Structured Abstract
Background:
Due to the limitations of existing clinical treatments for urinary incontinence, many women with incontinence are interested in complementary strategies for managing their symptoms. Yoga has been recommended as a behavioral self-management strategy for incontinence, but evidence of its feasibility, tolerability, and efficacy is lacking.
Objectives:
To evaluate the feasibility and tolerability of a group-based therapeutic yoga program for ambulatory middle-aged and older women with incontinence and examine preliminary changes in incontinence frequency as the primary efficacy outcome after 3 months.
Study Design:
Ambulatory women aged 50 years or older who reported at least daily stress-, urgency-, or mixed-type incontinence, were not already engaged in yoga, and were temporarily willing to forgo clinical incontinence treatments were recruited into a randomized trial in the San Francisco Bay area. Women were randomly assigned to take part in a program of twice weekly group classes and once weekly home practice focused on Iyengar-based yoga techniques selected by an expert yoga panel (yoga group) or a non-specific muscle stretching and strengthening program designed to provide a rigorous time-and-attention control (control group) for 3 months. All participants also received written, evidence-based information about behavioral incontinence self-management techniques (pelvic floor exercises, bladder training) consistent with usual first-line care. Incontinence frequency and type were assessed by validated voiding diaries. Analysis of covariance models examined within- and between-group changes in incontinence frequency as the primary efficacy outcome over 3 months.
Results:
Of the 56 women randomized (28 to yoga, 28 to control), mean age was 65.4 (±8.1) years (range 55–83 years), mean baseline incontinence frequency was 3.5 (±2.0) episodes/day, and 37 (66%) had urgency-predominant incontinence. Fifty women completed their assigned 3-month intervention program (89%), including 27 in the yoga and 23 in the control group (P=0.19). Of those, 24 (89%) in the yoga and 20 (87%) in the control group attended at least 80% of group classes. Over 3 months, total incontinence frequency decreased by an average of 76% from baseline in the yoga and 56% in the control group (P=0.07 for between-group difference). Stress incontinence frequency also decreased by an average of 61% in the yoga group and 35% in controls (P=0.045 for between-group difference), but changes in urgency incontinence frequency did not differ significantly between groups. Forty-eight non-serious adverse events were reported, including 23 in the yoga and 25 in the control group, but none were directly attributable to yoga or control program practice.
Conclusions:
Findings demonstrate the feasibility of recruiting and retaining incontinent women across the aging spectrum into a therapeutic yoga program and provide preliminary evidence of reduction in total and stress-type incontinence frequency after 3 months of yoga practice. When taught with attention to women’s clinical needs, yoga may offer a potential community-based behavioral self-management strategy for incontinence to enhance clinical treatment, although future research should assess whether yoga offers unique benefits for incontinence above and beyond other physical activity-based interventions.
Unstructured Abstract
Yoga has been recommended as a complementary behavioral self-management strategy for urinary incontinence, but evidence of its feasibility, tolerability, and efficacy is lacking. A single-center randomized trial was conducted to evaluate the feasibility and tolerability of a group-based therapeutic yoga program for incontinence in women and examine changes in incontinence frequency as the primary efficacy outcome after 3 months of yoga practice. Ambulatory women aged 50 years and older with daily stress-, urgency-, or mixed-type incontinence were randomly assigned to take part in a 3-month program involving twice weekly group yoga classes and once weekly home yoga practice designed by an expert yoga panel (yoga group) or a non-specific muscle stretching and strengthening program designed to provide a rigorous time-and-attention control (control group). Of the 56 women randomized (mean age of 65.4 ±8.1 years,) mean baseline incontinence frequency was 3.5 (±2.0) episodes/day. Fifty women completed the 3-month intervention program (89%), including 27 in the yoga and 23 in the control group. Of those, 89% in the yoga and 87% in the control group attended at least 80% of group classes. Over 3 months, total incontinence frequency decreased by an average of 76% from baseline in the yoga group and 56% in the control group (P=0.07 for between-group difference). Stress incontinence frequency also decreased by an average of 61% in the yoga group and 35% in controls (P=0.045 for between-group difference), but changes in urgency incontinence frequency were smaller and did not differ significantly between groups. Forty-eight non-serious adverse events were reported, including 23 in the yoga group and 25 in the control group, but none were directly attributable to yoga or control program practice. Findings demonstrate the feasibility of recruiting and retaining incontinent women across the aging spectrum into a therapeutic yoga program and provide preliminary evidence of reduction in total and stress-type incontinence frequency after 3 months of yoga practice. When taught with appropriate attention to women’s clinical needs, yoga may offer a potential community-based behavioral self-management strategy for incontinence to enhance clinical treatment.
Condensation (single sentence of up to 25 words)
Ambulatory women found a 3-month incontinence-specific yoga program to be well-tolerated, although their 76% decrease in incontinence frequency was not significantly greater than among time-and-attention controls.
Introduction
One in three women over the age of 50 suffers from urinary incontinence, a condition associated with depression, social isolation, falls and fractures, and loss of ability to live independently.1–9 Current first-line treatment consists of behavioral strategies such as pelvic floor exercises that can be difficult for women to practice effectively without one-on-one training with specialized healthcare practitioners.10–13 Second-line treatments such as anticholinergic medications have side effects that limit their safety and tolerability.14–17 As a result, there is a need for alternate management strategies that are not only effective, but also better tolerated and more accessible.
Yoga is a set of complementary physical and mental practices with the potential to improve incontinence in women through multiple mechanisms. When practiced with emphasis on mindful awareness of specific body structures, yoga can be used to help women identify and control their pelvic floor muscles to improve incontinence-related pelvic floor dysfunction. Restorative yoga practices also have the potential to reduce anxiety, perceived stress, and associated autonomic imbalance,18–24 as factors that can precipitate or worsen urgency incontinence.25–27 Regular practice of yoga can also improve lower extremity strength and conditioning28,29 to protect against incontinence in frail older women.30,31
Nevertheless, despite interest in yoga by women with incontinence,32–34 data to support yoga as a management strategy for incontinence are lacking. Our research team previously collaborated with an expert yoga panel to develop a group-based yoga program for incontinence in women.35 We now describe findings from a single-center trial to assess the feasibility of recruiting and retaining ambulatory incontinent women in this yoga program, assess the safety and tolerability of yoga, and evaluate preliminary changes in incontinence after 3 months.
