Abstract
The Global Trachoma Mapping Project (GTMP) is the largest infectious disease survey ever undertaken. With 60 partners, 2.6 million people were examined across 29 countries for the blinding neglected tropical disease (NTD) trachoma, establishing the prevalence of the disease globally. Such an achievement was only made possible by building a diverse worldwide consortium. This article examines that public–private consortium and attempts to highlight key factors in the success of its development and operation. Two critical factors in the project’s success were the establishment of an evidence-based common approach and urgency around a shared goal. The common approach (the GTMP methodologies, tools and training approach) and the goal (GET2020 through the SAFE strategy) are thoroughly detailed in this article. Transparency at all levels; clear roles for committees, partners, agencies and ministries of health and shared funding played important roles and are explored here. It is hoped that by examining and sharing the positive factors leading to the establishment and work of this specific consortium, other similar initiatives—for NTDs, for health more broadly and for other development areas—will be able to adopt such an approach for effective collaboration.
Keywords: collaboration, consortia, innovation, mapping, NTDs, trachoma
Introduction
Elimination of infectious diseases requires collaboration between many different stakeholders, as these efforts are too large for any single entity.1 The diversity of organizations working together towards such a goal can be seen as a great strength, combining a variety of skills, experiences and approaches. That diversity can also be seen as a weakness, creating confusion of roles, inefficiencies in process and planning, and competition for scarce resources. This article examines a successful public–private consortium developed to tackle an infectious blinding disease, trachoma, and attempts to highlight key success factors in the development and operation of that consortium.
The Global Trachoma Mapping Project (GTMP)—what the consortium accomplished
The World Health Organization (WHO) recognizes that a group of 17 diseases, known as the neglected tropical diseases (NTDs), represent a ‘serious impediment to poverty reduction and overall socioeconomic development’2 and must be addressed. Trachoma, one of these priority diseases, is the world’s leading infectious cause of blindness, caused by repeated infections of the conjunctiva with Chlamydia trachomatis. The disease is responsible for blindness or visual impairment in about 1.9 million people—and slightly more than 200 million people are at risk.3
The GTMP mapped the global prevalence of trachoma using a standardized, WHO-approved methodology in which house-to-house cluster random sample surveys were conducted.4 The prevalence of active trachoma (TF) and trachomatous trichiasis (TT) was determined, as well as information on access to water and sanitation. Survey teams examined people living in a sample of communities within pre-identified districts and captured data on smartphones. This was reviewed by data managers and approved by ministries of health, then was used to update national trachoma action plans and displayed publicly on the Global Atlas of Trachoma—an open access web-based tool for tracking the global burden of trachoma. The GTMP was delivered in collaboration with more than 60 partners working around the world. In all, 2.6 million people were examined across 1546 districts in 29 countries, representing a population of 224 million. More than 60 million data items were processed.
Background
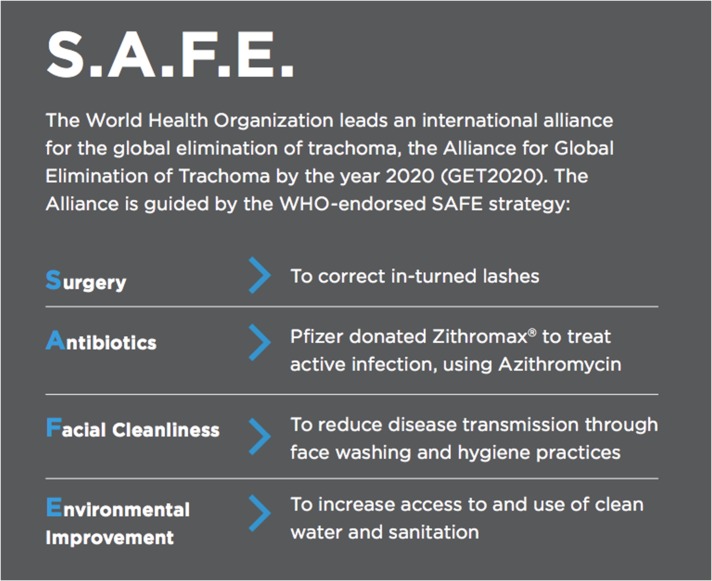
The strategy to eliminate blinding trachoma is the WHO-endorsed SAFE (Surgery for advanced disease, Antibiotics to clear C. trachomatis infection, Facial cleanliness and Environmental improvement to reduce transmission) strategy3 (Figure 1). Countries such as Cambodia, Ghana, Laos, Mexico, Morocco, Nepal, and Oman have already demonstrated that using the SAFE strategy can lead to elimination of trachoma as a public health problem.5
Figure 1.
