Abstract
On account of its proven clinical efficacy, the combination of systemically administered amoxicillin and metronidazole is frequently adjuncted to non-operative periodontal therapy and well documented. Potential drawbacks of this regimen, e.g., side effects and problems with the compliance, led to an ongoing search for alternatives. Azithromycin, an antibiotic extensively used in general medicine, has recently found its niche in periodontal therapy as well. This systematic review aimed to analyze the in vitro antimicrobial efficacy of amoxicillin plus metronidazole versus azithromycin. For this purpose, a systematic literature search was performed, and studies published up to 29 March 2018 referenced in Medline, Embase, Cochrane, and Biosis were independently screened by two authors. An additional hand search was performed and studies focusing on the evaluation of in vitro antimicrobial efficacy of amoxicillin + metronidazole or azithromycin on bacteria from the subgingival biofilm were included. English and German language research reports were considered. From 71 identified articles, only three articles were eligible for inclusion. These studies showed heterogeneity in terms of analytical methods and strains explored. However, all studies used multispecies biofilm models for analysis of the antimicrobial activity. Unanimously, studies reported on more pronounced antimicrobial effects when applying the combination of amoxicillin + metronidazole, compared to azithromycin. Based on the few studies available, the combination of amoxicillin + metronidazole seemed to display higher antimicrobial efficacy in vitro than azithromycin.
Keywords: systematic review, azithromycin, macrolide, amoxicillin, metronidazole, antimicrobial, in vitro
1. Introduction
Periodontitis is a highly prevalent infectious disease leading to an inflammatory host response, destruction of tooth supporting tissues, and finally tooth loss if left untreated [1]. In this context, oral bacteria colonize the tooth surfaces in the form of complex biofilms. Failure to control or eliminate pathogenic biofilms by means of adequate individual and/or professional oral hygiene measures, leads to bacterial shifts and dysbiosis. Clinically, the transition from gingivitis to periodontitis may occur [2]. Given this microbial etiology, the application of systemic antibiotics as an adjunctive therapy to mechanical biofilm management has been explored for various disease entities [3].
The clinical efficacy of the combination of amoxicillin (AMX) and metronidazole (MTZ), adjuncted to mechanical treatment, has been extensively studied and is well documented [4]. So far, distinct antibiotic medication superiority over AMX + MTZ in combination has not been shown, neither in vivo nor in vitro studies [5]. However, some clinical drawbacks, such as adverse side-effects, difficulties in maintaining patient compliance, the high dose prescribed, and duration of therapy/intake of drugs or alcohol incompatibility have shown to complicate or limit the outcome with these drugs [3].
Lately, the macrolide antibiotic azithromycin (AZM) has been proposed as a possible alternative [6]. This antibiotic is interesting for periodontal therapy due to several potential benefits, including a broad antimicrobial spectrum, anti-inflammatory activity, a lower intake dosage and duration/frequency of intake [2]. Unfortunately, comparative data on a direct clinical comparison between AZM and the combination of AMX + MTZ are still scarce and ongoing. However, a recent systematic review found clear evidence for AZM as a second choice alternative to the combination of AMX + MTZ in chronic periodontitis patients [6].
The clinical application of drugs needs to be supported by the evidence from in vitro analyses, which corroborate the adequate antimicrobial spectrum. However, comparative laboratory data from in vitro antimicrobial testing of AZM and AMX + MTZ have not been systematically assessed yet. Therefore, this systematic review aimed to evaluate the in vitro antimicrobial efficacy of AMX + MTZ versus AZM. We hypothesized that both antibiotic therapies were equally effective in eliminating in vitro, the growth of bacteria associated with periodontal disease.
2. Materials and Methods
This study matched the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines for systematic reviews [7]. The focused question was adjusted according to the PICO (Population, Intervention, Comparator, Outcome) criteria for comparing laboratory studies as follows [8]:
“What is the in vitro antimicrobial efficacy of amoxicillin + metronidazole compared to azithromycin when targeting periopathogenic bacteria?”
2.1. Search Strategy
A literature search was performed using the U.S. National Library of Medicine (Medline), Excerpta Medical Database (Embase), Biosis Previews Database, and the Cochrane Central Library. Articles were included up to and including 29 March 2018.
The following terms were explored: (azithromycin) OR (zithromax) AND (metronidazole AND amoxicillin) OR (“van winkelhoff”) AND (periodontitis) OR (periodontal) including the according MeSH terms respectively.
2.2. Study Selection
Two reviewers (MK, PL) independently screened titles and abstracts found in the electronic search and assessed them in a first step to possibly include them into the review. All potentially eligible studies were ordered and their full texts were assessed. Studies were included if published in English or in German. Disagreement between the reviewers was resolved by discussion.
2.3. Eligibility Criteria for Studies
Only in vitro studies were considered.
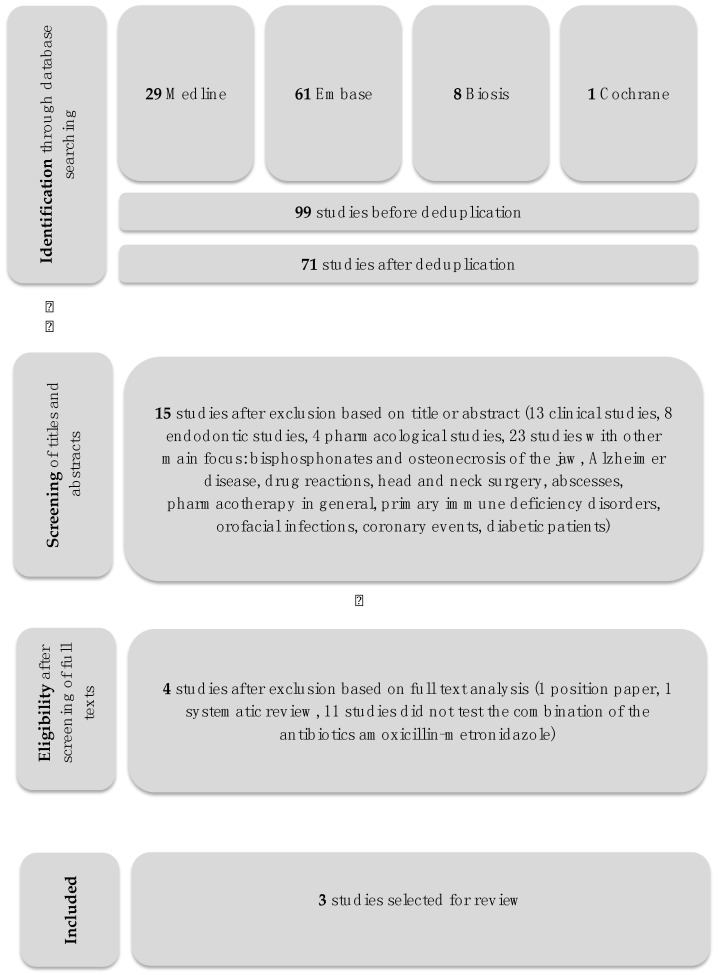
Figure 1 represents a PRISMA flowchart of the selection process of the included studies.
Figure 1.
Study selection flowchart.
2.4. Data Extraction
Excluded articles were classified hierarchically and explanations for exclusion were provided individually.
