Abstract
Primary enterolithiasis is a relatively uncommon but important cause of small bowel obstruction. We present a case of a 69-year-old male with a history of laparoscopic Roux-en-Y gastric bypass and asymptomatic duodenal diverticulum diagnosed with small bowel obstruction. CT imaging showed an obstruction distal to the jejunojejunostomy, and surgical intervention was warranted. A 4.5 cm enterolith removed from the distal jejunum was found to contain 100% bile salts, consistent with a primary enterolith. Clinicians should retain a high index of suspicion for enteroliths as a cause of small bowel obstruction, especially if multiple risk factors for enterolith formation are present.
1. Introduction
Enteroliths are intestinal concretions that vary widely in etiology, chemical composition, and clinical presentation. They can be categorized into primary (caused by intestinal stasis) and secondary (caused by migration via fistulous connection to the gallbladder or kidneys) [1]. Here, we present a case of primary intestinal enterolith causing small bowel obstruction that was originally diagnosed as a secondary gallstone ileus.
2. Case Presentation
A 69-year-old male with a remote history of laparoscopic Roux-en-Y gastric bypass 4 years earlier and a known duodenal diverticulum presented to the emergency department for bilateral upper quadrant abdominal pain for several weeks that had progressed rapidly to constant nausea, abdominal distension, and food intolerance. A CT scan of the abdomen revealed a very distended gastric remnant and what appeared to be a bowel obstruction distal to the jejunojejunostomy (Figure 1). A nasogastric tube was placed for decompression and he was taken emergently to the operating room for an exploratory laparotomy for presumed gallstone ileus. At the time of surgery, a 4.5 cm enterolith was found and removed from the distal jejunum via longitudinal enterotomy, followed by a cholecystectomy in which gallstones were found but no cholecystoenteric fistula was noted. The enterolith was sent to an outside laboratory for stone analysis and was found to contain 100% bile salts (Figure 2). The remainder of the patient's hospital stay was uneventful, and he was discharged on postoperative day 8. He remained in good health at his postoperative visit 2 weeks after surgery but then was lost to follow-up 1 month after surgery.
Figure 1.
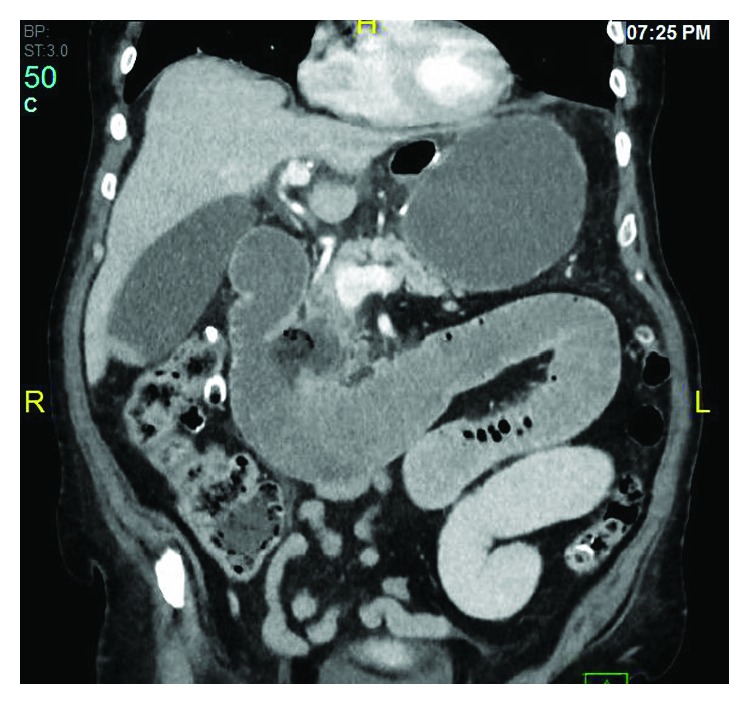
CT scan of the abdomen showing a duodenal diverticulum with dilation of the biliopancreatic limb secondary to high-grade obstruction at the distal jejunum.
Figure 2.
