition and Severity of Anaphylaxis
We used the summary report from the Second National Institute of Allergy and Infectious Disease/Food Allergy and Anaphylaxis Network Symposium12 to diagnose anaphylaxis cases. The severity of anaphylaxis was assessed by using a 3-point scale.13
Statistical Analysis
The analyses were performed by using version 9.4 of the SAS System for Windows (SAS institute Inc., Cary, NC). The Student's t-test and the χ2 test were used to compare demographics, patient characteristics, and symptoms between patients with anaphylaxis and those without anaphylaxis. Mantel-Haenszel test statistics were used to evaluate the associations of ordinal measures, e.g., symptom severity. Exploratory bivariate analyses were performed to evaluate the associations between patient disposition and various clinical risk factors and patient characteristics. Variables found to be associated with disposition in preliminary analyses were further examined by using multiple logistic regression after controlling for patient age. The regression analyses were carried out separately for children and adult samples when considering the heterogeneity of the two populations. Generalized logistic regression was performed to evaluate the association between patient characteristics and being admitted to hospital. All the tests were two-sided, and a p < 0.05 was considered statistically significant.
RESULTS
Demographics and Triggers
A total of 2463 charts over a 7-year period were reviewed during the initial screen. We identified 267 cases of anaphylaxis in which 143 (53.6%) were adults (ages, 22–85 years) and 124 (46.4%) were children (ages 7 months to 21 years). The demographics of the subjects are presented in Table 1. The mean age in the adult population was 39.9 years and, in the pediatric population, was 11.4 years. These 267 anaphylactic reactions in 258 patients represented 11% of the total caseload from the initial screening of patients with allergic symptoms.
Table 1.
Patient demographics, clinical characteristics, residence, and anaphylactic reaction-related mode of transportation, trigger, and disposition assessed in the emergency department
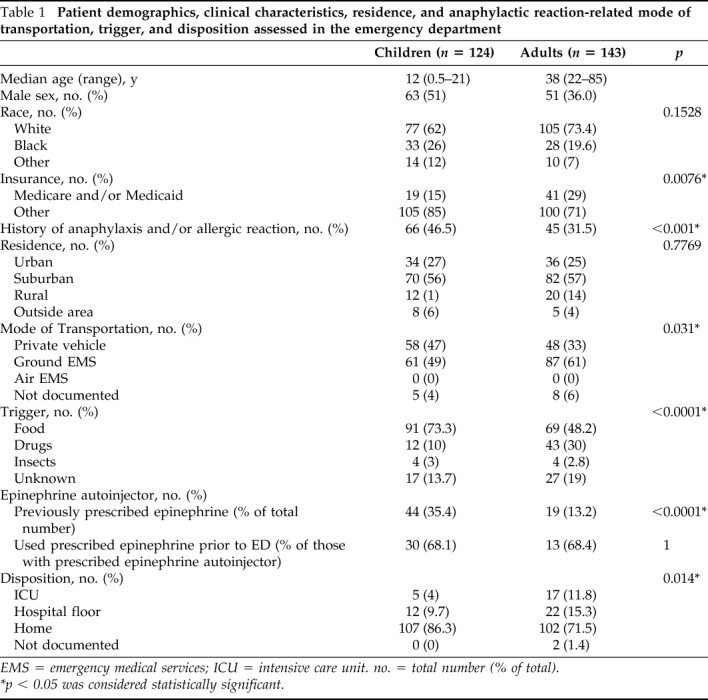
EMS = emergency medical services; ICU = intensive care unit. no. = total number (% of total).
*p < 0.05 was considered statistically significant.
The children were more likely to have a history of anaphylaxis or an allergic reaction compared with adults (46.5 versus 31.5%; p < 0.001) and to have an epinephrine autoinjector at home (35.4 versus 13.2%; p < 0.0001). Interestingly, in both children and adults who had an epinephrine autoinjector at home, epinephrine was self-administered at similar rates (68.1% in children versus 68.4% in adults). Of the patients evaluated in the ED, 184 were identified as residing in rural or suburban areas, and 70 were identified as residing in an urban location. Mode of transportation differed between adults and children (p = 0.031). Children were transported to the ED in private vehicles more often than adults (47 versus 33%); adults were transported more often by ground Emergency Medical Services (61 versus 41%). There were no children or adults who needed air transport in our study.