3. Results
3.1. Search and Screening
From 71 titles identified through the electronic search, sixty-seven articles were excluded (Figure 1, Table 1). The main reasons for exclusions were: In-vitro studies not testing the desired antibiotic regimen (12 studies), other study designs (total 23 studies: 2× surveys, 1× narrative review, 2× focus on head and neck infections, 3× testing of only one specific antibiotic, 1× evaluation of an odontogenic infection, 1× focus on HSV-1 and Alzheimer disease, 1× abscesses, 1× HIV, 1× vaccines and PDT, 1× critical review on antimicrobial treatments in general, 1× coronary events, 1× orofacial infections, 2× osteonecrosis of the jaw and bisphosphonates, 2× antibiotic resistance in general, 1× diabetic patients, 1× review on antibiotic prophylaxis, 1× immunology in general) or other topics within the dental field (20 clinical, 8 endodontic and 5 pharmacological, respectively). The inter-rater agreement was 100%.
Table 1.
Excluded studies. The reason for exclusion was arranged in categories pharma (for pharmacological studies), endo (for endodontic studies), other (for studies not addressing the research question), in-vitro (for in-vitro studies) or clin (for clinical studies).
| Reference | Category | Exclusion Criteria | |
|---|---|---|---|
| 1) | 2004 Position paper [10] | pharma | description of systemic antibiotics in periodontics in general, not specifically in vitro |
| 2) | 2017 Alattas et al. [11] | endo | reporting about prescription of antibiotics usus in southern Saudi Arabia focusing endodontic pathology |
| 3) | 2016 Barbosa-Ribeiro et al. [12] | endo | focusing antimicrobial susceptibility after failure of endodontic treatment |
| 4) | 2013 Bartold et al. [13] | other | focusing only AZM |
| 5) | 2014 Belibasakis & Thurnheer [14] | in-vitro | |
| 6) | 2013 Brook [15] | other | focus on head and neck infections in general rather than periodontal aspects |
| 7) | 2015 Brook [16] | other | focus on head and neck infections in general rather than periodontal aspects |
| 8) | 2000 Carrasco et al. [17] | in-vitro | the combination of the antibiotics AMX-MTZ wasn’t tested |
| 9) | 2015 Chopra et al. [18] | other | focus on cutaneous adverse drug reactions |
| 10) | 1995 Coulaud [19] | other | focusing only AZM |
| 11) | 2016 Dakic et al. [20] | clin | clinical study, AZM wasn’t tested, systematic review and meta-analysis |
| 12) | 2015 Ercan et al. [21] | clin | clinical study, patients with chronic periodontitis |
| 13) | 2001 Feik et al. [22] | in-vitro | the combination of the antibiotics AMX-MTZ wasn’t tested |
| 14) | 1997 Fresnadillo et al. [23] | clin | clinical study |
| 15) | 2014 Garg et al. [24] | other | survey |
| 16) | 2004 Greenstein et al. [25] | clin | clinical study |
| 17) | 2015 Harris et al. [26] | other | focus on HSV-1 and Alzheimer disease |
| 18) | 2003 Hernandez-rizzo [9] | in-vitro | full text wasn’t available until data |
| 19) | 2012 Herrera et al. [27] | clin | clinical study |
| 20) | 2008 Isla et al. [28] | other | focus on odontogenic infections in general rather than periodontitis |
| 21) | 2003 Jacinto et al. [29] | endo | focus on analysis of infected root canals |
| 22) | 2011 Japoni et al. [30] | in-vitro | the combination of the antibiotics AMX-MTZ wasn’t tested |
| 23) | 2005 Jaramillo et al. [31] | other | clin and in vitro, but focus on abscesses |
| 24) | 2016 Jentsch et al. [32] | clin | clinical study |
| 25) | 2015 Keestra et al. [33] | clin | clinical study, systematic review and meta-analysis |
| 26) | 2007 Kuriyama et al. [34] | in-vitro | the combination of the antibiotics AMX-MTZ wasn’t tested |
| 27) | 2013 Kuruvilla et al. [35] | other | focus on primary immune deficiency disorders |
| 28) | 2011 Leszczyńska et al. [36] | pharma | updated review, focus on periodontal pharmacotherapy in general |
| 29) | 2009 Liu et al. [37] | other | focus on vaccines and PDT |
| 30) | 1999 Loesche [38] | other | critical review, focus on antimicrobial treatment of periodontal disease |
| 31) | 2007 Maestre et al. [39] | in-vitro | the combination of the antibiotics AMX-MTZ wasn’t tested |
| 32) | 2012 Mahajan et al. [40] | endo | focus on management of endodontic infections |
| 33) | 2007 Mattina [41] | other | focus on Clarithromycin |
| 34) | 2018 McGowan et al. [42] | clin | clinical study, AZM wasn’t tested, systematic review and meta-analysis of RCTs |
| 35) | 2011 Mouratidou et al. [43] | in-vitro | the combination of the antibiotics AMX-MTZ wasn’t tested |
| 36) | 2013 Muniz et al. [44] | other | focusing only AZM |
| 37) | 2003 Murillo [45] | clin | focus on orofacial infections |
| 38) | 2017 Ong et al. [46] | in-vitro | |
| 39) | 2007 Paju et al. [47] | other | focus on coronary events |
| 40) | 2017 Palappallil et al. [48] | pharma | focus on adverse drug reactions |
| 41) | 2016 Papathanasiou et al. [49] | other | a survey of periodontists in the US |
| 42) | 2015 Parenti et al. [50] | other | narrative review with focus on endothelial dysfunction |
| 43) | 2011 Parnham [51] | other | focus on immunology in general |
| 44) | 2014 Rams et al. [52] | in-vitro | the combination of the antibiotics AMX-MTZ wasn’t tested |
| 45) | 2012 Ramu et al. [53] | other | practice review on antibiotic prophylaxis |
| 46) | 2015 Ranganathan et al. [54] | clin | clinical study |
| 47) | 2003 Rolim De Sousa et al. [55] | endo | bacteriological study of root canals associated with periapical abscesses |
| 48) | 2005 Ryan [56] | clin | clinical study |
| 49) | 2016 Saleh et al. [57] | clin | clinical study, patients with chronic periodontitis |
| 50) | 2015 Santos et al. [58] | other | focus on diabetic patients, systematic review |
| 51) | 2010 Segura-Egea et al. [59] | endo | focus on management of endodontic infections amongst Spanish oral surgeons |
| 51) | 2009 Serrano et al. [60] | other | focus on antibiotic resistance of periodontal pathogens |
| 52) | 2012 Sgolastra et al. [61] | clin | clinical study, AZM wasn’t tested, systematic review and meta-analysis |
| 53) | 2011 Shannon et al. [62] | other | focus on Bisphosphonates and osteonecrosis of the jaw |
| 54) | 2017 Shivi et al. [63] | clin | clinical study |
| 55) | 2013 Siqueira et al. [64] | other | focus on abscesses |
| 56) | 2015 Soares et al. [65] | in-vitro | |
| 57) | 2011 Somma et al. [66] | endo | focus on endo and general health |
| 58) | 2013 Sousa et al. [67] | endo | focus on antimicrobial susceptibility pattern of infected root canals |
| 59) | 2018 Souto et al. [68] | clin | clinical study, focus on diabetic subjects, systematic review and meta-analysis |
| 60) | 2004 Sweeny et al. [69] | other | focus on antibiotic resistance in the dental practice |
| 61) | 2001 Tarullo et al. [70] | clin | focus on Helicobacter pylori |
| 62) | 2014 Teughels et al. [71] | clin | clinical study, patients with aggressive periodontitis |
| 63) | 2007 Tomas et al. [72] | in-vitro | the combination of the antibiotics AMX-MTZ wasn’t tested |
| 64) | 2007 Van Den Wyngaert et al. [73] | other | focus on osteonecrosis of the jaw and bisphosphonates |
| 65a),65b) | 1999, 2000 van Winkelhoff et al. [74,75] | in-vitro | the combination of the antibiotics AMX-MTZ wasn’t tested |
| 66) | 2005 van Winkelhoff et al. [76] | in-vitro | the combination of the antibiotics AMX-MTZ wasn’t tested |
| 67) | 2012 Veloo et al. [77] | in-vitro | the combination of the antibiotics AMX-MTZ wasn’t tested |
| 68) | 2005 Voils et al. [78] | clin | clinical study |
| 69) | 2013 Zandbergen et al. [79] | clin | clinical study, AZM wasn’t tested, systematic review |
| 70) | 2016 Zhang et al. [80] | clin | clinical study, the combination of the antibiotics AMX-MTZ wasn’t tested, meta-analysis of RCTs |
Although one of the screened study met all inclusion criteria [9], the full text was not available despite contacting the respective authors and libraries. Therefore, the study had to be excluded. The remaining three full articles were again separately and independently assessed by both reviewers. Finally, three publications were included in the systematic analysis.