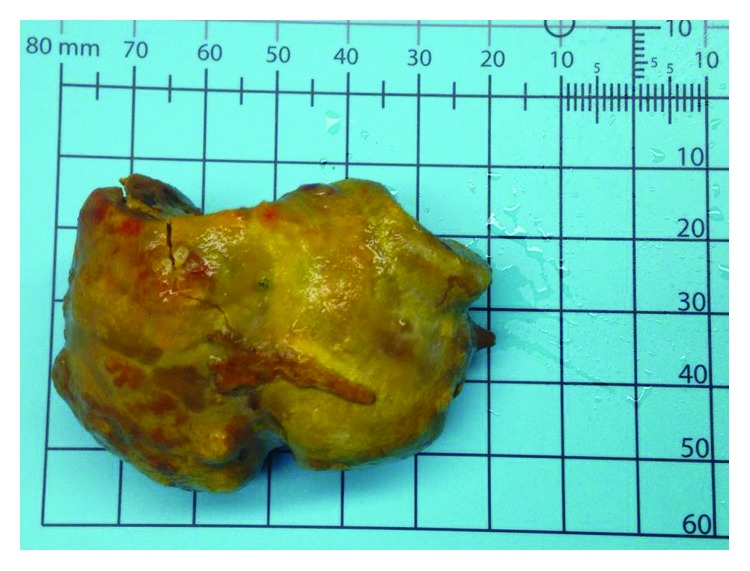
The 4.5 cm enterolith recovered from the distal jejunum/proximal ileum. Stone analysis showed this enterolith was composed of 100% bile salts.
3. Discussion
This case illustrates a primary enterolith ileus that was initially thought to be a gallstone ileus. However, no evidence of a biliary-enteric fistula was found on CT scan or upon visual inspection of the gallbladder in the operating room, which further confirms the diagnosis of primary enterolith.
The diagnosis of enterolith ileus is established by observing an unremarkable gallbladder and the presence of a small bowel diverticula [2], in this case a duodenal diverticulum. Duodenal diverticulosis is a long-recognized abnormality, first described in 1710 by French physician J.B.L. Chomel [3]. It is not a particularly rare condition, affecting anywhere from 2-7% of the population [1] and is usually of little clinical significance [4]. However, it may present as diverticulitis, hemorrhage, malabsorption, or obstruction [1, 5]. When stagnation of diverticular contents is present, the rare complication of enterolith formation and obstruction may occur [2, 6, 7]. Risk factors for enterolith development include Crohn's disease, hernias, bowel diverticula, surgical anastomoses and afferent loops, small intestinal tumors, and intestinal infections including tuberculosis [2, 8–16].
Optimal management for a patient presenting with an enterolith-induced bowel obstruction includes serial abdominal examination, correction of electrolyte abnormalities, and nasogastric decompression. This noninvasive strategy may be appropriate for enteroliths less than 2 cm in diameter that are more likely to spontaneously pass through the bowel [17]. Stones larger than 2 cm should undergo surgical excision which usually includes “milking” the enterolith to a less edematous portion of the small intestine where an enterotomy is performed for removal [18–20].
Our patient exhibited several risk factors for the development of an enterolith—a preexisting duodenal diverticulum, a Roux-en-Y gastric bypass with side-to-side anastomoses and afferent loop, and a disruption of normal bowel peristalsis secondary to his bariatric surgery [8]. We believe that these conditions promoted precipitation of bile salts in his duodenal diverticulum, allowing a large enterolith to form. These alterations in intestinal anatomy and function are key to making the diagnosis of bile salt enterolith obstruction in this patient, and a detailed history and physical exam are paramount to this investigation. Radiological studies including upper gastrointestinal series or CT scans should be used to investigate possible sources of bowel obstruction and to exclude mimics. Surgical management should be centered around obstruction relief and prevention of recurrence. Improved diagnostic imaging and innovations in laparoscopic and minimally invasive surgery will provide patients with decreased morbidity versus traditional laparotomy procedures.
Conflicts of Interest
The authors declare that they have no conflict of interest or disclosures.