Triggers of anaphylaxis differed significantly between adults and children (p < 0.001). Food was the most common trigger in both the adult and pediatric populations, although more common in children than in adults (73.4 versus 47.9%). Adults were more likely to have drugs as a trigger than children (30 versus 10%). Insect stings and unknown etiology were seen equally as often in adults and children. Of 267 patients total, 6 (2%) had repeated visits to the ED (Supplemental Table 1). Of these repeated visits five were female patients (83%), with median age of 29.5 years (range, 4–54 years). All of the repeated visits had food as a trigger, and four patients had a known food allergy. Five patients received epinephrine prescription at discharge, and only two patients were referred to an allergist at discharge.
Adults Presented with More Severe Symptoms When Compared to Children But Did Not Receive Epinephrine at Higher Rates
The conditions of 66 adults (46%) and 62 children (50%) were not coded as anaphylaxis despite fulfilling the criteria for anaphylaxis (Table 2). Common diagnoses that were given instead included allergic reaction and allergic urticaria. When using the severity criteria by Huang et al.,13 most reactions were mild to moderate in severity. Adults more often than children met the grading criteria for a severe reaction (13 versus 5%). Adults, but not children, whose conditions were coded as having anaphylaxis presented more often with hypotension (p = 0.006) and loss of consciousness (p = 0.01) whereas those reactions, including hives, were more commonly coded as nonanaphylactic (p = 0.002). When comparing presentation in adults and children, adults presented more often with difficulty breathing (p = 0.04) and with hypotension (p = 0.03) than did children, whereas children more often had emesis (p = 0.002) (Table 2).
Table 2.
Coding of anaphylaxis and associated severity, symptoms and treatment between children and adults
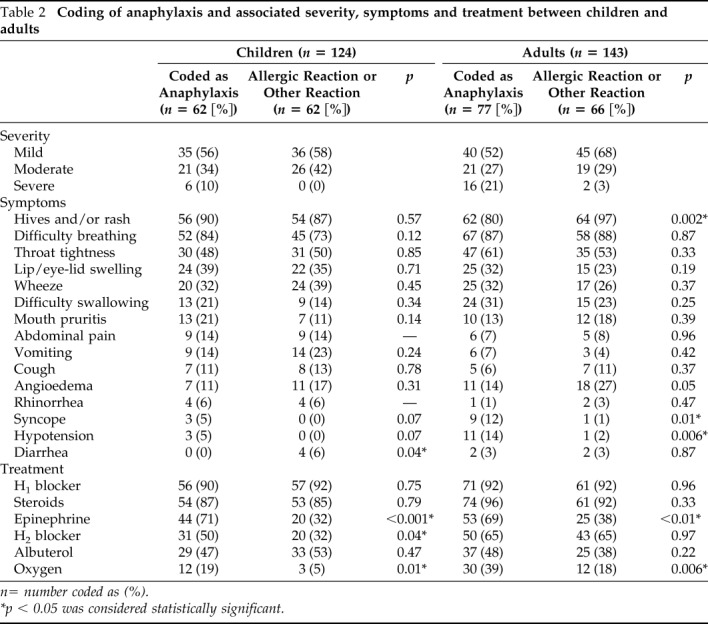
n= number coded as (%).
*p < 0.05 was considered statistically significant.
The most common treatment was antihistamine, followed by oral or parenteral steroid medications and epinephrine. Oxygen was administered more often in those coded as anaphylactic reactions than in nonanaphylactic ones both in children and adults (p = 0.01 and p = 0.006, respectively). Oral or parenteral steroids, oxygen, and H2 blockers were administered more commonly in adults than in children (p < 0.02, p < 0.001, and p < 0.001, respectively). Only half of both children and adults were treated with epinephrine; more commonly in reactions coded as anaphylaxis than as nonanaphylaxis (p < 0.001 and p < 0.01, respectively) (Table 2).
