Summary
Background and objectives
In 2007, the Emory Transplant Center (ETC) kidney transplant program implemented a required educational session for ESRD patients referred for renal transplant evaluation to increase patient awareness and decrease loss to follow-up. The purpose of this study was to evaluate the association of the ETC education program on completion of the transplant evaluation process.
Design, setting, participants, & measurements
Incident, adult ESRD patients referred from 2005 to 2008 were included. Patient data were abstracted from medical records and linked with data from the United States Renal Data System. Evaluation completion was compared by pre- and posteducational intervention groups in binomial regression models accounting for temporal confounding.
Results
A total of 1126 adult ESRD patients were examined in two transplant evaluation eras (75% pre- and 25% postintervention). One-year evaluation completion was higher in the post- versus preintervention group (80.4% versus 44.7%, P<0.0001). In adjusted analyses controlling for time trends, the adjusted probability of evaluation completion at 1 year was higher among the intervention versus nonintervention group (risk ratio=1.38, 95% confidence interval=1.12–1.71). The effect of the intervention was stronger among black patients and those patients living in poor neighborhoods (likelihood ratio test for interaction, P<0.05).
Conclusion
Standardizing transplant education may help reduce some of the racial and socioeconomic disparities observed in kidney transplantation.
Introduction
Kidney transplantation is the preferred treatment for ESRD patients and is associated with increased quality of life and reduced morbidity and mortality compared with dialysis (1). Despite strong evidence for improved quality of life and survival after transplantation, there is a large gap between the number of patients who need a kidney transplant and the number of available organs (2). Racial disparities in access to kidney transplantation have been documented in several steps in the renal transplant process, including referral, evaluation completion, and waitlisting (3–9). The reasons for the disparities are likely multifactorial, and they may not be entirely explained by clinical factors (10–12). Lack of patient education about kidney disease and the renal transplant process may be one explanation for disparities observed in completion of transplant evaluation (13–15).
Evidence to guide interventions to reduce disparities in access to earlier steps of the renal transplant process, including evaluation completion, is limited. In mid-2007, the kidney transplant program at the Emory Transplant Center (ETC) implemented a formal educational intervention to better inform patients of the transplant process and decrease loss to follow- up of patients evaluated for renal transplantation. The purpose of this study was to determine if the intervention increased the proportion of patients completing the formal evaluation process and improved or hindered access to renal transplantation among black patients and individuals with lower socioeconomic status (SES).
Materials and Methods
Data Sources
Patient demographic, clinical, and follow-up data were obtained from EC hardcopy and electronic medical records. ETC patient data were linked with United States Renal Data System (USRDS) surveillance data to obtain patient information at the time of ESRD start. Patient residential addresses were geocoded and assigned a census tract using ArcGIS 9.2. Data on neighborhood poverty by census tract were obtained from the American Community Survey 2005–2009.
Study Population
A total of 2694 adult (age>18years) ESRD patients were referred to the ETC for kidney transplant evaluation from January 1, 2005 to March 31, 2008. Of these patients, 1519 patients started the kidney transplant evaluation process. The following exclusion criteria were applied: (1) patients missing a home address, having an address listed as a PO Box (n=7), or having a residential address outside of the southeast (GA, AL, FL, SC, NC, and TN) region (n=83); (2) patients who reported other race or Hispanic ethnicity (n=130); (3) patients with no USRDS record (n=57); and (4) patients listed at other transplant centers before referral (n=116). A total of 1126 patients were included in the final study population (Figure 1).
Figure 1. |.

Flow diagram of study inclusion criteria and follow-up status.
Explanatory Variables
The primary exposure variable for all analyses was attendance at the formal educational session. Patients starting the evaluation process after September 4, 2007, were required to attend a formal educational session consisting of an in-center, half-day patient education class involving lectures and discussions from a transplant co-ordinator, financial coordinator, and social worker. These patients were assigned to the posteducational intervention group. Education before September 4, 2007, was decentralized and less structured, with various elements of the education occurring during the evaluation process. These patients were defined as the pre-educational intervention group.
The secondary exposure of interest was self-reported race (black or white) based on data collected from the ETC at the time of renal transplant evaluation.