References
- 1.Gurvits G. E., Lan G. Enterolithiasis. World Journal of Gastroenterology. 2014;20(47):17819–17829. doi: 10.3748/wjg.v20.i47.17819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wilson I., Parampalli U., Butler C., Ahmed I., Mowat A. Multiple large enteroliths associated with an incisional hernia: a rare case. Annals of the Royal College of Surgeons of England. 2012;94(7):e20–s22. doi: 10.1308/003588412X13373405385890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cattell R. B., Mudge T. J. The surgical significance of duodenal diverticula. The New England Journal of Medicine. 1952;246(9):317–324. doi: 10.1056/NEJM195202282460901. [DOI] [PubMed] [Google Scholar]
- 4.Melnick S., Fareedy S., Gish D., Nazir S. Duodenal diverticulum: incidental finding with potentially dangerous outcomes. Journal of Community Hospital Internal Medicine Perspectives. 2017;7(1):56–57. doi: 10.1080/20009666.2017.1291784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Desai K., Wermers J. D., Beteselassie N. Lemmel syndrome secondary to duodenal diverticulitis: a case report. Cureus. 2017;9(3, article e1066) doi: 10.7759/cureus.1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hayee B., Khan H. N., Al-Mishlab T., McPartlin J. F. A case of enterolith small bowel obstruction and jejunal diverticulosis. World Journal of Gastroenterology. 2003;9(4):883–884. doi: 10.3748/wjg.v9.i4.883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ichikawa T., Koizumi J., Onoue K., et al. CT features of juxtapapillary duodenal diverticula with complications. The Tokai Journal of Experimental and Clinical Medicine. 2008;33(2):90–94. [PubMed] [Google Scholar]
- 8.Beal S. L., Walton C. B., Bodai B. I. Enterolith ileus resulting from small bowel diverticulosis. The American Journal of Gastroenterology. 1987;82(2):162–164. [PubMed] [Google Scholar]
- 9.Cartanese C., Campanella G., Milano E., Sacco M. Enterolith causing acute afferent loop syndrome after Billroth II gastrectomy: a case report. Il Giornale di Chirurgia. 2013;34(5-6):164–166. doi: 10.11138/gchir/2013.34.5.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee M. C., Bui J. T., Knuttinen M. G., Gaba R. C., Scott Helton W., Owens C. A. Enterolith causing afferent loop obstruction: a case report and literature review. Cardiovascular and Interventional Radiology. 2009;32(5):1091–1096. doi: 10.1007/s00270-009-9561-3. [DOI] [PubMed] [Google Scholar]
- 11.Sarli L., Iusco D., Violi V., Roncoroni L. Enterolith ileus complicating afferent loop syndrome simulating acute pancreatitis. International Surgery. 2003;88(3):129–132. [PubMed] [Google Scholar]
- 12.Sato K., Banshodani M., Nishihara M., et al. Afferent loop obstruction with obstructive jaundice and ileus due to an enterolith after distal gastrectomy: a case report. International Journal of Surgery Case Reports. 2018;50:9–12. doi: 10.1016/j.ijscr.2018.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shin J. K., Choi S. H., Hong S. D., et al. Common bile duct obstruction due to a large stone at the duodenal stump. The Korean Journal of Gastroenterology. 2016;67(3):150–152. doi: 10.4166/kjg.2016.67.3.150. [DOI] [PubMed] [Google Scholar]
- 14.Shivathirthan N., Maheshwari G., Kamath D., Haldar P. Enterolithiasis complicating eosinophilic enteritis: a case report and review of literature. World Journal of Gastrointestinal Surgery. 2009;1(1):68–70. doi: 10.4240/wjgs.v1.i1.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tien Y. W., Lee P. H., Chang K. J. Enterolith: an unusual cause of afferent loop obstruction. The American Journal of Gastroenterology. 1999;94(5):1391–1392. doi: 10.1111/j.1572-0241.1999.01092.x. [DOI] [PubMed] [Google Scholar]
- 16.Perathoner A., Kogler P., Denecke C., Pratschke J., Kafka-Ritsch R., Zitt M. Enterolithiasis-associated ileus in Crohn's disease. World Journal of Gastroenterology. 2012;18(42):6160–6163. doi: 10.3748/wjg.v18.i42.6160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ihara E., Ochiai T., Yamamoto K., Kabemura T., Harada N. A case of gallstone ileus with a spontaneous evacuation. The American Journal of Gastroenterology. 2002;97(5):1259–1260. doi: 10.1111/j.1572-0241.2002.05715.x. [DOI] [PubMed] [Google Scholar]
- 18.Leow C. K., Lau W. Y. Treatment of small bowel obstruction by jejunal enterolith. Surgery. 1997;122(5):977–978. doi: 10.1016/S0039-6060(97)90349-4. [DOI] [PubMed] [Google Scholar]
- 19.Phelan M., Kaufman H., Becker J., Fitzpatrick G. Small bowel obstruction by jejunal enterolith. Surgery. 1997;121(2):229–230. doi: 10.1016/S0039-6060(97)90296-8. [DOI] [PubMed] [Google Scholar]
- 20.Shocket E., Simon S. A. Small bowel obstruction due to enterolith (bezoar) formed in a duodenal diverticulum: a case report and review of the literature. The American Journal of Gastroenterology. 1982;77(9):621–624. [PubMed] [Google Scholar]