Adults were Hospitalized More Often and Required Multiple Doses of Epinephrine When Compared to Children
Overall, a higher proportion of adults required hospitalization (15.3 versus 9.7% in children) and ICU admission (11.8 versus 4% in children) (Table 1) when compared with children (p = 0.014). In contrast, children were discharged home from the ED more commonly than adults. The mean length of stay for hospitalization in children was 1.3 days (range, 1–4 days) and 2.6 days (range, 1–15 days) for adults. In this study, there were no reported fatalities related to anaphylaxis. Epinephrine was administered before presentation to the ED more often in children than in adults (82 versus 73%). Children who received epinephrine before arrival to the ED were more likely to be discharged home (p = 0.05) when compared with adults. Those adults who received epinephrine in the ED were admitted to the floors more often when compared with those who received epinephrine before arriving at the ED (28 versus 10%, p = 0.05) (Supplemental Table 2).
Risk Factors for Hospitalization
In multivariate logistic regression analysis, we assessed the predictors of hospitalization or ICU admission, including type of insurance, symptoms, sex, comorbidities (diabetes, chronic obstructive pulmonary disease). In children, anaphylaxis severity of 2 (odds ratio [OR] 1.17 [95% confidence interval [CI], 0.32–4.17], p = 0.042), a severity of 3 (OR 41.86 [95% CI, 2.90–602.48], p = 0.006), and received multiple doses of epinephrine (OR 15.36 [95% CI, 1.90–121.4[, p = 0.009) were associated with hospitalization. In adults, an anaphylaxis severity of 3 (OR 32.53 [95% CI, 6.28–168.35], p < 0.001) and having received multiple doses of epinephrine (OR 11.49 [95% CI, 3.08–44.13], p < 0.001) were associated with hospitalization (Table 3).
Table 3.
Logistic regression predicting combined floor and ICU admission by patient cohort
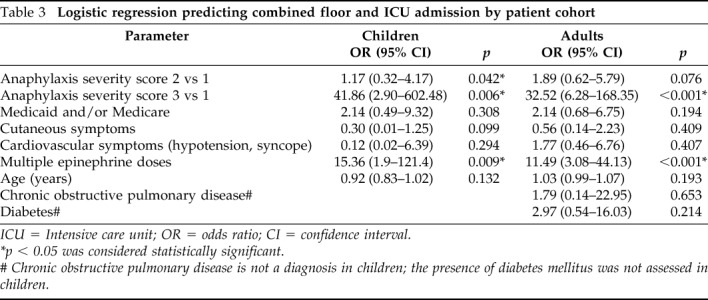
ICU = Intensive care unit; OR = odds ratio; CI = confidence interval.
*p < 0.05 was considered statistically significant.
# Chronic obstructive pulmonary disease is not a diagnosis in children; the presence of diabetes mellitus was not assessed in children.
Interestingly, when the data on the children and the adults were combined, which increased the power of the analysis, the factors associated with an increased chance of floor admission were anaphylaxis severity of 3 (OR 15.13 [95% CI, 3.92–58.42], p < 0.001), and multiple doses of epinephrine (OR, 6.83 [95% CI 2.13–22.08], p = 0.001). Factors associated with ICU admission were an anaphylaxis severity score of 3 (OR 29.39 [95% CI, 4.61–187.34], p < 0.001), Medicare and/or Medicaid insurance (OR 4.96 [95% CI, 1.14–21.67], p = 0.033), cutaneous symptoms (OR 0.19 [95% CI, 0.04–0.79], p = 0.023), cardiovascular symptoms (OR 5.8 [95% CI, 1.16–28.87], p = 0.032), and multiple doses of epinephrine (OR 37.12 [95% CI, 8.01–170.69], p < 0.001) (Supplemental Table 3).
