Abstract
We recently reported the clinical results of a Phase I trial combining ipilimumab with a vaccine containing transgenes for prostate-specific antigen (PSA) and for a triad of costimulatory molecules (PROSTVAC) in patients with metastatic castration-resistant prostate cancer. Thirty patients were treated with escalating ipilimumab and a fixed dose of vaccine. Of 24 chemotherapy-naïve patients, 58 % had a PSA decline. Combination therapy did not exacerbate the immune-related adverse events associated with ipilimumab. Here, we present updated survival data and an evaluation of 36 immune cell subsets pre- and post-therapy. Peripheral blood mononuclear cells were collected before therapy, at 13 days and at 70 days post-initiation of therapy, and phenotyped by flow cytometry for the subsets of T cells, regulatory T cells, natural killer cells, and myeloid-derived suppressor cells. Associations between overall survival (OS) and immune cell subsets prior to treatment, and the change in a given immune cell subset 70 days post-initiation of therapy, were evaluated. The median OS was 2.63 years (1.77–3.45). There were trends toward associations for longer OS and certain immune cell subsets before immunotherapy: lower PD-1+Tim-3NEGCD4EM (P = 0.005, adjusted P = 0.010), higher PD-1NEGTim-3+CD8 (P = 0.002, adjusted P = 0.004), and a higher number of CTLA-4NEG Tregs (P = 0.005, adjusted P = 0.010). We also found that an increase in Tim-3+ natural killer cells post- versus pre-vaccination associated with longer OS (P = 0.0074, adjusted P = 0.015). These results should be considered as hypothesis generating and should be further evaluated in larger immunotherapy trials.
Keywords: Ipilimumab, Vaccine, PROSTVAC, T cells, NK cells, Immunotherapy
Introduction
Two immunotherapeutic agents for cancer have recently been approved by the Food and Drug Administration (FDA): sipuleucel-T for prostate cancer and ipilimumab for metastatic melanoma. Sipuleucel-T (PROVENGE®, Dendreon Corp.) is a therapeutic vaccine generated by the isolation of the patient’s peripheral blood mononuclear cells (PBMCs) and culturing them in vitro with a fusion protein of prostatic acid phosphatase (PAP) and granulocyte–macrophage colony-stimulating factor (GM-CSF). The product is then reinfused into the patient. The Phase III IMPACT trial showed a 4.1-month improvement in overall survival (OS) and a 22 % relative reduction in risk of death, and it was approved for use in prostate cancer in 2010 [1].
Another vaccine, designated as PROSTVAC, has shown evidence of clinical activity in metastatic prostate cancer in two Phase II trials [2, 3], and a Phase III trial is currently ongoing (NCT01322490 [4]). PROSTVAC (PSA–TRICOM, Bavarian Nordic, Inc.) consists of a prime–boost regimen with recombinant vaccinia (prime) and fowlpox (boost) vectors, containing transgenes for prostate-specific antigen (PSA) and three costimulatory molecules for cytotoxic T lymphocytes (B7.1, ICAM-1, and LFA-3, designated TRICOM) [5]. A multicenter, randomized, placebo-controlled Phase II study showed an 8.5-month improvement in overall survival and a 44 % reduction in death rate compared to placebo in patients with asymptomatic or minimally symptomatic metastatic castration-resistant prostate cancer (mCRPC) [2]. The median OS was 25.1 months for vaccinated patients (n = 82) versus 16.6 months for controls (n = 40). In a second Phase II single-arm trial in mCRPC at the National Cancer Institute (NCI), the median survival was 26.6 months (n = 32) [3]. A retrospective analysis of this trial evaluated patients based on the Halabi nomogram [6] and found that patients with a more indolent disease (predicted survival >18 months) displayed greater improvements in survival than patients with more aggressive disease. PROSTVAC vaccination was also shown to generate an antigen-specific immune response [3]. In addition, it was shown that patients who had a decrease in the cytotoxic T-lymphocyte-associated antigen-4 (CTLA-4)+ regulatory T-cell (Treg) population post-vaccination displayed longer overall survival [7].
Ipilimumab (Yervoy®, Bristol-Myers Squibb) is a fully human monoclonal antibody that targets CTLA-4. It is the first in a new class of agents called immune checkpoint inhibitors. It has been extensively studied in metastatic melanoma and has shown an improvement of overall survival of 2–4 months compared to active control groups, which led to FDA approval [8, 9]. Ipilimumab has also previously been investigated for the treatment for prostate cancer in a pilot trial of patients with hormone-refractory prostate cancer [10]. They found a PSA decline of ≥50 % in 2/14 patients and concluded that further investigations were warranted. Ipilimumab alone or in combination with radiotherapy was also investigated in a recently reported Phase I/II trial of 75 patients with mCRPC [11]. Both PSA decline and tumor response were observed, and 8/34 patients in the 10 mg/kg ± radiotherapy group had a confirmed PSA decline of ≥50 %. Of these, six had received prior chemotherapy and two were chemotherapy-naïve. One of the tumor-evaluable patients in the 10 mg/kg ± radiotherapy group achieved a confirmed complete response, and 2 patients achieved an unconfirmed partial response. Six patients had stable disease. The median OS was 17.4 months [11].
In the PSA–TRICOM trials, no adverse events above grade 1 or 2 toxicity and no evidence of autoimmunity were observed. In the ipilimumab trials, there were some severe adverse events involving autoimmunity, including colitis, panhypophysitis, adrenal insufficiency, raised aminotransferases, and neutropenia. Since PSA–TRICOM has three costimulatory molecules designed to enhance T-cell immunity, and the ipilimumab checkpoint inhibitor is designed to reduce the immune suppressive CTLA-4 entity, it was important to determine whether the combination of PSA–TRICOM and ipilimumab would exacerbate the autoimmunity seen with ipilimumab alone.
We have recently reported [12] the clinical results of a Phase I study combining ipilimumab with PSA–TRICOM vaccine in patients with mCRPC. Thirty patients were treated with an escalating dose of ipilimumab and a fixed dose of vaccine. Of the 24 chemotherapy-naïve patients, 14 patients (58 %) had a PSA decline from baseline, with six of these ≥50 %. Combination therapy did not seem to exacerbate the immune-related adverse events associated with ipilimumab, and there was no apparent association between immune-related adverse events and clinical outcome. In the present study, we report on updated survival data, which was evaluated in terms of several patient characteristics such as Gleason score and Halabi nomogram. Here, we have also investigated whether any of 36 specific immune cell subsets of patients prior to therapy correlate with clinical outcome and whether changes in any of these subsets during therapy correlate with survival. For each of these immune cell subsets, we have analyzed phenotypes based on known immunologic markers, many of which have previously been shown to correlate with biologic activity [7, 13–19].
Materials and methods
Patients
Thirty patients with mCRPC were enrolled on a Phase I trial of combination therapy with ipilimumab and PROSTVAC, a poxviral vaccine targeting PSA and containing transgenes for three T-cell costimulatory molecules (NCT00113984) [12, 20]. Recombinant vaccinia PROSTVAC was given as a prime with recombinant fowlpox PROSTVAC given as monthly boosts starting on day 15. GM-CSF was given on 4 consecutive days with each vaccination. Ipilimumab was given at the dose levels of 1, 3, 5, and 10 mg/kg. Ipilimumab treatment was started after 2 weeks, at the time of the first boost vaccination, and given monthly on the same day as vaccine. Initially, our protocol allowed for only six courses with ipilimumab; however, a protocol amendment gave patients with stable disease the option of additional ipilimumab every 3 months for a maximum of four additional doses. The maintenance dose of monthly vaccine could continue until there was evidence of disease progression on imaging studies, or toxic effects that required discontinuation. All injections were given at the NIH Clinical Center (Bethesda, MD, USA). All patients reviewed and signed an informed consent form approved by the NCI’s Institutional Review Board.
Collection of peripheral blood mononuclear cells
Peripheral blood mononuclear cells were collected at baseline, after 13 days and after approximately 70 days of treatment. Briefly, 60 ml of blood was collected, and the mononuclear fraction was separated by Ficoll–Hypaque density gradient separation, washed three times, and preserved in 90 % heat-inactivated human AB serum (Gemini Bio-Products, W Sacramento, CA, USA) and 10 % DMSO in liquid nitrogen at a concentration of 1 × 107 cells/ml until assayed.
