Watch a video presentation of this article
The digital age has made the Internet an important source of health information. In a study by the Pew Research Center, approximately 60% of Americans sought health information online that was used for self‐diagnosis or to get more information about their disease.1 With the freedom and anonymity provided by the Internet, users are able to research their health topics and engage in a better‐informed decision‐making process. However, the hypothesis that whether the available material is sufficiently complete and accurate to support shared decision making has not been thoroughly investigated. Health Literacy, as defined by the Patient Protection and Affordable Care Act of 2010, Title V, is the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions.2 In the American Medical Association's review of health literacy and patient safety,3 it was found that literacy was a stronger predictor of health status than education, ethnicity, or socioeconomic status. People with limited health literacy, as defined by the review to have basic or below basic levels on the National Assessment of Adult Literacy survey,4 were susceptible to worse health care outcomes. It has also been shown that patient compliance to treatment is better when patient literacy is taken into account and explained in a way that the patient can comprehend.5 In a UK‐based study, patients with low health literacy (as defined by a scoring criteria adjudging comprehension based on instructions similar to those found on a bottle of aspirin) had a hazard ratio for all‐cause mortality of 1.4 (95% confidence interval: 1.15‐1.72) when compared against those with higher health literacy.6
Patients with chronic liver disease comprise a challenging patient cohort that forms a substantial portion of the global disease burden. Many basic facets of liver disease are also often misunderstood. For example, in a study of 401 patients with liver disease, only about 16% of patients were able to identify the maximum dose of acetaminophen or that many common analgesic medications such as Percocet contained acetaminophen.7 It was also noted that in people with hepatitis B, hepatitis C, and cirrhosis, simple but formal education sessions significantly improved patient knowledge about their liver diseases.8, 9, 10 Furthermore, in an assessment of knowledge among the residents of Melbourne on chronic hepatitis B, the majority was not able to identify their disease as a risk for cirrhosis and hepatocellular cancer.11 On the other hand, in patients who have undergone liver transplant, it was found that limited health literacy was often associated with more hospitalizations and poorer outcomes.12 This leads to the important task of identifying factors that can aid in improving health literacy among our liver disease patient cohort.
One of the determinants of health literacy is the capacity to obtain and process basic health information. Readability is the ease with which a reader can understand a written text. Readability determination is a vital yardstick for assessment of physician–patient communication. Numerous validated formulae take into account average sentence length, number of difficult words, percentage of unique words, and other similar metrics to determine the reading grade level for a given text. These tests evaluate text independent of its structure, relationship, or syntax. These are illustrated in Table 1. One of the earliest and most frequently used readability tests is the Flesch Reading Ease, devised by Rudolf Flesch in 1948. Flesch Reading Ease reports a score from 0 to 100, with 90 to 100 intended for 11‐year‐old students, 60 to 70 for 13‐ to 15‐year‐olds, and 0 to 30 best understood by university graduates. After adaptation by Peter Kincaid in 1975, called the Flesch‐Kincaid test, it became the Department of Defense standard, with military manuals requiring adherence to specified grade levels. The National Institutes of Health recommends that patient reading material be targeted for an audience below seventh grade.13 However, a study done by our group showed that the mean readability of online information on hepatitis B and C, cirrhosis, and hepatocellular cancer was close to tenth‐grade level.14 This study subdivided each article into different subsections and measured the readability. It was further shown that the treatment and symptoms subsections had the highest median grade levels of 10.8 (range 5.5‐16.1) and 10.4 (range 4.7‐17.9), respectively (Fig. 1). It is depicted that none of the subsections complied with the recommended reading grade level of up to seventh grade.
Table 1.