3.2. Experimental Methods in the Evaluated Studies
The in vitro experiments in this review were assessed for methodological heterogeneity. The experiments are briefly described below.
Belibasakis & Thurnheer [14] employed an in vitro subgingival biofilm model with 10 species [81]. After culturing the bacteria for 40.5 h, the biofilms were exposed to the following antibiotics for another 24 h at concentrations detected in the pocket environment following systematic administration (15 mg/L MTZ, 15 mg/L AMX, a combination of 15 mg/L MTZ + 15 mg/L AMX, 2 mg/L doxycycline and 10 mg/L AZM). Bacterial counts and final concentrations of the antibiotics in the culture media were then measured. Three independent experiments were performed for control as well.
Ong and co-workers [46] evaluated the efficacy of AZM on mono- and polymicrobial biofilm formations consisting of P. gingivalis, T. denticola, and T. forsythia in comparison to AMX + MTZ in combination in vitro. The antibiotics were dispersed using deionized water and final antibiotic concentrations in the range between 0.01–100 mg/L were tested in the respective supernatants of the microbial cultures. Monitoring the growth for 48 h, they measured absorbance at a wavelength of 620 nm (AU620) using a microplate reader. The minimum inhibitory concentration (MIC) and the minimal biofilm inhibitory concentration (MBIC) for the antibiotics were calculated.
Soares et al. [65] tested the antimicrobial effects of AZM and the combination of AMX + MTZ on a polymicrobial biofilm model with 35 subgingival bacterial species, including S. oralis, F. nucleatum, P. gingivalis, P. intermedia, A. actinomycetemcomitans, and T. forsythia. A 2,3,5-triphenyltetrazolium chloride (TTC) was used in this study to discern metabolically active and inactive cells. The white substrate was enzymatically reduced to red 1,3,4-triphenylformazan (TFP) by living bacterial cells, as a result of dehydrogenase activity. By reading changing substrate color through fluorescence spectrophotometry, the reduction rate was registered. To measure the undergoing metamorphosis of the biofilms, the remaining pegs were rinsed in solution twice and moved onto 9 plates where the TTC conversion was taken at 485 nm. After the TTC assay, the pegs were washed, extracted from the cover and transferred to Eppendorf tubes (final solution). Using checkerboard DNA–DNA hybridization technique [82], the samples then were individually analyzed. The database from a previous study by the same group was examined to obtain reference values for the composition of in vivo biofilms. The consistency of the microbial profiles was tested across and between the nine in vitro biofilm samples, and the in vivo reference values by using a so-called minimum similarity coefficient. The total DNA probe count was calculated for each species in each in vitro biofilm sample, and for the mean reference values for in vivo biofilms. Once the minimum similarity value for each species in a pair of samples was calculated, the values were summed to give a summary measurement for the entire microbial community.
For each time point, the three negative-control optical density (OD) values were averaged and each assay result was divided by this number, which yielded the proportion of activity remaining in the presence of the antibiotic. This proportion was then subtracted from 1 and multiplied by 100 to derive the percent inhibition.
At chosen time points (12, 24, 36 h), four different concentrations of the antibiotics (1:1, 1:3, 1:9, 1:27) were tested. The 1:27 dilutions at the 36 h time point were considered to be the primary analysis, as this concentration was likely to be closest to that achieved in periodontal pockets when antibiotics are administered systemically. The analyses for the remaining dilutions and time points were considered exploratory.
3.3. Antimicrobial Results
AMX + MTZ reduced the biofilm 27% more than AZM [14]. The metabolic activity was reduced 84% through AMX + MTZ whereas only by 17% through AZM [65]. The MIC and MBIC of AMX + MTZ in combination was found to be almost 10-fold lower than the one of AZM [46].
Taken together, all of the studies reported on more pronounced antimicrobial effects (biofilm reduction, growth inhibition or reduction of metabolic activity) of AMX + MTZ compared to AZM in in vitro biofilm models.
Table 2 Comparison of the three studies selected in the review.
Table 2.
Comparison of the three studies.
| Reference | Tested Outcome Parameters | Antibiotic | Results | Difference (Δ parameter:AMX/MTZ - AZM) |
|---|---|---|---|---|
|
2014 Belibasakis and Thurnheer Validation of antibiotic efficacy on in vitro subgingival biofilms. [14] |
Log10 Reduction (TBC) Reduction of biofilm in % |
Azithromycin | 0.4 log 60% |
Δ 0.5 log Δ 27% |
| Amoxicillin/ Metronidazole |
0.9 log 87% |
|||
|
2017 Ong et al. Effect of azithromycin on a red complex polymicrobial biofilm. [46] |
MIC MBIC |
Azithromycin | MIC 1.52 mg/L MBIC 10.6 mg/L |
Δ MIC 1.35 mg/L Δ MBIC 9.3 mg/L |
| Amoxicillin/ Metronidazole |
MIC 0.17 mg/L MBIC 1.3 mg/L |
|||
|
2015 Soares et al. Effects of azithromycin, metronidazole, amoxicillin, and metronidazole plus amoxicillin on an in vitro polymicrobial subgingival biofilm model. Antimicrobial agents and chemotherapy. [65] |
Reduction of metabolic activity in % | Azithromycin | 17% | Δ 67% |
| Amoxicillin/ Metronidazole |
84% |
4. Discussion
The purpose of the present review was to evaluate the available literature for the in vitro antimicrobial efficacy of AZM, compared to the combination of AMX + MTZ. Based on the few studies available, the combination of AMX + MTZ was unequivocally shown to have a higher antimicrobial efficacy in vitro, compared to AZM.
Despite these results and within the main limitation of this review, namely a low number of underlying studies supporting this finding, antibiotics have a specific antimicrobial range of efficacy which has to be taken into account. The range of indications and the use of these antibiotics need to be matched with the suspected microbes, but should also be as broad as possible.