Materials and Methods
Eligibility and recruitment
Ambulatory women with incontinence were recruited into a single-center, parallel-group, randomized trial of a 3-month therapeutic yoga program versus non-specific muscle stretching and strengthening control program. To be eligible, women had to be at least 50 years of age, report incontinence for at least 3 months, document at least 3 episodes of incontinence on a screening 3-day voiding diary,36,37 and self-report predominantly stress-, urgency-, or mixed-type incontinence. Participants also had to agree to forgo other clinical incontinence treatments during the 3-month trial, including practitioner-supervised behavioral treatments such as pelvic floor therapy.
Women were excluded if they had major mobility limitations such as being unable to walk two blocks on level ground or get up from a supine to standing position unassisted. Participants could not already be engaged in organized yoga classes or have completed prior yoga training directed specifically at treatment of incontinence. Other exclusion criteria included pregnancy in the past 6 months; current urinary tract infection or hematuria; history of 3 or more urinary tract infections in the past year; major neurologic condition such as stroke; history of bladder or rectal fistula, pelvic cancer or radiation, interstitial cystitis or chronic pelvic pain, or congenital defect leading to incontinence; current symptomatic pelvic organ prolapse; prior anti-incontinence or urethral surgery; or other pelvic surgery in the past 3 months.
Participants were recruited from the San Francisco Bay area using flyers posted in community centers, newspaper advertisements, community mailings, and recruitment of female patients from University of California San Francisco (UCSF) Medical Center. Before undergoing in-person screening, all women provided written informed consent. All study procedures were approved by the UCSF institutional review board (IRB#14–14732), and the trial was registered in clinicaltrials.gov (NCT02342678).
Randomization and blinding
Eligible participants were randomly assigned in equal ratios to either the yoga intervention or muscle stretching/strengthening control intervention. Randomization was stratified by clinical incontinence type (e.g., stress- versus urgency-predominant) and performed by computer using randomly permuted blocks of sizes 2 and 4. Standard allocation concealment procedures were followed to avoid manipulation of randomization.38
Due to the behavioral nature of the interventions, participants were aware of intervention assignment, as were study personnel involved in administering interventions or assessing adherence, but investigators and all staff involved in abstracting data from outcome instruments were blinded. To minimize differential expectations of treatment success, participants were told that they were participating in a study of two different types of low-impact physical activity-based interventions for incontinence, and that the investigators did not know which, if any, might be more effective.
Incontinence self-management pamphlet
At randomization, participants in both groups were given a written pamphlet providing basic patient-directed information about behavioral self-management of incontinence (such as pelvic floor exercises and timed urination) consistent with usual first-line care.39 Systematic provision of this information was designed to minimize differential use of self-management strategies, but participants received no additional instruction in these techniques.
Yoga program
The therapeutic yoga program was designed to provide instruction and practice in selected yoga postures and techniques chosen for their potential to improve bladder control in women as well as promote safety and feasibility in this population. The program was based on Iyengar yoga, a form of Hatha yoga that is known for its potential therapeutic applications, which has been employed successfully in studies of yoga for other indications,18,20,40–46 and differs from other yoga styles in ways expected to maximize both efficacy and safety. These included: 1) emphasis on precise anatomical alignment and awareness of specific bodily structures during practice of yoga postures; 2) incorporation of yoga props to minimize risk of injury and accommodate those with less strength or flexibility; and 3) emphasis on mindful awareness during practice of postures rather than rapid cycling through postures.
The program focused on a core set of 15 yoga postures widely used in Hatha yoga practice, including active postures to engage the pelvic floor and passive postures to promote relaxation (Appendix A). The resulting program was designed to maximize awareness and control of the pelvic floor, reduce underlying stress and anxiety, and improve overall physical function, while still being feasible for women with mild-to-moderate mobility limitations, as well as grounded in techniques common to Iyengar yoga at large.
During each intervention wave, participants engaged in twice weekly 90-minute group classes with an average of 6 to 8 students, led by an instructor who had undergone study-specific training with the study’s yoga consultants. The instructor followed a study-specific guide to introduce participants to yoga postures and called attention to ways in which postures could improve pelvic floor function, while guiding women in adapting postures and using props to accommodate physical limitations as needed.
In addition to attending group classes, participants were asked to practice yoga at home at least one additional hour per week. Women were also given a written manual that included pictures and descriptions of each yoga posture to guide them in home practice, as well as a yoga mat, belt, and two blocks for home practice.
Stretching/strengthening control program
Women randomized to the control group took part in a non-specific muscle stretching and strengthening program designed to provide a rigorous time-and-attention control for the yoga program. Exercises were adapted from those used in a prior trial of yoga for metabolic syndrome and were designed to avoid engaging the pelvic floor or promoting mindful relaxation.47
Similar to the yoga program, the control program consisted of a series of twice weekly 90-minute group classes, led by an instructor who had undergone training with the study’s physical therapy consultant. Control group participants were also instructed to practice exercises at home at least an hour per week using a written manual and received stretch straps, resistance bands, and a mat to use at home.
Feasibility, safety, and efficacy measures
Feasibility was evaluated through assessment of adherence as well as self-reported and observed success in learning to practice yoga. Adherence to intervention classes was documented by instructors using attendance logs. Adherence to home practice was documented by participants in home logs that included the dates and times of practice. At the end of each intervention program, participants were asked to rate their confidence in performing each of the postures/exercises featured in their program (extremely, very, moderately, somewhat, and not at all confident). During the last week of class, a study expert consultant observed each participant in attendance and rated her success in performing postures/exercises (extremely, very, moderately, somewhat, and not at all successful).
Safety and tolerability were assessed by asking participants about any negative changes in their health at each follow-up visit or phone call, which were documented as adverse events. At the end of the intervention programs, participants were also asked to indicate how easy it would be to continue practicing their assignment intervention (extremely, very, moderately, somewhat, and not at all easy).
For preliminary assessment of efficacy, changes in frequency of incontinence were assessed using validated 3-day voiding diaries.36,37 At baseline and after 3 months, each participant received written instructions and a blank diary to take home to record all incontinence episodes over a 3-day period and to classify episodes by type (urgency, stress, other). Blinded analysts abstracted data to determine change in frequency of total incontinence (as the primary efficacy outcome), as well as urgency and stress incontinence (as secondary efficacy outcomes) over 3 months.
To assess change in incontinence-related quality of life as an additional secondary efficacy outcome, participants also completed multiple standardized questionnaires at baseline and at 3 months: 1) the 28-item Incontinence Impact Questionnaire (IIQ);48,49 2) the 6-item Urogenital Distress Inventory-6 (UDI-6);49 and 3) the single-item Patient Perception of Bladder Condition (PPBC).50,51
Sample size and statistical analyses
The investigative team set a goal of randomizing a minimum of 50 participants and conducting a minimum of 3 intervention class waves in order to explore the feasibility of recruiting and retaining participants, teaching intervention techniques across multiple waves and class instructors, and administering primary and secondary efficacy outcome measures. No formal sample size calculations were performed in advance of the study, since the trial was not designed to test formal hypotheses about efficacy.
