Abstract
Background:
Electronic health record-based portal tools may help patients engage in advance care planning (ACP). We designed and implemented portal-based ACP tools to enable patients to create a Medical Durable Power of Attorney (MDPOA).
Intervention:
Stakeholder-informed portal-based ACP tools including an electronic MDPOA form, patient educational webpage, online messaging, and patient access to completed advance directives.
Measures:
MDPOA documentation and System Usability Scale.
Outcomes:
2814 patients used the tools over 15 months. Patients were mean age 45 years (17 to 98 years) and 69% were women. 89% completed an MDPOA form, 2% called or sent online messages, and 8% viewed the MDPOA form but did not complete it. The tools were rated highly usable.
Conclusions:
Patients demonstrated willingness to use the portal to complete an MDPOA and rated the new ACP tools as highly usable. Future work will optimize population-based outreach strategies to engage patients in ACP through the portal.
Keywords: advance care planning, advance directive, surrogate decision maker, patient portal, health information technology, electronic health record
Background
Advance care planning (ACP) is a process that supports adults in understanding and sharing personal values, life goals, and preferences regarding future medical care.1 ACP is associated with improved quality of care at the end of life, more hospice use, less intensive care unit use, and fewer in-hospital deaths.2 Part of the ACP process is choosing a medical decision maker to make medical decisions when the person is no longer physically or mentally capable to make decisions on his or her own. However, rates of documenting a medical power of attorney, which is the legal process of designating a medical decision maker, remain low in the US, and availability of ACP documentation in electronic health records (EHRs) is limited.3
Web-based technologies may provide a person-centered and time-efficient method for engaging patients in ACP and documenting their preferences in the EHR.4 While there are shared decision making tools that engage patients in ACP, most of these tools or the resulting ACP documents are not linked to a patient’s EHR so that the patient’s preferences are accessible when patients and families need them.5 EHR-based patient portals can provide patient access to web-based education, engagement tools, and protected electronic patient-provider communication that together can lead to improved patient-centered care. Some healthcare systems have developed integrated ACP tools through EHR-based patient portals, though reported usage rates were low and none enable completion of an advance directive document. Additionally, other portals involve multiple steps to complete an advance directive including printing, signing, and then bringing a physical copy to the healthcare system for storage in the EHR.6–8
In Colorado, individuals can appoint a medical durable power of attorney (MDPOA) with a state-specific advance directive form that has legal standing and does not require witnesses or a notary. Therefore, we designed and implemented portal-based ACP tools to facilitate opportunities for patient engagement related to ACP, including a) providing educational materials about ACP, b) creating a legal advance directive, specifically the MDPOA form that appoints a medical decision maker, and c) storing the MDPOA form in the EHR. We describe the process of incorporating multi-level stakeholder input into the design of the portal-based ACP tools, a phased implementation into the healthcare system, and an evaluation of the tools for usability and lessons learned related to implementation.
Design
Setting
This quality improvement initiative was conducted within UCHealth, an academic-community health system in multiple geographic regions that includes ten hospitals and more than 300 ambulatory practices. UCHealth provides more than 2 million patient visits annually and serves approximately 286,000 patients who use My Health Connection, UCHealth’s name for the patient portal integrated with the EHR. UCHealth uses the Epic EHR (Epic Systems, version 2017, Verona, WI). My Health Connection enables patients to view and update medical history, exchange messages with clinicians, schedule appointments, refill medications, view laboratory results, and view clinicians’ notes. Importantly, My Health Connection allows patients to electronically sign forms, such as consents for treatment. Additionally, My Health Connection has questionnaires that enable patients to provide information (i.e., standardized health history questions) to clinicians for review and integration into the EHR. Prior to this initiative, there were no ACP system-wide tools in My Health Connection. The Colorado Multiple Institutional Review Board approved this project.
Multi-level stakeholder engagement
The multidisciplinary project team included a geriatric primary care and palliative care physician (H.L.), a project coordinator (A.B.), and UCHealth Epic analysts. The team first presented the initiative to design and implement portal-based ACP tools (referred to as the “initiative”) to the My Health Connection Steering Committee, which approved it based on strong alignment with the healthcare system’s priorities and the availability of external funding to support program implementation related to patient portals. The team then engaged in gathering stakeholder input and reviewing existing literature related to patient portal tools, evidence-based or public-facing ACP educational resources, and state-specific advance directives. The team conducted more than 10 presentations and feedback sessions to understand key stakeholder preferences on a) design of the ACP tools (i.e., what functions or processes should be built), b) integration into clinical practice and operational systems, and c) promotion and outreach to patients and staff. Stakeholders included patients and family members, interprofessional healthcare members, legal counsel, health literacy experts, health information management, healthcare system leadership, and patient experience and marketing personnel. Input was collected through meeting notes and discussed at weekly team meetings for operationalization into the design and implementation of the initiative.