Flow cytometry
Multi-color flow cytometry analysis was performed on PBMCs from all time points by staining for 30 min at 4 °C with CD3-V450, CD8-FITC or APC, ICOS-PE, HLA-DR-PerCP-Cy5.5, CD25-PE-Cy7, CD45RA-PerCP-Cy5.5, CD62L-FITC, CD127-V450, PD-1-PE, Tim-3-AF700, CD4-APC-Cy7 (BD Biosciences, San Jose, CA, USA), CCR7-PE-Cy7 (R&D Systems, Minneapolis, MN, USA), CTLA-4-FITC (LSBio, Seattle, WA, USA), and FoxP3-APC (eBioscience, San Diego, CA, USA) for T cells. For natural killer (NK) cells, CD3-V450, CD16-APC-Cy7, CD56-PE-Cy7, and Tim-3-AF700 (BD) were used. For myeloid-derived suppressor cells (MDSCs), CD33-PE, CD11b-APC-Cy7, HLA-DR-PerCP-Cy5.5, CD14-V450, and CD15-APC (BD) were used. 1 × 105 cells were acquired on an LSRII (BD), and data were analyzed using FlowJo software (Tree Star Inc., Ashland, OR, USA). The appropriate isotype controls were used, and dead cells were excluded from the analysis.
Induction and analysis of TH17 cells
TH17 cells were analyzed using the Human TH1/TH17 Phenotyping kit (BD). Briefly, PBMCs were thawed and incubated overnight at 37 °C. 1 × 106 cells/ml were stimulated for 5 h with PMA/Ionomycin in the presence of GolgiStop (Leukocyte Activation Cocktail with BD GolgiPlug, BD). The cells were then fixed, permeabilized, and stained according to the manufacturer’s instructions. CD4-PerCP-Cy5.5, interleukin (IL)-17A-PE, and interferon (IFN)γ-FITC (BD) were used. 1 × 105 cells were acquired on an LSRII (BD), and data were analyzed using FACSDiva software (BD). The appropriate isotype controls were used, and dead cells were excluded from the analysis.
Statistical analysis
In an exploratory manner, an actuarial analysis was performed on overall survival using the Kaplan–Meier method. OS was calculated as the period between the on-study date and date of death, or last follow-up. The log-rank test was used to compare strata or test for a trend (where appropriate). For both immune cell parameters and clinical parameters, baseline values were used to create strata for use in the actuarial analysis. For immune cell parameters, the percent difference from baseline (day 70–day 0) data was also used to create strata. The cutoffs were selected post hoc. Based upon the number of subjects available, the data were divided in tertiles to perform an exploratory evaluation of the association between the parameters and OS. For those parameters in which the log-rank P < 0.10, adjacent strata were combined and the two new strata with the smallest P value were used (in which case the log-rank test P value was adjusted for the implicit number of tests performed). Subsequently, a Cox proportional hazards regression analysis was performed on the data. The initial regression model included parameters from the actuarial analysis such that the log-rank P < 0.05. Both stepwise and backward selection processes were performed on the data.
Either a parametric or nonparametric analysis was performed on the immunological data, as appropriate. A repeated measures analysis of variance (ANOVA) was performed on the data if the ANOVA assumptions were satisfied. A Box–Cox transformation was performed on the data prior to ANOVA, and the data were transformed as appropriate. We also tested for linear and curvilinear trends over time using orthogonal polynomial contrasts. Residuals were examined for normality to verify ANOVA assumptions. If ANOVA was not appropriate for the data, we first used Friedman’s test and then used the Wilcoxon signed rank test to make pairwise comparisons between distributions of time periods. For both methods, all three pairwise comparisons were made and the P values were adjusted using Holm’s method (step down Bonferroni). In view of the very large number of tests performed on the survival and immunological data, we consider P < 0.005 as being statistically significant, while 0.005 < P < 0.05 would be considered trends. All reported P values are two-tailed.
Results
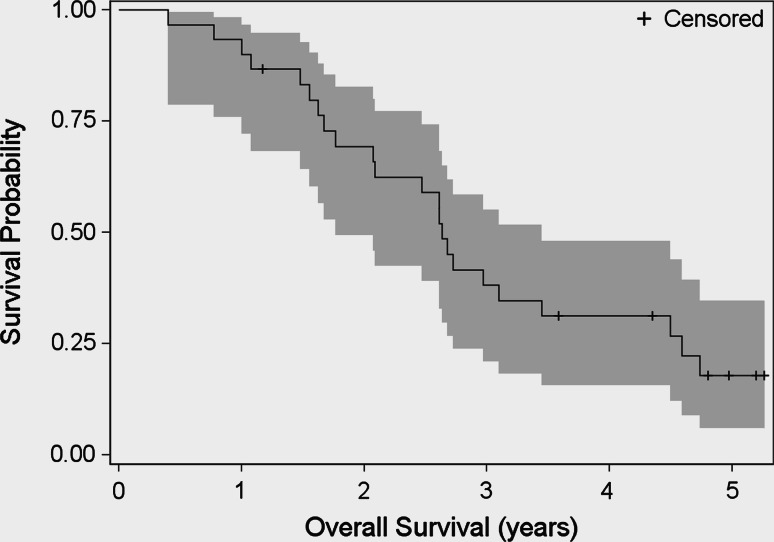
Overall survival of all 30 patients has been updated from the previous publication [12] and was calculated as the difference between the on-study date and the date of death (n = 23), or the date of last follow-up (n = 7). Figure 1 shows the Kaplan–Meier plot for overall survival for all patients. The median survival time was 2.63 years (95 % confidence limits 1.77–3.45). Probability of survival (95 % confidence limits) at 1, 2, and 3 years was 0.93 (0.76–0.98), 0.69 (0.49–0.83), and 0.38 (0.21–0.55), respectively.
Fig. 1.
Overall survival. Kaplan–Meier curve for overall survival in years for all patients (n = 30), calculated as the difference between the on-study date and the date of death (n = 23), or the date of last follow-up (n = 7). The median survival time was 2.63 years (95 % confidence limits 1.77–3.45). Probability of survival (95 % confidence limits) at 1, 2, and 3 years was 0.93 (0.76–0.98), 0.69 (0.49–0.83), and 0.38 (0.21–0.55), respectively
We performed an actuarial analysis of overall survival on the clinical characteristics data. As can be seen in Table 1, there were trends favoring a low Halabi score <117, which corresponds to a Halabi predicted survival of greater than approximately 18 months, a longer PSA-doubling time (DT) at baseline >2.42 months, and a baseline hemoglobin >12.4 g/dl. These results have previously been reported to be prognostic favorable factors [6, 21]. No other clinical variables were found to associate significantly with overall survival.
Table 1.
Risk analysis for clinical parameters versus overall survival
| Log rank | Trend | Favored | |
|---|---|---|---|
| Halabi score | 0.070 | 0.063 | <117 |
| Gleason score | 0.024 | 0.42 | None |
| Baseline PSA | 0.28 | 0.69 | None |
| Off study PSA | 0.46 | 0.61 | None |
| PSA–DT (months) | 0.023 | 0.015 | >2.42 |
| Baseline hemoglobin | 0.061 | 0.029 | >12.4 |
Actuarial analysis results after dichotomizing the data for clinical characteristics showing the log-rank and trend test P values, as well as the favored group
PSA–DT prostate-specific antigen-doubling time
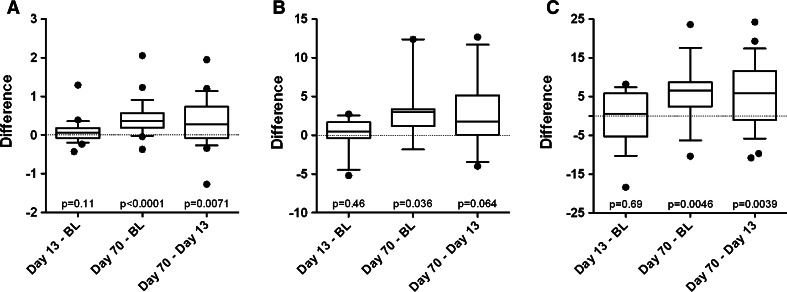
Using seven-color flow cytometry, we have now evaluated the subsets of CD4, CD8, NK, Tregs, TH17 cells, and MDSC at three time points: pre-treatment, day 13 (post-first vaccine and pre-ipilimumab), and day 70 (during vaccine/ipilimumab treatment). For each of these immune cell subsets, we have analyzed phenotypes based on known immunologic markers, some of which have previously been shown to correlate with a specific biologic activity [7, 13–19]. The description of each of these 36 subsets is given in Table 2. Figure 2 shows the three immune cell subsets that increased during therapy. For the three parameters shown, the differences between baseline (BL) and day 70, and day 13 and day 70, were generally significantly larger than zero, that is, the day 70 values were significantly larger than the baseline and day 13 values. Linear trends tests confirmed these findings for absolute lymphocyte count (ALC) (P < 0.0001) (Fig. 2A), ICOS+ CD4+ T cells (P < 0.0080) (Fig. 2B), and IFNγ+ CD4+ T cells (P < 0.0006) (Fig. 2C). The significance of these immune cell subsets will be further discussed. All other studied immune cell subsets shown in Table 2 did not change significantly from baseline to day 13 or day 70 of treatment, or from day 13 to 70.
