ABSTRACT
Background
Collaboration between graduate medical education (GME) and health systems is essential for the success of patient safety initiatives. One example is the development of an incentive program aligning trainee performance with health system quality and safety priorities.
Objective
We aimed to improve trainee safety event reporting and engagement in patient safety through a GME incentive program.
Methods
The incentive program was implemented to provide financial incentives to drive behavior and engage residents and fellows in safety efforts. Safety event reporting was measured beginning in the 2014–2015 academic year. A training module was introduced and the system reporting link was added to the institution's Resident Management System homepage. The number of reports by trainees was tracked over time, with a target of 2 reports per trainee per year.
Results
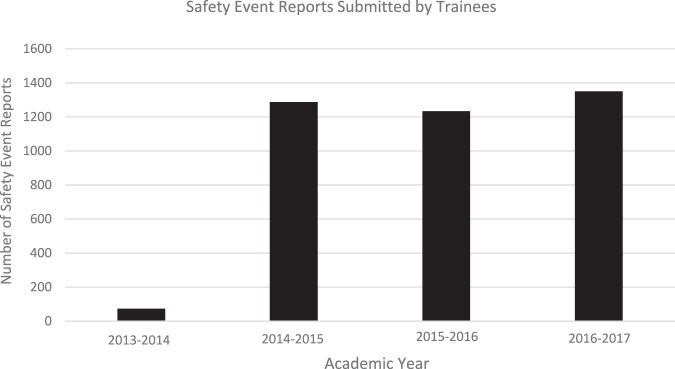
Baseline data for the year prior to implementation of the incentive program showed less than 0.5% (74 of 16 498) of safety reports were submitted by trainees, in contrast with 1288 reports (7% of institutional reports) by trainees in 2014–2015 (P < .0001). A total of 516 trainees (57%), from 37 programs, received payment for the metric, based on a predefined program target of a mean of 2 reports per trainee. In 2015–2016 and 2016–2017 the submission rate was sustained, with 1234 and 1350 reports submitted by trainees, respectively.
Conclusions
An incentive program as part of a larger effort to address safety events is feasible and resulted in increased reporting by trainees.
What was known and gap
Institutions are interested in increasing the reporting of safety events, yet there is little data on the effectiveness of different approaches.
What is new
An institutional graduate medical education (GME) incentive program significantly increased the number of patient safety events reported by trainees.
Limitations
Single institution study limits generalizability; the multifaceted intervention makes it difficult to isolate the effect of the incentives.
Bottom line
A GME incentive program is feasible and resulted in increased reporting by trainees.
Introduction
Patient safety and quality of care are crucial elements of health care and graduate medical education (GME).1–3 The Accreditation Council for Graduate Medical Education (ACGME) has established safety and health care quality as focus areas through the Clinical Learning Environment Review (CLER), with safety event reporting constituting an important priority.2 Given that physicians historically underreport events, this area represents a substantial opportunity for interventions to increase reporting, which could contribute to enhanced understanding of failures in care delivery.4–7
One example of a collaborative approach to enhance engagement in quality improvement is a financial incentive program.8–11 Several examples of financial incentive programs have been described in the literature, and findings suggest that these approaches can change health care provider behaviors, yet the impact of such programs on GME trainees has not been extensively assessed.7,11,12 To our knowledge, there has only been 1 study of the impact of a financial incentive (in the form of a retirement benefit) on event reporting by trainees.12
Beginning in academic year 2014–2015, safety event reporting was added as a metric in our institutional GME incentive program. The incentive program had been established to improve care for patients, while providing trainees experience with a model in which their professional decisions had personal financial implications. The objective of this initiative was to enhance safety event reporting and improve patient safety.
Methods
Duke University Hospital is a 957-bed tertiary academic medical center with more than 150 GME programs and approximately 1000 trainees.
Beginning in academic year 2014–2015, and continuing for 2016–2017, safety event reporting was selected as 1 of 4 measures for the GME incentive program, which provides a bonus of $200 per metric to trainees based on achievement of predefined targets. For event reporting, a target of 2 reports per trainee per academic year was established, and this metric was paid to trainees based on the training program's overall performance. Each resident or fellow was eligible to receive payment if his or her program cumulatively achieved an average of 2 reports per trainee over the course of the academic year. This program was funded by the sponsoring institution, with a total potential cost of $197,000 per year if all programs achieved the reporting threshold.
In July 2014, an educational module was implemented to introduce a new online safety event reporting system. The module included content on the importance of safety event reporting and instructions for using the new system. The module has been required for all new trainees joining our institution since that time. In addition, a link for the reporting site was added to our institutional Resident Management System homepage. Trainee reports were tracked over time by the hospital's patient safety office. Reports were aggregated to the program level, and the number of safety events submitted from each program was provided as a scorecard to trainees on a monthly basis via e-mail. The GME Patient Safety and Quality Council, which consists of trainees and faculty advisors from all clinical departments, shared the data with program leadership. All safety event reports were individually reviewed by leaders in the patient safety office, with the support of relevant GME leaders. Issues identified were forwarded to the relevant clinical service unit, institutional, program, and department leaders for appropriate follow-up.