Intervention
The portal-based ACP tools include patient educational resources on a custom ACP webpage, ability for patients to send an online message to a centralized ACP Support Team, ability to complete and electronically sign a Colorado MDPOA form to appoint a legal healthcare agent, and ability to view advance directives in the EHR. In particular, the educational webpage in the portal provides links to three public educational resources (e.g., National Institute on Aging website, The Conversation Project, and PREPARE - www.prepareforyourcare.org).
The purpose of these resources is to help patients learn more about ACP and encourage them to have conversations about their preferences, complete the MDPOA form if they are ready, or be prepared to discuss ACP with their healthcare team. External educational resources were approved by patients, clinicians, legal counsel, health literacy, and patient experience representatives. A secure, online message enables patients to send questions to the ACP Support Team. Patients can also call a centralized telephone number. A patient-initiated questionnaire provides information about appointing a medical decision maker, shows the exact language of the legal MDPOA form, utilizes any existing medical decision maker data from the EHR, and allows the patient to choose a decision maker and add up to two alternative decision makers. The process creates a printable PDF of the MDPOA form with an electronic signature and date/time stamp. The decision maker data are displayed in a specific area of the EHR that is accessed by clinical teams. The ACP coordinator is notified of electronic MDPOA forms and briefly reviews the patient’s problem list and relevant clinical documentation for possible decision making incapacity, then sends a message to the patient to confirm receipt of the MDPOA form and sends a message to a primary healthcare provider to notify them that the patient completed the MDPOA form. For out-of-state patients, the message additionally notes that the MDPOA is valid for medical care received in Colorado.
Phased implementation
The ACP tools were introduced in three planned phases that were based on the sequential release of new functionality in the portal, as well as a fourth phase based on observations during the implementation process. Phase 1 (May 2, 2017) included the ACP webpage and ability to send an online message to the ACP Support Team. Phase 2 (July 11, 2017) included the electronic MDPOA form. The electronic MDPOA form was refined and approved by legal counsel, health literacy experts, and the healthcare system committee that reviews patient forms. Clinical implementation involved project team decisions on revocation language of prior MDPOA forms, location of the questionnaire in My Health Connection, and creation of new document storage types to ensure accurate reporting and storage of advance directives. Phase 3 (October 22, 2017) added patient ability to view advance directive documents stored in the EHR via the portal. Phase 4 (March, 12, 2018) modified the MDPOA form completion process to provide one additional step for patients to review the information for accuracy, as well as a verification step for patients to acknowledge their choice to execute the electronic MDPOA.
Measures and Evaluation
Multiple methods were used to understand patient use and usability of the ACP tools over the first 15 months of phased implementation. Chart abstraction included patient age, gender, and type of ACP tool used (i.e., MDPOA form, online message, viewing the MDPOA form but not completing it). The number of patients who viewed the MDPOA form but did not complete it is based on patients who started the MDPOA form completion process and chose “No, I do not wish to complete an MDPOA form” (which notified the ACP Support Team). Data is not available for total page visits to each ACP portal tool. Early in phase 2, a random subset of patients (n=11) who used the ACP tools were surveyed using the System Usability Scale (SUS). The SUS has known validity for samples as small as 5 participants, includes 10 statements that represent factors of perceived usability of tools based on a 5-point Likert scale (Supplemental Appendix).9 We contacted participants by phone and interviewees did not receive compensation for participating. Participation was voluntary. All surveys were conducted within four weeks of using the ACP tools. SUS was scored according to published guidelines, and graphically depicted to estimate a percentile rank based on the score.9 A percentile rank higher than 90% denotes likelihood to recommend the tools to someone else.
