ABSTRACT
Background: Older individuals are at high risk for morbidity and mortality due to influenza, and the most effective way to prevent influenza is yearly vaccination. In China, the influenza vaccine is not covered by the national Expanded Program on Immunization, and more evidence is needed about influenza vaccine usage among older individuals.
Objective: To determine the influenza vaccination coverage and its influencing factors, and understand barriers to older adults receiving influenza vaccinations in Shanghai, China.
Methods: A cross-sectional survey was conducted with residents aged 60 and older. Vaccination status in the 2016–17 influenza season and reasons for or against vaccination were surveyed. The vaccination coverage rates were adjusted by gender, age and community distribution, and potential factors influencing vaccination uptake were determined by bivariate logistic regression.
Results: In total, 253 of the 4417 respondents received an influenza vaccine during the 2016–17 season, yielding an adjusted coverage rate of 5.2% (95% CI, 4.5-5.8). The frequency of receiving the vaccine was higher for older individuals living with family/friends than that for those living alone (p < 0.05), and lower among individuals with chronic respiratory diseases (p < 0.05). Among unvaccinated respondents, lack of influenza vaccine awareness was the most common reason for being unvaccinated (48.3%, 2012/4164).
Conclusion: Influenza vaccination coverage is extremely low among older people in Shanghai, and lack of awareness of the influenza vaccine might be a potential barrier to vaccination. Our study highlights the need for an appropriate influenza vaccination strategy and program targeting the older population.
KEYWORDS: coverage, influenza, older people, vaccination
Introduction
Influenza is a common infectious disease caused by the influenza virus. Although influenza can seriously affect all populations, approximately 90% of influenza-associated deaths occur in people aged 65 years and older.1
Many studies have demonstrated that influenza-related hospitalizations and deaths in this population group can be significantly reduced by influenza vaccination. The Chinese Centers for Disease Control and Prevention (China CDC) has recommended that individuals aged 60 years and above be treated as a priority group for seasonal influenza vaccination,2 which is consistent with the position paper by the World Health Organization (WHO)3 and the US Centers for Disease Control and Prevention (CDC).4
The influenza vaccine is not currently included in the national Expanded Program on Immunization (EPI) in China. The coverage rate and influencing factors of the influenza vaccine among Chinese older adults have not been well explored or discussed. Since 2007, the governments of some cities such as Beijing,5 Karamay,6 and Xinxiang7 have published policies providing free influenza vaccinations to local elderly people. In addition, some areas of Guizhou and Zhejiang Province have implemented subsidy policies such as including the influenza vaccine in medical insurance for target groups.8-9 In recent years, a few studies have been conducted to understand the current influenza vaccination coverage rate (VCR) among older individuals, as well as to consider efficient policies to increase it.10-12
Shanghai is a major city in eastern China and is one of the most developed cities worldwide. Over the past decade, the proportion of older adults in Shanghai has rapidly increased. At the end of 2016, the proportion of the Shanghai population aged ≥60 years was 31.6% (4.58 million people), and the life expectancy of the city residents was 83.2 years. These findings highlight the need for health-related strategies to cope with an aging society.13According to our previous study, influenza virus is the dominant pathogen among older people with acute respiratory infections in Shanghai.14
This study aimed to assess the influenza VCR among older people in Shanghai during the 2016–17 influenza season and determine the reasons for vaccination or non-vaccination. The findings of this study are intended to provide scientific evidence for the implementation of appropriate strategies and programs targeting older people in Shanghai, and other developed areas with the potential condition for considering a subsidy policy for influenza vaccination.
Results
Subject characteristics
A total of 10579 older adults were invited to participate in our survey, and 4794 of them agreed to be interviewed and successfully finished the questionnaire, yielding a response rate of 45.3% (4794/10579). Because our study focused on influenza vaccination, 377 participants whose vaccination status during the 2016–17 influenza season was classified as “unknown” were excluded from the analysis (Figure 1).
Figure 1.

Completion of Enrollment survey questions among 4417 older adults recruited in Shanghai, China, 2017.
The ages of the respondents ranged from 60.0 to 105.0 years, with a median age of 71.7[interquartile range (IQR): 66.2–79.8] years, and women accounted for 53.4% of the respondents. The majority of the respondents (82.8%) had less than a high school-level education. More than one-third (39.5%) of the participants self-assessed their health status as very healthy/healthy, whereas 20.8%, 20.2% and 7.9% of the individuals suffered from cardiovascular disease, diabetes and chronic respiratory disease, respectively.