Patient-Level Covariates
Patient demographic and clinical characteristics collected at the time of transplant evaluation included age, sex, etiology of ESRD, body mass index >35 kg/m2, and time on dialysis. To obtain information about a patient’s health status at the time of ESRD start, patient data were obtained from the USRDS medical evidence form (CMS 2728 form). Clinical variables included predialysis erythropoiesis- stimulating agent use (yes/no), hemoglobin (<11 versus ≥11 g/dl), serum albumin (<3.5 versus ≥3.5 g/dl), history of cardiovascular disease (CVD), tobacco use (yes/no), and history of cancer (yes/no) at dialysis initiation.
We defined individual SES using health insurance, highest education, and employment status. Health insurance at the time of ESRD start and at the time of evaluation was categorized as private (employer), Medicare, or Medicaid. Patient SES data were abstracted from the psychosocial evaluation or history and physical notes from patient records.
Neighborhood-Level Covariates
We estimated neighborhood SES with the 2005–2009 American Community Survey data on the proportion of individuals residing below the poverty line within the area. We categorized high poverty as a neighborhood with at least 20% of census tract residents living below the federal poverty line.
Outcome Variables
The primary outcome was completion of the evaluation process within 1 year (yes/no) defined by the date a patient completed all evaluation requirements as deemed by the multidisciplinary transplant team. We also examined the time (in days) from evaluation start to completion.
Statistical Analyses
Differences in the means and proportions of baseline patient demographic and clinical characteristics by pre- and postintervention group were examined using chi-squared and t tests and ANOVA. The proportion of patients completing the evaluation process within 1 year was calculated by pre- and posteducational intervention groups. To determine whether evaluation completion differed from pre- to post-eras among disadvantaged groups, we calculated the proportion of patients completing the evaluation by intervention group for each racial and socioeconomic group. A multivariable, binomial regression model was developed to assess the effect of the educational intervention on evaluation completion, while considering the multilevel effects of both individual and neighborhood (census tract) effects. To control for time trends over the cohort follow-up period, we adjusted analyses for time of entry into the study cohort (in days; centered at the median time of follow-up) for each patient to account for temporal confounding by unmeasured factors that affect time trend independent of the intervention.
To investigate our hypothesis that the effect of the educational intervention varied by race and SES, we examined effect modification of the intervention and race for each SES variable in binomial regression models using the likelihood ratio (LR) test to assess significance. If interaction was detected, the risk ratio (RR) and corresponding 95% confidence intervals (CIs) for the effect of the intervention on evaluation completion was explored among each subgroup.
To determine whether the time from evaluation start to completion at 1 year varied by intervention group, we examined the time (in days) from evaluation start to completion using Kaplan-Meier methods and the log-rank test for significance. Furthermore, because 25 people died during the 1-year follow-up period, we also examined the crude and multivariable-adjusted effects of the educational intervention in Cox Proportional Hazards models (16). Patients were censored at death or after 365 days of follow-up. The robust sandwich variance estimator with census tract as the cluster variable was used to examine neighborhood- and individual-level covariates simultaneously, while also accounting for potential correlation of patients within neighborhoods (17). For all analyses, two-tailed P<0.05 was considered statistically significant. ArcGIS 9.2 was used for geocoding and spatial joining. SAS 9.2 was used for all statistical analyses. This study protocol was approved by the Emory Institutional Review Board.
Sensitivity Analyses
To reduce the potential impact of confounding by time period effects in our study, we restricted the analyses to a 6-month time period that compared pre- and postintervention groups from May of 2007 to December of 2007 only and calculated crude and multivariable-adjusted RR values to examine the effect of evaluation completion by group.
Detailed SES data were only abstracted for patients evaluated at ETC through March of 2008, and thus, the two groups (pre- and posteducational interventions) were unequal in size. To examine whether the smaller, postintervention group was different from patients evaluated after this period, we also examined evaluation completion among patients evaluated in the 2 years after the study in sensitivity analyses.
Results
Study Population Characteristics
Among the 1126 adult ESRD patients evaluated for kidney transplant candidacy at the ETC, the mean age was 50.5 (±13.3) years, 58.9% were male, 58.7% were black, and 39.8% had a history of CVD (Table 1). More than one-half (57.6%) of the study population had private health insurance, over 80% had at least a high school education, and 34.1% were employed at the time of evaluation start. Compared with patients in the pre-educational intervention group, a greater proportion of patients who started the evaluation process at the ETC after the intervention was implemented was black (63.4% in post- versus 57.2% in preintervention group, P=0.07), had a history of CVD (48.0% versus 37.0%, P=0.001), and had been on dialysis >24 months (28.5% versus 20.7% preintervention, P=0.04).