Table 2.
Immune cell subsets
| Immune cell | Meaning |
|---|---|
| ALC | Absolute lymphocyte count |
| CD4 | T helper cells |
| CD4CM | Central memory T helper cells (CD4+CD45RANEGCD62L+CCR7+) |
| PD-1+ TIM-3NEG CD4CM | Activated central memory CD4 T cells, negative immune regulator |
| PD-1NEG TIM-3+ CD4CM | Activated central memory CD4 T cells, negative immune regulator |
| PD-1+ TIM-3+ CD4CM | Severe exhaustion of central memory CD4 T cells |
| CD4EM | Effector memory T helper cells (CD4+CD45RANEGCD62LNEGCCR7NEG) |
| PD-1 + TIM-3 NEG CD4 EM | Activated effector memory CD4 T cells, negative immune regulator |
| PD-1NEG TIM-3+ CD4EM | Exhausted effector memory CD4 T cells, negative immune regulator |
| PD-1+ TIM-3+ CD4EM | Severe exhaustion of effector memory CD4 T cells |
| ICOS+ CD4 | Activated T helper cells |
| IFNγ+ CD4 | Activated T helper cells |
| TH17 | T helper cell type 17, unclear role in cancer |
| IFNγ+ TH17 | More activated T helper cell type 17 |
| CD8 | Cytotoxic T cells |
| PD-1 NEG TIM-3 + CD8 | Activated CD8 T cells, negative immune regulator |
| CD8CM | Central memory cytotoxic T cells (CD8+CD45RANEGCD62L+CCR7+) |
| PD-1+ TIM-3NEG CD8CM | Activated central memory CD8 T cells, negative immune regulator |
| PD-1NEG TIM-3+ CD8CM | Activated central memory CD8 T cells, negative immune regulator |
| PD-1+ TIM-3+ CD8CM | Severe exhaustion of central memory cytotoxic T cells |
| CD8EM | Effector memory CD8 T cells (CD8+CD45RANEGCD62LNEGCCR7NEG) |
| PD-1+ TIM-3NEG CD8EM | Activated effector memory CD8 T cells, negative immune regulator |
| PD-1NEG TIM-3+ CD8EM | Activated effector memory CD8 T cells, negative immune regulator |
| PD-1+ TIM-3+ CD8EM | Severe exhaustion of effector memory cytotoxic T cells |
| ICOS+ CD8 | Activated cytotoxic T cells |
| TREGS | Regulatory T cells (CD4 + CD25 HI FoxP3 + CD127 NEG ) |
| CD4 : TREG RATIO | Ratio of effector T cells to regulatory T cells |
| CD8 : TREG RATIO | Ratio of effector T cells to regulatory T cells |
| NK CELLS | Natural killer cells (CD3NEGCD56+) |
| CD16+CD56BR | Functional intermediate, lytic, and cytokine production |
| TIM-3+ CD16+CD56BR | Fully functional intermediate |
| CD16+CD56DIM | Mature, more cytokine production |
| TIM-3+ CD16+CD56DIM | Fully functional mature |
| CD16NEGCD56BR | Immature, more lytic |
| TIM-3 + CD16 NEG CD56 BR | Immature NK cells transitioning into more mature (CD16 + CD56 DIM ) phenotype |
| MDSC | Myeloid-derived suppressor cells (HLA-DRNEGCD33+CD11b+) |
| MDSCMO | Monocytic MDSC (CD14+CD15NEG) |
| MDSCGR | Granulocytic MDSC (CD14NEGCD15+) |
| MDSCLIN- | Non-lineage MDSC (CD14NEGCD15NEG) |
| MARKERS | |
| CTLA-4 | Cytotoxic T-lymphocyte-associated antigen-4 |
| ICOS |
Inducible costimulator Costimulatory for the activation of T cells |
| PD-1 |
Programmed death 1 receptor On activated T cells and B cells, and on mature dendritic cells. Negative immune regulator, engagement with PD-L1, can downregulate T-cell activation. |
| TIM-3 |
T-cell immunoglobulin and mucin domain-containing molecule-3 Activation and maturation marker, and negative regulator of NK cells. Negative immune regulator expressed on T cells. |
These 36 different immune cell subsets were analyzed by flow cytometry at baseline, day 13 and day 70, as described in “Materials and methods.” Subsets shown in bold were associated with overall survival in subsequent analyses. One parameter, PD-1+ TIM-3NEG CD8CM, was not analyzed because many values were zero
Fig. 2.
Analysis of immune cell subsets pre-therapy and during therapy. Thirty patients with metastatic castration-resistant prostate cancer were treated with an increasing dose (1, 3, 5, or 10 mg/kg) of ipilimumab in combination with PROSTVAC vaccine and GM-CSF. Peripheral blood mononuclear cells (PBMCs) were collected at baseline, day 13, and day 70 and analyzed by flow cytometry. a There was a trend for increase in the absolute lymphocyte count (ALC) during therapy (n = 27–29). b There was a trend for increase in the frequency of ICOS+ CD4+ T cells during therapy (baseline: n = 12, day 13: n = 16, day 70: n = 14). c There was a trend for increase in the frequency of IFNγ+ CD4+ T cells during therapy (n = 19–29). For the three parameters shown, the differences between baseline (BL) and day 70, and day 13 and day 70, were generally significantly larger than zero, that is, the day 70 values were significantly larger than the baseline and day 13 values. Linear trends tests confirmed these findings. The box plots display the differences for each pairwise comparison between the time points, from baseline to day 13 or day 70 of treatment, or from day 13 to day 70. BL baseline
Analyses of clinical and immune cell subset baseline values were performed, as well as differences from baseline of the immune cell subsets, to evaluate whether any association existed with subsequent overall survival (Table 3). PBMCs were not available for flow cytometry analysis for 2 out of the 30 patients, so they were excluded from these comparisons.
Table 3.