The demographic characteristics of the respondents are presented in Table 1.
Table 1.
General characteristics of the study participants.
| Age group (years) |
||||
|---|---|---|---|---|
| Overall | 60–69 | 70-79 | ≥80 | |
| Demographic characteristics | N = 4417, n(%) | 1852(41.9) | 1490(33.7) | 1075(24.3) |
| Gender | ||||
| Male | 2058(46.6) | 835(45.1) | 717(48.1) | 506(47.1) |
| Female | 2359(53.4) | 1017(54.9) | 773(51.9) | 569(52.9) |
| Age, median (IQR, years) | 71.7 (66.2–79.8) | 65.3 (62.6–67.7) | 74.1 (71.8–76.9) | 83.8 (81.8–86.4) |
| Living status | ||||
| Live alone | 463(10.5) | 75(4.1) | 162(10.9) | 226(21.0) |
| Live with family or friends | 3954(89.5) | 1777(96.0) | 1328(89.1) | 849(79.0) |
| Education attainment | ||||
| Primary school | 2209(50.0) | 673(36.3) | 745(50.0) | 791(73.6) |
| Secondary school2 | 1450(32.8) | 816(44.1) | 449(30.1) | 185(17.2) |
| High school | 543(12.3) | 271(14.6) | 202(13.6) | 70(6.5) |
| Bachelor's degree or above | 215(4.9) | 92(5.0) | 94(6.3) | 29 (2.7) |
| Self-evaluation of health situation | ||||
| Very healthy | 149(3.4) | 90(4.9) | 37(2.5) | 22(2.1) |
| Healthy | 1594(36.1) | 803(43.4) | 497(33.4) | 294(27.4) |
| Normal | 2242(50.8) | 849(45.8) | 785(52.7) | 608(56.6) |
| Unhealthy | 432(9.8) | 110(5.9) | 171(11.5) | 151(14.1) |
| Monthly household income, (Chinese yuan) | ||||
| <2000 | 696(20.3) | 202(10.9) | 238(16.0) | 256(23.8) |
| 2000-4999 | 1557(45.4) | 682(36.8) | 555(37.3) | 320(29.8) |
| 5000-7999 | 801(23.3) | 364(19.7) | 264(17.7) | 173(16.1) |
| ≥8000 | 378(11.0) | 201(10.9) | 106(7.1) | 71(6.6) |
| Unknown | 985(22.3) | 403(21.8) | 327(22.0) | 255(23.7) |
| Specific underlying diseases | ||||
| Chronic respiratory diseases | 377 (7.9) | 113 (6.2) | 124 (7.4) | 140 (10.8) |
| Diabetes | 969 (20.2) | 312 (17.1) | 370 (22.2) | 287 (22.1) |
| Cardiovascular disease | 995 (20.8) | 225 (12.3) | 371 (22.2) | 399 (30.7) |
IQR: interquartile range.
In China, secondary school education refers to the three-year period between primary school and high school. The ages of secondary school students are approximately 12 to 15 years old.
1 US dollar≈6.43 Chinese yuan.
Influenza vaccination coverage rates and their influencing factors
A total of 253 respondents received an influenza vaccination during the 2016–17 season. The raw and adjusted VCRs were 5.7% [95% confidence interval (CI): 5.1–6.5)] and 5.2% (95% CI: 4.5-5.8), respectively (Table 2). There was no statistically significant difference in the adjusted VCR among men(5.0%) and women(5.3%). Among the three age groups, the highest and lowest vaccination rates were obtained among the respondents older than 80 years (5.8%, 95% CI: 4.3–7.2) and those aged 70–79 years (4.2%, 95% CI: 3.1-5.2), respectively. There were no significant differences in the VCR among older individuals with diabetes (6.2%, 95%CI:4.5–8.1) and among those with cardiovascular disease (4.6%, 95%CI:3.2–6.2). However, none of the above results showed significant differences. The VCR among those respondents suffering from chronic respiratory disease (3.0%, 95% CI: 1.3-4.9) was significantly lower (p ) than the others. The VCR was also significantly lower among older people living alone (2.4%, 95%CI:1.5–5.3) than those living with family or friends (5.3%, 95%CI:4.6–6.1,p = 0.02).
Table 2.