Outcomes
Stakeholder input
Patient priorities included integration as “routine care” rather than “end-of-life care”, using understandable language, and the ability to view, update, and upload existing advance directives through the patient portal. Providers preferred workflows for review of patient-entered MDPOA information into existing clinical sections of the EHR, monitoring of appropriate patient use of the MDPOA form, and provision of patient education, outreach, and support for ACP by healthcare staff. Healthcare system leaders preferred access to ACP information across different clinical settings, use of an MDPOA form aligned with legal statutes, use of language no higher than an 8th grade reading level, accurate reporting of ACP quality metrics, training and standardized use of ACP tools, and availability on a mobile App. On-going monitoring by the ACP Support Team during the initial phases resulted in the Phase 4 refinement to the MDPOA form process because multiple submissions within 24 hours were occasionally observed with the same or slightly corrected healthcare decision maker information (the revised process includes an additional step that may help serve as a check point and reduce resubmissions because of inaccuracy). The project team iteratively implemented as much of the input as possible, though not all input could be incorporated. For example, building the ACP tools into the portal mobile App is not yet available due to technical limitations. Additionally, legal advisors requested language aligned with state laws.
Patient use of tools
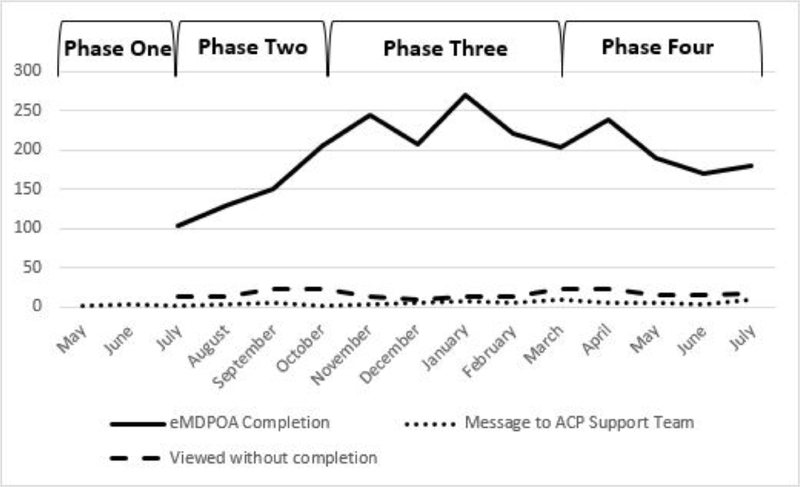
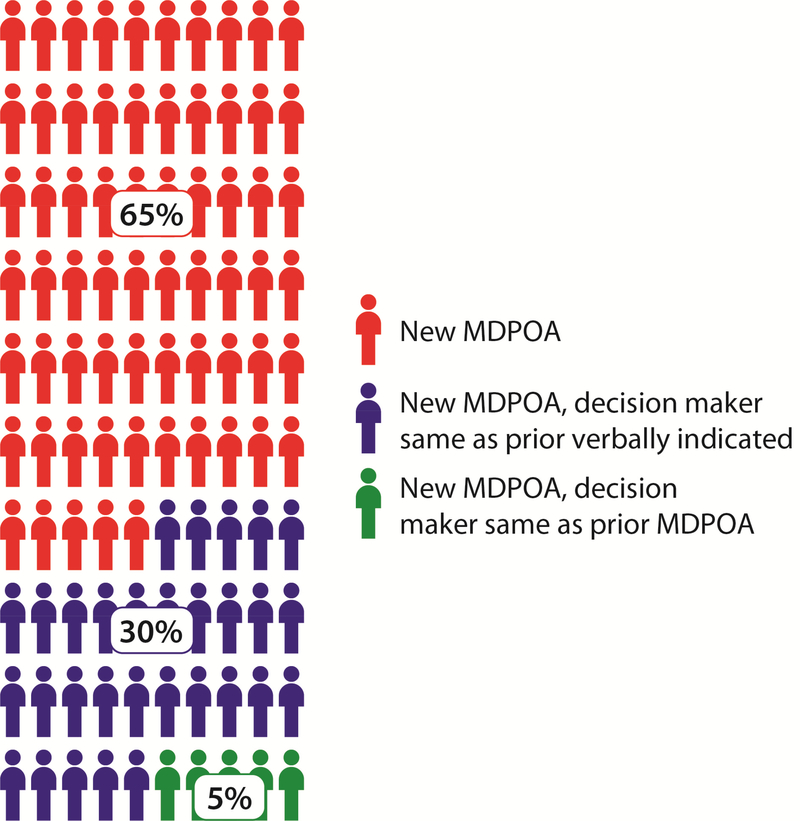
Over 15 months of phased implementation, 2814 patients used the portal-based ACP tools without any specific direct-to-patients announcement or clinic-based dissemination of the new tools. Patients had a mean age of 45 years, range of 17 to 98 years. Patients were mostly female (68%). Patients were from all three healthcare system regions within Colorado (31% north region, 42% metro Denver region, 23% south) and sixteen states (4% out of state). The number of unique patients and types of interactions with the ACP tools varied within each implementation phase (Figure 1), with six patients in phase 1, 584 patients in phase 2, 870 patients in phase 3, and 1354 patients in phase 4. Of patients who used the portal-based tools, 2514 (89%) users completed an MDPOA form, 69 (2%) called or sent online messages, and 219 (8%) viewed the MDPOA form but did not complete it (27 patients utilized two different parts). Over 92% of patients who completed the MDPOA form did not have a prior written advance directive naming a medical decision maker in the EHR, though approximately one-third had previously verbally indicated a decision maker in the EHR (Figure 2). Thirteen (0.5%) submitted an invalid MDPOA by selecting themselves as the decision maker or lacked decision making capacity as determined upon quality assurance review and discussion with a listed emergency contact. We did not collect data on the total number of decision makers, including alternates. The average usability ranking was very high (average score 89 out of 100) corresponding with a 100% ranking and an “A” grade, based on the SUS scores from 11 patients (Online Supplement Figure 1).
Figure 1. Patient interactions with advance care planning tools, by month.
Over four implementation phases, the number of patients per month who a) completed the electronic MDPOA (solid line), b) sent an online message to the Advance Care Planning Support team (dotted line), or c) viewed the MDPOA form without completing it (dashed line). MDPOA – Medical Durable Power of Attorney.