WHO-endorsed SAFE strategy for the global elimination of trachoma.
The WHO set up the Global Elimination of Trachoma by 2020 (GET2020) project in 1996.6 The 2020 challenge required countries to plan in a different way and move away from a ‘business-as-usual’ approach. A template for national trachoma action plans was created to help countries develop their own roadmap to elimination. What was still missing was a global roadmap to ensure that overall progress towards global elimination was being tracked and to address issues of global significance, such as resourcing and evidence.
First steps
The establishment of two key organizations undoubtedly played a role in later successes. First, the International Trachoma Initiative (ITI) was founded in 1998. The ITI’s founding partners, Pfizer and the Edna McConnell Clark Foundation, saw the need for a non-governmental organization dedicated solely to the elimination of trachoma. The ITI was put in place to collaborate with governmental and non-governmental agencies at the local, national and international levels.
Second, the International Coalition for Trachoma Control (ICTC) was established in 2004 for the purpose of contributing to the global effort to eliminate trachoma. The ICTC is composed of non-governmental development organizations (NGDOs), academic institutions, donors, the private sector and foundations. The original purpose of the coalition was to ‘contribute to global efforts to eliminate trachoma by supporting the GET2020 Alliance and to advocate for and implement the WHO-endorsed SAFE strategy’.7
The ICTC is a member of the NTD NGDO network and forms part of a network of disease groups that bring together lymphatic filariasis, onchocerciasis, soil-transmitted helminths, schistosomiasis and leprosy. The first group to form was for onchocerciasis in 1992, the success of which inspired the formation of other groups such as that for trachoma.8 The ICTC itself, and the GTMP, have built on experiences from these other NTD networks9 and shares lessons with them.
In 2010, the ITI brought the trachoma community together to develop a global roadmap for trachoma. The 2020 INSight: the end in sight,10 identified an urgent need for action. Crucial steps included mapping disease prevalence, resource mobilization at the global and national levels and scaling up interventions through implementation of trachoma action plans in all endemic countries by 2015.
The result of the global roadmap development process was a community that was aligned around a common strategy and aware that the goal of trachoma elimination is achievable but will require hard work, and collaboration, between all partners.
The need
One of the major barriers identified by 2020 INSight to scaling up was the lack of knowledge on where and where not to implement programs. It was decided that the ITI would develop a plan to internationally standardize the trachoma mapping approach and create a roadmap to finish mapping. The ITI first set up a steering committee. To ensure broad engagement from the trachoma community and utilize all expertise available, several working groups were also established, focused on
Methodologies: to determine which assessment types would be utilized
Tools: to devise the most cost-effective means to undertake assessments and manage data
Training: to develop a training program and materials that could be rolled out quickly and effectively
Prioritization: to develop a plan of action for the order in which the estimated 1200 districts were to be mapped.
GTMP: a consortium in practice
Resourcing
Establishment of the steering committee ensured that a collaborative, rather than competitive, approach to raising and managing the resources required was followed. This approach was highly effective, avoided inefficient competitive tendering processes and enabled the UK’s Department for International Development (DFID) to agree to a grant of £10.6 million. The steering committee agreed that Sightsavers should undertake management of the DFID grant. As the lead agency, Sightsavers provided overall coordination and ensured the program progressed according to agreed timelines and that it operated within DFID’s grant conditions, while the ITI remained the secretariat of the steering committee and provided technical support. The grant allowed the ICTC partners to map trachoma wherever there was unmet need within a 2.5 y time period.