DISCUSSION
Our study assessed the access to care and risk factors for hospitalization by comparing pediatric and adult populations in an upstate New York ED that serves urban, suburban, and rural populations. We confirmed the innate complexity involved in an anaphylaxis diagnosis and management across all age groups. We found that adults were admitted to the ICU more frequently than children and that patient characteristics associated with ICU admission included cardiovascular or cutaneous symptoms at presentation, Medicare and/or Medicaid insurance, and having received multiple doses of epinephrine when data for adults and children were combined.
The finding that adult age was associated with higher rates for hospitalization and ICU admission was consistent with other population-based studies that showed increased rates of hospitalization for anaphylaxis associated with increased age, including all age groups from childhood to adulthood.14–16 This may be related to our finding that the severity of presentation of anaphylaxis differed between children and adults. Adults tended to have more cardiovascular symptoms, such as hypotension and difficulty breathing, whereas children were more likely to have gastrointestinal symptoms, such as emesis and abdominal pain, in part, consistent with previous reports.17–20 Additional factors may be related to higher rates of hospitalization in adults. In a recent study, Motosue et al.16 investigated risk factors for severe anaphylaxis, defined as events that required hospitalization, admission to the ICU, endotracheal intubation, or meeting criteria for near-fatal anaphylaxis. They found that, in addition to age ≥65 years, medication-induced anaphylaxis and the presence of cardiac and/or lung disease were associated with increased odds of severe anaphylaxis.
Approximately 40% of the children and adults were treated with antihistamines and/or steroids without administration of epinephrine, despite a lack of evidence that demonstrated efficacy of these treatment modalities when used alone in anaphylactic reactions.19 Despite the presentation of anaphylaxis and that hospitalization rates were higher in adults, we found similar rates of treatment with epinephrine in adults (47%) and children (51%), similar to those previously reported (32–44% in adults ages ≥ 50 years18 and 41–79% in children13,21). This raises the question of whether epinephrine was relatively underutilized in adults and whether more frequent use of epinephrine might have prevented increased rates of hospitalization in that age group.
There have been conflicting reports as to whether early administration of epinephrine was associated with lower rates of hospitalization.13,21–23 We found that, among adults, those who received epinephrine before arrival to the ED were less likely to be admitted to the hospital floor and that even one dose of epinephrine in the ED was associated with a higher likelihood of hospitalization. Interestingly, epinephrine administration before arrival to the ED was associated with a greater likelihood of discharge to home, more often in children than in adults, even in those who received two doses of epinephrine before arrival to the ED. Therefore, prompt treatment with epinephrine before coming to the ED is associated with a decreased rate of hospitalization. This calls for the need for a more accurate diagnosis of anaphylaxis to the increase rates of administration with epinephrine, which can lead to decreased rates for hospitalization, although contradictory findings have been reported for foods.24 Also, our study revealed that all the patients who received more than two doses of epinephrine were hospitalized, most of them to the ICU, which likely reflected the severity of the reaction.
Another concern was repeated ED visits and hospitalization rates from food allergy. We found foods associated with multiple ED visits, consistent with a previous study in children.13 Almost half of the visits resulted in hospitalization, which may be due to the lower threshold for admission given a known history of anaphylaxis and history of previous visits. Five patients received epinephrine at discharge, but only two were referred to an allergist, which was consistent with previous studies that showed that referral and follow-up is inadequate.11,25 It is recommended that patients who experienced anaphylaxis should be referred to an allergist.26
Limitations of this study included those inherent in a retrospective medical record review, including reliance on data extractable from electronic health records and the possibility that data could be incomplete or inaccurate. Also, we used a relatively small number of patients from a single upstate New York ED. Strengths of this study included the ability to compare pediatric and adult populations seen in a single ED, which is not done in most studies. In the future, a large, multicenter, prospective study would help to address some of these limitations.