Table 1.
Characteristics of patients evaluated for renal transplantation at Emory Transplant Center from 2005 to 2008 by the Educational Intervention Group
| Characteristic | Study Population (n=1126) |
Preimplementation of Education Intervention (n=845; 75.0%) |
Postimplementation of Educational Intervention (n=281; 25.0%) |
P Value |
|---|---|---|---|---|
| Patient-level characteristics at evaluation start | ||||
| mean age in years (SD) | 50.5±13.3 | 50.6±13.0 | 50.7±13.3 | 0.85 |
| age category (%) | 0.63 | |||
| 20–39 years | 265 (23.5%) | 190 (22.5%) | 75 (26.7%) | |
| 40–49 years | 251 (22.3%) | 194 (23.0%) | 57 (20.3%) | |
| 50–59 years | 319 (28.3%) | 242 (28.6%) | 77 (27.4%) | |
| 60–69 years | 212 (18.8%) | 161 (19.1%) | 51 (18.2%) | |
| 70–85 years | 79 (7.0%) | 58 (6.9%) | 21 (7.5%) | |
| male (%) | 663 (58.9%) | 499 (59.1%) | 164 (58.4%) | 0.84 |
| race | 0.07 | |||
| white | 465 (41.3%) | 362 (42.8%) | 103 (36.7%) | |
| black | 661 (58.7%) | 483 (57.2%) | 178 (63.4%) | |
| cause of ESRD (%) | 0.73 | |||
| diabetes | 415 (36.9%) | 306 (36.2%) | 109 (38.8%) | |
| hypertension | 331 (29.4%) | 255 (30.2%) | 76 (27.1%) | |
| glomerulonephritis | 130 (11.6%) | 99 (11.7%) | 31 (11.0%) | |
| other | 250 (22.2%) | 185 (21.9%) | 65 (21.1%) | |
| time on dialysis | 0.04 | |||
| no dialysis | 249 (22.1%) | 201 (23.8%) | 48 (17.1%) | |
| 0–6 months | 210 (18.7%) | 160 (18.9%) | 50 (17.8%) | |
| 6–12 months | 237 (21.1%) | 177 (21.0%) | 60 (21.4%) | |
| 12–24 months | 175 (15.5%) | 132 (15.6%) | 43 (15.3%) | |
| >24 months | 255 (22.7%) | 175 (20.7%) | 80 (28.5%) | |
| Clinical and laboratory measures | ||||
| body mass index >35 kg/m2 | 163 (14.5%) | 127 (15.0%) | 26 (12.8%) | 0.36 |
| history of CVDa | 448 (39.8%) | 313 (37.0%) | 135 (48.0%) | 0.001 |
| history of cancer | 19 (1.7%) | 12 (1.4%) | 7 (2.5%) | 0.23 |
| serum albumin <3.5 g/dl at dialysis initiation | 716 (63.6%) | 531 (62.8%) | 185 (65.8%) | 0.37 |
| hemoglobin <10 g/dl at dialysis initiation | 556 (49.4%) | 411 (48.6%) | 145 (51.6%) | 0.39 |
| predialysis ESAb | 349 (31.1%) | 257 (30.4%) | 92 (32.7%) | 0.47 |
| Socioeconomic characteristics at evaluation start | ||||
| health insurance coverage | 0.25 | |||
| Medicaid | 232 (20.6%) | 182 (31.5%) | 50 (17.8%) | |
| Medicare | 245 (21.8%) | 176 (20.8%) | 69 (24.6%) | |
| private | 649 (57.6%) | 487 (57.6%) | 162 (57.7%) | |
| highest education | 0.32 | |||
| less than high school degree | 199 (17.7%) | 153 (18.1%) | 46 (16.4%) | |
| completed high school | 376 (33.4%) | 292 (34.6%) | 84 (29.9%) | |
| some college | 308 (27.4%) | 218 (25.8%) | 90 (32.0%) | |
| completed college | 215 (19.1%) | 161 (19.1%) | 54 (19.2%) | |
| unknown | 28 (2.5%) | 21 (2.5%) | 7 (2.5%) | |
| employment statusc | 0.89 | |||
| employed or full-time student | 384 (34.1%) | 284 (33.6%) | 100 (35.6%) | |
| disabled or not working | 414 (36.8%) | 315 (37.3%) | 99 (35.2%) | |
| retired | 328 (29.1%) | 246 (29.1%) | 82 (29.2%) | |
| neighborhood poverty (percent census tract below poverty) | 0.31 | |||
| <20% | 800 (71.1%) | 607 (71.8%) | 193 (68.7%) | |
| ≥20% | 326 (28.9%) | 238 (28.2%) | 88 (31.3%) |
CVD, cardiovascular disease (defined as history of congestive heart failure, ischemic heart disease, cardiac arrest, myocardial infarction, cardiac dysrhythmia, pericarditis, or cerebrovascular disease).
