ABSTRACT
Background
There are few studies describing remediation for unprofessional behavior in residents and faculty and none that assess the long-term impact of remediation.
Objective
We implemented a simulation-based personalized remediation program for unprofessional behavior in residents and faculty and collected assessments from participants and referring supervisors.
Methods
Residents and faculty were referred for unprofessional behaviors, including aggressive, condescending, and argumentative communication styles as well as an inability to read social cues. We had standardized patients recreate the scenarios that triggered the unprofessional behavior. After each scenario, participants reviewed a videotape of their performance, participated in guided self-reflection and feedback, and then iteratively practiced skills. In 2017, about 2 to 4 years after the intervention, we conducted structured phenomenological qualitative interviews until thematic saturation was reached. Transcripts were analyzed inductively for themes by 2 reviewers (J.G. and research assistant).
Results
Requests for interviews were sent to 16 residents, 8 faculty members, and 24 supervisors, including program directors. Nine remediation participants (38%) and 19 referring supervisors (79%) were interviewed. Sixteen supervisors reported no recurrence of unprofessional behavior in participants 2 to 4 years after the intervention, and participants identified behavioral strategies to reduce unprofessional behavior. Participants and respective supervisors reported similar themes of behavior changes that resulted in improved professional interaction with others.
Conclusions
A simulation-based personalized remediation program for unprofessional behavior, where faculty and residents practice behaviors with guided feedback, can lead to sustained positive behavior change in participants.
Introduction
Remedial training methods for physicians who struggle with unprofessional behavior are often ad hoc, are poorly described, and have unknown long-term results.1 While a 2011 report of the Association of American Medical Colleges survey concluded that medical simulation is being used to teach and assess students, residents, and practicing physicians in nearly all of the Accreditation Council for Graduate Medical Education core competencies, including professionalism, only 44% of medical schools and 19% of teaching hospitals reported using simulation for the remediation of professionalism.2 In 2012, a think tank of experts on professional behavior identified a need for the academic community to develop evidence-based interventions to remediate lapses in professional behavior.1
In this article, we describe the simulation-based remediation methodology used to address individual skill deficiencies in struggling residents and practicing physicians at the University of Colorado School of Medicine.3 The study assessed the long-term effect of simulation used for specific unprofessional behaviors in residents and faculty referred for remediation.
Methods
Setting and Participants
In 2017, about 2 to 4 years after the remediation intervention, a research assistant conducted structured telephone interviews with participants and their referring supervisors to assess perceptions of the remediation, impact on subsequent performance, sustainability of any described changes, and subsequent career outcomes. The interview guide was designed by 2 investigators (J.G. and E.M.A.) through an iterative consensus-building process and was conducted by a research assistant to allow for confidential responses (interview guide provided as online supplemental material). A phenomenological qualitative interview approach was chosen to obtain in-depth descriptions of the impact of the remediation and the perspectives of the participants and supervisors involved in the process. This qualitative approach allowed us to better understand the experience of the participants. Invitations to participate were sent to all 24 participants in the remediation simulation and to their supervisors. Participants did not know that the supervisors were invited to participate.
Description of the Intervention
From 2013 to 2015, remedial training was conducted at a simulation center, led by 2 physicians and a communication skills specialist with prior experience and successful outcomes in remedial training (the remediation team). Faculty and residents were referred by program directors, department chairs, or the office of professionalism, which receives and investigates reports of unprofessional behavior. Behaviors that triggered the need for a remediation intervention included aggressive, condescending, and argumentative communication styles; events resulting from these deficiencies; and the inability to read social cues. Referrals were substantiated with collateral information using multisource evaluations and verbal and e-mail reports from administrators, faculty, learners, and staff. The remediation team then met with each referred individual for 1 hour to review the person's performance history and perspectives on the performance challenges, events related to the referral, current impact on work performance, and prior attempts at behavior change. The interviewers attempted to identify and verify patterns of behavior and triggering events.
To prepare for the remediation, we designed cases and scenarios based on data we collected. Cases typically included interactions involving respectful dissent; managing disoriented or disruptive patients, family, and team members; providing feedback to challenging supervisors, peers, and learners; managing interdepartmental and interprofessional peer conflicts; and advocating for self, team, program, and resources further up the organizational chain.3 The scenarios were designed to replicate the situations that resulted in the referral and were vetted with the respective clinical departments for validity. We trained a core group of standardized patients who had been previously trained in advanced communication, feedback, and coaching skills on the scenario goals and portrayals.