This project was deemed exempt by the Duke Institutional Review Board as education-based research.
Chi-square analysis was used for statistical comparison of the annual number of reports.
Results
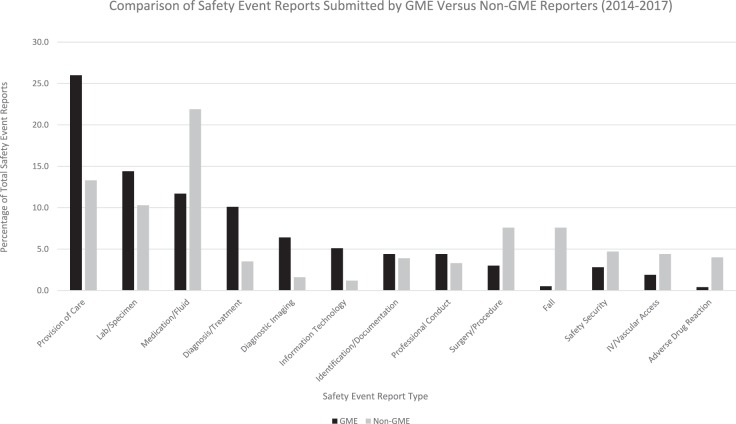
All 988 residents and fellows completed the online module in 2014–2015. Baseline data demonstrated that in the year prior to implementation of the new reporting system, educational module, and incentive program, only 74 of 16 498 safety event reports (less than 0.5%) were submitted by trainees. This rate represented a mean of approximately 6 reports per month submitted by residents and fellows. In 2014–2015, 1288 reports were submitted by trainees, representing 7% of total institutional safety event reports and more than 100 reports per month (P < .0001; Figure 1), and 451 (46%) individual trainees completed at least 1 report. Thirty-seven (31%) GME programs met the metric of a mean of 2 reports per trainee for their program over the course of the academic year, and 516 (57%) individual residents and fellows in these programs received the $200 bonus. In 2015–2016 and 2016–2017, numbers of submissions were sustained with 1234 (7% of total institutional reports, mean of 1.2 reports per trainee) and 1350 (8% total institutional reports, mean of 1.3 reports per trainee) reports from trainees, respectively (Figure 1). The content of these reports helped to identify opportunities to address safety problems, and improve systems and processes across a range of categories (Figure 2), a number of which have led to broader initiatives to improve patient safety and quality.
Figure 1.
Resident and Fellow Safety Event Reports
Figure 2.
Comparison of Safety Event Reports by Category
Discussion
We demonstrated that a GME incentive program for resident and fellow event reporting can substantially increase reporting of patient safety events, and that the increased reporting was sustained in subsequent years.
There have been other attempts to improve event reporting in trainees in a variety of ways, including educational efforts, addressing barriers to reporting, and linking reporting to retirement benefits.12–15 To our knowledge, this effort is the first to demonstrate improved and sustained GME safety event reporting through a direct financial incentive program.
As frontline clinicians, trainees have a valuable perspective on potential patient safety issues and can offer unique insight into understanding vulnerabilities in care delivery. These differences in perspective are demonstrated in their reported event types. Most GME reports were in the Provision of Care category (Figure 2). Reports in this category encompassed a range of themes, such as responses to patient condition, completion of orders, transitions of care, and protocols/care standard deviations or violations. This category of reporting differed substantially from the types of reports most commonly submitted by other members of the team in our institution. These reports highlighted a variety of unique challenges in multidisciplinary communication and system vulnerabilities, that offered opportunities for leaders to effect change in these important areas.
As part of the approach, leaders in a single GME program engaged all trainees in that program in a series of meetings to discuss patient safety and quality concerns. As a group, these trainees developed a cumulative list of safety concerns encountered as part of their clinical work that was subsequently submitted by a single trainee representative. While this example demonstrates the success of this GME incentive program, the large influx of complex reports at a single time created substantial challenges for leaders of clinical services to address in a timely way with existing resources and infrastructure.
As resources are considered, the impact of cost on the sustainability of an incentive program must be considered. Cost may be a limitation to the broader applicability, adaptability, and sustainability of an incentive program, with more detailed analysis needed to determine if the costs for such a program could be recouped through institutional and avoidance of penalties as a result of improved patient safety outcomes.