Figure 2. Patient selection of medical decision maker.
Of patients who completed an MDPOA form, 65% had no prior documentation of a medical decision maker, 30% documented the same person in the MDPOA form as had been verbally indicated, and 5% completed an MDPOA form with the same decision maker as previously documented in an MDPOA on file in the EHR. Colorado law recognizes verbal indication of a medical decision maker, the EHR has a designated area for healthcare providers to document a patient’s verbal choice. MDPOA – Medical Durable Power of Attorney; EHR – electronic health record
Key lessons from implementation
This quality improvement initiative resulted in several lessons learned. An important facilitator was initial external funding, which assisted with achieving strong clinical and operational support from the beginning. Additional key lessons included seeking legal and marketing team input early and iteratively; utilizing a phased implementation approach to ensure workflows were sufficient; communicating early and repeatedly with multiple clinical leadership teams and staff for introducing new patient portal tools; ongoing review of external website links to ensure functionality; and ensuring appropriate age restrictions and proxy access related to the MDPOA form process.
Discussion
This report describes the phased implementation of novel portal-based ACP tools in a large healthcare system to improve patient engagement in ACP. Importantly, more than 2500 patients appointed a legal medical decision maker by completing the electronic MDPOA form via the patient portal. For over two-thirds of these patients, there was no prior EHR documentation of a preferred medical decision maker. Patient users rated the tools as highly usable.
This study demonstrates the feasibility and usability of the ACP tools based on the actions and input from initial users. While the usability testing is highly favorable, ongoing and expanded assessment of patient acceptability, suggestions to increase usability, and potential impact on ACP conversations or future medical care is needed. Multiple stakeholders have expressed interest in future updates, including the ability for patients to upload existing advance directives via the portal and ensuring patient access through mobile technology. Although the ACP tools are available to all My Health Connection users in the healthcare system, future work should also focus on stakeholder engagement for specific dissemination plans to clinicians and clinical units to raise system-wide awareness of the tools.
This initiative has several limitations. Because it was conducted in one healthcare system with EHR-based patient portal tools that align with state-specific laws, the findings are not generalizable to other states. In particular, this process could be developed and implemented because Colorado does not require additional individuals, such as witnesses or a notary public, to also sign. Secure electronic solutions that enable multiple individuals to sign could address this barrier. Additionally, the findings are limited to patients who used the ACP tools (i.e., completed an electronic MDPOA, sent an online message, or viewed the MDPOA form but chose not to complete it), rather than all My Health Connection users. Specifically, we were not able to evaluate or interview any patients who found the ACP tools but did not take one of the above actions.