Delivery
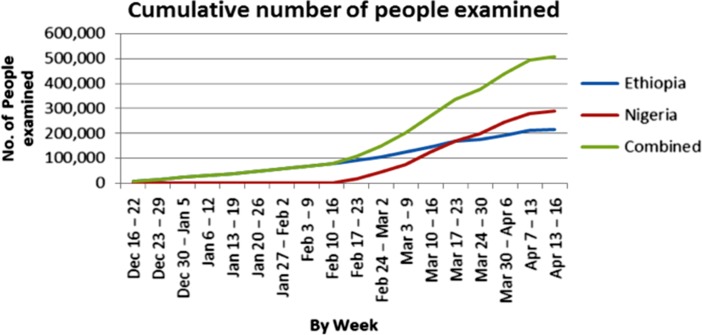
The emphasis in delivery was on quality of results and ability to scale up quickly (see Figure 2). This is where the consortium approach had huge advantages, as there was a range of partners with both a geographic reach and technical expertise. This also emphasizes the importance of central management and methodology; however, it should be noted that this is only effective if all those participating have the necessary skills, understanding and tools.
Figure 2.
Pace of scale-up. One million people were examined within the first 5 months alone.
Ministries of health
In line with the foundation of both the Sustainable Development Goals and the human rights framework—that nation states are the duty bearers in health and other areas of development—there was a central role for ministries of health, as project partners, in project planning, implementation and data ownership. There was early agreement on the collection, control and management of the survey data gathered. A key principle of the GTMP was that national ministries have sovereignty over their data, while still being able to provide quality control and analyses using an internationally standardized approach. These data were consistently put to use in national NTD master plans. Furthermore, at the operational level, it was overwhelmingly ministry of health staff who were involved in staffing the mapping teams. Teams consisted of a grader, who examined eyelids and graded them for signs of trachoma, a recorder, who captured the data on an Android-based smartphone, a driver, a local guide and a supervisor (Figure 3).
Figure 3.

Halima Suleiman does an eye examination in Nigeria while a recorder captures details.
Innovation
Lack of financial competition between organizations played in the consortium’s favor, increasing the appetite to adopt innovative approaches. This does not fit into the paradigm that competition always benefits development; however, the shared elimination goal and trusted methodology changed that dynamic. As stated earlier, this benefited the project in the bidding process. Another example was the consortium encouraging the ITI to develop a completely new data management system to support the mapping. Data were collected on Android smartphones, then transferred securely from the field to a central web-based reporting and data management system. This system allowed quick resolution of issues and an automated process to deliver results and approvals. This was the first time a system like this had been used on a global scale, reducing the time taken to process data and supporting quality improvement by resolving issues while the teams were still in the field. Data were then made available in-country through the country’s own health management information system. After approval from the national ministry of health, data were published through the open-access Trachoma Atlas (www.trachomaatlas.org), which shares population-based trachoma prevalence data at the district level to support advocacy and efficient allocation of resources.
Value for money
Cost efficiency was achieved by combining efforts across the consortium to reduce duplication and ensure that effective and low-cost approaches were used. The emphasis on standardization across training, mapping and data management and the introduction of an electronic data capture system enabled a fast and efficient scale-up supported by relatively few staff. That shared methodology also allowed the project to compare survey microplanning across countries to find outliers and share lessons.
Each mapping budget was linked very closely to the planned district outputs. Inputs from the chief scientist and project epidemiologists ensured that the appropriate sampling methodology for the area concerned was properly reflected in budgets (e.g. a widespread district may require more days per cluster to map). An example of the effectiveness of the budget review, query and approval process is that the first Oromia mapping budget in Ethiopia was successfully reduced by 28% from that originally submitted by the partner.
Finally, an online portal for submission, approval and consolidation/reporting of GTMP agreements, budgets and claims was developed by Sightsavers. This provided a robust audit trail and facilitated ongoing tracking of key unit costs from across the range of partners. Unit costs have been analyzed in a study examining in-country expenditures, which also highlights variations in costs based on geographic, demographic and seasonal effects. This is an effort to help plan future trachoma surveys and other disease mapping programs11.