In vitro biofilm models have been proposed as a means to examine the higher tolerance to antimicrobials that this mode of growth confers to bacteria [83]. It has been argued that, due to greater tolerance to antimicrobials, that MICs calculated using bacterial cells grown planktonically would bear little relevance to in vivo situations [2]. The higher tolerance of biofilms to antimicrobials has also led periodontists to recommend that the use of these agents be accompanied or preceded by mechanical disruption of the subgingival biomass.
In medicine AZM is extensively used as medication for a widespread spectrum of infections [2]. It is an industrially processed analogue of erythromycin with a supplementary nitrogen atom in the macrocyclic lactone ring [84]. In AZM, structural stability is provided through the extra nitrogen atom. Compared with erythromycin, tissue penetration is optimized, toxicity is low, and half-life is almost three days [85]. As the course of administration is short along with the list of side effects as well, patient compliance is excellent [86]. In susceptible organisms, AZM reversibly hinders bacterial protein synthesis by addressing the 23S ribosomal RNA of the 50S ribosomal subunit [87]. Macrolides decrease bacterial adhesion, resulting in minified biofilm formation. This process is dose-dependent and occurs even at very low macrolide concentrations [88]. AZM has bacteriostatic effects against a wide spectrum of bacteria in vitro and is particularly effective against gram-negative anaerobic bacteria [89]. Gingival crevicular fluid (GCF) concentrations of AZM, following a 500 mg oral dose, have been shown to reach up to 7–8 mg/L. Levels of AZM in serum are 40-fold lower [24]. The authors attributed this to cells of peripheral tissues which accumulate AZM actively. Significant immunomodulatory effects of AZM have been observed. In vitro concentrations of AZM lower than MIC could significantly inhibit quorum-sensing signals and biofilm formation of P. aeruginosa [25]. Beneficially, AZM may possibly decrease proinflammatory cytokine production [90]. It must be noted that such mechanisms were not investigated in the included articles, which focused on antimicrobial actions only. Therefore, additional working actions may increase the efficacy of AZM, which has to be compared in a respective systematic evaluation of clinical studies. This is another shortcoming of this study—if interpreted as a singular antimicrobial evaluation, as it ignores additional modes of action as mentioned above.
AMX is a bacteriolytical lactame-antibiotic with a wide spectrum and a half-life of 1 to 1.5 h. MTZ is, as a nitroimidazole, especially effective against anaerobes and protozoa with a half-life of 6 to 7 h. The simultaneous administration of these two medications has gained increased significance over the last two decades. Both active substances in combination cover most of the aerobic and anaerobic bacteria. Furthermore, they overlap in their effect on facultative bacteria. The combination of MTZ + AMX has gained recognition mostly due to its efficacy against A. actinomycetemcomitans, a periodontal pathogen closely associated with the etiology of rapid periodontitis progression [91]. A possible explanation for the synergistic effects of MTZ + AMX may be increased uptake of MTZ in the presence of AMX, as has been described for A. actinomycetemcomitans in Reference [28]. AMX + MTZ have been prescribed for more than three decades; their effects and side-effects are well documented. The most common adverse reactions to AMX are allergic, often mild forms, limited exanthema on the head and neck. Heavy reactions may cause swelling of joints. Anaphylactic reactions are possible with highly sensitive patients. Possible side-effects of MTZ are nausea, headache, lack of appetite, diarrhea or metallic taste, seldom rashes [4]. Additionally, this combi-cocktail requires increased patient-compliance with the intake of two tablets, three times daily, over a period of seven days [6]. In case of penicillin allergy, the combination of MTZ (500 mg) and Ciprofloxacin (250 mg) twice daily is recommended [92].
For a number of putative periodontal pathogens, the MIC is shown to be below the antibiotic concentrations achievable in GCF [93]. The concentration in the GCF rises three days after administration of 500 mg AMX at 14 g/mL [94], and two days after administration of 500 mg MTZ at 13 g/mL [95]. Administration of 500 mg AZM, followed by 250 mg, results in 7.5 g/mL after two days and 2.5 g/mL after fifteen days [96]. “The antibiotic concentration in GCF should be considerably higher than the MICs indicated by their in vitro efficacy to be effective within the environment” [34].
At a concentration of 15 mg/L, Reference [14] reported that total cell numbers were reduced through AMX + MTZ in combination, and significantly reduced P. gingivalis numbers, whereas AZM, at a concentration of 10 mg/L, reduced total cell numbers at less than 0.5 log. However, the clinical efficacy might be underestimated as in vivo the microbial load of P. gingivalis might be markedly lower compared to those reported in the three studies.
Soares et al. [65] stated that they were able to consistently recover 35 of the initial 40 bacteria used in their biofilm model. The missing bacteria, especially Gram-negative Prevotella species, might explain the increased tolerance of the in vitro biofilm to MTZ, which specifically targets strict anaerobic Gram-negative bacteria. Furthermore, Treponema species were also excluded from the in vitro model, due to difficulties in growing these strict anaerobes. Despite this, biofilm models provide a more relevant test scenario for testing the efficacy of antibiotics as opposed to bacterial cultures in a planktonic state, for which the MICs are purportedly lower.
By using only three bacterial species as in the study by Ong [46], the complexity of the polymicrobial biofilms accomplished with subgingival plaque might not have been completely represented. Still, these three species close to the gingival epithelium, forming a bilateral bacterial neighborhood, are affiliated with disease severity and progression [88]. However, the Zurich biofilm model does not include host immune cells. These cells in the periodontal pocket environment could support the effect of antibiotics. Two of the studies used bacterial strains taken from the American Typing Collection (ATCC). The Zurich group [14] took bacterial strains from their own cultivation (OMZ: Institute for Oral Biology, Section for Oral Microbiology and General Immunology, University of Zurich, Zurich, Switzerland).
All authors of the three studies agreed that it was difficult to reconcile longitudinal studies with in vitro antimicrobial testing. The subgingival biofilm model used in the Soares study [65] might simulate the most realistic clinical situation yet. However, in general, in vitro oral multispecies biofilm models all suffer from one or more limitations and are comprised of only up to 5 or 10 species [89].
5. Conclusions
This review of the literature does not allow drawing definitive conclusions regarding the clinical efficacy of AMX + MTZ in combination versus AZM, due to the small number of studies available for inclusion and the very different test protocols. In addition, only antimicrobial assessment was performed, neglecting other potential action models. Whilst the combination of AMX + MTZ performed in 3 out of 3 studies better and seemed to have a higher antimicrobial efficacy in vitro as compared to AZM, further studies are required to evaluate the comparative laboratory susceptibility and the clinical relevance of AZM in particular.
Author Contributions
M.K. drafted the manuscript. P.L. and M.K. did the literature search. C.W. verified the analytical methods, discussed the results and contributed to the final manuscript. T.T. helped to supervise the methodological correctness of the compared in vitro studies. T.A. validated the manuscript. D.B.W. helped with the statistical evaluation of the papers and the tables and participated in its design. P.R.S. conceived the study and supervised the study and the literature search. All authors carefully read and approved the final text.