In conclusion, this initiative demonstrates the design, implementation, and use of portalbased ACP tools that were designed with multi-level stakeholder input. This initiative used a phased implementation process that allowed ongoing input and refinement to improve functionality and patient experience. This study focuses on the implementation outcome of patient usability from the patient perspective10; next steps should evaluate additional implementation outcomes including cost, sustainability, and the potential positive or negative impact on patient, providers, and clinical team workflows.
Supplementary Material
Acknowledgements
This project would not have been possible without the significant organizational support of multiple UCHealth leaders and champions. We specifically thank Josh Conrad, Leah Rusinek, and Sally Nietfeld for their work building and integrating the patient portal tools. Other key supporters include staff members of the Ambulatory Health Promotion and Office of Value-based Performance; the UCHealth Metro Palliative Care Clinical Champions; the UCHealth North Advance Directive Stakeholder Group; the UCHealth Patient and Family Advisory Council; Dr. Aimee English and A.F. Williams Family Medicine Clinic Patient and Family Advisory Council; Dr. Bennett Parnes and the Lone Tree Senior Care Clinic Patient and Family Advisory Council; UCHealth Practice Transformation Clinical Champions; Dr. Daniel Matlock and the ACCORDS Research Stakeholder Group; Alison Sorkin for UCHealth legal counsel; Monique McCollum for UCHealth health literacy expertise; and Kate Pittenger for the My Health Connection Steering Committee. We are also grateful to Dr. Jodi Holtrop and Ms. Elizabeth Staton for providing helpful input on early versions of this manuscript.
Funding/Support: This initiative is funded by The Colorado Health Foundation with additional support from the National Institute on Aging of the National Institutes of Health (K76AG054782) and the Colorado Clinical & Translational Sciences Institute (CCTSI) with the Development and Informatics Service Center (DISC) grant support (NIH/NCRR Colorado CTSI Grant Number UL1 RR025780) for use of REDCap-based data management.
Role of the Funder/Sponsor: The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Department of Veterans Affairs.
Footnotes
Conflict of Interest
All authors have no known conflicts of interest associated with this publication.
Data Availability: De-identified data is available to qualified individuals upon reasonable request.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Sudore RL, Lum HD, You JJ, et al. Defining Advance Care Planning for Adults: A Consensus Definition From a Multidisciplinary Delphi Panel. J Pain Symptom Manage. 2017;53(5):821–832.e821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Silveira MJ, Kim SY, Langa KM. Advance directives and outcomes of surrogate decision making before death. N Engl J Med. 2010;362(13):1211–1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yadav KN, Gabler NB, Cooney E, et al. Approximately One In Three US Adults Completes Any Type Of Advance Directive For End-Of-Life Care. Health Aff (Millwood). 2017;36(7):1244–1251. [DOI] [PubMed] [Google Scholar]
- 4.Chiarchiaro J, Arnold RM, White DB. Reengineering advance care planning to create scalable, patient- and family-centered interventions. JAMA. 2015;313(11):1103–1104. [DOI] [PubMed] [Google Scholar]
- 5.Austin CA, Mohottige D, Sudore RL, Smith AK, Hanson LC. Tools to Promote Shared Decision Making in Serious Illness: A Systematic Review. JAMA Intern Med. 2015;175(7):1213–1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bose-Brill S, Kretovics M, Ballenger T, et al. Testing of a tethered personal health record framework for early end-of-life discussions. Am J Manag Care. 2016;22(7):e258–263. [PubMed] [Google Scholar]
- 7.Tieu C, Chaudhry R, Schroeder DR, Bock FA, Hanson GJ, Tung EE. Utilization of Patient Electronic Messaging to Promote Advance Care Planning in the Primary Care Setting. Am J Hosp Palliat Care. 2016. [DOI] [PubMed] [Google Scholar]
- 8.Bajracharya AS, Crotty BH, Kowaloff HB, Safran C, Slack WV. Improving health care proxy documentation using a web-based interview through a patient portal. J Am Med Inform Assoc. 2016;23(3):580–587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sauro J Measuring Usability with the System Usability Scale (SUS). 2011; https://measuringu.com/sus/. Accessed January 8, 2018.
- 10.Proctor E, Silmere H, Raghavan R, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health. 2011;38(2):65–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.