Cox model results for specific immune cell subsets versus overall survival
| Parametera | Parameter levelsb | P value | Hazard ratio | 95 % confidence limits |
|---|---|---|---|---|
| Baseline % PD1+ of CD4EM | <4.77 versus >4.77 | 0.026 | 3.17 | 1.15–8.75 |
| Baseline number of Tregs | <98 versus >98 | 0.0013 | 0.153 | 0.049–0.481 |
| Baseline % Tim-3+ of CD8 | <40.9 versus >40.9 | 0.002 | 0.155 | 0.047–0.505 |
| % PD-1+ of CD8EM | <50 versus >50 | 0.027 | 3.03 | 1.33–8.07 |
| % Tim-3+ of CD16NEGCD56BR | <57.8 versus >57.8 | 0.055 | 0.283 | 0.078–1.029 |
| Baseline hemoglobin | <12.4 versus >12.4 | 0.011 | 0.271 | 0.100–0.739 |
aThe first three laboratory parameters are baseline values and were included in an analysis of clinical and immune cell subset baseline values, as well as differences from baseline of the immune cell subsets. The other laboratory parameters are percent differences from baseline, and this analysis was based solely on the differences between baseline and the clinical baseline variables
bThe first level indicated is the reference level
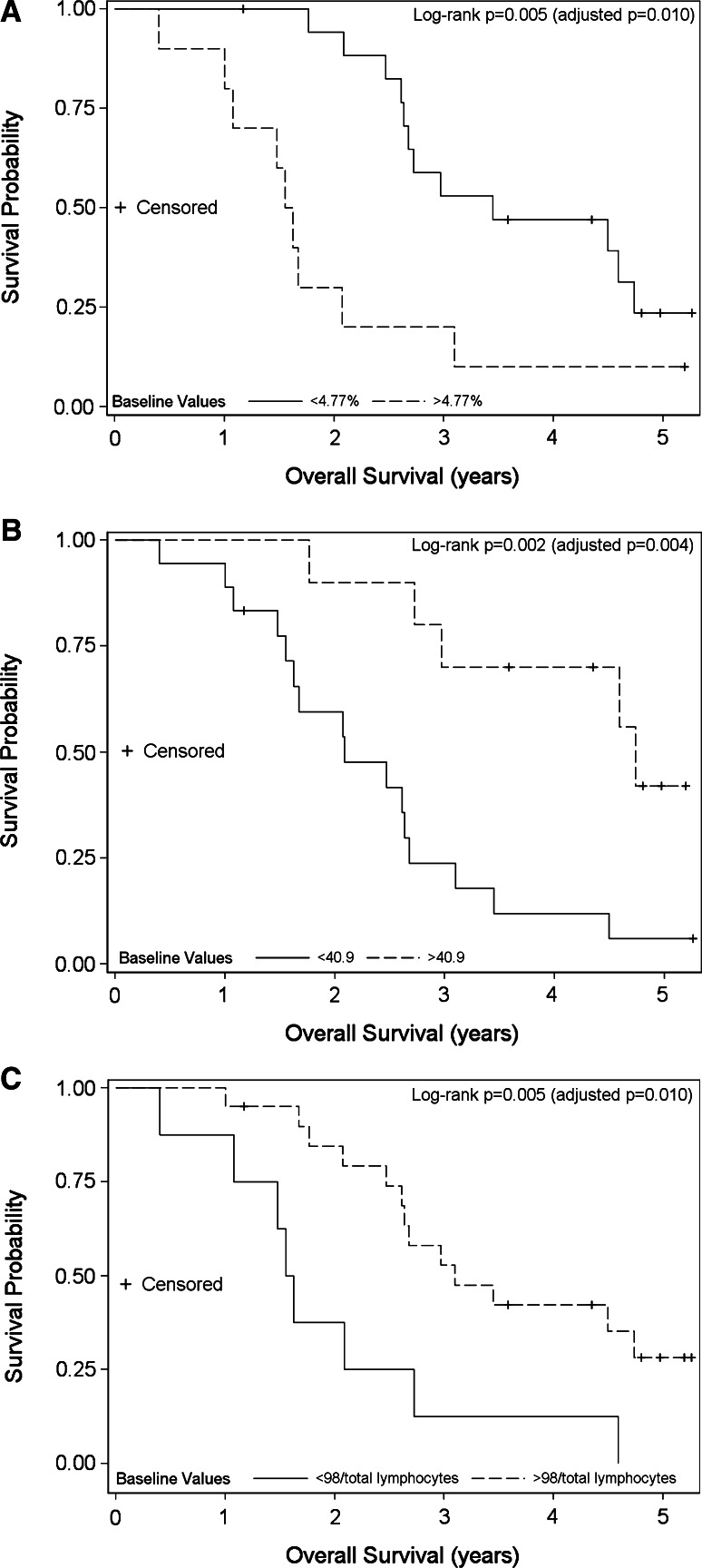
Actuarial analyses were performed to identify immune cell subsets that were associated with longer OS. Subsequently, Cox regression analyses were performed on the immune cell subsets showing evidence for being associated with longer OS. Three immune cell subsets at baseline were found to be jointly predictive of OS, but are presented in a univariate manner. As seen in Fig. 3a, patients with a lower percentage of PD-1+Tim-3NEG CD4 effector memory (CD4EM) cells at baseline (<4.77 %) displayed longer survival (P = 0.005, adjusted P = 0.010). As shown in Fig. 3b, patients with a higher percentage (>40.9 %) of activated Tim-3 single positive (Tim-3+PD-1NEG) CD8+ T lymphocytes at baseline displayed longer overall survival (P = 0.002, adjusted P = 0.004). Surprisingly, an increased number of Tregs at baseline also correlated with longer OS (P = 0.005, adjusted P = 0.010) (Fig. 3c); however, it should be noted that these were the CTLA-4NEG Tregs (CD4+ CD25HI FoxP3+ CD127NEG CTLA-4NEG), and not the CTLA-4+ Tregs, which have previously been found to be the most highly suppressive subset [7]. These immune cell subsets will be further discussed. The Cox model did not identify any other immune cell subsets as being predictive of OS.
Fig. 3.
Analysis of immune cell subsets at baseline versus overall survival. Thirty patients with metastatic castration-resistant prostate cancer were treated with an increasing dose (1, 3, 5, or 10 mg/kg) of ipilimumab in combination with PROSTVAC vaccine and GM-CSF. Peripheral blood mononuclear cells from baseline and day 70 were available for 28 patients, and were analyzed by flow cytometry. Kaplan–Meier curves representing overall survival versus immune cell subsets after dichotomizing the data at one of the tertiles are shown. a Baseline % PD-1+Tim-3NEG activated effector memory CD4+ T cells. Dashed lines denote overall survival of patients with immune cell subset values greater than the upper tertile. Solid lines denote overall survival of patients with immune cell subset values below the upper tertile. b Baseline % Tim-3+PD-1NEG activated CD8+ T cells. Dashed lines denote overall survival of patients with immune cell subset values greater than the upper tertile. Solid lines denote overall survival of patients with immune cell subset values below the upper tertile. c Baseline number of CTLA-4NEG Tregs (CD4+ CD25HI FoxP3+ CD127NEG CTLA-4NEG). Dashed lines denote overall survival of patients with immune cell subset values greater than the lower tertile. Solid lines denote overall survival of patients with immune cell subset values below the lower tertile
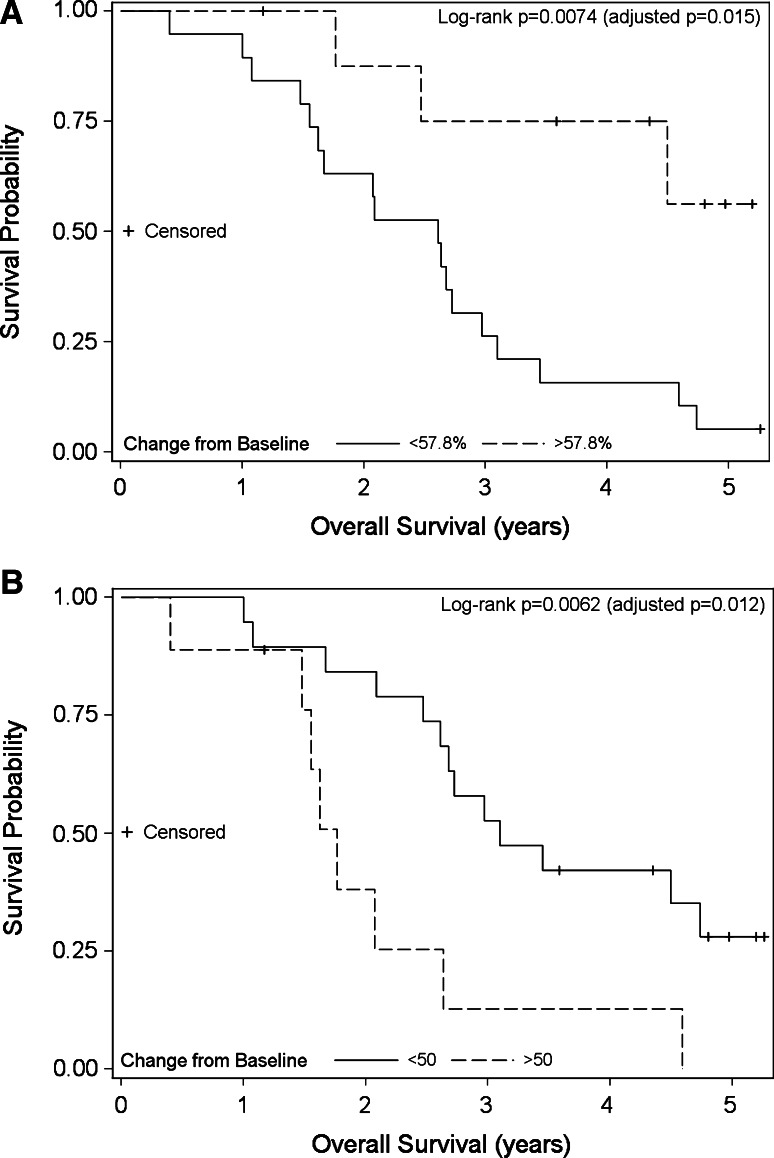
We then evaluated whether any association existed between overall survival and the change in a specific immune cell subset at 70 days of therapy, compared to the baseline level. This analysis was based solely on the change in immune cell subsets and the clinical baseline variables. Adjusting for the baseline level of hemoglobin, two other immune cell subsets were associated with OS (Table 3). There was a trend toward an increased OS in patients who had a larger increase in the population of immature NK cells transitioning into a more mature NK phenotype (TIM-3+ CD3NEG CD16NEG CD56BR) versus those patients who had a smaller increase or a decrease in this NK-cell subset (P = 0.0074, adjusted P = 0.015) (Fig. 4a), as well as a trend toward an increased OS in patients who had a decrease or less than 50 % increase in the percentage of PD-1+ Tim-3NEG CD8EM T cells versus those patients who had an increase >50 % in this subset on day 70 (P = 0.0062, adjusted P = 0.012) (Fig. 4b). No additional associations with OS were observed for the other immune cell subsets studied.