ESA, erythropoiesis-stimulating agent.
For patients with missing employment status at the time of ESRD (n=31), employment status at the time of evaluation was used.
Evaluation Completion
One-year evaluation completion was significantly higher in the post- versus pre-educational intervention group (44.7% in the pre- and 80.4% in the postevaluation groups), with the overall probability of evaluation completion 1.7 times higher than the probability of evaluation completion among the pre-educational intervention group (crude RR=1.72, 95% CI=1.51–1.95). In multivariable-adjusted analyses that also accounted for temporal confounding, this effect was attenuated but significant (RR=1.38; 95% CI=1.12–1.71).
Increases in evaluation completion were observed across all racial and socioeconomic groups. In the pre-educational intervention group, significant differences in evaluation completion within racial and socioeconomic subgroup were observed, where a greater proportion of patients completing the evaluation were white versus black (49.7% versus 41.0%), had private insurance (51.1%) versus Medicare (42.1%) or Medicaid (30.2%), had at least some college education (53.2%) versus less than a high school degree (28.8%), and lived in wealthy (48.8%) versus poor (34.5%) neighborhoods (P<0.01 for all). However, after implementation of the educational intervention, no significant differences were observed by racial or socioeconomic group (Table 2).
Table 2.
Evaluation completion among racial and socioeconomic groups by pre- and posteducaitonal intervention
| Subgroup | Preimplementation of Educational Intervention (Evaluation Status) |
Postimplementation of Educational Intervention (Evaluation Status) |
Change(%) | P Valuea | ||
|---|---|---|---|---|---|---|
| Started | Completed at 1 Year (%) |
Started | Completed at 1 Year (%) |
|||
| Total population | 845 | 378 (44.7) | 281 | 226 (80.4) | +35.7 | <0.001 |
| Raceb | ||||||
| white | 362 | 180 (49.7) | 103 | 84 (81.6) | +31.9 | <0.001 |
| black | 483 | 198 (41.0) | 178 | 142 (79.8) | +38.8 | <0.001 |
| Health insurance coverageb | ||||||
| Medicaid | 182 | 55 (30.2) | 50 | 35 (70.0) | +39.8 | <0.001 |
| Medicare | 176 | 74 (42.1) | 69 | 56 (81.2) | +39.1 | <0.001 |
| private | 487 | 249 (51.1) | 162 | 135 (83.3) | +32.2 | <0.001 |
| Highest educationb | ||||||
| less than high school | 153 | 44 (28.8) | 46 | 34 (73.9) | +45.1 | <0.001 |
| completed high school | 292 | 127 (43.5) | 84 | 71 (84.5) | +41.0 | <0.001 |
| some college | 218 | 116 (53.2) | 90 | 68 (75.6) | +22.4 | <0.001 |
| completed college | 161 | 83 (51.6) | 54 | 48 (88.9) | +37.3 | <0.001 |
| Employmentb | ||||||
| employed | 284 | 151 (53.2) | 100 | 86 (86.0) | +32.8 | <0.001 |
| unemployed | 315 | 134 (42.5) | 99 | 74 (74.8) | +32.3 | <0.001 |
| retired | 246 | 93 (37.8) | 82 | 66 (80.5) | +42.7 | <0.001 |
| Neighborhood povertyb | ||||||
| <20% | 607 | 296 (48.8) | 193 | 155 (80.3) | +31.5 | <0.001 |
| ≥20% | 238 | 82 (34.5) | 88 | 71 (80.7) | +46.2 | <0.001 |
Values are testing the difference between the pre- and postintervention groups by subgroup.