Baseline characteristics of participants in each group were compared using t-tests and chi-square tests, as appropriate. Participant drop-out and adherence rates in each group were compared using Fisher’s exact tests. Fisher’s exact tests were also used to compare participants’ self-reported confidence in performing postures/exercises and observed success in performing postures/exercises at 3 months, as well as safety and tolerability as measured by rates of adverse events and self-reported ease of continuing to practice postures/exercises after 3 months.
Analysis of covariance models were developed to examine change in incontinence frequency and quality of life outcomes over 3 months. Separate models were developed to examine: 1) absolute change in outcomes adjusting for baseline values, and 2) percent change in outcomes from baseline. Results were summarized using least square mean estimates of changes in incontinence frequency and quality of life outcomes in each group, as well as estimates of between-group difference in change in outcomes.
Main efficacy analyses included all participants regardless of drop-out or adherence, consistent with an intention-to-treat principle. To address the potential for bias stemming from missing bladder diary data for up to 16% of participants who dropped out of interventions early, a multiple imputation procedure (SAS PROC MI, SAS Institute, Inc.) was used to impute values for data missing at follow-up.52 Imputation models included outcomes, randomization group, and baseline values. On the hypothesis that dropouts in both groups would experience the same average changes observed in the control group, imputed follow-up incontinence outcomes in both groups were standardized to the mean and standard deviation of the observed follow-up values in controls. Finally, analysis of the resulting 10 imputed datasets was performed using SAS PROC MIANALYZE, which provides standard errors reflecting uncertainty in the imputed data. Additional exploratory “per protocol” analyses of intervention effects on incontinence frequency were also performed, which omitted participants who discontinued interventions early.
Results
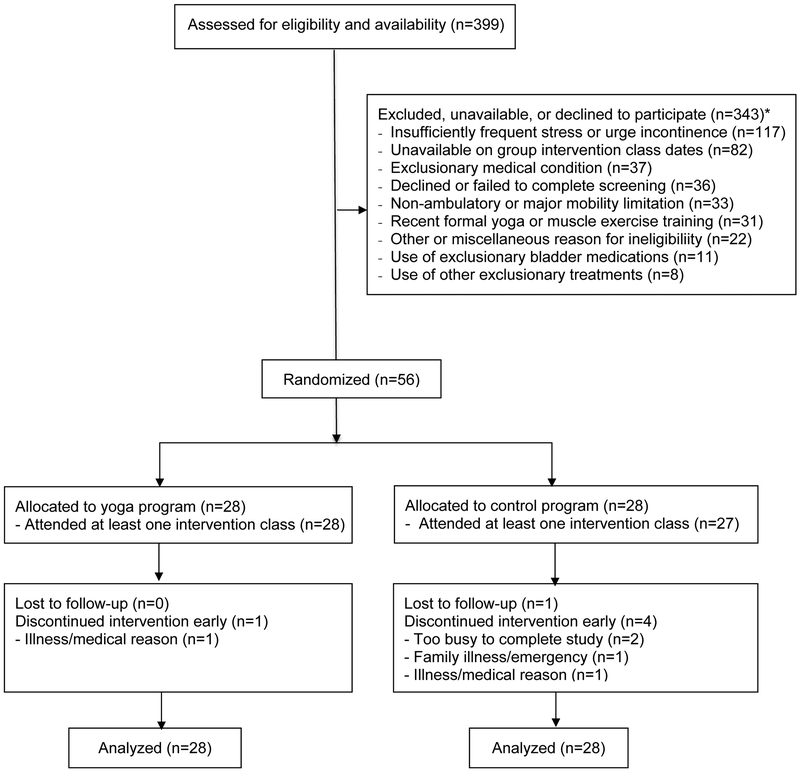
Of the 399 women contacted by telephone from 2015–2017, 91 attended an in-person screening visit. Twenty-eight were randomized to yoga, and 28 to the control group (Figure 1). Of the randomized women, 27 in the yoga group (95%) and 23 in the control group (83%) completed the 3-month program (P=.19 for between-group difference). All women completing the intervention provided 3-month bladder diary data on the primary efficacy outcome.
Figure1.
Flowchart of Participant Recruitment, Randomization, and Retention
The mean age was 65.4 (±8.1) years (range 55–83 years), and over 60% were racial or ethnic minorities (Table 1). Participants reported an average of 3.5 (±2.0) incontinence episodes/day at baseline, with over 60% having urgency-predominant incontinence. No significant between-group differences in baseline participant characteristics were detected.
Table 1:
Baseline Participant Characteristics, by Intervention Assignment
| Yoga Group (N=28) | Control Group (N=28) | P-valuea | |
|---|---|---|---|
| Demographic history | |||
| Race/ethnicity | 0.96 | ||
| Married | 10 (36%) | 11 (39%) | 0.78 |
| Gynecologic history | |||
| General medical history | |||
| Health-related habits | |||
| Physical and mental function scores | |||
| Physical exam measures | |||
| Clinical incontinence type |
0.71 |
||
| Incontinence frequency (episodes/day) | |||
| Incontinence duration |
0.37 |
||
| Urinary symptom questionnaire scores | |||
Data are presented as mean (± standard deviation), number (percentage), or range.
P-values were calculated using t-tests or chi-square or Fisher’s exact tests, as appropriate.
Data were missing for 1 participant for arthritis, 1 for diabetes, 1 for heart disease, 1 for lung disease, 1 for systolic blood pressure, and 1 for diastolic blood pressure.
Among women completing the 3-month yoga program, 89% attended at least 20 group classes, and 44% attended all 24 classes (Table 2). Over 90% of women completing the yoga program documented completion of at least 9 home practice hours, and over 80% reported completing all 12 recommended home practice hours. No significant between-group differences in adherence were detected.