Funding
This research received no external funding
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Harris R.J. Untreated periodontal disease: A follow-up on 30 cases. J. Periodontol. 2003;74:672–678. doi: 10.1902/jop.2003.74.5.672. [DOI] [PubMed] [Google Scholar]
- 2.Meyle J., Chapple I. Molecular aspects of the pathogenesis of periodontitis. Periodontology 2000. 2015;69:7–17. doi: 10.1111/prd.12104. [DOI] [PubMed] [Google Scholar]
- 3.Slots J., Ting M. Systemic antibiotics in the treatment of periodontal disease. Periodontology 2000. 2002;28:106–176. doi: 10.1034/j.1600-0757.2002.280106.x. [DOI] [PubMed] [Google Scholar]
- 4.Mombelli A., Cionca N., Almaghlouth A. Does adjunctive antimicrobial therapy reduce the perceived need for periodontal surgery. Periodontology 2000. 2011;55:205–216. doi: 10.1111/j.1600-0757.2010.00356.x. [DOI] [PubMed] [Google Scholar]
- 5.Mombelli A. Microbial colonization of the periodontal pocket and its significance for periodontal therapy. Periodontology 2000. 2018;76:85–96. doi: 10.1111/prd.12147. [DOI] [PubMed] [Google Scholar]
- 6.Buset L.S., Zitzmann N.U., Weiger R., Walter C. Non-surgical periodontal therapy supplemented with systemically administered azithromycin: A systematic review of RCTs. Clin Oral Investig. 2015;19:1763–1775. doi: 10.1007/s00784-015-1499-z. [DOI] [PubMed] [Google Scholar]
- 7.Shamseer L., Moher D., Clarke M., Ghersi D., Liberati A., Petticrew M., Shekelle P., Stewart L.A., Prisma-p G. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015, 2015, elaboration and explanation. BMJ. 2015;350:G7647. doi: 10.1136/bmj.g7647. [DOI] [PubMed] [Google Scholar]
- 8.Forrest L.J., Miller S.A. Evidence-based decision making in action: Part 1—Finding the best clinical evidence. J. Contemp. Dent. Pract. 2002;3:10–26. [PubMed] [Google Scholar]
- 9.Hernández-rizzo G.A. Usefulness of antimicrobial agents in periodontal disease. Inf. Med. 2003;5:97–100. [Google Scholar]
- 10.Slots J. Position paper: Systemic antibiotics in periodontics. J. Periodontol. 2004;75:1553–1565. doi: 10.1902/jop.2004.75.11.1553. [DOI] [PubMed] [Google Scholar]
- 11.Alattas A.H., Alyami S.H. Prescription of antibiotics for pulpal and periapical pathology among dentists in southern Saudi Arabia. J. Glob. Antimicrob. Resist. 2017;9:82–84. doi: 10.1016/j.jgar.2017.01.012. [DOI] [PubMed] [Google Scholar]
- 12.Barbosa-ribeiro M., De-jesus-soares A., Zaia A.A., Ferraz C.C.R., Almeida J.F.A., Gomes B.P.F.A. Antimicrobial susceptibility and characterization of virulence genes of enterococcus faecalis isolates from teeth with failure of the endodontic treatment. J. Endod. 2016;42:1022–1028. doi: 10.1016/j.joen.2016.03.015. [DOI] [PubMed] [Google Scholar]
- 13.Bartold M.P., Bois A.H.D., Gannon S., Haynes D.R., Hirsch R.S. Antibacterial and immunomodulatory properties of azithromycin treatment implications for periodontitis. Inflammopharmacology. 2013;21:321–338. doi: 10.1007/s10787-012-0165-1. [DOI] [PubMed] [Google Scholar]
- 14.Belibasakis N.G., Thurnheer T. Validation of antibiotic efficacy on in vitro subgingival biofilms. J. Periodontol. 2014;85:343–348. doi: 10.1902/jop.2013.130167. [DOI] [PubMed] [Google Scholar]
- 15.Brook I. Fusobacterial infections in children. Curr. Infect. Dis. Rep. 2013;15:288–294. doi: 10.1007/s11908-013-0340-6. [DOI] [PubMed] [Google Scholar]
- 16.Brook I. Fusobacterial head and neck infections in children. Int. J. Pediatr. Otorhinolaryngol. 2015;79:953–958. doi: 10.1016/j.ijporl.2015.04.045. [DOI] [PubMed] [Google Scholar]
- 17.Carrasco E., Martinez M., Calbacho M., Wilckens M. In vitro activity of amoxicillin, tetracyclines, azithromycin, ofloxacin and metronidazole against porphyromonas gingivalis, prevotella intermedia and fusobacterium nucleatum strains. Anaerobe. 2000;5:443–445. doi: 10.1006/anae.1999.0270. [DOI] [Google Scholar]
- 18.Chopra D., Sharma V., Kapoor R., Dwivedi S. An observational study of cutaneous adverse drug reactions in a teaching hospital. Int. J. Clin. Pharm. 2015;37:996–999. doi: 10.1007/s11096-015-0161-9. [DOI] [PubMed] [Google Scholar]
- 19.Coulaud J.P. Azithromyin: New trends. Pathol. Boil. 1995;43:547–550. [PubMed] [Google Scholar]
- 20.Dakic A., Boillot A., Colliot C., Carra M.C., Czernichow S., Bouchard P. Detection of porphyromonas gingivalis and aggregatibacter actinomycetemcomitans after systemic administration of amoxicillin plus metronidazole as an adjunct to non-surgical periodontal therapy: A systematic review and meta-analysis. Front. Microbiol. 2016;7:1277. doi: 10.3389/fmicb.2016.01277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ercan E., Uzun B.C., Ustaoglu G. Effects of azithromycin versus metronidazole-amoxicillin combination as an adjunct to nonsurgical periodontal therapy of generalized aggressive periodontitis. Niger. J. Clin. Pract. 2015;18:506–510. doi: 10.4103/1119-3077.154221. [DOI] [PubMed] [Google Scholar]
- 22.Feik D., Mortensen J.E., Rhoads S.L., Egleton J., Rams T.E. Antibiotic susceptibility profile of periodontal streptococcus constellatus. Abstr. Gen. Meet. Am. Soc. Microbiol. 2001;101:3–4. [Google Scholar]
- 23.Martinez M.J.F., de castro A.M.B., Sanchez E.G., Sanchez J.E.G., Rodriguez J.A.G. The current state and perspectives on antibiotic treatment for odontogene infections. Rev. Espanola De Quimioter. 1997;10:203–211. [Google Scholar]
- 24.Garg K.A., Agrawal N., Tewari R.K., Kumar A., Chandra A. Antibiotic prescription pattern among indian oral healthcare providers: A cross-sectional survey. J. Antimicrob. Chemother. 2014;69:526–528. doi: 10.1093/jac/dkt351. [DOI] [PubMed] [Google Scholar]
- 25.Greenstein G. Efficacy of subantimicrobial-dose doxycycline in the treatment of periodontal diseases: A critical evaluation. Int. J. Periodontics Restor. Dent. 2004;24:528–543. [PubMed] [Google Scholar]
- 26.Harris A.S., Harris E.A. Herpes simplex virus type 1 and other pathogens are key causative factors in sporadic alzheimer’s disease. J. Alzheimer’s Dis. 2015;48:319–353. doi: 10.3233/JAD-142853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Herrera D., Matesanz P., Bascones-martinez A., Sanz M. Local and systemic antimicrobial therapy in periodontics. J. Evid.-Based Dent. Pract. 2012;12:50–60. doi: 10.1016/S1532-3382(12)70013-1. [DOI] [PubMed] [Google Scholar]