Statistically significant difference in evaluation completion within subgroup observed in pre- but not posteducational group
In multilevel analyses accounting for potential correlation of patients living in the same neighborhood and adjusting for sociodemographic and clinical characteristics and the potential confounding by time period, the effect of the intervention varied across racial and socioeconomic groups. Figure 2 shows the crude and multivariable-adjusted RR and corresponding 95% CI values for evaluation completion by racial and socioeconomic group. The intervention significantly improved the probability of 1-year evaluation completion among black (RR=1.46, 95% CI=1.11–1.94) but not white (RR=1.02, 95% CI=0.75–1.38) patients (LR P value=0.02), and it was higher among patients living in poor (RR=1.65, 95% CI=0.98–2.78) than wealthy neighborhoods (RR=1.28, 95% CI=1.01–1.62; LR P value= 0.01).
Figure 2. |. Effect of intervention differed across racial and socioeconomic groups.
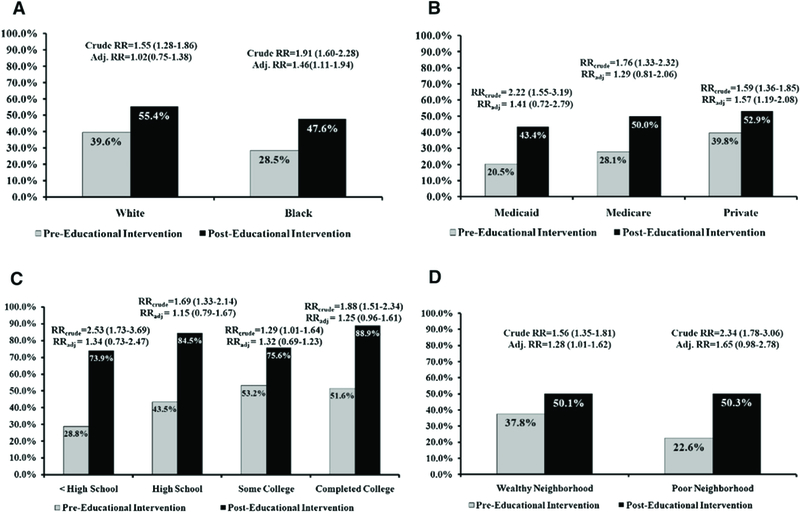
The effect of intervention by racial group is illustrated in A (likelihood ratio [LR] test for interaction in adjusted analyses, P=0.02). The effect of the intervention by insurance status is illustrated in B (LR test for interaction in adjusted analyses, P=0.14). (C) Interaction by educational level was not significant in crude and adjusted analyses. (D) The effect of the intervention differed by neighborhood poverty (LR test for interaction oin adjusted analyses, P=0.01). Analyses were adjusted for age, sex, race, time of entry into study, duration of dialysis, history of cardiovascular disease, health insurance, employment status, educational attainment, and neighborhood poverty.
Kaplan-Meier estimates showed consistent results. The median time to evaluation completion was 378 days (interquartile range=198–656) among patients in the pre- and 204 days (interquartile range=116–309) among patients in the postintervention group (log-rank P<0.0001) (Figure 3). In crude Cox models, the rate of completion was more than two times as high among patients in the post- versus pre-educational intervention group (hazard ratio=2.20, 95% CI=1.77–2.73, P<0.0001) but was attenuated in multivariable-adjusted results accounting for time period effects (hazard ratio=1.32, 95% CI=0.97–1.79). Subgroup analyses examining the effect of the intervention among racial and socioeconomic groups were consistent with binomial regression analyses, where the effect of the intervention was more pronounced among black patients and those patients living in poor neighborhoods (LR P value for interaction< 0.05).
Figure 3. |.