CONCLUSION
Anaphylaxis still remains greatly unrecognized and misdiagnosed. We identified that Medicare and/or Medicaid insurance, cardiovascular or cutaneous symptoms, and patients treated with multiple doses of epinephrine had increased odds of an ICU admission when data for adults and children were combined. Adults had a more severe presentation of anaphylaxis to the ED and more comorbid conditions, and were hospitalized more frequently when compared with children. This may reflect health-care disparities and the need for improved management of comorbid conditions in populations at risk for anaphylaxis. Emergency preparedness, including an anaphylaxis action plan, education, and identification are of vital importance.27 In the future, early recognition and efficient treatment in this vulnerable patient population may result in fewer ICU admissions, less overall cost, and improved care.
ACKNOWLEDGMENTS
We thank Keith Sweeney, M.S., and Michael Lavelle, M.S., for their contributions to data collection.
Footnotes
K.M. Järvinen was supported in part by grant AI091655 from the National Institute of Allergy and Infectious Diseases. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Allergy and Infectious Diseases or the National Institutes of Health
Presented as an abstract at the American Academy of Allergy, Asthma and Immunology annual meeting, March 2014, San Diego, California
No external funding sources reported
The authors have no conflicts of interest to declare pertaining to this article
Supplemental data available at www.IngentaConnect.com
REFERENCES
- 1. Lieberman P, Camargo CA, Jr, Bohlke K, et al. Epidemiology of anaphylaxis: findings of the American College of Allergy. Asthma and Immunology Epidemiology of Anaphylaxis Working Group. Ann Allergy Asthma Immunol. 2006; 97:596–602. [DOI] [PubMed] [Google Scholar]
- 2. Clark S, Camargo CA., Jr Epidemiology of anaphylaxis. Immunol Allergy Clin North Am. 2007; 27:145–63, v. [DOI] [PubMed] [Google Scholar]
- 3. Decker WW, Campbell RL, Manivannan V, et al. The etiology and incidence of anaphylaxis in Rochester, Minnesota: a report from the Rochester Epidemiology Project. J Allergy Clin Immunol. 2008; 122:1161–1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lee S, Hess EP, Lohse C, Gilani W, Chamberlain AM, Campbell RL. Trends, characteristics, and incidence of anaphylaxis in 2001–2010: A population-based study. J Allergy Clin Immunol. 2017; 139:182–188.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Motosue MS, Bellolio MF, Van Houten HK, Shah ND, Campbell RL. Increasing emergency department visits for anaphylaxis, 2005–2014. J Allergy Clin Immunol Pract. 2017; 5:171–175.e3. [DOI] [PubMed] [Google Scholar]
- 6. Simons FE. Anaphylaxis. J Allergy Clin Immunol. 2010; 125:S161–S181. [DOI] [PubMed] [Google Scholar]
- 7. Wood RA, Camargo CA, Jr, Lieberman P, et al. Anaphylaxis in America: the prevalence and characteristics of anaphylaxis in the United States. J Allergy Clin Immunol. 2014; 133:461–467. [DOI] [PubMed] [Google Scholar]
- 8. Simons FE, Ardusso LR, Bilo MB, et al. World Allergy Organization anaphylaxis guidelines: summary. J Allergy Clin Immunol. 2011; 127:587–593.e1–22. [DOI] [PubMed] [Google Scholar]
- 9. Koplin JJ, Martin PE, Allen KJ. An update on epidemiology of anaphylaxis in children and adults. Curr Opin Allergy Clin Immunol. 2011; 11:492–496. [DOI] [PubMed] [Google Scholar]
- 10. Banerji A, Rudders S, Clark S, Wei W, Long AA, Camargo CA., Jr Retrospective study of drug-induced anaphylaxis treated in the emergency department or hospital: patient characteristics, management, and 1-year follow-up. J Allergy Clin Immunol Pract. 2014; 2:46–51. [DOI] [PubMed] [Google Scholar]
- 11. World Health Organization. International Classification of Diseases-9-CM, 2017. Available from http://www.who.int/classifications/icd/en/.