Table 2:
Intervention Adherence and Process Outcomes, by Intervention Assignment
| Yoga Group (N=27)a | Control Group (N=23)a | P-valueb | |
|---|---|---|---|
| Adherence to group intervention classesc | |||
| Attended 24 group classes (100% adherence) | 12 (44%) | 11 (48%) | 0.81 |
| Attended 20 to 23 group classes (>80% but <100% adherence) | 12 (44%) | 9 (39%) | 0.70 |
| Attended 19 or fewer group classes (>80% adherence) | 3 (11.11%) | 3 (13%) | 0.83 |
| Adherence to home intervention practicec | |||
| Completed all 12 recommended home practice hours (100% adherence) | 22 (82%) | 15 (65%) | 0.19 |
| Completed 10–11 recommended home practice hours (>80% but <100% adherence) | 2 (7.4%) | 5 (22%) | 0.23 |
| Completed <10 recommended home practice hours <80% adherence) | 3 (11%) | 3 (13%) | 0.83 |
| Participant-reported self-confidence in performing postures or exercisesd | |||
| Very/extremely confident in performing all postures or exercises | 6 (22%) | 15 (65%) | 0.002 |
| At least moderately confident in performing all postures or exercises | 20 (74%) | 20 (87%) | 0.26 |
| Independent assessment of participants’ ability to perform postures or exercisese | |||
| Rated by expert consultant as being very/extremely successful in executing all postures or exercises | 3 (13%) | 20 (100%) | <0.001 |
| Rated by expert consultant as being at least moderately successful in executing all postures or exercises | 22 (96%) | 20 (100%) | 0.35 |
| Participant-reported ease of continuing to practice postures or exercisesf | |||
| Very easy to continue to practice yoga or stretching/strengthening to reduce urinary incontinence | 15 (55%) | 9 (41%) | 0.31 |
| At least moderately easy to continue to practice yoga or stretching/strengthening exercises to reduce urinary incontinence | 22 (81%) | 16 (73%) | 0.46 |
Data are presented as number (percentage). Percentages are column percentages.
Adherence outcomes assessed among participants who completed the 12-week intervention program (27 in the yoga group, 23 in the muscle stretching/strengthening group)
P-values comparing intervention adherence and process outcomes between groups were calculated by Fisher’s exact tests
Adherence to group classes was assessed by attendance logs kept the class instructors, while adherence to home practice was assessed by diaries in which participants recorded the dates and times of their home intervention practice.
Participants in both intervention groups were asked during the last week of their 3-month intervention program to rate their confidence in performing each yoga posture or stretching/strengthening exercise on a 5-point Likert scale (not at all, slightly, moderately, very, or extremely confident).
An expert consultant visited the final group class of each intervention program and independently rated each participant’s success in performing each yoga posture or muscle stretching/strengthening exercise on a 5-point Likert scale (not at all, slightly, moderately, very, or extremely successful). Data were missing for 4 participants in the yoga group and 3 in the control group who were missed the session in which this assessment was performed.
Participants in both intervention groups were asked during the last week of their 3-month intervention program to indicate how easy it would be to continue practicing their assigned to improve their incontinence on a 5-point Likert scale (very easy, moderately easy, neither difficult nor easy, moderately difficult, very difficult). Data were missing for one participant in the control group.
At the end of the 3-month yoga program, 91% of yoga participants indicated that they were at least “moderately” confident and 26% were at least “very” confident of their ability to perform all postures in the program (Table 2). Of the women who underwent evaluation by an expert yoga consultant at the end of the program, 96% were rated as being at least “moderately” successful and 13% as at least “very” successful in performing all observed postures.
Forty-eight adverse events were reported (Table 3), including 8 events in the yoga group and 7 events in the control group that were musculoskeletal symptoms or injuries. However, none of these events occurred during practice of yoga or control exercises or were attributed by participants to either intervention. No serious adverse events defined by death, disability, or hospitalization were detected.
Table 3.
Adverse Events, by Intervention Group
| Yoga Group N=28 | Control Group N=28 | P-valuea | |
|---|---|---|---|
| Total number of adverse eventsb reported | 23 | 25 | 0.77 |
| Number of participants with at least one adverse eventb | 17 | 14 | 0.59 |
| Total number of adverse events by body/organ system | |||
| Gastrointestinal adverse events | 0 | 2 | 0.16 |
| Genitourinary adverse events | 1 | 0 | 0.32 |
| Musculoskeletal adverse events | 9 | 8 | 0.80 |
| Neurological or psychological adverse events | 4 | 4 | 1.00 |
| Ophthalmologic adverse events | 1 | 3 | 0.32 |
| Respiratory or sinus adverse events | 8 | 9 | 0.80 |
| Number of participants with an adverse event by body system | |||
| Gastrointestinal adverse events | 0 | 2 | 0.16 |
| Genitourinary adverse events | 1 | 0 | 0.32 |
| Musculoskeletal adverse events | 8 | 7 | 0.80 |
| Neurological or psychological adverse events | 4 | 4 | 1.00 |
| Ophthalmologic adverse events | 1 | 3 | 0.32 |
| Respiratory or sinus adverse events | 8 | 9 | 0.80 |
| Total number of serious adverse eventsc | 0 | 0 | 1.00 |
| Number of participants with serious adverse eventsc | 0 | 0 | 1.00 |
P-values for between-group differences in adverse events were calculated from chi-square goodness-of-fit tests.
Adverse events were assessed at each study visit or phone call by asking participants to report any negative changes in health since their last visit or call, regardless of relationship to study participation.
Serious adverse events were defined by the standard definition of death, life-threatening event, hospitalization, or permanent disability
Over 3 months, total incontinence frequency decreased by an estimated 76% from baseline in the yoga group and 56% from baseline in the control group (P=.072 for between-group difference, Table 4). Stress incontinence frequency decreased by an average of 61% in the yoga group and 35% in the control group (P=.045), and urgency incontinence frequency decreased by an average of 30% in the yoga group and 17% in the control group (P=.77). Scores on the IIQ, UDI-6, and PPBC measures improved in both groups, but no significant between-group differences were detected (Table 4). In per protocol analyses, estimated effects were similar, but the between-group difference in change in stress-type incontinence was no longer significant (p=.06, Appendix B).
Table 4.