Formulae for Different Readability Grade Estimation Models for Differentiating Textual Information
| Readability Test | Formula | Description | Interpretation |
|---|---|---|---|
| Coleman‐Liau Index19 | = 0.0588L − 0.296S − 15.8 | Calculates the grade level based on the character length of the words and length of the sentences | |
| Flesch‐Kincaid20 | = (0.39 × ASL) + (11.8 × ASW) −15.59 | Grade level is calculated based on the word length of sentences and syllable length of the words | |
| New Dale‐Chall21 | = 0.1579 × PDW + 0.0496 × ASL + 3.6365 | Calculates based on the number of words not present in a predetermined list of words that a fourth‐grade student would know, as well as word length of sentences | Reported on a grade scale where a score of 11 is equivalent to reading material that is most suitable for those with an 11th‐grade education or higher |
| Gunning Fog22 | = 0.4 (ASL + PHW) | The readability is determined by the word length of sentences, as well as the number of words with >2 syllables | |
| SMOG23 | = 3 + | Difficulty of the text is determined by the number of words with >2 syllables | |
| Flesch‐Reading Ease24 | = 206.835 − (1.015 × ASL) − (84.6 × ASW) | Readability is determined by the word length of the sentences, as well as the syllable length of word | Reported on a scale of 0‐100, where 100 is considered very easy and 0 is considered very difficult, most suitable for those who have a fourth‐grade education and a college education, respectively |
Abbreviations: ASL, number of words divided by the number of sentences; ASW, number of syllables divided by the number of words; L, mean number of letters per 100 words; PDW, percentage of difficult words, which are words that are not on the list of words that a fourth‐grade American student can understand; PHW, number of three or more syllable words divided by the total number of words; PSW, number of words with 3 or more syllables in 10 consecutive sentences from the beginning, middle, and end of the text; S, mean number of sentences per 100 words; SMOG, Simple Measure of Gobbledygook.
Figure 1.
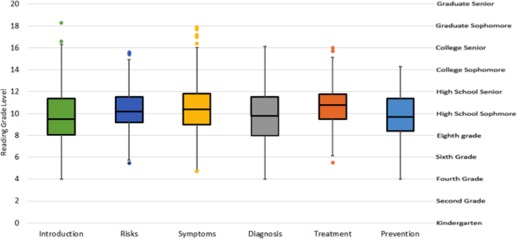
Box plot graph depicting the readability grade distribution of article subsections of sampled articles pertaining to hepatitis B, hepatitis C, cirrhosis, and hepatocellular carcinoma. None of the subsections conforms to the recommended readability of below the seventh grade. Reproduced with permission from European Journal of Gastroenterology & Hepatology.14 Copyright 2016, Wolters Kluwer Health.
It can be argued that limited health literacy can lead to increased health care resource utilization. In a study of approximately 93,000 veterans within the Veteran's Health Administration system, it was found that patients with inadequate/marginal health literacy (defined on scores attained on BRIEF health literacy screening tool) required roughly $32,000 in resources compared with $17,000 in those with adequate health literacy over a course of 3 years, totaling up to $143 million more in estimated expenditure.15 Moreover, inadequate health literacy, as measured by reading fluency, has also been associated with increased risk for mortality in the elderly population.16 This disparity was believed to be caused by inability to understand written instructions or follow through on recommendations in management of their health.
Studies demonstrating the impact of improved patient engagement and health literacy in liver disease remain sparse. In addition, there is a lack of large‐scale studies demonstrating differences in health‐resource utilization among patients with limited health literacy and those with adequate knowledge for liver diseases. It was shown in a small study that patients were more engaged during a nutrition evaluation when a questionnaire was presented to them with improved readability.17 Future areas of work should focus on characterizing impact of limited health literacy in liver diseases and measuring changes after simplifying patient‐directed information to a reasonable grade level. In this regard, language with simpler word structure and broad usage should be used. For example, simple and effective techniques include “often” can be used for “usually,” “make” for “develop,” “broadly” for “generally,” and so on. For guidance, many toolkits have been developed, such as those by Centers for Medicare & Medicaid, Agency for Healthcare Research and Quality.18
Potential conflict of interest: Nothing to report.
REFERENCES
- 1. Fox S, Duggan M. Health Online 2013. Published January 15, 2013. http://www.pewinternet.org/2013/01/15/health-online-2013
- 2.Patient Protection and Affordable Care Act, Title 5, 42 U.S.C. § 18001 (2010).