- 28.Isla A.A., Canut A., Rodriguez-gascon P., Planells P., Beltri-orta J.I., Salmeron-escobar A., Labora A., Pedraz J.L. Antibiotic therapy in odontogenic infections in children and adolescents: Pharmacokinetic/pharmacodynamic analysis. Enferm. Infecc. Microbiol. Clin. 2008;26:621–628. doi: 10.1016/S0213-005X(08)75278-9. [DOI] [PubMed] [Google Scholar]
- 29.Jacinto C.R., Gomes B.P.F.A., Ferraz C.C.R., Zaia A.A., Filho F.J.S. Microbiological analysis of infected root canals from symptomatic and asymptomatic teeth with periapical periodontitis and the antimicrobial susceptibility of some isolated anaerobic bacteria. Oral Microbiol. Immunol. 2003;18:285–292. doi: 10.1034/j.1399-302X.2003.00078.x. [DOI] [PubMed] [Google Scholar]
- 30.Japoni A., Vasin A., Noushadi S., Kiany F., Japoni S., Alborzi A. Antibacterial susceptibility patterns of porphyromonas gingivalis isolated from chronic periodontitis patients. Med. Oral Patol. Oral Cir. Bucal. 2011;16:e1031-5. doi: 10.4317/medoral.17174. [DOI] [PubMed] [Google Scholar]
- 31.Jaramillo A., Arce R.M., Herrera D., Betancourth M., Botero J.E., Contreras A. Clinical and microbiological characterization of periodontal abscesses. J. Clin. Periodontol. 2005;32:1213–1218. doi: 10.1111/j.1600-051X.2005.00839.x. [DOI] [PubMed] [Google Scholar]
- 32.Jentsch R.H.F., Buchmann A., Friedrich A., Eick S. Nonsurgical therapy of chronic periodontitis with adjunctive systemic azithromycin or amoxicillin/metronidazole. Clin. Oral Investig. 2016;20:1765–1773. doi: 10.1007/s00784-015-1683-1. [DOI] [PubMed] [Google Scholar]
- 33.Keestra J.J.A., Grosjean I., Coucke W., Quirynen M., Teughels W. Non-surgical periodontal therapy with systemic antibiotics in patients with untreated chronic periodontitis: A systematic review and meta-analysis. J. Periodontal Res. 2015;50:294–314. doi: 10.1111/jre.12221. [DOI] [PubMed] [Google Scholar]
- 34.Kuriyama T., Williams D.W., Yanagisawa M., Iwahara K., Shimizu C., Nakagawa K., Yamamoto E., Karasawa T. Antimicrobial susceptibility of 800 anaerobic isolates from patients with dentoalveolar infection to 13 oral antibiotics. Oral Microbiol. Immunol. 2007;22:285–288. doi: 10.1111/j.1399-302X.2007.00365.x. [DOI] [PubMed] [Google Scholar]
- 35.Kuruvilla M., de la morena M.T. Antibiotic prophylaxis in primary immune deficiency disorders. J. Allergy Clin. Immunol. Pract. 2013;1:573–582. doi: 10.1016/j.jaip.2013.09.013. [DOI] [PubMed] [Google Scholar]
- 36.Leszczyńska A., Buczko P., Buczko W., Pietruska M. Periodontal pharmacotherapy—An updated review. Adv. Med. Sci. 2011;56:123–131. doi: 10.2478/v10039-011-0044-9. [DOI] [PubMed] [Google Scholar]
- 37.Liu F.P., Zhu W.H., Huang C.M. Vaccines and photodynamic therapies for oral microbial-related diseases. Curr. Drug Metab. 2009;10:90–94. doi: 10.2174/138920009787048365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Loesche W.J. The antimicrobial treatment of periodontal disease: Changing the treatment paradigm. Crit. Rev. Oral Boil. Med. 1999;10:245–275. doi: 10.1177/10454411990100030101. [DOI] [PubMed] [Google Scholar]
- 39.Maestre R.J., Bascones A., Sanchez P., Matesanz P., Aguilar L., Gimenez M.J., Perez-balcabao I., Granizo J.J., Prieto J. Odontogenic bacteria in periodontal disease and resistance patterns to common antibiotics used as treatment and prophylaxis in odontology in Spain. Rev. Esp. Quimioter. Publ. De La Soc. Esp. De Quimioter. 2007;20:61–67. [PubMed] [Google Scholar]
- 40.Mahajan A., Sharma V., Vats A., Srivastav A. Pattern of antibiotic prescription in the management of endodontic infections amongst oral and maxillofacial surgeons and endodontists in Gujarat. Indian J. Public Health Res. Dev. 2012;3:1–3. [Google Scholar]
- 41.Mattina R. Clarithromycin in dental infections. Trends Med. 2007;7:71–80. [Google Scholar]
- 42.Mcgowan K. Insufficient evidence to compare the efficacy of treatments for medication-related osteonecrosis of the jaws. J. Evid. Based Dent. Pract. 2018;18:70–72. doi: 10.1016/j.jebdp.2017.12.001. [DOI] [PubMed] [Google Scholar]
- 43.Mouratidou A., Karbach J., D’hoedt B., Al-nawas B. Antibiotic susceptibility of cocultures in polymicrobial infections such as peri-implantitis or periodontitis: An in vitro model. J. Periodontol. 2011;82:1360–1366. doi: 10.1902/jop.2011.100657. [DOI] [PubMed] [Google Scholar]
- 44.Muniz G.F.W.M., de oliveira C.C., Carvalho R.D., Moreira M.M.S.M., de moraes M.E.A., Martins R.S. Azithromycin: A new concept in adjuvant treatment of periodontitis. Eur. J. Pharmacol. 2013;705:135–139. doi: 10.1016/j.ejphar.2013.02.044. [DOI] [PubMed] [Google Scholar]
- 45.Murillo J. Treatment of bacterial orofacial infections. Med. Oral. 2003;8:154. [PubMed] [Google Scholar]
- 46.Ong S.H., Oettinger-barak O., Dashper S.G., Darby I.B., Tan K.H., Reynolds E.C. Effect of azithromycin on a red complex polymicrobial biofilm. J. Oral Microbiol. 2017;9:1339579. doi: 10.1080/20002297.2017.1339579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Paju S., Sinisalo J., Pussinen P.J., Valtonen V., Nieminen M.S. Is periodontal infection behind the failure of antibiotics to prevent coronary events? Atherosclerosis. 2007;193:193–195. doi: 10.1016/j.atherosclerosis.2006.06.015. [DOI] [PubMed] [Google Scholar]
- 48.Palappallil S.D., Ramnath S.N., Gangadhar R. Adverse drug reactions: Two years’ experience from a tertiary teaching hospital in Kerala. Natl. J. Physiol. Pharm. Pharmacol. 2017;7:403–411. doi: 10.5455/njppp.2017.7.1131212122016. [DOI] [Google Scholar]
- 49.Papathanasiou E., Finkelman M., Hanley J., Parashis A.O. Prevalence, etiology and treatment of peri-implant mucositis and peri-implantitis: A survey of periodontists in the United States. J. Periodontol. 2016;87:493–501. doi: 10.1902/jop.2015.150476. [DOI] [PubMed] [Google Scholar]