Each remediation session lasted 10 to 15 minutes and included 3 to 4 simulated scenarios. Immediately after each scenario, the participant, remediation team, and standardized patient reviewed a video recording of the interaction. Participants were asked to openly reflect on their performance. Standardized patients and the remediation team provided focused and skill-based feedback with techniques participants could try in subsequent encounters. The participants also provided feedback and constructed action plans for an individual with a professionalism lapse similar to their own. This allowed the remediation team to assess the individual's skill retention and capacity for deeper reflection.
Following the remediation session, participants received a written summary of how to implement the recommendations in their clinical environment. The entire process took approximately 8 hours (a case example with sample recommendations is provided as online supplemental material).
The study was deemed exempt by the Colorado Multiple Institutional Review Board.
Outcomes and Analysis
Interviews were audiorecorded for transcription, and transcripts were deidentified prior to analysis. One investigator (J.G.) and 1 research assistant both independently developed an initial coding scheme, compared and identified common emergent categories to create a thematic framework, coded the transcripts independently, and met to compare results until agreement on final themes, subthemes, and codes was achieved. Similar themes and subthemes were paired between residents and faculty when possible, highlighting similarities and differences between these 2 groups. Interviews continued until saturation was reached. Final codes and themes were member checked and confirmed to be correct.
Results
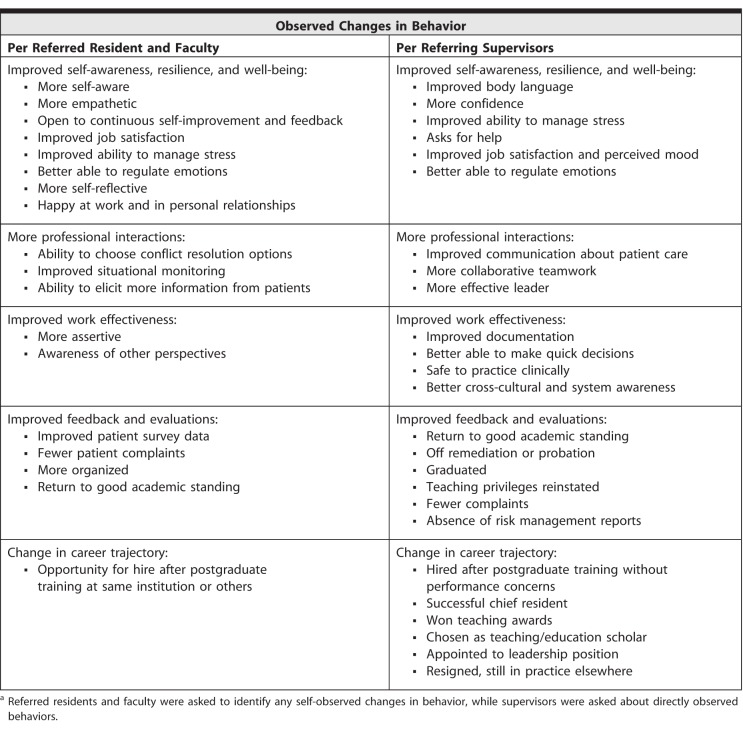
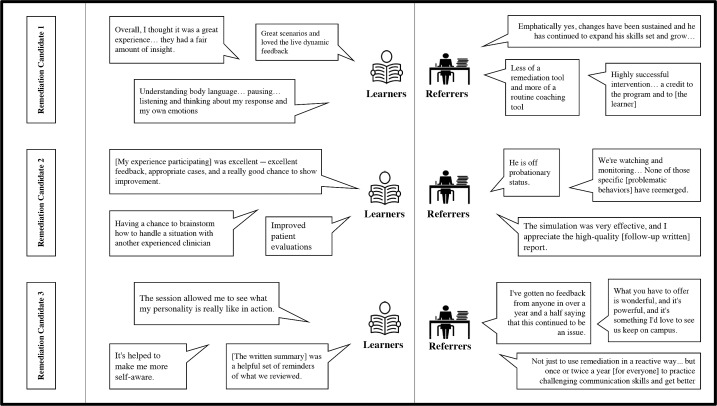
Nine participants (6 residents, 3 faculty; 38%) and 19 referring supervisors (1 dean, 11 residency program directors, 7 department chairs; 79%) participated in the guided interviews. While all interviewed individuals reflected positively on their experience at the simulation center, 3 (33%) acknowledged frustration that remediation was mandatory and described feeling targeted. All participants readily identified behavioral strategies acquired during the remediation and reported appreciation for and repeated use of the postintervention written summary. Participants and supervisors both reported similar changes in behavior as a result of the intervention (Table). The Figure includes paired comments from participants and supervisors.
Table.
Reported Observed Changes in Behavior After Intervention From Referred and Referrer Perspectivesa
Figure.