Risks
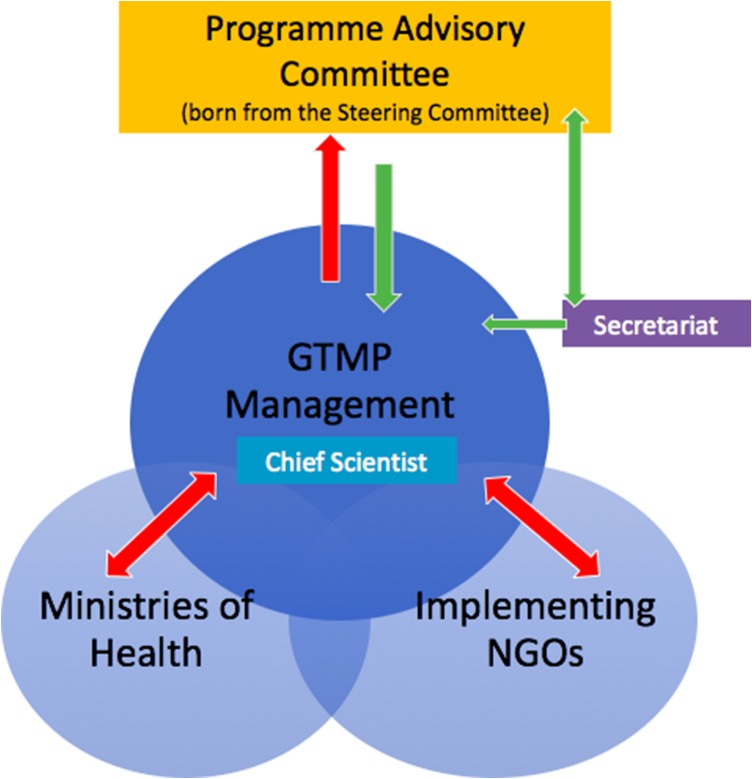
There are a number of risks inherent with a large consortium, the most obvious one being difficulty in managing different interests and making far-reaching decisions. This risk was mitigated successfully with the clear management structure and effective operation of a program advisory committee (born from the original steering committee). The GTMP management structure delineated grant management, program management and mapping implementation responsibilities across the consortium; the program advisory committee, comprised of the major stakeholders, advised the core delivery team on programmatic and operational issues. The committee met three to four times a year throughout the project, where possible in conjunction with other international gatherings (Figure 4).
Figure 4.
Advising and reporting within the consortium.
Large consortia can also experience difficulty in aligning approaches across all actors in a multiactor environment. In practice this has been an area of strength. The GTMP tools and methodologies are now being used on other trachoma mapping activities outside the scope of this project. The expected result of using this ‘gold standard’ is high-quality mapping and rapid availability of the resulting data.
Finally, at the country level, the program had one coordinating NGDO responsible for overall coordination of implementing the partners’ activities and for relationships with the national ministry of health. This provided an element of shared risk across the global program.
Success factors
This discussion focused on the critical success factors identified as the consortium developed. The GTMP meant a shift from bodies (ITI, ICTC) coordinating research, advocacy and resource mobilization to fully coordinated complex developmental interventions with multiple stakeholders in multiple countries. This shift has further clarified the success factors that needed to be in place in advance for this project to have progressed as it did.