Fig. 4.
Analysis of change in immune cell subsets versus overall survival. Thirty patients with metastatic castration-resistant prostate cancer were treated with an increasing dose (1, 3, 5, or 10 mg/kg) of ipilimumab in combination with PROSTVAC vaccine and GM-CSF. Peripheral blood mononuclear cells from baseline and day 70 were available for 28 patients and were analyzed by flow cytometry. Kaplan–Meier curves representing overall survival versus immune cell subsets after dichotomizing the data at one of the tertiles. a The change from baseline to day 70 in the percentage of immature natural killer cells transitioning into a more mature phenotype (TIM-3+ CD16NEG CD56BR). Dashed lines denote overall survival of patients with immune cell subset changes greater than the upper tertile. Solid lines denote overall survival of patients with immune cell subset changes below the upper tertile. b The change from baseline to day 70 in the percentage of PD-1+Tim-3NEG CD8EM T cells (CD8+ CD45RANEG CD62LNEG CCR7NEG). Dashed lines denote overall survival of patients with an increase >50 % in this immune cell subset. Solid lines denote overall survival of patients with a decrease, or an increase <50 %, in this immune cell subset
Discussion
The study reported here provides an update on survival data from a Phase I trial combining therapy with a viral vector vaccine, PROSTVAC, and ipilimumab, an immune checkpoint inhibitor [12], as well as an evaluation of 36 discrete immune cell subsets in peripheral blood before and during this therapy.
The rationale for employing immunotherapy in prostate cancer is that previous studies have shown the presence of tumor-infiltrating lymphocytes in prostate cancer tissue, even when no therapy has been given previously [22, 23], and increased infiltration after androgen deprivation therapy [24]. In one study, the magnitude and quality of the infiltrate was shown to be a prognostic factor for survival [22]. This suggests that an immune reaction can be mounted, but it is not strong enough to inhibit tumor growth. A recent phenotypic study has shown that skewing of the intraprostatic immune cell infiltrate toward the TH17 and Treg phenotypes may be involved in the development and progression of prostate cancer [25]. Immunotherapies provide several different strategies to increase the immune response by increasing the immune cell infiltrate, by making the effector cells more proficient at killing the tumor cells, by decreasing immune suppressive entities such as Tregs and MDSC, or by changing the composition of the immune cell infiltrate, and thereby decreasing immunosuppression and overcoming immune tolerance. In addition, the presence of specific immune cell subsets prior to immunotherapy in some patients may render them more amenable to immunotherapy and vice versa. Prostate cancer provides a good model for immunotherapy since there are several known tumor-associated antigens [PSA, prostate-specific membrane antigen (PSMA), and PAP, for example] that are minimally expressed in other organs, decreasing the risk of immune-related side effects.
It has previously been shown that incorporation of transgenes for a tumor antigen and a triad of costimulatory molecules into the vaccine enhances the quantity and the quality of the CD8+ T cells generated [26, 27]. In addition, another preclinical study showed that simultaneously providing positive costimulation and inhibiting negative costimulatory signals using anti-CTLA-4 monoclonal antibodies resulted in greatly enhanced (10-fold) avidity of the T cells [28]. Since PSA–TRICOM has three costimulatory molecules designed to enhance T-cell immunity, and the ipilimumab checkpoint inhibitor is designed to reduce the immune suppressive CTLA-4 entity, it was important to determine whether the combination of PSA–TRICOM and ipilimumab would exacerbate the autoimmunity seen with ipilimumab alone. However, no increase in the frequency or severity of immune-related adverse events above that observed with ipilimumab alone was seen. The most common toxic effect seen in this study was grade 1–2 vaccination site reactions (3 patients had grade 1 and 26 patients had grade 2). Twenty-one patients had immune-related adverse events of grade 2 or higher. These included grade 3–4 diarrhea or colitis (4 patients), grade 3 rash (2 patients), grade 3 raised aminotransferases (2 patients), grade 3 endocrine events (2 patients), and grade 4 neutropenia (1 patient) [12].
The updated median OS in the trial reported here was 2.63 years (31.6 months). The patient population was similar to that in the previous Phase II trial of PSA–TRICOM alone, where the median survival in the vaccine arm was 25.1 months versus 16.6 months in the control arm. The results compare quite favorably with the results of a Phase II study employing PROSTVAC alone in a similar population. There also appeared to be a greater serum PSA response in the chemotherapy-naïve patients in the combination study [12, 29]. A Phase III trial of ipilimumab with radiation in advanced metastatic prostate cancer did not show a statistical survival benefit, i.e., only a 1.2-month difference in OS versus the placebo arm [30]. A 3-arm randomized trial will need to be conducted comparing the efficacy of vaccine versus ipilimumab versus vaccine + ipilimumab.
In the current trial, there were trends for longer overall survival favoring a lower Halabi score (i.e., a longer predicted survival), a longer PSA–DT, and a higher hemoglobin level at baseline, but no other clinical variables (Table 1). Interestingly, after adjusting for baseline hemoglobin levels, the immune subset variables still seem to significantly associate with longer survival (Table 3). It should be pointed out that all four doses of ipilimumab were included in the comparisons with OS, and one must be well aware of the risk that numerous comparisons could lead to false positives, which could lead to false conclusions. Therefore, the data generated in this study should strictly be considered as hypothesis generating data, and larger randomized studies are necessary to draw more definitive conclusions.
The rate of increase in ALC during the treatment for melanoma patients with ipilimumab has been shown to associate with clinical benefit in some previous trials, but many trials have also refuted this hypothesis [31, 32]. The current study could not show an association of increased ALC with clinical benefit, which may be due to any number of factors (e.g., melanoma vs. prostate cancer patients), although there was a slight trend for increased OS in patients with higher ALC at baseline (P = 0.057, adjusted P = 0.11).
We evaluated the frequencies of 36 different immune cell subsets at three time points—one prior to and two post-therapy—and performed correlative studies with overall survival. We found an increased frequency of ICOS+ CD4+ T cells after therapy (Fig. 2b), in accordance with the previous studies [33, 34], although this increase did not correlate with survival. Expression of ICOS on CD4+ T cells is necessary for effector memory development, reactivation, and survival [35, 36]. The frequency of ICOS+ was analyzed from the entire CD4+ population excluding Tregs. The ICOS/ICOSL pathway has been reported to be required for maximal anti-tumor effects following treatment with anti-CTLA-4 monoclonal antibodies [37], and a persistent increase in ICOS+ CD4+ T cells over 12 weeks correlated with OS in a retrospective analysis of melanoma patients treated with ipilimumab [38]. As seen in Fig. 2C, there was an increase in the frequency of IFNγ+ CD4+ T cells during therapy in the study reported here. This may be beneficial by activating CD8+ T cells and macrophages in the tumor microenvironment [39], thereby enhancing anti-tumor immunity.
Regulatory T cells are a major immunosuppressive entity, which increases tolerance and counteracts successful immunotherapy. We defined Tregs as CD4+ CD25HI FoxP3+ CD127NEG and further evaluated the expression of CTLA-4 on the surface. The CTLA-4+ Treg population was previously shown to be more suppressive than the CTLA-4NEG population in prostate cancer patients treated with PSA–TRICOM [7]. In the present study, there was an association (P = 0.005, adjusted P = 0.01) between the absolute number of CTLA-4NEG Tregs at baseline and survival (Fig. 3C). However, there was no association of survival with the more suppressive subset of Tregs (CTLA-4+) at baseline (P = 0.82). Regimens that decrease the numbers and/or activity of the Treg population have shown promising results, and one previous study showed that the efficacy of anti-CTLA-4 treatment against melanoma was mediated by Fc-dependent depletion of tumor-infiltrating Tregs [40]. It has also been shown in melanoma that CTLA-4 blockade of T effectors and Tregs concomitantly gives the greatest treatment efficacy [41].
In this trial, lower levels of PD-1+ Tim-3 NEG CD4EM cells at baseline associated with longer survival (Fig. 3a, P = 0.005, adjusted P = 0.01). This could suggest that therapy blocking PD-1 could be beneficial for the patients who display high levels of PD-1+ T cells. PD-1 is expressed by activated lymphocytes [42] and inhibits the effector functions and proliferation after binding to its ligand, PD-L1 (B7-H1). Interruption of the PD-1/PD-L1 pathway is currently being investigated and has shown promising results in melanoma and several carcinomas [43, 44]. In T-cell exhaustion, PD-1 and Tim-3 are coexpressed on the cell surface [45], and these cells produce fewer cytokines and show less proliferation. Some reports suggest that when PD-1 is expressed without Tim-3, this may be more indicative of T-cell activation than of T-cell exhaustion.