- 12. Sampson HA, Munoz-Furlong A, Campbell RL, et al. Second symposium on the definition and management of anaphylaxis: summary report–second National Institute of Allergy and Infectious Disease/Food Allergy and Anaphylaxis Network symposium. Ann Emerg Med. 2006; 47:373–380. [DOI] [PubMed] [Google Scholar]
- 13. Huang F, Chawla K, Jarvinen KM, Nowak-Wegrzyn A. Anaphylaxis in a New York City pediatric emergency department: triggers, treatments, and outcomes. J Allergy Clin Immunol. 2012; 129:162–168.e1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Mulla ZD, Simon MR. Hospitalizations for anaphylaxis in Florida: epidemiologic analysis of a population-based dataset. Int Arch Allergy Immunol. 2007; 144:128–136. [DOI] [PubMed] [Google Scholar]
- 15. Sheikh A, Alves B. Age, sex, geographical and socio-economic variations in admissions for anaphylaxis: analysis of four years of English hospital data. Clin Exp Allergy. 2001; 31:1571–1576. [DOI] [PubMed] [Google Scholar]
- 16. Motosue MS, Bellolio MF, Van Houten HK, Shah ND, Campbell RL. Risk factors for severe anaphylaxis in the United States. Ann Allergy Asthma Immunol. 2017; 119:356–361.e2. [DOI] [PubMed] [Google Scholar]
- 17. Clark S, Wei W, Rudders SA, Camargo CA., Jr Risk factors for severe anaphylaxis in patients receiving anaphylaxis treatment in US emergency departments and hospitals. J Allergy Clin Immunol. 2014; 134:1125–1130. [DOI] [PubMed] [Google Scholar]
- 18. Campbell RL, Hagan JB, Li JT, et al. Anaphylaxis in emergency department patients 50 or 65 years or older. Ann Allergy Asthma Immunol. 2011; 106:401–406. [DOI] [PubMed] [Google Scholar]
- 19. Rolla G, Mietta S, Raie A, et al. Incidence of food anaphylaxis in Piemonte region (Italy): data from registry of Center for Severe Allergic Reactions. Intern Emerg Med. 2013; 8:615–620. [DOI] [PubMed] [Google Scholar]
- 20. Nowak RM, Macias CG. Anaphylaxis on the other front line: perspectives from the emergency department. Am J Med. 2014; 127(Suppl):S34–S44. [DOI] [PubMed] [Google Scholar]
- 21. Tiyyagura GK, Arnold L, Cone DC, Langhan M. Pediatric anaphylaxis management in the prehospital setting. Prehosp Emerg Care. 2014; 18:46–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Banerji A, Rudders SA, Corel B, Garth AM, Clark S, Camargo CA., Jr Repeat epinephrine treatments for food-related allergic reactions that present to the emergency department. Allergy Asthma Proc. 2010; 31:308–316. [DOI] [PubMed] [Google Scholar]
- 23. Fleming JT, Clark S, Camargo CA, Jr, Rudders SA. Early treatment of food-induced anaphylaxis with epinephrine is associated with a lower risk of hospitalization. J Allergy Clin Immunol Pract. 2015; 3:57–62. [DOI] [PubMed] [Google Scholar]
- 24. Banerji A, Rudders SA, Corel B, Garth AP, Clark S, Camargo CA., Jr Predictors of hospital admission for food-related allergic reactions that present to the emergency department. Ann Allergy Asthma Immunol. 2011; 106:42–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Poulos LM, Waters AM, Correll PK, Loblay RH, Marks GB. Trends in hospitalizations for anaphylaxis, angioedema, and urticaria in Australia, 1993–1994 to 2004–2005. J Allergy Clin Immunol. 2007; 120:878–884. [DOI] [PubMed] [Google Scholar]
- 26. Yocum MW, Butterfield JH, Klein JS, Volcheck GW, Schroeder DR, Silverstein MD. Epidemiology of anaphylaxis in Olmsted County: A population-based study. J Allergy Clin Immunol. 1999; 104:452–456. [DOI] [PubMed] [Google Scholar]
- 27. Simons FE. Anaphylaxis: recent advances in assessment and treatment. J Allergy Clin Immunol. 2009; 124:625–636; quiz 637–638. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