Average Change in Daily Urinary Incontinence Frequency and Incontinence-Related Quality of Life after 3 Months, by Intervention Assignment
| Yoga Group | Control Group | P-Value for Between-Group Difference | ||||
|---|---|---|---|---|---|---|
| Absolute change (95% CI) | Percent change (95% CI) | Absolute change (95% CI) | Percent change (95% CI) | Absolute change | Percent change | |
| Incontinence frequency | ||||||
| Total (any) incontinence | −2.8 (−3.6, −2.0) | −76% (−90%, −61%) | −1.9 (−2.8, −0.9) | −56% (−72%, −41%) | 0.13 | 0.07 |
| Stress-type incontinence | −0.8 (−1.2, −0.4) | −61% (−78%, −43%) | −0.4 (−0.9, 0.1) | −35% (−55%, −16%) | 0.18 | 0.045 |
| Urgency-type incontinence | −1.7 (−2.6, −0.91) | −30% (−91%, 32%) | −1.7 (−2.6, −0.7) | −17% (−81%, 48%) | 0.89 | 0.77 |
| Total daytime incontinence | −2.5 (−3.3, −1.8) | −71% (−81%, −61%) | −1.6 (−2.5, −0.8) | −55% (−65%, −44%) | 0.13 | 0.02 |
| Total nighttime incontinence | −0.3 (−0.5, −0.1) | −36% (−54%, −18%) | −0.2 (−0.5, 0.0) | −24% (−44%, −5.0%) | 0.74 | 0.39 |
| Incontinence-related quality of life scores | ||||||
| Incontinence Impact Questionnaire | −74 (−103, −45) | −66% (−76%, −55%) | −94 (−127, −60) | −64% (−75%, −53%) | 0.39 | 0.85 |
| Urogenital Distress Inventory-6 | −21 (−27, −15) | −53% (−67%, −40%) | −15 (−23, −8) | −37% (−52%, −23%) | 0.24 | 0.11 |
| Patient Perception of Bladder Condition | −1.3 (−1.7, −0.8) | −33% (−47%, −19%) | −1.0 (−1.5, −0.5) | −21% (−36%, −5.6%) | 0.46 | 0.22 |
For incontinence frequency outcomes, absolute change is presented as change in the number of incontinence episodes per day, and percent change is presented as percent change from baseline. For incontinence quality of life measures outcomes, absolute change is presented as change in questionnaire scores, and percent change presented as percent change in scores from baseline. Least square mean estimates and confidence intervals were derived from analysis of covariance models, using multiple imputation to address missing data; models examining absolute change adjusted for baseline levels of outcomes.
Comment
In this randomized trial of a group-based yoga program for urinary incontinence, over 95% of women assigned to yoga completed the 3-month program, and over 80% attended at least 80% of group classes and home practice sessions. Based on both self-assessment and expert evaluation, over 90% were at least moderately successful in learning to practice program-specific yoga techniques after 3 months. Women in the yoga group also demonstrated an over 75% average improvement in incontinence frequency over 3 months, although those assigned to the non-specific muscle stretching/strengthening control group also demonstrated an over 55% reduction in incontinence frequency.
Overall, these results provide promising evidence of the feasibility and tolerability of yoga as a complementary behavioral self-management strategy for incontinence in ambulatory women. Findings also provide preliminary evidence that yoga practice may be associated with reductions in incontinence frequency, although benefits were also seen with the control intervention involving non-specific stretching/strengthening exercises. Results also raise the possibility of differential effects of yoga on stress- versus urgency-type incontinence, although small numbers limit the reliability of type-specific incontinence effects.
Despite efforts to improve diagnosis and treatment for incontinence, studies show that many incontinent women go without treatment, either because they do not report their symptoms, do not have access to a healthcare provider who is willing and able to treat incontinence, or cannot tolerate conventional treatments.53–56 Yoga may be useful for incontinent women in the community who lack access to incontinence specialists, are unable to use clinical therapies, or wish to enhance conventional care. Since yoga can be practiced in a group setting without continuous supervision by healthcare specialists, it offers a potentially cost-effective, community-based self-management strategy for incontinence, provided that it can be taught with appropriate attention to safety and to patients’ clinical needs.
Although yoga has been incorporated into treatment programs for other health conditions such as low back pain or cancer-related symptoms,57–62 there are currently no evidence-based yoga programs for incontinence. Several uncontrolled studies have reported beneficial effects of yoga on urinary symptoms in other populations, including a yoga program in adults with multiple sclerosis resulting in neurogenic bladder63 and a combination pelvic muscle exercise and Yin-Yang yoga program in Korean women with incontinence.64 Our own group previously reported a 70% average decrease in incontinence frequency among women taking part in a 6-week version of the yoga program featured in this report.35 In contrast, a recent pilot trial of a mindfulness-based stress reduction (MBSR) program versus yoga control among 24 women with incontinence reported greater benefits associated with MBSR than yoga.65
Limitations of this trial include its modest size, which was not designed for detection of between-group differences in efficacy outcomes. Additionally, this trial was conducted at only one location, even though generalizability was increased by the use of multiple instructors over several intervention waves. This study also focused on ambulatory women without complex urologic histories, and the feasibility, tolerability, and efficacy of yoga may differ for women with limited mobility or medically/surgically complicated incontinence. Importantly, this study featured an Iyengar/alignment-based yoga program designed specifically for incontinent women, and the feasibility, tolerability, and efficacy of other yoga styles may differ.
This trial also featured an active control intervention involving training and practice of non-specific muscle stretching and strengthening exercises. Although this provided a rigorous time-and-attention control for yoga, it may have offered meaningful benefits for incontinence, which is not surprising given that physical deconditioning is a known contributor to incontinence in older adults.30,31
Overall, these findings support the feasibility and tolerability of a group-based yoga program for urinary incontinence in ambulatory women and provide evidence of reduction in incontinence frequency associated with yoga practice. Multicenter, extended trials may be indicated to provide more definitive evidence of whether yoga offers unique benefits in comparison to other physical activity-based interventions, confirm differential treatment effects by incontinence type, and evaluate for persistence of effects over time.
Acknowledgments
The investigators gratefully acknowledge the contributions of Ms. Leslie Howard and Dr. Judith Hanson Lasater as the expert yoga consultants for this study, who developed the content of the study yoga program and evaluated participants’ ability to perform the study yoga postures and techniques in collaboration with the other members of the research team.
We also gratefully acknowledge the efforts of Ms. Traci Plaut, Ann Chang, and Lisa Abinanti in overseeing participant recruitment and follow-up, data collection, data cleaning, and data management for this research, as study personnel employed by the University of California San Francisco.
Funding for all authors and individuals named in the Acknowledgements section was provided by grant #R34AT008028 from the National Center for Complementary and Integrative Medicine and from the University of California San Francisco Osher Center for Integrative Medicine’s Bradley fund. Dr. Leslee Subak was also supported by grant #5K24DK080775 from the National Institute of Diabetes and Digestive and Kidney Disorders.
Drs. Alison Huang and Leslee Subak have received funding from Pfizer Inc. and Astellas through grants awarded to the University of California San Francisco to conduct research unrelated to this report. Ms. Leslie Howard and Dr. Judith Hanson Lasater are professional yoga teachers who are privately employed in teaching yoga for health-related indications, including pelvic health conditions. No other potential conflicts of interest are reported by the authors or by individuals named in the Acknowledgements.
Research funding: This study was supported by National Center for Complementary and Integrative Medicine grant #R34AT008028 and the UCSF Osher Center for Integrative Medicine’s Bradley fund. Dr. Subak was also supported by grant #5K24DK080775 from the National Institute of Diabetes and Digestive and Kidney Disorders.