We also found a trend that higher levels of Tim-3+ PD-1NEG CD8+ T cells at baseline associated with longer overall survival (Fig. 3b, P = 0.002, adjusted P = 0.004). It has previously been reported that Tim-3-expressing human CD8+ T cells exhibit an effector memory phenotype, and strong effector functions in tuberculosis [46], which would support our finding. In contrast, T cells expressing both Tim-3 and PD-1 may exhibit an exhausted phenotype. We did not find any associations between the central memory subsets of CD8+ T cells and clinical outcome in this trial.
We found that an increase during therapy in the NK-cell immature subset that expresses Tim-3 was associated with increased survival (Fig. 4a, P = 0.0074, adjusted P = 0.015). Tim-3 is a maturation marker on NK cells and acts as a coreceptor to enhance IFNγ production [47]. Tim-3+ NK cells are fully responsive with respect to cytokine production and cytotoxicity, but may be negatively regulated when encountering target cells expressing ligands of Tim-3 [16]. This may thus be an important immune cell subset to monitor in future clinical immunotherapy trials.
In addition to the comparisons with all patients, we also evaluated whether there were any differences in OS between the cohort of patients that received 10 mg/kg of ipilimumab (n = 15), compared to the combined cohorts that received <10 mg/kg (n = 15) for 6 of the parameters; there were no statistical differences in the baseline Tim-3+ PD-1NEG CD8 T cells, baseline PSA–DT, baseline hemoglobin, or the change in Tim-3+ NK cells. There were greater differences in OS at baseline in PD-1+ Tim-3NEG effector memory CD4+ T cells and CTLA-4NEG Tregs in patients receiving lower doses of ipilimumab versus 10 mg/kg dose (P = 0.0001 vs. P = 0.36, and P = 0.021 vs. P = 0.22, respectively). This may suggest that the higher dose level of ipilimumab can overcome some of the underlying immune deficiencies present in patients, whereas in the lower dose groups, a deficiency in either of these cell subsets has an impact on the clinical outcome.
We have previously published the results of IFNγ ELISPOT analysis for PSA-peptide responses in this trial [12]. Unfortunately, only 9 of the 30 patients enrolled on this trial had the MHC class I allele HLA-A2, which to date is the only allele for which we have a functional ELISPOT assay to measure PSA-specific responses. Of the 9 patients who were HLA-A2+, 6 were in the <10 mg/kg cohort and 3 were in the 10 mg/kg cohort. The only 3 patients that had any post-vaccine level of elevation of PSA-specific T cells above the pre-vaccine levels were the 3 patients in the 10 mg/kg cohort. Therefore, it was not feasible for the current trial to relate the findings in immune cell subsets with the PSA-specific responses.
It should also be pointed out that both preclinical and clinical studies have indicated the potential importance of “antigen cascade,” also termed “epitope spreading,” in anti-tumor responses. For example, in one study [48, 49], CEA transgenic mice bearing CEA-expressing tumors were vaccinated with a recombinant vaccine directed against CEA. While control studies showed CEA was needed to be present in both the vaccine and tumor for the induction of anti-tumor responses, it was determined that the more significant immune response primarily responsible for the anti-tumor effect was that directed against an endogenous antigen (gp70) present in the tumor. Clinical studies in breast cancer also showed that there was a correlation with clinical benefit for those patients who demonstrated the phenomenon of antigen cascade in PBMCs post-vaccination [50–53]. Future vaccine-based clinical studies are being designed to measure the breadth of antigen-specific responses post-vaccination if sufficient PBMCs are available.
The data reported here are intended to be hypothesis generating, and larger randomized, controlled immunotherapy trials need to be evaluated in a similar manner to determine whether the analysis of specific immune cell subsets pre-treatment or early in the treatment cycle are predictive of clinical outcome. Results of such analysis may of course depend on the immunotherapeutic agent being evaluated, prior therapies of patients, and the disease and disease stage being investigated. It is interesting to note that in the study reported here, strong associations with OS were seen in specific immune cell subsets (Figs. 3, 4) as compared to conventional clinical parameters such as Gleason score, baseline PSA, and PSA-doubling time (Table 1). Adjusting for the independent effect of baseline hemoglobin levels, the changes during therapy in the other variables still seem to be associated with longer survival.
Acknowledgments
Grant support was provided by the Intramural Research Program of the Center for Cancer Research, National Cancer Institute, National Institutes of Health. The authors thank Debra Weingarten for her editorial assistance in the preparation of this manuscript.
Conflict of interest
The authors declare that they have no conflict of interest.
Abbreviations
- ALC
Absolute lymphocyte count
- CTLA-4
Cytotoxic T-lymphocyte-associated antigen-4
- DT
Doubling time
- EM
Effector memory
- GM-CSF
Granulocyte–macrophage colony-stimulating factor
- ICOS
Inducible costimulator
- IFN
Interferon
- IL
Interleukin
- mCRPC
Metastatic castration-resistant prostate cancer
- MDSC
Myeloid-derived suppressor cell
- NK
Natural killer
- OS
Overall survival
- PAP
Prostatic acid phosphatase
- PBMC
Peripheral blood mononuclear cell
- PD-1
Programmed death 1 receptor
- PSA
Prostate-specific antigen
- PSMA
Prostate-specific membrane antigen
- TIM-3
T-cell immunoglobulin and mucin domain-containing molecule-3
- Tregs
Regulatory T cells
- TRICOM
Triad of costimulatory molecules (ICAM-1, B7.1, and LFA-3)
Footnotes
James L. Gulley and Jeffrey Schlom have contributed equally to this study.
References
- 1.Kantoff PW, Higano CS, Shore ND, Berger ER, Small EJ, Penson DF, Redfern CH, Ferrari AC, Dreicer R, Sims RB, Xu Y, Frohlich MW, Schellhammer PF. Sipuleucel-T immunotherapy for castration-resistant prostate cancer. N Engl J Med. 2010;363:411–422. doi: 10.1056/NEJMoa1001294. [DOI] [PubMed] [Google Scholar]
- 2.Kantoff PW, Schuetz TJ, Blumenstein BA, Glode LM, Bilhartz DL, Wyand M, Manson K, Panicali DL, Laus R, Schlom J, Dahut WL, Arlen PM, Gulley JL, Godfrey WR. Overall survival analysis of a phase II randomized controlled trial of a poxviral-based PSA-targeted immunotherapy in metastatic castration-resistant prostate cancer. J Clin Oncol. 2010;28:1099–1105. doi: 10.1200/JCO.2009.25.0597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gulley JL, Arlen PM, Madan RA, Tsang KY, Pazdur MP, Skarupa L, Jones JL, Poole DJ, Higgins JP, Hodge JW, Cereda V, Vergati M, Steinberg SM, Halabi S, Jones E, Chen C, Parnes H, Wright JJ, Dahut WL, Schlom J. Immunologic and prognostic factors associated with overall survival employing a poxviral-based PSA vaccine in metastatic castrate-resistant prostate cancer. Cancer Immunol Immunother. 2010;59:663–674. doi: 10.1007/s00262-009-0782-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.A Randomized, Double-blind, Phase 3 Efficacy Trial of PROSTVAC-V/F +/− GM-CSF in Men With Asymptomatic or Minimally Symptomatic Metastatic Castrate-Resistant Prostate Cancer (Prospect) http://clinicaltrials.gov/ct2/show/NCT01322490
- 5.Hodge JW, Sabzevari H, Yafal AG, Gritz L, Lorenz MG, Schlom J. A triad of costimulatory molecules synergize to amplify T-cell activation. Cancer Res. 1999;59:5800–5807. [PubMed] [Google Scholar]
- 6.Halabi S, Small EJ, Kantoff PW, Kattan MW, Kaplan EB, Dawson NA, Levine EG, Blumenstein BA, Vogelzang NJ. Prognostic model for predicting survival in men with hormone-refractory metastatic prostate cancer. J Clin Oncol. 2003;21:1232–1237. doi: 10.1200/JCO.2003.06.100. [DOI] [PubMed] [Google Scholar]