Interlinked primary success factors
Arguably the two most critical factors in the bringing together of so many partners into one consortium was the establishment of an evidence-based common approach and urgency around a shared goal. The common approach (the GTMP methodologies, tools and training approach) and the goal (GET2020 through the SAFE strategy) were detailed earlier in the article. However, we argue that it is the combination of these two that is crucial. Both are necessary, but insufficient on their own. To cite a contrasting example, many of the agencies involved in the consortium overlap in other areas of their work, including several other NTDs,12 broader eye health programs and disability. Although there are coordination processes and joint programs in several of these sectors, none has brought together the global community of practice for a global implementation program in the same way as the trachoma consortium. They often have a common goal (e.g. in disability, to end discrimination against disabled people, or in Vision 2020, to eliminate avoidable blindness by 2020). They may also have some broad agreement over the issues involved and areas of priority (e.g. Vision 2020’s list of key diseases). However, they do not share a common approach and often use different evidence and experiences to guide program design. As a result, collaborative advocacy tends to be at a much higher level (‘including disabled people is important’ or ‘eye health is an essential component of an effective health system’), the use of the evidence base tends to be selective and individual rather than summative and agreed, and collaboration tends to involve a series of more or less similar projects in separate geographic or thematic areas rather than a single coherent program with many actors involved.
Secondary success factors
There are several secondary success factors involved. These are vital and necessary to the success of the consortium, although it can be argued that they have largely grown from the first two.
A history of research and advocacy collaboration. The early establishment of relationships and a common purpose was key. Because of this early collaboration, there was less risk of ill feelings between consortium members, as none had joined after resources had been fought for and won or as the profile of activities rose. There is a genuine understanding that the progress made was owned jointly rather than by one or two key individuals or organizations—although obviously there are also examples where individuals have made particular and outstanding contributions.
Overall transparency and a clear leadership role for the ITI, which had no conflict of interest. It is important to note that the ITI shifted most of its strategic focus to Zithromax donations, and their use of a clear approach and evidence base to make decisions on whether programs qualify for drug donation or not was key. This structure reduced the potential for complaints of partiality in access to resources. The early establishment of structure and communications between the steering committee and the core project team was also key. However, the later transition of the original steering committee to a GTMP program advisory group could have involved clearer communication to all parties. This shift was part of the necessary evolution of the project—the steering committee, which played an essential role in structuring the project, was transitioned to a program advisory group, which needed to play additional roles as the project was implemented, including technical support, advocacy, monitoring and learning. This is a lesson that shifting structures—even when those shifts benefit the project—require transparency and clear communication to avoid frustration over unclear roles and responsibilities.
A clear lead agency for the funding bids for the program—Sightsavers—with the unanimous support from all partners for this role. As Sightsavers had both an established prior funding relationship at a strategic level with the DFID and was also headquartered in the UK, relationships between the donor and the consortium were easier to maintain and this facilitated the donor’s sense of ongoing engagement with the program through both set quarterly reviews and more frequent needs-based meetings.
A clearly established final arbiter in scientific, knowledge and methodological debates. From the beginning of the GTMP, a scientist who started at the London School of Hygiene and Tropical Medicine and later moved to the World Health Organization was chosen by the consortium as the final decision maker. This ensured that NGOs and ministries of health felt treated equally and left little room for second guessing.
A process for establishing various agencies in-country to share the work enabled all agencies to be as engaged as they were able—neither giving all the mapping resources and responsibilities to one agency per country and leaving others out, nor making demands of agencies unable to deliver in the time required with the resources available. This has inevitably led to some agencies taking on larger workloads than others but, with agencies working toward a common goal, this was not contentious. Interestingly, this transparency combined with the shared goal led to agencies occasionally sharing resources; NGOs supported each other locally by sharing office space and technical resources when needed.
Work after the GTMP
Tropical Data—extending the legacy of the GTMP
The GTMP came to an end late in 2015, but an initiative called Tropical Data has been created by those behind it to extend the prevalence mapping to other survey needs countries have on their path to elimination. Baseline, impact, surveillance and TT-only surveys are available through the service. Lessons learned from the GTMP on the importance of standardized methodologies, clear scientific arbitration and shared goals were key in creating the service, though the model is slightly different. Unlike with the GTMP, national programs are responsible for the delivery and funding of in-country implementation, including project planning, training, field work and results. Tropical Data still provides support, including epidemiology, trainers, survey tools, technical guidelines, scientific oversight, data processing and data reviews. Tropical Data has benefited enormously from the acceptance and appreciation of the GTMP’s methods and success.