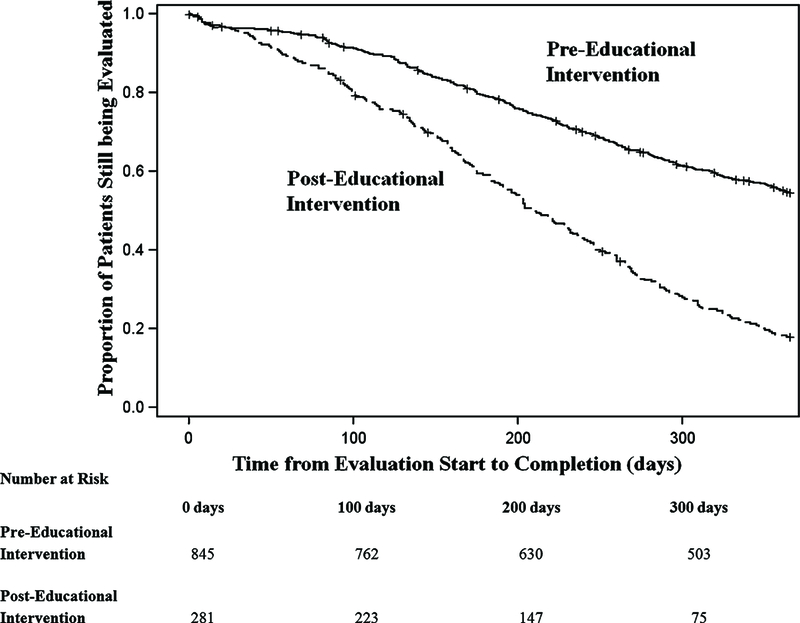
Kaplan-Meier estimates for time to evaluation completion by pre- and posteducational intervention groups.
Sensitivity Analyses
Analyses examining the probability of evaluation completion by intervention group among only renal transplant evaluations from May of 2007 to December of 2007 resulted in nearly identical results to the main analyses that adjusted for time period cohort effects. Racial and SES subgroup analyses examining evaluation completion were also consistent (results not shown).
We examined the demographic and clinical characteristics of patients evaluated from 2008 to 2010 and compared them with patients included in the intervention group of this study. Patient characteristics were similar, and the effect of the intervention was sustained throughout the 2- year period. For example, among patients evaluated from 2008 to 2010, a total of 79.7% completed the evaluation at 1 year (versus 80.4% in the study intervention group). Racial differences were fairly consistent, with 82.4% of white patients completing the evaluation at 1 year versus 78.3% of black patients.
Discussion
This retrospective assessment of a single-center patient education program for renal transplant candidates showed that the probability of completing a renal transplant evaluation was higher after the implementation of a patient education program. Although randomization of the formal education program would have been ideal to eliminate the potential for confounding by time, a randomized trial would have been costly, and the results would be limited in their generalizability. Our analysis offers an efficient, replicable method to compare the effect of a historical intervention on all patients evaluated. Results of this study suggest that requiring a formal patient education class may have improved both the efficiency of the transplant process and access to renal transplantation for poor and minority patients.
Although clinical guidelines for the evaluation of renal transplant candidates have been developed, comprehensive recommendations for the content and format of the patient education component of the evaluation process do not currently exist (18). There are few, if any, evaluations of interventions to improve racial disparities in access to kidney transplantation. A retrospective comparative effectiveness study that evaluates the impact of a formal, in-center patient education program compared with no formal education is cost-efficient, and the design and analysis of the present study is simple to replicate in other centers. In addition, the present study is novel in its focus on completion of the transplant evaluation, a crucial early step in the renal transplant process. Furthermore, this study is the first study that we are aware of that examines how an education program impacts access to renal transplant evaluation by examining levels of both individual- and neighborhood-level SES.
Previous research at our center suggests that racial disparities exist in the renal transplant process, where the rate of kidney transplantation among blacks is 59% lower compared with whites, even after accounting for individual- and neighborhood-level SES (3). In our study, white (vs. black) patients were significantly more likely to complete the evaluation process before the implementation of the educational intervention, but these disparities in evaluation completion were attenuated after the educational intervention. Prior studies have suggested that minorities have decreased access to transplant because of decreased awareness of transplantation and that disparities are alleviated among patients with higher education (19). One potential explanation for the increased evaluation completion that we observed among poor and black patients is that the formal patient educational session better informed patients about the transplant process through the group question and answer session, where all attendees and their family members could benefit from the tailored answers to patient questions about the transplant process. This finding may also explain why evaluation completion increased for all patients, regardless of race or SES level. Health literacy is also associated with access to transplant (20), and the emphasis on interactive patient education may be one reason why patients with lower SES saw an improvement in evaluation completion after the intervention at our center. An additional explanation may be that the formal education session indirectly improved evaluation completion. For example, the in-center class may have promoted an opportunity for patients to develop sustained relationships with other patients and members of the transplant team, thereby improving attendance at follow-up visits.