ClinicalTrials.gov Identifier: NCT02342678 (https://clinicaltrials.gov/ct2/show/NCT02342678)
Appendix A. Yoga postures featured in the study yoga program:
Standing postures
Parsvokonasana (side angle pose)
Parsvottasana (intense side stretch pose)
Tadasana (mountain pose)
Trikonasana (triangle pose)
Utkatasana (chair pose)
Virabhadrasana 2 (warrior 2 pose).
Seated postures
Baddha Konasana (bounded angle pose)
Bharadvajasana (seated twist pose)
Malasana (squat pose)
Supine postures
Salamba Set Bandhasana (supported bridge pose)
Supta Baddha Konasana (reclined cobbler’s pose)
Supta Padagushthasana (reclined big toe pose)
Restorative postures
Savasana (corpse pose)
Viparita Karani Variation (legs up the wall pose)
Prone postures
Salabhasana (locust pose)
Appendix B.
Average Change in Daily Urinary Incontinence Frequency of Incontinence after 3 Months, by Intervention Assignment, Among Participants Completing the Intervention
| Yoga Group | Control Group | P-Value for Between-Group Difference | ||||
|---|---|---|---|---|---|---|
| Absolute change (95% CI) | Percent change (95% CI) | Absolute change (95% CI) | Percent change (95% CI) | Absolute change | Percent change | |
| Incontinence frequency | ||||||
| Total (any) incontinence | −2.8 (−3.7, −2.0) | −75% (−90%, −61%) | −1.8 (−2.7, −0.9) | −56% (−72%, −40%) | 0.09 | 0.07 |
| Stress-type incontinence | −0.8 (−1.3, −0.4) | −62% (−79%, −44%) | −0.3 (−0.8, 0.1) | −37% (−55%, −19%) | 0.13 | 0.06 |
| Urgency-type incontinence | −1.8 (−2.6, −0.9) | −33% (−94%, 26%) | −1.6 (−2.5, −0.7) | −22% (−94%, 26%) | 0.76 | 0.80 |
| Total daytime incontinence | −2.5 (−3.3, −1.8) | −72% (−81%, −62%) | −1.6 (−2.4, −0.7) | −55% (−81%, −62%) | 0.09 | 0.02 |
| Total nighttime incontinence | −0.3 (−0.5, −0.1) | −37% (−55%, −18%) | −0.2 (−0.4, 0.0) | −24% (−44%, −4.0%) | 0.62 | 0.36 |
For incontinence frequency outcomes, absolute change is presented as change in the number of incontinence episodes per day, and percent change is presented as percent change from baseline. Least square mean estimates and confidence intervals were derived from analysis of covariance models. Only participants who completed the 3-month intervention and provided 3-month follow-up data are included in these exploratory “per protocol” analyses.
Footnotes
Conflicts of interest: Drs. Huang and Subak have received funding from Pfizer Inc. and Astellas through grants awarded to the University of California San Francisco (UCSF) to conduct research unrelated to this report. No other authors report any potential conflicts of interest.
Presentations: This research was presented as a podium presentation at the American Urological Association’s annual scientific meeting in San Francisco in May, 2018.
References
- 1.Melville JL, Katon W, Delaney K, Newton K. Urinary incontinence in US women: a population-based study. Arch Intern Med. 2005;165(5):537–542. [DOI] [PubMed] [Google Scholar]
- 2.Thom DH, van den Eeden SK, Ragins AI, et al. Differences in prevalence of urinary incontinence by race/ethnicity. J Urol. 2006;175(1):259–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thom DH, Haan MN, Van Den Eeden SK. Medically recognized urinary incontinence and risks of hospitalization, nursing home admission and mortality. Age Ageing. 1997;26(5):367–374. [DOI] [PubMed] [Google Scholar]
- 4.Langa KM, Fultz NH, Saint S, Kabeto MU, Herzog AR. Informal caregiving time and costs for urinary incontinence in older individuals in the United States. J Am Geriatr Soc. 2002;50(4):733–737. [DOI] [PubMed] [Google Scholar]
- 5.Fultz NH, Fisher GG, Jenkins KR. Does urinary incontinence affect middle-aged and older women’s time use and activity patterns? Obstet Gynecol. 2004;104(6):1327–1334. [DOI] [PubMed] [Google Scholar]
- 6.Sampselle CM, Harlow SD, Skurnick J, Brubaker L, Bondarenko I. Urinary incontinence predictors and life impact in ethnically diverse perimenopausal women. Obstet Gynecol. 2002;100(6):1230–1238. [DOI] [PubMed] [Google Scholar]
- 7.Bogner HR. Urinary incontinence and psychological distress in community-dwelling older African Americans and whites. J Am Geriatr Soc. 2004;52(11):1870–1874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brown JS, Vittinghoff E, Wyman JF, et al. Urinary incontinence: does it increase risk for falls and fractures? Study of Osteoporotic Fractures Research Group. J Am Geriatr Soc. 2000;48(7):721–725. [DOI] [PubMed] [Google Scholar]
- 9.Fultz NH, Herzog AR. Self-reported social and emotional impact of urinary incontinence. J Am Geriatr Soc. 2001;49(7):892–899. [DOI] [PubMed] [Google Scholar]
- 10.Bump RC, Hurt WG, Fantl JA, Wyman JF. Assessment of Kegel pelvic muscle exercise performance after brief verbal instruction. Am J Obstet Gynecol. 1991;165(2):322–327; discussion 327–329. [DOI] [PubMed] [Google Scholar]
- 11.Borello-France D, Burgio KL, Goode PS, et al. Adherence to behavioral interventions for urge incontinence when combined with drug therapy: adherence rates, barriers, and predictors. Physical therapy. 2010;90(10):1493–1505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Milne JL, Moore KN. Factors impacting self-care for urinary incontinence. Urologic nursing. 2006;26(1):41–51. [PubMed] [Google Scholar]
- 13.Borello-France D, Burgio KL, Goode PS, et al. Adherence to behavioral interventions for stress incontinence: rates, barriers, and predictors. Physical therapy. 2013;93(6):757–773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gopal M, Haynes K, Bellamy SL, Arya LA. Discontinuation rates of anticholinergic medications used for the treatment of lower urinary tract symptoms. Obstet Gynecol. 2008;112(6):1311–1318. [DOI] [PubMed] [Google Scholar]
- 15.Diokno A, Yuhico M, Jr. Preference, compliance and initial outcome of therapeutic options chosen by female patients with urinary incontinence. J Urol. 1995;154(5):1727–1730; discussion 1731. [PubMed] [Google Scholar]