SAFE: The consortium to 2020
Although this article has focused on the delivery of the GTMP, this is only one aspect of the consortium’s current work. The same consortium, under the ICTC’s auspices, has worked together to secure bids for enormous upscaling in the global delivery of the SAFE strategy, with funds provided by the US Agency for International Development, AusAid, the DFID and the Queen Elizabeth Diamond Jubilee Trust. These are more complex programs than the GTMP, arguably larger in both scope and certainly in scale. They will inevitably add pressures to the consortium and further lessons will undoubtedly be learned.
Current work and plans (confirmation of continued strength in the consortium) are outlined in last year’s Eliminating Trachoma: Accelerating Towards 2020 document.13
Conclusions
The trachoma consortium has so far proved to be an excellent example of how multiple actors can work together to achieve concrete social goals. Now that this vehicle has been established, and as further resources become available, progress is being made with ever-greater efficiency towards the eventual goal of the elimination of trachoma as a public health problem by 2020.
That in itself would be a huge achievement. We also believe this can be the first in a discussion on how to establish a serviceable framework for success. By examining and sharing the positive factors leading to the establishment and operation of this specific consortium, other similar initiatives—for NTDs, for health more broadly and for other development areas—will be able to adopt this approach for effective collaboration.
Acknowledgments
Authors’ contributions: DH, SB and DH conceived of the paper. SB joined as the lead writer. All authors read and approved the final manuscript.
Acknowledgements: Thank you to the over 60 partners who made the GTMP a success, and to both DFID and USAID for supporting the project.
Funding: None.
Competing interests: None declared.
Ethical approval: Not required.
References
- 1. Foege WH. House on fire: the fight to eradicate smallpox. Berkeley: University of California Press, 2011. [Google Scholar]
- 2. World Health Organization Neglected tropical diseases. http://www.who.int/neglected_diseases/about/en/ (accessed 11 January 2018).
- 3. World Health Organization Trachoma. http://www.who.int/mediacentre/factsheets/fs382/en/ (accessed 11 January 2018).
- 4. Solomon AW, Pavluck AL, Courtright P et al. The Global Trachoma Mapping Project: methodology of a 34-country population-based study. Ophthalmic Epidemiol 2015;22(3):214–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. World Health Organization Morocco defeats trachoma. http://www.who.int/neglected_diseases/news/Morocco_defeats_trachoma/en/ (accessed 11 January 2018).
- 6. World Health Organization Prevention of blindness and visual impairment. http://www.who.int/blindness/causes/trachoma/en/index.html (accessed 11 January 2018).
- 7. International Coalition for Trachoma Control ICTC strategic plan 2015–2020. http://www.trachomacoalition.org/sites/default/files/ICTC-strategic-plan-2015-2020-FINAL.pdf (accessed 11 January 2018).
- 8. Bush S, Hopkins AD. Public-private partnerships in neglected tropical disease control: the role of non-governmental organisations. Acta Trop 2011;120(Suppl 10):S169–72. [DOI] [PubMed] [Google Scholar]
- 9. Haddad D, Cross C, Thylefors B et al. Health care at the end of the road: opportunities from 20 years of partnership in onchocerciasis control. Glob Public Health 2008;3(2):187–96. [DOI] [PubMed] [Google Scholar]
- 10.International Coalition for Trachoma Control. The end in sight: 2020 InSight http://www.trachomacoalition.org/sites/default/files/content/resources/files/ICTC_EnglishJuly21lowres.pdf (accessed 11 January 2018).
- 11. Trotignon G, Jones E, Engels T et al. The cost of mapping trachoma: data from the Global Trachoma Mapping Project. PLoS Negl Trop Dis 2017;11(10):e0006023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Neglected Tropical Disease NGDO Network http://www.ntd-ngdonetwork.org/ (accessed 11 January 2018).
- 13.WHO Alliance for the Global Elimination of Trachoma by 2020. Eliminating trachoma: accelerating towards 2020 http://www.trachomacoalition.org/GET2020/ (accessed 11 January 2018).