This study has several strengths. The racial distribution of our study (61% black) provides us with sufficient power to examine racial and socioeconomic differences in evaluation completion by intervention group. We assessed poverty by both individual- and group-level estimates of SES, which permitted the evaluation of poverty in a multilevel framework. Research suggests that, among area-based socioeconomic measures, census-tract level analyses yield the most consistent, robust, and sensitive results (21). National studies that examine access to transplant typically consider all dialysis patients as eligible for a renal transplant. However, not all patients are eligible for transplant because of medical comorbidities (22). Studies that examine disparities in transplant steps typically use waitlisting as a proxy for evaluation completion, but because United Network for Organ Sharing implemented a policy to allow patients to list before evaluation completion, assessing disparities in evaluation completion by using waitlisting as an endpoint may not provide a valid assessment. A strength of this study is the measurement of evaluation completion as a separate outcome from waitlisting, because we were particularly interested in understanding the patient-driven reasons for evaluation completion rather than medical reasons.
The limitations of this study must be noted. First, confounding is a methodological challenge for all observational studies. However, the underlying cohort of patients from pre- to postintervention groups was similar over time with respect to socioeconomic, demographic, and clinical characteristics, indicating that these factors are unlikely to be confounders of the association of the effect of the intervention on evaluation completion. Because this study compared two separate periods in time, controlling for temporal confounding is a methodological challenge. However, we assessed time trends and found that time period effects were not entirely responsible for the observed differences before and after implementation of the formal education program. Furthermore, the effect of the formal education program seems to have been sustained for 2 years after the intervention. Second, information on the reasons that a patient had incomplete evaluation requirements was unknown; prospective studies should aim to collect this information. Third, because the study population reflects the referral population of a single center, our findings may not be generalizable to other centers. Fourth, although we have several individual-level SES measures and a sensitive measure for neighborhood SES, these measures are unlikely to completely capture a patient’s poverty level.
In a diverse ESRD population in the southeastern United States, racial and socioeconomic disparities in evaluation completion were attenuated after the implementation of a required patient education program for patients referred for renal transplantation. Standardizing transplant education may help reduce inequity in access to renal transplantation in the southeastern United States. As a proof of concept study, these results may also give other transplant centers an idea of how to design and evaluate their own center’s educational programs. Because requirements for patient education vary by dialysis facility and transplant center, national surveillance systems should aim to collect information about patient educational programs to examine equitability in the renal transplant evaluation process and aid in developing recommendations for national guidelines for patient education in the kidney transplant process.
Acknowledgments
We thank Paul Eggers and Rebecca Zhang, MS, for assistance in US Renal Data System data acquisition.
A portion of this work was presented at the American Society of Nephrology 2011 Annual Meeting, Philadelphia, Pennsylvania, November 8–13, 2011.
Footnotes
Disclosures
None.