- 16.Shamliyan T, Wyman J, Kane RL. Nonsurgical Treatments for Urinary Incontinence in Adult Women: Diagnosis and Comparative Effectiveness. Rockville MD: 2012. [PubMed] [Google Scholar]
- 17.Sultana CJ, Campbell JW, Pisanelli WS, Sivinski L, Rimm AA. Morbidity and mortality of incontinence surgery in elderly women: an analysis of Medicare data. Am J Obstet Gynecol. 1997;176(2):344–348. [DOI] [PubMed] [Google Scholar]
- 18.Michalsen A, Grossman P, Acil A, et al. Rapid stress reduction and anxiolysis among distressed women as a consequence of a three-month intensive yoga program. Med Sci Monit. 2005;11(12):CR555–561. [PubMed] [Google Scholar]
- 19.Rao MR, Raghuram N, Nagendra HR, et al. Anxiolytic effects of a yoga program in early breast cancer patients undergoing conventional treatment: a randomized controlled trial. Complement Ther Med. 2009;17(1):1–8. [DOI] [PubMed] [Google Scholar]
- 20.Beddoe AE, Paul Yang CP, Kennedy HP, Weiss SJ, Lee KA. The effects of mindfulness-based yoga during pregnancy on maternal psychological and physical distress. Journal of obstetric, gynecologic, and neonatal nursing : JOGNN / NAACOG. 2009;38(3):310–319. [DOI] [PubMed] [Google Scholar]
- 21.Damodaran A, Malathi A, Patil N, Shah N, Suryavansihi, Marathe S. Therapeutic potential of yoga practices in modifying cardiovascular risk profile in middle aged men and women. J Assoc Physicians India. 2002;50(5):633–640. [PubMed] [Google Scholar]
- 22.Udupa K, Madanmohan, Bhavanani AB, Vijayalakshmi P, Krishnamurthy N. Effect of pranayam training on cardiac function in normal young volunteers. Indian journal of physiology and pharmacology. 2003;47(1):27–33. [PubMed] [Google Scholar]
- 23.Vempati RP, Telles S. Yoga-based guided relaxation reduces sympathetic activity judged from baseline levels. Psychol Rep. 2002;90(2):487–494. [DOI] [PubMed] [Google Scholar]
- 24.Telles S, Nagarathna R, Nagendra HR, Desiraju T. Physiological changes in sports teachers following 3 months of training in Yoga. Indian J Med Sci. 1993;47(10):235–238. [PubMed] [Google Scholar]
- 25.Im HW, Kim MD, Kim JC, Choi JB. Autonomous nervous system activity in women with detrusor overactivity. Korean J Urol. 2010;51(3):183–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Choi JB, Kim YB, Kim BT, Kim YS. Analysis of heart rate variability in female patients with overactive bladder. Urology. 2005;65(6):1109–1112; discussion 1113. [DOI] [PubMed] [Google Scholar]
- 27.Hubeaux K, Deffieux X, Ismael SS, Raibaut P, Amarenco G. Autonomic nervous system activity during bladder filling assessed by heart rate variability analysis in women with idiopathic overactive bladder syndrome or stress urinary incontinence. J Urol. 2007;178(6):2483–2487. [DOI] [PubMed] [Google Scholar]
- 28.Chen KM, Fan JT, Wang HH, Wu SJ, Li CH, Lin HS. Silver yoga exercises improved physical fitness of transitional frail elders. Nurs Res. 2010;59(5):364–370. [DOI] [PubMed] [Google Scholar]
- 29.Fan JT, Chen KM. Using silver yoga exercises to promote physical and mental health of elders with dementia in long-term care facilities. Int Psychogeriatr. 2011;23(8):1222–1230. [DOI] [PubMed] [Google Scholar]
- 30.Brown JS, Seeley DG, Fong J, Black DM, Ensrud KE, Grady D. Urinary incontinence in older women: who is at risk? Study of Osteoporotic Fractures Research Group. Obstet Gynecol. 1996;87(5 Pt 1):715–721. [DOI] [PubMed] [Google Scholar]
- 31.Tinetti ME, Inouye SK, Gill TM, Doucette JT. Shared risk factors for falls, incontinence, and functional dependence. Unifying the approach to geriatric syndromes. JAMA. 1995;273(17):1348–1353. [PubMed] [Google Scholar]
- 32.Frawley J, Sibbritt D, Steel A, Chang S, Adams J. Complementary and Conventional Health-care Utilization Among Young Australian Women With Urinary Incontinence. Urology. 2017;99:92–99. [DOI] [PubMed] [Google Scholar]
- 33.Peng W, Adams J, Hickman L, Sibbritt DW. Association between consultations with complementary/alternative medicine practitioners and menopause-related symptoms: a cross-sectional study. Climacteric : the journal of the International Menopause Society. 2015;18(4):551–558. [DOI] [PubMed] [Google Scholar]
- 34.Slavin SL, Rogers RG, Komesu Y, et al. Complementary and alternative medicine (CAM) use in women with pelvic floor disorders: a cohort study. International urogynecology journal. 2010;21(4):431–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Huang AJ, Jenny HE, Chesney MA, Schembri M, Subak LL. A group-based yoga therapy intervention for urinary incontinence in women: a pilot randomized trial. Female Pelvic Med Reconstr Surg. 2014;20(3):147–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Locher JL, Goode PS, Roth DL, Worrell RL, Burgio KL. Reliability assessment of the bladder diary for urinary incontinence in older women. J Gerontol A Biol Sci Med Sci. 2001;56(1):M32–35. [DOI] [PubMed] [Google Scholar]
- 37.Brown JS, McNaughton KS, Wyman JF, et al. Measurement characteristics of a voiding diary for use by men and women with overactive bladder. Urology. 2003;61(4):802–809. [DOI] [PubMed] [Google Scholar]
- 38.Schulz KF, Grimes DA. Allocation concealment in randomised trials: defending against deciphering. Lancet. 2002;359(9306):614–618. [DOI] [PubMed] [Google Scholar]
- 39.Huang AJ, Grady D, Appa A, Subak LL. A pilot randomized trial of a behavioral slow-breathing intervention to treat urgency incontinence in women American Geriatrics Society Annual Scientific Meeting; May 4, 2012, 2012; Seattle, Washington. [Google Scholar]
- 40.Banasik J, Williams H, Haberman M, Blank SE, Bendel R. Effect of Iyengar yoga practice on fatigue and diurnal salivary cortisol concentration in breast cancer survivors. J Am Acad Nurse Pract. 2011;23(3):135–142. [DOI] [PubMed] [Google Scholar]