- 3. Weiss BD. Manual for Clinicians. American Medical Association Foundation and American Medical Association; 2007. Chicago, IL. [Google Scholar]
- 4. Kutner M, Greenberg E, Jin Y, Paulsen C. The health literacy of America's adults. Results from the 2003 National Assessment of Adult Literacy. Washington, DC: National Center for Education Statistics; 2006. https://nces.ed.gov/pubs2006/2006483.pdf [Google Scholar]
- 5. Rothman RL, DeWalt DA, Malone R, Bryant B, Shintani A, Crigler B, et al. Influence of patient literacy on the effectiveness of a primary care‐based diabetes disease management program. JAMA 2004;292(14):1711‐1716. [DOI] [PubMed] [Google Scholar]
- 6. Bostock S, Steptoe A. Association between low functional health literacy and mortality in older adults: longitudinal cohort study. BMJ 2012;344:e1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Saab S, Konyn PG, Viramontes MR, Jimenez MA, Grotts JF, Hamidzadah W, et al. Limited knowledge of acetaminophen in patients with liver disease. J Clin Transl Hepatol 2016;4(4):281‐287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Surjadi M, Torruellas C, Ayala C, Yee HF Jr, Khalili M. Formal patient education improves patient knowledge of hepatitis C in vulnerable populations. Dig Dis Sci 2011;56(1):213‐219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Volk ML, Fisher N, Fontana RJ. Patient knowledge about disease self‐management in cirrhosis. Am J Gastroenterol 2013;108(3):302‐305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Mohamed R, Ng CJ, Tong WT, Abidin SZ, Wong LP, Low WY. Knowledge, attitudes and practices among people with chronic hepatitis B attending a hepatology clinic in Malaysia: a cross sectional study. BMC Public Health 2012;12:601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Dahl TF, Cowie BC, Biggs BA, Leder K, MacLachlan JH, Marshall C. Health literacy in patients with chronic hepatitis B attending a tertiary hospital in Melbourne: a questionnaire based survey. BMC Infect Dis 2014;14:537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Serper M, Patzer RE, Reese PP, Przytula K, Koval R, Ladner DP, et al. Medication misuse, nonadherence, and clinical outcomes among liver transplant recipients. Liver Transpl 2015;21(1):22‐28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Iverson SA, Howard KB, Penney BK. Impact of internet use on health‐related behaviors and the patient‐physician relationship: a survey‐based study and review. J Am Osteopath Assoc 2008;108(12):699‐711. [PubMed] [Google Scholar]
- 14. Gulati R, Nawaz M, Pyrsopoulos NT. Comparative analysis of online patient education material pertaining to hepatitis and its complications. Eur J Gastroenterol Hepatol 2016;28(5):558‐566. [DOI] [PubMed] [Google Scholar]
- 15. Haun JN, Patel NR, French DD, Campbell RR, Bradham DD, Lapcevic WA. Association between health literacy and medical care costs in an integrated healthcare system: a regional population based study. BMC Health Serv Res 2015;15:249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Baker DW, Wolf MS, Feinglass J, Thompson JA, Gazmararian JA, Huang J. Health literacy and mortality among elderly persons. Arch Intern Med 2007;167(14):1503‐1509. [DOI] [PubMed] [Google Scholar]
- 17. Townsend MS, Sylva K, Martin A, Metz D, Wooten‐Swanson P. Improving readability of an evaluation tool for low‐income clients using visual information processing theories. J Nutr Educ Behav 2008;40(3):181‐186. [DOI] [PubMed] [Google Scholar]
- 18. Brega AG, Barnard J, Mabachi NM, Weiss BD, DeWalt DA, Brach C, et al. AHRQ Health Literacy Universal Precautions Toolkit. Rockville, MD: Agency for Healthcare Research and Quality; 2015. [Google Scholar]
- 19. Coleman M, Liau TL. A computer readability formula designed for machine scoring. J Appl Psychol 1975;60:283‐284. [Google Scholar]
- 20. Kincaid JP, Fishburne RP, Rogers RL, Chissom BS. Derivation of new readability formulas (automated readability index, fog count, and Flesch reading ease formula) for Navy enlisted personnel. Research Branch Report 8‐75. Memphis, TN: Naval Technical Training, U.S. Naval Air Station; 1975. [Google Scholar]
- 21. Chall JS, Dale E. Readability Revisited. 1995. Brookline Books/Lumen Editions, Cambridge, MA.
- 22. Gunning R. The Technique of Clear Writing, First Edition. McGraw‐Hill, 1971. New York, NY. [Google Scholar]
- 23. Scranton MA. SMOG grading: a readability formula by G. Harry McLaughlin. Manhattan, KS: Kansas State University, 1970. [Google Scholar]
- 24. Flesch R. The Art of Readable Writing. New York: Harper; 1949. [Google Scholar]