- 7.Vergati M, Cereda V, Madan RA, Gulley JL, Huen NY, Rogers CJ, Hance KW, Arlen PM, Schlom J, Tsang KY. Analysis of circulating regulatory T cells in patients with metastatic prostate cancer pre- versus post-vaccination. Cancer Immunol Immunother. 2011;60:197–206. doi: 10.1007/s00262-010-0927-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hodi FS, O’Day SJ, McDermott DF, Weber RW, Sosman JA, Haanen JB, Gonzalez R, Robert C, Schadendorf D, Hassel JC, Akerley W, van den Eertwegh AJ, Lutzky J, Lorigan P, Vaubel JM, Linette GP, Hogg D, Ottensmeier CH, Lebbe C, Peschel C, Quirt I, Clark JI, Wolchok JD, Weber JS, Tian J, Yellin MJ, Nichol GM, Hoos A, Urba WJ. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363:711–723. doi: 10.1056/NEJMoa1003466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Robert C, Thomas L, Bondarenko I, O’Day S, Weber J, Garbe C, Lebbe C, Baurain JF, Testori A, Grob JJ, Davidson N, Richards J, Maio M, Hauschild A, Miller WH, Jr, Gascon P, Lotem M, Harmankaya K, Ibrahim R, Francis S, Chen TT, Humphrey R, Hoos A, Wolchok JD. Ipilimumab plus dacarbazine for previously untreated metastatic melanoma. N Engl J Med. 2011;364:2517–2526. doi: 10.1056/NEJMoa1104621. [DOI] [PubMed] [Google Scholar]
- 10.Small EJ, Tchekmedyian NS, Rini BI, Fong L, Lowy I, Allison JP. A pilot trial of CTLA-4 blockade with human anti-CTLA-4 in patients with hormone-refractory prostate cancer. Clin Cancer Res. 2007;13:1810–1815. doi: 10.1158/1078-0432.CCR-06-2318. [DOI] [PubMed] [Google Scholar]
- 11.Slovin SF, Higano CS, Hamid O, Tejwani S, Harzstark A, Alumkal JJ, Scher HI, Chin K, Gagnier P, McHenry MB, Beer TM. Ipilimumab alone or in combination with radiotherapy in metastatic castration-resistant prostate cancer: results from an open-label, multicenter phase I/II study. Ann Oncol. 2013;24:1813–1821. doi: 10.1093/annonc/mdt107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Madan RA, Mohebtash M, Arlen PM, Vergati M, Rauckhorst M, Steinberg SM, Tsang KY, Poole DJ, Parnes HL, Wright JJ, Dahut WL, Schlom J, Gulley JL. Ipilimumab and a poxviral vaccine targeting prostate-specific antigen in metastatic castration-resistant prostate cancer: a phase 1 dose-escalation trial. Lancet Oncol. 2012;13:501–508. doi: 10.1016/S1470-2045(12)70006-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sallusto F, Geginat J, Lanzavecchia A. Central memory and effector memory T cell subsets: function, generation, and maintenance. Annu Rev Immunol. 2004;22:745–763. doi: 10.1146/annurev.immunol.22.012703.104702. [DOI] [PubMed] [Google Scholar]
- 14.Wing K, Onishi Y, Prieto-Martin P, Yamaguchi T, Miyara M, Fehervari Z, Nomura T, Sakaguchi S. CTLA-4 control over Foxp3 + regulatory T cell function. Science. 2008;322:271–275. doi: 10.1126/science.1160062. [DOI] [PubMed] [Google Scholar]
- 15.Huen NY, Pang AL, Tucker JA, Lee TL, Vergati M, Jochems C, Intrivici C, Cereda V, Chan WY, Rennert OM, Madan RA, Gulley JL, Schlom J, Tsang KY. Up-regulation of proliferative and migratory genes in regulatory T cells from patients with metastatic castration-resistant prostate cancer. Int J Cancer. 2013 doi: 10.1002/ijc.28026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ndhlovu LC, Lopez-Verges S, Barbour JD, Jones RB, Jha AR, Long BR, Schoeffler EC, Fujita T, Nixon DF, Lanier LL. Tim-3 marks human natural killer cell maturation and suppresses cell-mediated cytotoxicity. Blood. 2012;119:3734–3743. doi: 10.1182/blood-2011-11-392951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Beziat V, Duffy D, Quoc SN, Le Garff-Tavernier M, Decocq J, Combadiere B, Debre P, Vieillard V. CD56brightCD16 + NK cells: a functional intermediate stage of NK cell differentiation. J Immunol. 2011;186:6753–6761. doi: 10.4049/jimmunol.1100330. [DOI] [PubMed] [Google Scholar]
- 18.Vuk-Pavlovic S, Bulur PA, Lin Y, Qin R, Szumlanski CL, Zhao X, Dietz AB. Immunosuppressive CD14 + HLA-DRlow/- monocytes in prostate cancer. Prostate. 2010;70:443–455. doi: 10.1002/pros.21078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Greten TF, Manns MP, Korangy F. Myeloid derived suppressor cells in human diseases. Int Immunopharmacol. 2011;11:802–807. doi: 10.1016/j.intimp.2011.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vaccine and Antibody Treatment of Prostate Cancer. http://clinicaltrials.gov/show/NCT00113984
- 21.Teeter AE, Presti JC, Jr, Aronson WJ, Terris MK, Kane CJ, Amling CL, Freedland SJ. Does PSADT after radical prostatectomy correlate with overall survival?—a report from the SEARCH database group. Urology. 2011;77:149–153. doi: 10.1016/j.urology.2010.04.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vesalainen S, Lipponen P, Talja M, Syrjanen K. Histological grade, perineural infiltration, tumour-infiltrating lymphocytes and apoptosis as determinants of long-term prognosis in prostatic adenocarcinoma. Eur J Cancer. 1994;30A:1797–1803. doi: 10.1016/0959-8049(94)E0159-2. [DOI] [PubMed] [Google Scholar]
- 23.Karja V, Aaltomaa S, Lipponen P, Isotalo T, Talja M, Mokka R. Tumour-infiltrating lymphocytes: a prognostic factor of PSA-free survival in patients with local prostate carcinoma treated by radical prostatectomy. Anticancer Res. 2005;25:4435–4438. [PubMed] [Google Scholar]
- 24.Mercader M, Bodner BK, Moser MT, Kwon PS, Park ES, Manecke RG, Ellis TM, Wojcik EM, Yang D, Flanigan RC, Waters WB, Kast WM, Kwon ED. T cell infiltration of the prostate induced by androgen withdrawal in patients with prostate cancer. Proc Natl Acad Sci USA. 2001;98:14565–14570. doi: 10.1073/pnas.251140998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sfanos KS, Bruno TC, Maris CH, Xu L, Thoburn CJ, DeMarzo AM, Meeker AK, Isaacs WB, Drake CG. Phenotypic analysis of prostate-infiltrating lymphocytes reveals TH17 and Treg skewing. Clin Cancer Res. 2008;14:3254–3261. doi: 10.1158/1078-0432.CCR-07-5164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yang S, Hodge JW, Grosenbach DW, Schlom J. Vaccines with enhanced costimulation maintain high avidity memory CTL. J Immunol. 2005;175:3715–3723. doi: 10.4049/jimmunol.175.6.3715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hodge JW, Chakraborty M, Kudo-Saito C, Garnett CT, Schlom J. Multiple costimulatory modalities enhance CTL avidity. J Immunol. 2005;174:5994–6004. doi: 10.4049/jimmunol.174.10.5994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chakraborty M, Schlom J, Hodge JW. The combined activation of positive costimulatory signals with modulation of a negative costimulatory signal for the enhancement of vaccine-mediated T-cell responses. Cancer Immunol Immunother. 2007;56:1471–1484. doi: 10.1007/s00262-007-0291-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.van den Eertwegh AJ, Versluis J, van den Berg HP, Santegoets SJ, van Moorselaar RJ, van der Sluis TM, Gall HE, Harding TC, Jooss K, Lowy I, Pinedo HM, Scheper RJ, Stam AG, von Blomberg BM, de Gruijl TD, Hege K, Sacks N, Gerritsen WR. Combined immunotherapy with granulocyte-macrophage colony-stimulating factor-transduced allogeneic prostate cancer cells and ipilimumab in patients with metastatic castration-resistant prostate cancer: a phase 1 dose-escalation trial. Lancet Oncol. 2012;13:509–517. doi: 10.1016/S1470-2045(12)70007-4. [DOI] [PubMed] [Google Scholar]
- 30.Gerritsen WR (2013) CA184-043: a randomized, multicenter, double-blind phase 3 trial comparing overall survival (OS) in patients (pts) with post-docetaxel castration-resistant prostate cancer (CRPC) and bone metastases treated with ipilimumab (ipi) vs placebo (pbo), each following single-dose radiotherapy (RT). The European Cancer Congress, Sept. 27–Oct. 1, 2013; abstr 2850