- 50.Parenti A., Paccosi S., Cairo F., Defraia E. Treatment of periodontitis for the prevention of endothelial dysfunction: A narrative review. Curr. Vasc. Pharmacol. 2015;13:749–758. doi: 10.2174/1570161113666150818110653. [DOI] [PubMed] [Google Scholar]
- 51.Parnham M.J. Immunomodulatory approaches to the treatment of infections. Infektol. Glas. 2011;31:15–27. [Google Scholar]
- 52.Rams E.T., Feik D., Mortensen J.E., Degener J.E., van winkelhoff A.J. Antibiotic susceptibility of periodontal streptococcus constellatus and streptococcus intermedius clinical isolates. J. Periodontol. 2014;85:1792–1798. doi: 10.1902/jop.2014.130291. [DOI] [PubMed] [Google Scholar]
- 53.Ramu C., Padmanabhan T.V. Indications of antibiotic prophylaxis in dental practice-review. Asian Pac. J. Trop. Biomed. 2012;2:749–754. doi: 10.1016/S2221-1691(12)60222-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ranganathan A.T., Gita B., Ramya V. Role of systemic antibiotics in the management of periodontal diseases. Biomed. Pharmacol. J. 2015;8SE:691–694. doi: 10.13005/bpj/769. [DOI] [Google Scholar]
- 55.De sousa E.L.R., Ferraz C.C.R., Gomes B.P.F.D., Pinheiro E.T., Teixeira F.B., de souza-filho F.J. Bacteriological study of root canals associated with periapical abscesses. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2003;96:332–339. doi: 10.1016/S1079-2104(03)00261-0. [DOI] [PubMed] [Google Scholar]
- 56.Ryan M.E. Nonsurgical approaches for the treatment of periodontal diseases. Dent. Clin. N. Am. 2005;49:611–636. doi: 10.1016/j.cden.2005.03.010. [DOI] [PubMed] [Google Scholar]
- 57.Saleh A., Rincon J., Tan A., Firth M. Comparison of adjunctive azithromycin and amoxicillin/metronidazole for patients with chronic periodontitis: Preliminary randomized control trial. Aust. Dent. J. 2016;61:469–481. doi: 10.1111/adj.12415. [DOI] [PubMed] [Google Scholar]
- 58.Santos L.C.M.M., Lira R., Fischer R.G., Santos A.P.P., Oliveira B.H. Systemic antibiotics in periodontal treatment of diabetic patients: A systematic review. PLoS ONE. 2015;10:doi. doi: 10.1371/journal.pone.0145262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Segura-egea J.J., Velasco-ortega E., Torres-lagares D., Velasco-ponferrada M.C., Monsalve-guil L., Llamas-carreras J.M. Pattern of antibiotic prescription in the management of endodontic infections amongst Spanish oral surgeons. Int. Endod. J. 2010;43:342–350. doi: 10.1111/j.1365-2591.2010.01691.x. [DOI] [PubMed] [Google Scholar]
- 60.Serrano C., Torres N., Valdivieso C., Castano C., Barrera M., Cabrales A. Antibiotic resistance of periodontal pathogens obtained from frequent antibiotic users. Acta Odontol. Latinoam. AOL. 2009;22:99–104. [PubMed] [Google Scholar]
- 61.Sgolastra F., Severino M., Petrucci A., Gatto R., Monaco A. Effectiveness of metronidazole as an adjunct to scaling and root planing in the treatment of chronic periodontitis: A systematic review and meta-analysis. J. Periodontal Res. 2014;49:10–19. doi: 10.1111/jre.12089. [DOI] [PubMed] [Google Scholar]
- 62.Shannon J., Shannon J., Modelevsky S., Grippo A.A. Bisphosphonates and osteonecrosis of the jaw. J. Am. Geriatr. Soc. 2011;59:2350–2355. doi: 10.1111/j.1532-5415.2011.03713.x. [DOI] [PubMed] [Google Scholar]
- 63.Arora A., Khattri S., Ismail N.M., Nagraj S.K., Prashanti E. School dental screening programmes for oral health. Cochrane Database Syst. Rev. 2017;12:CD012595. doi: 10.1002/14651858.CD012595.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Siqueira F.J., Rôças I.N. Microbiology and treatment of acute apical abscesses. Clin. Microbiol. Rev. 2013;26:255–273. doi: 10.1128/CMR.00082-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Soares S.G.M., Teles F., Starr J.R., Feres M., Patel M., Martin L., Teles R. Effects of azithromycin, metronidazole, amoxicillin, and metronidazole plus amoxicillin on an in vitro polymicrobial subgingival biofilm model. Antimicrob. Agents Chemother. 2015;59:2791–2798. doi: 10.1128/AAC.04974-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Somma F., Castagnola R., Bollino D., Marigo L. Oral inflammatory process and general health part 2011, 2, how does the periapical inflammatory process compromise general health? Eur. Rev. Med. Pharmacol. Sci. 2011;15:35–51. [PubMed] [Google Scholar]
- 67.Sousa R.E.L., Gomes B.P.F.A., Jacinto R.C., Zaia A.A., Ferraz C.C.R. Microbiological profile and antimicrobial susceptibility pattern of infected root canals associated with periapical abscesses. Eur. J. Clin. Microbiol. Infect. Dis. Off. Publ. Eur. Soc. Clin. Microbiol. 2013;32:573–580. doi: 10.1007/s10096-012-1777-5. [DOI] [PubMed] [Google Scholar]
- 68.Souto S.M.L., Rovai E.S., Ganhito J.A., Holzhausen M., Chambrone L., Pannuti C.M. Efficacy of systemic antibiotics in nonsurgical periodontal therapy for diabetic subjects: A systematic review and meta-analysis. Int. Dent. J. 2018;68:207–220. doi: 10.1111/idj.12384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Sweeny C.L., Dave J., Chambers P.A., Heritage J. Antibiotic resistance in general dental practice—A cause for concern? J. Antimicrob. Chemother. 2004;53:567–576. doi: 10.1093/jac/dkh137. [DOI] [PubMed] [Google Scholar]
- 70.Tarullo A., Tattoli M., Cagiano R. Persistent eradication of helicobacter pylori after systemic politherapy associated with periodontal pockets treatment with metronidazole and calcium sulphate. Eur. Rev. Med. Pharmacol. Sci. 2001;5:127–129. [PubMed] [Google Scholar]
- 71.Teughels W., Dhondt R., Dekeyser C., Quirynen M. Treatment of aggressive periodontitis. Periodontology 2000. 2014;65:107–133. doi: 10.1111/prd.12020. [DOI] [PubMed] [Google Scholar]
- 72.Tomas I., Tomas M., Alvarez M., Velasco D., Potel C., Limeres J., Diz P. Susceptibility of oral obligate anaerobes to telithromycin, moxifloxacin and a number of commonly used antibacterials. Oral Microbiol. Immunol. 2007;22:298–303. doi: 10.1111/j.1399-302X.2007.00359.x. [DOI] [PubMed] [Google Scholar]
- 73.Van den wyngaert T., Huizing M.T., Vermorken J.B. Osteonecrosis of the jaw related to the use of bisphosphonates. Curr. Opin. Oncol. 2007;19:315–322. doi: 10.1097/CCO.0b013e32819f820b. [DOI] [PubMed] [Google Scholar]