Our study has limitations. It was conducted at a single site, potentially reducing the applicability of the intervention in other settings. It also was not possible to determine the exact impact of the incentive program on GME event reporting relative to other ongoing initiatives that include the CLER program, the educational aspects of our intervention, and general institutional quality and safety initiatives. Additionally, no balancing measures were included in this project, potentially leading to decreases in other resident functions as event reporting increased. Finally, some increase in reporting may have resulted from residents “checking a box” or responding to peer pressure to submit reports, rather than increased engagement in institutional safety culture. These areas present opportunities for future investigation.
An important next step is to develop mechanisms to integrate trainee analysis of reports into existing institutional infrastructure, as an increase in safety event reporting by itself will not achieve the desired impact on patient safety unless reporting is paired with robust feedback and demonstrable changes in practice. In addition, the longer-term impact of this program on faculty reporting and behavior, as residents and fellows transition to faculty members, is another key area for future study.
Conclusion
We showed that a financial incentive program can increase and sustain safety event reporting by residents and fellows, and that the types of events reported by trainees differ from those of other health professionals.
References
- 1.Bagian JP. The future of graduate medical education: a systems-based approach to ensure patient safety. Acad Med. 2015;90(9):1199–1202. doi: 10.1097/ACM.0000000000000824. [DOI] [PubMed] [Google Scholar]
- 2.Accreditation Council for Graduate Medical Education. Clinical Learning Environment Review Pathways to Excellence. 2018 http://www.acgme.org/portals/0/PDFs/CLER/CLER_Brochure.pdf Accessed October 29,
- 3.Accreditation Council for Graduate Medical Education. ACGME Common Program Requirements. 2018 http://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/CPRs_2017-07-01.pdf Accessed October 29,
- 4.Kaldjian LC, Forman-Hoffman VL, Jones EW, et al. Do faculty and resident physicians discuss their medical errors? J Med Ethics. 2008;34(10):717–722. doi: 10.1136/jme.2007.023713. [DOI] [PubMed] [Google Scholar]
- 5.Kaldjian LC, Jones EW, Wu BJ, et al. Reporting medical errors to improve patient safety: a survey of physicians in teaching hospitals. Arch Intern Med. 2008;168(1):40–46. doi: 10.1001/archinternmed.2007.12. [DOI] [PubMed] [Google Scholar]
- 6.Rowin EJ, Lucier D, Pauker SG, et al. Does error and adverse event reporting by physicians and nurses differ? Jt Comm J Qual Patient Saf. 2008;34(9):537–545. doi: 10.1016/s1553-7250(08)34068-9. [DOI] [PubMed] [Google Scholar]
- 7.Taylor JA, Brownstein D, Christakis DA, et al. Use of incident reports by physicians and nurses to document medical errors in pediatric patients. Pediatrics. 2004;114(3):729–735. doi: 10.1542/peds.2003-1124-L. [DOI] [PubMed] [Google Scholar]
- 8.Bailit MH, Burns ME, Dyer MB. Implementing value-based physician compensation: advice from early adopters. Healthc Financ Manage. 2015;69(7):40–47. [PubMed] [Google Scholar]
- 9.Flodgren G, Eccles MP, Shepperd S, et al. An overview of reviews evaluating the effectiveness of financial incentives in changing healthcare professional behaviours and patient outcomes. Cochrane Database Syst Rev. 2011. 7:CD009255. [DOI] [PMC free article] [PubMed]
- 10.Scott A, Sivey P, Ait Ouakrim D, et al. The effect of financial incentives on the quality of health care provided by primary care physicians. Cochrane Database Syst Rev. 2011. 9:CD008451. [DOI] [PubMed]
- 11.Vidyarthi AR, Green AL, Rosenbluth G, et al. Engaging residents and fellows to improve institution-wide quality: the first six years of a novel financial incentive program. Acad Med. 2014;89(3):460–468. doi: 10.1097/ACM.0000000000000159. [DOI] [PubMed] [Google Scholar]
- 12.Scott DR, Weimer M, English C, et al. A novel approach to increase residents' involvement in reporting adverse events. Acad Med. 2011;86(6):742–746. doi: 10.1097/ACM.0b013e318217e12a. [DOI] [PubMed] [Google Scholar]
- 13.Macht R, Balen A, McAneny D, et al. A multifacted intervention to increase surgery resident engagement in reporting adverse events. J Surg Educ. 2015;72(6):e117–e122. doi: 10.1016/j.jsurg.2015.06.022. [DOI] [PubMed] [Google Scholar]
- 14.Tevis SE, Schmocker RK, Wetterneck TB. Adverse event reporting: harnessing residents to improve patient safety. J Patient Saf. 2017 Oct 13; doi: 10.1097/PTS.0000000000000333. [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 15.Stewart DA, Junn J, Adams MA, et al. House staff participation in patient safety reporting: identification of predominant barriers and implementation of a pilot program. South Med J. 2016;109(7):395–400. doi: 10.14423/SMJ.0000000000000486. [DOI] [PubMed] [Google Scholar]