- 41.Evans S, Cousins L, Tsao JC, Sternlieb B, Zeltzer LK. Protocol for a randomized controlled study of Iyengar yoga for youth with irritable bowel syndrome. Trials. 2011;12:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Evans S, Cousins L, Tsao JC, Subramanian S, Sternlieb B, Zeltzer LK. A randomized controlled trial examining Iyengar yoga for young adults with rheumatoid arthritis: a study protocol. Trials. 2011;12:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Williams K, Abildso C, Steinberg L, et al. Evaluation of the effectiveness and efficacy of Iyengar yoga therapy on chronic low back pain. Spine. 2009;34(19):2066–2076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Williams KA, Petronis J, Smith D, et al. Effect of Iyengar yoga therapy for chronic low back pain. Pain. 2005;115(1–2):107–117. [DOI] [PubMed] [Google Scholar]
- 45.Kolasinski SL, Garfinkel M, Tsai AG, Matz W, Van Dyke A, Schumacher HR. Iyengar yoga for treating symptoms of osteoarthritis of the knees: a pilot study. J Altern Complement Med. 2005;11(4):689–693. [DOI] [PubMed] [Google Scholar]
- 46.Oken BS, Kishiyama S, Zajdel D, et al. Randomized controlled trial of yoga and exercise in multiple sclerosis. Neurology. 2004;62(11):2058–2064. [DOI] [PubMed] [Google Scholar]
- 47.Kanaya AM, Araneta MR, Pawlowsky SB, et al. Restorative yoga and metabolic risk factors: the Practicing Restorative Yoga vs. Stretching for the Metabolic Syndrome (PRYSMS) randomized trial. Journal of diabetes and its complications. 2014;28(3):406–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shumaker SA, Wyman JF, Uebersax JS, McClish D, Fantl JA. Health-related quality of life measures for women with urinary incontinence: the Incontinence Impact Questionnaire and the Urogenital Distress Inventory. Continence Program in Women (CPW) Research Group. Qual Life Res. 1994;3(5):291–306. [DOI] [PubMed] [Google Scholar]
- 49.Uebersax JS, Wyman JF, Shumaker SA, McClish DK, Fantl JA. Short forms to assess life quality and symptom distress for urinary incontinence in women: the Incontinence Impact Questionnaire and the Urogenital Distress Inventory. Continence Program for Women Research Group. Neurourol Urodyn. 1995;14(2):131–139. [DOI] [PubMed] [Google Scholar]
- 50.Coyne KS, Matza LS, Kopp Z, Abrams P. The validation of the patient perception of bladder condition (PPBC): a single-item global measure for patients with overactive bladder. Eur Urol. 2006;49(6):1079–1086. [DOI] [PubMed] [Google Scholar]
- 51.Matza LS, Thompson CL, Krasnow J, Brewster-Jordan J, Zyczynski T, Coyne KS. Test-retest reliability of four questionnaires for patients with overactive bladder: the overactive bladder questionnaire (OAB-q), patient perception of bladder condition (PPBC), urgency questionnaire (UQ), and the primary OAB symptom questionnaire (POSQ). Neurourol Urodyn. 2005;24(3):215–225. [DOI] [PubMed] [Google Scholar]
- 52.SAS. SAS/STAT® 9.2 User’s Guide. 2008. [Google Scholar]
- 53.Burgio KL, Ives DG, Locher JL, Arena VC, Kuller LH. Treatment seeking for urinary incontinence in older adults. J Am Geriatr Soc. 1994;42(2):208–212. [DOI] [PubMed] [Google Scholar]
- 54.Huang AJ, Brown JS, Kanaya AM, et al. Quality-of-life impact and treatment of urinary incontinence in ethnically diverse older women. Arch Intern Med. 2006;166(18):2000–2006. [DOI] [PubMed] [Google Scholar]
- 55.Dugan E, Roberts CP, Cohen SJ, et al. Why older community-dwelling adults do not discuss urinary incontinence with their primary care physicians. J Am Geriatr Soc. 2001;49(4):462–465. [DOI] [PubMed] [Google Scholar]
- 56.Shaw C, Tansey R, Jackson C, Hyde C, Allan R. Barriers to help seeking in people with urinary symptoms. Fam Pract. 2001;18(1):48–52. [DOI] [PubMed] [Google Scholar]
- 57.Tilbrook HE, Cox H, Hewitt CE, et al. Yoga for chronic low back pain: a randomized trial. Ann Intern Med. 2011;155(9):569–578. [DOI] [PubMed] [Google Scholar]
- 58.Sherman KJ, Cherkin DC, Erro J, Miglioretti DL, Deyo RA. Comparing yoga, exercise, and a self-care book for chronic low back pain: a randomized, controlled trial. Ann Intern Med. 2005;143(12):849–856. [DOI] [PubMed] [Google Scholar]
- 59.Vempati R, Bijlani RL, Deepak KK. The efficacy of a comprehensive lifestyle modification programme based on yoga in the management of bronchial asthma: a randomized controlled trial. BMC Pulm Med. 2009;9:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Garfinkel MS, Singhal A, Katz WA, Allan DA, Reshetar R, Schumacher HR Jr. Yoga-based intervention for carpal tunnel syndrome: a randomized trial. JAMA. 1998;280(18):1601–1603. [DOI] [PubMed] [Google Scholar]
- 61.Patel C 12-month follow-up of yoga and bio-feedback in the management of hypertension. Lancet. 1975;1(7898):62–64. [DOI] [PubMed] [Google Scholar]
- 62.Patel C, North WR. Randomised controlled trial of yoga and bio-feedback in management of hypertension. Lancet. 1975;2(7925):93–95. [DOI] [PubMed] [Google Scholar]
- 63.Patil NJ, Nagaratna R, Garner C, Raghuram NV, Crisan R. Effect of integrated Yoga on neurogenic bladder dysfunction in patients with multiple sclerosis-A prospective observational case series. Complementary therapies in medicine. 2012;20(6):424–430. [DOI] [PubMed] [Google Scholar]
- 64.Kim GS, Kim EG, Shin KY, Choo HJ, Kim MJ. Combined pelvic muscle exercise and yoga program for urinary incontinence in middle-aged women. Japan journal of nursing science : JJNS. 2015. [DOI] [PubMed] [Google Scholar]
- 65.Baker J, Costa D, Guarino JM, Nygaard I. Comparison of mindfulness-based stress reduction versus yoga on urinary urge incontinence: a randomized pilot study. with 6-month and 1-year follow-up visits. Female Pelvic Med Reconstr Surg. 2014;20(3):141–146. [DOI] [PubMed] [Google Scholar]