- 74.Van winkelhoff A.J., Herrera D., Winkel E.G., Dellemijn-kippuw N., Vandenbroucke-grauls C.M., Sanz M. Antibiotic resistance in the subgingival microflora in patients with adult periodontitis. A comparative survey between Spain and The Netherlands. Antibiot. De Subgingivale Microflora Patienten Met Adulte Parod. Een Vgl. Onderz. Tussen Spanje En Ned. 1999;106:290–294. [PubMed] [Google Scholar]
- 75.Van Winkelhoff A.J., Gonzales D.H., Winkel E.G., Dellemijn-kippuw N., Vandenbroucke-grauls C.M., Sanz M. Antimicrobial resistance in the subgingival microflora in patients with adult periodontitis. A comparison between The Netherlands and Spain. J. Clin. Periodontol. 2000;27:79–86. doi: 10.1034/j.1600-051x.2000.027002079.x. [DOI] [PubMed] [Google Scholar]
- 76.Van Winkelhoff A.J., Herrera D., Oteo A., Sanz M. Antimicrobial profiles of periodontal pathogens isolated from periodontitis patients in The Netherlands and Spain. J. Clin. Periodontol. 2005;32:893–898. doi: 10.1111/j.1600-051X.2005.00782.x. [DOI] [PubMed] [Google Scholar]
- 77.Veloo M.A.C., Seme K., Raangs E., Rurenga P., Singadji Z., Wekema-mulder G., van winkelhoff A.J. Antibiotic susceptibility profiles of oral pathogens. Int. J. Antimicrob. Agents. 2012;40:450–454. doi: 10.1016/j.ijantimicag.2012.07.004. [DOI] [PubMed] [Google Scholar]
- 78.Voils A.S., Evans M.E., Lane M.T., Schosser R.H., Rapp R.P. Use of macrolides and tetracyclines for chronic inflammatory diseases. Ann. Pharmacother. 2005;39:86–94. doi: 10.1345/aph.1E282. [DOI] [PubMed] [Google Scholar]
- 79.Zandbergen D., Slot D.E., Cobb C.M., van der weijden F.A. The clinical effect of scaling and root planing and the concomitant administration of systemic amoxicillin and metronidazole: A systematic review. J. Periodontol. 2013;84:332–351. doi: 10.1902/jop.2012.120040. [DOI] [PubMed] [Google Scholar]
- 80.Zhang Z., Zheng Y., Bian X. Clinical effect of azithromycin as an adjunct to non-surgical treatment of chronic periodontitis: A meta-analysis of randomized controlled clinical trials. J. Periodontal Res. 2016;51:275–283. doi: 10.1111/jre.12319. [DOI] [PubMed] [Google Scholar]
- 81.Ammann W.T., Bostanci N., Belibasakis G.N., Thurnheer T. Validation of a quantitative real-time PCR assay and comparison with fluorescence microscopy and selective agar plate counting for species-specific quantification of an in vitro subgingival biofilm model. J. Periodontal Res. 2013;48:517–526. doi: 10.1111/jre.12034. [DOI] [PubMed] [Google Scholar]
- 82.Socransky S.S., Haffajee A.D., Smith C., Martin L., Haffajee J.A., Uzel N.G., Goodson J.M. Use of checkerboard DNA-DNA hybridization to study complex microbial ecosystems. Oral Microbiol. Immunol. 2004;19:352–362. doi: 10.1111/j.1399-302x.2004.00168.x. [DOI] [PubMed] [Google Scholar]
- 83.Socransky S.S., Haffajee A.D. Dental biofilms: Difficult therapeutic targets. Periodontology 2000. 2002;28:12–55. doi: 10.1034/j.1600-0757.2002.280102.x. [DOI] [PubMed] [Google Scholar]
- 84.Greenwood D. Antimicrobial Drugs. Oxford University Press; Oxford, UK: 2008. [Google Scholar]
- 85.Gomi K., Yashima A., Iino F., Kanazashi M., Nagano T., Shibukawa N., Ohshima T., Maeda N., Arai T. Drug concentration in inflamed periodontal tissues after systemically administered azithromycin. J. Periodontol. 2007;78:918–923. doi: 10.1902/jop.2007.060246. [DOI] [PubMed] [Google Scholar]
- 86.Haffajee D.A., Patel M., Socransky S.S. Microbiological changes associated with four different periodontal therapies for the treatment of chronic periodontitis. Oral Microbiol. Immunol. 2008;23:148–157. doi: 10.1111/j.1399-302X.2007.00403.x. [DOI] [PubMed] [Google Scholar]
- 87.López-boado S.Y., Rubin B.K. Macrolides as immunomodulatory medications for the therapy of chronic lung diseases. Curr. Opin. Pharmacol. 2008;8:286–291. doi: 10.1016/j.coph.2008.01.010. [DOI] [PubMed] [Google Scholar]
- 88.Schreiber F., Szewzyk U. Environmentally relevant concentrations of pharmaceuticals influence the initial adhesion of bacteria. Aquat. Toxicol. 2008;87:227–233. doi: 10.1016/j.aquatox.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 89.Hardy J.D., Hensey D.M., Beyer J.M., Vojtko C., Mcdonald E.J., Fernandes P.B. Comparative in vitro activities of new 14-, 15-, and 16-membered macrolides. Antimicrob. Agents Chemother. 1988;32:1710–1719. doi: 10.1128/AAC.32.11.1710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Murphy S.B., Sundareshan V., Cory T.J., Hayes D., Anstead M.I., Feola D.J. Azithromycin alters macrophage phenotype. J. Antimicrob. Chemother. 2008;61:554–560. doi: 10.1093/jac/dkn007. [DOI] [PubMed] [Google Scholar]
- 91.Winkel G.E., van winkelhoff A.J., Timmerman M.F., van der velden U., van der weijden G.A. Amoxicillin plus metronidazole in the treatment of adult periodontitis patients. A double-blind placebo-controlled study. J. Clin. Periodontol. 2001;28:296–305. doi: 10.1034/j.1600-051x.2001.028004296.x. [DOI] [PubMed] [Google Scholar]
- 92.Beikler T., Karch H., Flemmig T.F. Adjuvante antibiotika in der parodontitistherapie. Dtsch Zahnärztl. 2003;58:263–265. [Google Scholar]
- 93.Kleinfelder W.J., Müller R.F., Lange D.E. Antibiotic susceptibility of putative periodontal pathogens in advanced periodontitis patients. J. Clin. Periodontol. 1999;26:347–351. doi: 10.1034/j.1600-051X.1999.260603.x. [DOI] [PubMed] [Google Scholar]
- 94.Heekin D.R., Shorter D., Kosten T.R. Current status and future prospects for the development of substance abuse vaccines. Expert Rev. Vaccines. 2017;16:1067–1077. doi: 10.1080/14760584.2017.1378577. [DOI] [PubMed] [Google Scholar]
- 95.Pähkla R.E., Koppel T., Saag M., Pähkla R. Metronidazole concentrations in plasma, saliva and periodontal pockets in patients with periodontitis. J. Clin. Periodontol. 2005;32:163–166. doi: 10.1111/j.1600-051X.2005.00653.x. [DOI] [PubMed] [Google Scholar]
- 96.Jain N., Lai P.C., Walters J.D. Effect of gingivitis on azithromycin concentrations in gingival crevicular fluid. J. Periodontol. 2012;83:1122–1128. doi: 10.1902/jop.2012.110558. [DOI] [PMC free article] [PubMed] [Google Scholar]