References
- 1.USRDS: US Renal Data System 2009 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States, Bethesda, MD, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2009 [Google Scholar]
- 2.Eggers PW: Racial disparities in access to transplantation: A tough nut to crack. Kidney Int 76: 589–590, 2009 [DOI] [PubMed] [Google Scholar]
- 3.Patzer RE, Perryman J, Schrager JS, Pastan S, Amaral SA, Kutner N, Klein M, Gazmararian J, McClellan WM: The role of race and poverty on steps to kidney transplantation in the southeastern United States. Am J Transplant 12: 358–368, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patzer RE, Amaral S, Wasse H, Volkova N, Kleinbaum D, McClellan WM: Neighborhood poverty and racial disparities in kidney transplant waitlisting. J Am Soc Nephrol 20: 1333–1340, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alexander GC, Sehgal AR: Why hemodialysis patients fail to complete the transplantation process. Am J Kidney Dis 37: 321–328, 2001 [DOI] [PubMed] [Google Scholar]
- 6.Hall YN, Choi AI, Xu P, O’Hare AM, Chertow GM: Racial ethnic differences in rates and determinants of deceased donor kidney transplantation. J Am Soc Nephrol 22: 743–751, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Klassen AC, Hall AG, Saksvig B, Curbow B, Klassen DK: Relationship between patients’ perceptions of disadvantage and discrimination and listing for kidney transplantation. AmJ Public Health 92: 811–817, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Weng FL, Joffe MM, Feldman HI, Mange KC: Rates of completion of the medical evaluation for renal transplantation. Am J Kidney Dis 46: 734–745, 2005 [DOI] [PubMed] [Google Scholar]
- 9.Schold JD, Gregg JA, Harman JS, Hall AG, Patton PR, Meier- Kriesche HU: Barriers to evaluation and wait listing for kidney transplantation. Clin J Am Soc Nephrol 6: 1 760–1767, 2011 [DOI] [PubMed] [Google Scholar]
- 10.Powe NR: To have and have not: Health and health care disparities in chronic kidney disease. Kidney Int 64: 763–772, 2003 [DOI] [PubMed] [Google Scholar]
- 11.Wolfe RA, Ashby VB, Milford EL, Bloembergen WE, Agodoa LY, Held PJ, Port FK: Differences in access to cadaveric renal transplantation in the United States. Am J Kidney Dis 36: 1025–1033, 2000 [DOI] [PubMed] [Google Scholar]
- 12.Navaneethan SD, Singh S: A systematic review of barriers in access to renal transplantation among African Americans in the United States. Clin Transplant 20: 769–775, 2006 [DOI] [PubMed] [Google Scholar]
- 13.Neyhart CD: Education of patients pre and post-transplant: Improving outcomes by overcoming the barriers. Nephrol NursJ 35: 409–410, 2008 [PubMed] [Google Scholar]
- 14.Waterman AD, Browne T, Waterman BM, Gladstone EH, Hostetter T: Attitudes and behaviors of African Americans regarding early detection of kidney disease. Am J Kidney Dis 51 : 554–562, 2008 [DOI] [PubMed] [Google Scholar]
- 15.Kucirka LM, Grams ME, Balhara KS, Jaar BG, Segev DL: Disparities in provision of transplant information affect access to kidney transplantation. Am J Transplant 12: 351–357, 2012 [DOI] [PubMed] [Google Scholar]
- 16.Kleinbaum DG, Klein M: Surival Analysis A Self-Learning Text, 2nd Ed., edited by Gail M, New York, Springer Science+Business Media, Inc., 2005 [Google Scholar]
- 17.Lin DY, Wei LJ: The robust inference for the Cox Proportional Hazards Model. J Am Stat Assoc 84: 1074–1078, 1989 [Google Scholar]
- 18.Kasiske BL, Cangro CB, Hariharan S, Hricik DE, Kerman RH, Roth D, Rush DN, Vazquez MA, Weir MR; American Society of Transplantation: The evaluation of renal transplantation candidates: Clinical practice guidelines. Am J Transplant 1 [Suppl 2]: 3–95, 2001 [PubMed] [Google Scholar]
- 19.Goldfarb-Rumyantzev AS, Sandhu GS, Baird B, Barenbaum A, Yoon JH, Dimitri N, Koford JK, Shihab F: Effect of education on racial disparities in access to kidney transplantation [published online ahead of print December27, 2010]. Clin Transplant doi: 10.1111/j.1399-0012.2010.01390.x [DOI] [PubMed] [Google Scholar]
- 20.Grubbs V, Gregorich SE, Perez-Stable EJ, Hsu CY: Health literacy and access to kidney transplantation. Clin J Am Soc Nephrol 4: 195–200, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Krieger N, Chen JT, Waterman PD, Soobader MJ, Subramanian SV, Carson R: Geocoding and monitoring of US socioeconomic inequalities in mortality and cancer incidence: Does the choice of area-based measure and geographic level matter? The Public Health Disparities Geocoding Project. AmJ Epidemiol 156:471–482, 2002 [DOI] [PubMed] [Google Scholar]
- 22.Ayanian JZ, Cleary PD, Weissman JS, Epstein AM: The effect of patients’ preferences on racial differences in access to renal transplantation. N Engl J Med 341: 1661–1669, 1999 [DOI] [PubMed] [Google Scholar]