- 31.Ku GY, Yuan J, Page DB, Schroeder SE, Panageas KS, Carvajal RD, Chapman PB, Schwartz GK, Allison JP, Wolchok JD. Single-institution experience with ipilimumab in advanced melanoma patients in the compassionate use setting: lymphocyte count after 2 doses correlates with survival. Cancer. 2010;116:1767–1775. doi: 10.1002/cncr.24951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Berman D, Wolchok J, Weber J, Hamid O, O’Day S, Chasalow S (2009) Association of peripheral blood absolute lymphocyte count (ALC) and clinical activity in patients (pts) with advanced melanoma treated with ipilimumab. J Clin Oncol 27(Suppl; abstr 3020)
- 33.Liakou CI, Kamat A, Tang DN, Chen H, Sun J, Troncoso P, Logothetis C, Sharma P. CTLA-4 blockade increases IFNgamma-producing CD4 + ICOShi cells to shift the ratio of effector to regulatory T cells in cancer patients. Proc Natl Acad Sci USA. 2008;105:14987–14992. doi: 10.1073/pnas.0806075105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chen H, Liakou CI, Kamat A, Pettaway C, Ward JF, Tang DN, Sun J, Jungbluth AA, Troncoso P, Logothetis C, Sharma P. Anti-CTLA-4 therapy results in higher CD4 + ICOShi T cell frequency and IFN-gamma levels in both nonmalignant and malignant prostate tissues. Proc Natl Acad Sci USA. 2009;106:2729–2734. doi: 10.1073/pnas.0813175106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mahajan S, Cervera A, MacLeod M, Fillatreau S, Perona-Wright G, Meek S, Smith A, MacDonald A, Gray D. The role of ICOS in the development of CD4 T cell help and the reactivation of memory T cells. Eur J Immunol. 2007;37:1796–1808. doi: 10.1002/eji.200636661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Moore TV, Clay BS, Ferreira CM, Williams JW, Rogozinska M, Cannon JL, Shilling RA, Marzo AL, Sperling AI. Protective effector memory CD4 T cells depend on ICOS for survival. PLoS ONE. 2011;6:e16529. doi: 10.1371/journal.pone.0016529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fu T, He Q, Sharma P. The ICOS/ICOSL pathway is required for optimal antitumor responses mediated by anti-CTLA-4 therapy. Cancer Res. 2011;71:5445–5454. doi: 10.1158/0008-5472.CAN-11-1138. [DOI] [PubMed] [Google Scholar]
- 38.Carthon BC, Wolchok JD, Yuan J, Kamat A, Ng Tang DS, Sun J, Ku G, Troncoso P, Logothetis CJ, Allison JP, Sharma P. Preoperative CTLA-4 blockade: tolerability and immune monitoring in the setting of a presurgical clinical trial. Clin Cancer Res. 2010;16:2861–2871. doi: 10.1158/1078-0432.CCR-10-0569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Corthay A, Skovseth DK, Lundin KU, Rosjo E, Omholt H, Hofgaard PO, Haraldsen G, Bogen B. Primary antitumor immune response mediated by CD4 + T cells. Immunity. 2005;22:371–383. doi: 10.1016/j.immuni.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 40.Simpson TR, Li F, Montalvo-Ortiz W, Sepulveda MA, Bergerhoff K, Arce F, Roddie C, Henry JY, Yagita H, Wolchok JD, Peggs KS, Ravetch JV, Allison JP, Quezada SA. Fc-dependent depletion of tumor-infiltrating regulatory T cells co-defines the efficacy of anti-CTLA-4 therapy against melanoma. J Exp Med. 2013 doi: 10.1084/jem.20130579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Peggs KS, Quezada SA, Chambers CA, Korman AJ, Allison JP. Blockade of CTLA-4 on both effector and regulatory T cell compartments contributes to the antitumor activity of anti-CTLA-4 antibodies. J Exp Med. 2009;206:1717–1725. doi: 10.1084/jem.20082492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Vibhakar R, Juan G, Traganos F, Darzynkiewicz Z, Finger LR. Activation-induced expression of human programmed death-1 gene in T-lymphocytes. Exp Cell Res. 1997;232:25–28. doi: 10.1006/excr.1997.3493. [DOI] [PubMed] [Google Scholar]
- 43.Topalian SL, Hodi FS, Brahmer JR, Gettinger SN, Smith DC, McDermott DF, Powderly JD, Carvajal RD, Sosman JA, Atkins MB, Leming PD, Spigel DR, Antonia SJ, Horn L, Drake CG, Pardoll DM, Chen L, Sharfman WH, Anders RA, Taube JM, McMiller TL, Xu H, Korman AJ, Jure-Kunkel M, Agrawal S, McDonald D, Kollia GD, Gupta A, Wigginton JM, Sznol M. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med. 2012;366:2443–2454. doi: 10.1056/NEJMoa1200690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Brahmer JR, Tykodi SS, Chow LQ, Hwu WJ, Topalian SL, Hwu P, Drake CG, Camacho LH, Kauh J, Odunsi K, Pitot HC, Hamid O, Bhatia S, Martins R, Eaton K, Chen S, Salay TM, Alaparthy S, Grosso JF, Korman AJ, Parker SM, Agrawal S, Goldberg SM, Pardoll DM, Gupta A, Wigginton JM. Safety and activity of anti-PD-L1 antibody in patients with advanced cancer. N Engl J Med. 2012;366:2455–2465. doi: 10.1056/NEJMoa1200694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jin HT, Anderson AC, Tan WG, West EE, Ha SJ, Araki K, Freeman GJ, Kuchroo VK, Ahmed R. Cooperation of Tim-3 and PD-1 in CD8 T-cell exhaustion during chronic viral infection. Proc Natl Acad Sci USA. 2010;107:14733–14738. doi: 10.1073/pnas.1009731107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Qiu Y, Chen J, Liao H, Zhang Y, Wang H, Li S, Luo Y, Fang D, Li G, Zhou B, Shen L, Chen CY, Huang D, Cai J, Cao K, Jiang L, Zeng G, Chen ZW. Tim-3-expressing CD4 + and CD8 + T cells in human tuberculosis (TB) exhibit polarized effector memory phenotypes and stronger anti-TB effector functions. PLoS Pathog. 2012;8:e1002984. doi: 10.1371/journal.ppat.1002984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gleason MK, Lenvik TR, McCullar V, Felices M, O’Brien MS, Cooley SA, Verneris MR, Cichocki F, Holman CJ, Panoskaltsis-Mortari A, Niki T, Hirashima M, Blazar BR, Miller JS. Tim-3 is an inducible human natural killer cell receptor that enhances interferon gamma production in response to galectin-9. Blood. 2012;119:3064–3072. doi: 10.1182/blood-2011-06-360321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kudo-Saito C, Garnett CT, Wansley EK, Schlom J, Hodge JW. Intratumoral delivery of vector mediated IL-2 in combination with vaccine results in enhanced T cell avidity and anti-tumor activity. Cancer Immunol Immunother. 2007;56:1897–1910. doi: 10.1007/s00262-007-0332-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kudo-Saito C, Schlom J, Camphausen K, Coleman CN, Hodge JW. The requirement of multimodal therapy (vaccine, local tumor radiation, and reduction of suppressor cells) to eliminate established tumors. Clin Cancer Res. 2005;11:4533–4544. doi: 10.1158/1078-0432.CCR-04-2237. [DOI] [PubMed] [Google Scholar]
- 50.Disis ML. Enhancing cancer vaccine efficacy via modulation of the tumor microenvironment. Clin Cancer Res. 2009;15:6476–6478. doi: 10.1158/1078-0432.CCR-09-2256. [DOI] [PubMed] [Google Scholar]
- 51.Disis ML. Immunologic biomarkers as correlates of clinical response to cancer immunotherapy. Cancer Immunol Immunother. 2011;60:433–442. doi: 10.1007/s00262-010-0960-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hardwick N, Chain B. Epitope spreading contributes to effective immunotherapy in metastatic melanoma patients. Immunotherapy. 2011;3:731–733. doi: 10.2217/imt.11.62. [DOI] [PubMed] [Google Scholar]
- 53.Walter S, Weinschenk T, Stenzl A, Zdrojowy R, Pluzanska A, Szczylik C, Staehler M, Brugger W, Dietrich PY, Mendrzyk R, Hilf N, Schoor O, Fritsche J, Mahr A, Maurer D, Vass V, Trautwein C, Lewandrowski P, Flohr C, Pohla H, Stanczak JJ, Bronte V, Mandruzzato S, Biedermann T, Pawelec G, Derhovanessian E, Yamagishi H, Miki T, Hongo F, Takaha N, Hirakawa K, Tanaka H, Stevanovic S, Frisch J, Mayer-Mokler A, Kirner A, Rammensee HG, Reinhardt C, Singh-Jasuja H. Multipeptide immune response to cancer vaccine IMA901 after single-dose cyclophosphamide associates with longer patient survival. Nat Med. 2012;18:1254–1261. doi: 10.1038/nm.2883. [DOI] [PubMed] [Google Scholar]