Paired Comments From Referred Individuals and Their Supervisors
Of the 19 supervisors interviewed, 16 reported that the participant had shown no recurrence of unprofessional behavior. Two reported that the participant had continued to demonstrate the same behaviors that resulted in his or her referral, and 1 reported improvement but not complete cessation of unprofessional behavior. Four referred individuals were hired following their postgraduate training and remained employed at the time of the interview. The supervisors identified 11 individuals for their subsequent achievements, with 8 being appointed to positions of leadership, 2 winning teaching awards, and 1 achieving both. Four participants had fewer subsequent risk management reports than prior to referral for remediation. One individual resigned but is in practice in new settings.
Discussion
While medical schools and teaching hospitals report using simulation for the remediation of professionalism, further description of how it was used is not available.2 To our knowledge, this is the first description of a personalized remediation program with encouraging long-term outcomes.4,5
The remediation methodology, grounded in expertise theory,6 represents a unique approach to provide remedial training for those who struggle with professionalism. Prior studies on the remediation of unprofessional behavior have focused on describing remediation methods without individual outcomes,7,8 or as 1 area of deficiency embedded in a larger remediation program.9–11
This study has several limitations. The intervention occurred at 1 institution with special resources, including a remediation team and a well-developed simulation center with highly skilled standardized patients, which may not be feasible for all programs. Although we reached saturation with the interviews, only 38% of the total participants and 79% of their supervisors were interviewed. It is possible that those with more positive results volunteered to participate. The study was conducted 2 to 4 years after remediation, and behaviors may have regressed as participants continue in their careers.
Our next steps include reproducing this program at other institutions, reassessing participants' status in 7 to 10 years, and seeking less resource-intensive methods to achieve similar results.
Conclusion
A simulation-based personalized remediation program for unprofessional behavior, which is supportive of faculty and residents practicing positive behaviors with guided feedback, appears to result in long-term positive behavior change in participants.
Supplementary Material
References
- 1.Papadakis MA, Paauw DS, Hafferty FW, et al. Perspective: the education community must develop best practices informed by evidence-based research to remediate lapses of professionalism. Acad Med. 2012;87(12):1694–1698. doi: 10.1097/ACM.0b013e318271bc0b. [DOI] [PubMed] [Google Scholar]
- 2.Passiment M, Sacks H, Huang G. Medical simulation in medical education: results of an AAMC survey. September 2011. https://www.aamc.org/download/259760/data/medicalsimulationinmedicaleducationanaamcsurvey.pdf. Accessed October 11, 2018.
- 3.Broadfoot K, Guerrasio J, Aagaard E. Beyond procedures and checklists: using simulation to remediate communication and professionalism skill challenges. SGIM Forum. 2015;38(9):1–2. [Google Scholar]
- 4.Ericsson KA. Acquisition and maintenance of medical expertise: a perspective from the performance approach with deliberate practice. Acad Med. 2015;90(11):1471–1486. doi: 10.1097/ACM.0000000000000939. [DOI] [PubMed] [Google Scholar]
- 5.Eppich WJ, Hunt EA, Duval-Arnould JM, et al. Structuring feedback and debriefing to achieve mastery learning goals. Acad Med. 2015;90(11):1501–1508. doi: 10.1097/ACM.0000000000000934. [DOI] [PubMed] [Google Scholar]
- 6.Ericsson KA, Smith J. Toward a General Theory of Expertise: Prospects and Limits. Cambridge, MA: Cambridge University Press;; 1991. [Google Scholar]
- 7.Regan L, Hexom B, Nazario S, et al. Remediation methods for milestones related to interpersonal and communication skills and professionalism. J Grad Med Educ. 2016;8(1):18–23. doi: 10.4300/JGME-D-15-00060.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ziring D, Danoff D, Grosseman S, et al. How do medical schools identify and remediate professionalism lapses in medical students? A study of US and Canadian medical schools. Acad Med. 2015;90(7):913–920. doi: 10.1097/ACM.0000000000000737. [DOI] [PubMed] [Google Scholar]
- 9.Warbuton KM, Goren E, Dine J. Comprehensive assessment of struggling learners referred to a graduate medical education remediation program. J Grad Med Educ. 2017;9(6):763–767. doi: 10.4300/JGME-D-17-00175.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guerrasio J, Garrity MJ, Aagaard EM. Learner deficits and academic outcomes of medical students, residents, fellows and physicians referred to a remediation program, 2006–2012. Acad Med. 2014;89(2)):352–358. doi: 10.1097/ACM.0000000000000122. [DOI] [PubMed] [Google Scholar]
- 11.Zbieranowski I, Takahashi SG, Verma S, et al. Remediation of residents in difficulty: a retrospective 10-year review of the experience of a postgraduate board of examiners. Acad Med. 2013;88(1):111–116. doi: 10.1097/ACM.0b013e3182764cb6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.