Coverage rates of seasonal influenza vaccination among older people in Pudong New Area, Shanghai, in the 2016–17 influenza season (n = 4417).
| Characteristics | No. of Vaccinated Individuals | Raw VCR(95% CI) | Adjusted VCR(95% CI) | OR(95%CI) | p |
|---|---|---|---|---|---|
| Total | 253 | 5.7(5.1-6.5) | 5.2(4.5-5.8) | ||
| Gender | |||||
| Male | 113 | 5.5(4.6-6.6) | 5.0(4.1-6.0) | ref | |
| Female | 140 | 5.9(5.0-7.0) | 5.3(4.3-6.2) | 1.2(0.8-1.6) | 0.41 |
| Age group (years) | |||||
| 60-69 | 114 | 6.2(5.1-7.4) | 5.6(4.5-6.7) | 0.9(0.6-1.4) | 0.76 |
| 70-79 | 71 | 4.8(3.7-6.0) | 4.2(3.1-5.2) | 0.8(0.5-1.2) | 0.25 |
| ≥80 | 68 | 6.3(5.0-8.0) | 5.8(4.3-7.2) | ref | |
| Education attainment | |||||
| Primary school | 119 | 5.4(4.5-6.4) | 4.4(3.5-5.3) | ref | |
| Secondary school | 96 | 6.6(5.4-8.0) | 6.4(5.0-7.7) | 1.5(1.0 -2.1) | 0.06 |
| High school | 31 | 5.7(3.9-8.0) | 5.2(3.3-7.1) | 1.0(0.6-1.8) | 0.91 |
| Bachelor's degree or above | 7 | 3.3(1.3-6.6) | 3.6(1.0-6.2) | 0.5(0.1-1.6) | 0.22 |
| Self-evaluation of health situation | |||||
| Very healthy | 6 | 4.0(1.5-8.6) | 3.9(0.4-7.5) | Ref | |
| Healthy | 91 | 5.7(4.6-7.0) | 4.9(3.8-6.0) | 1.5(0.4-5.2) | 0.51 |
| Normal | 131 | 5.8(4.9-6.9) | 5.5(4.5-6.5) | 1.6(0.5-5.4) | 0.48 |
| Unhealthy | 25 | 5.8(3.8-8.4) | 5.1(2.9-7.3) | 2.1(0.6-7.8) | 0.26 |
| Living status | |||||
| Live alone | 18 | 3.9(2.3-6.1) | 2.4(1.5-5.3) | Ref | |
| Live with family | 235 | 5.9(5.2-6.7) | 5.3(4.6-6.1) | 2.7(1.9-3.2) | 0.04 |
| Monthly household income, (Chinese yuan) | |||||
| <2000 | 39 | 5.6(4.0-7.6) | 4.8(3.1-6.6) | 1.2(0.7-2.4) | 0.51 |
| 2000-4999 | 83 | 5.3(4.3-6.6) | 4.9(3.8-6.1) | 1.1(0.6-1.9) | 0.78 |
| 5000-7999 | 49 | 6.1(4.6-8.0) | 5.5(3.9-7.1) | 1.2(0.7-2.1) | 0.59 |
| ≥8000 | 19 | 5.0(3.1-7.7) | 4.5(2.4-6.5) | Ref | |
| Underlying chronic diseases | |||||
| Chronic respiratory diseases | 14 | 4.0(2.1-6.1) | 3.0(1.3-4.9) | 1.1(0.7-1.8) | 0.67 |
| Diabetes | 59 | 6.6(5.1-8.3) | 6.2(4.5-8.1) | 0.5(0.3-1.1) | 0.08 |
| Cardiovascular disease | 46 | 5.1(3.8-6.7) | 4.6(3.2-6.2) | 0.9(0.5-1.4) | 0.55 |
In China, secondary school education refers to the three-year period between primary school and high school. The ages of secondary school students are approximately 12 to 15 years old.
US dollar≈6.43 Chinese yuan.
Respondents whose monthly household income was unknown were not included in this analysis.
Similar results were found in the logistic regression model (Table 2). Among all the potential influencing factors, living with family/friends was the only factor that was significantly associated with an increased likelihood of receiving the influenza vaccine compared with older people living alone, with an odds ratio (OR) of 2.7 (95% CI: 1.9–3.2, p = 0.04).
Reasons for receiving or not receiving the influenza vaccine
Among the 253 respondents who received an influenza vaccination during the 2016–17 influenza season, 73.1% made this decision based on their belief that the influenza vaccine was effective, 36.4% believed that the vaccination could reduce complications due to influenza, and 32.8% of the vaccinated respondents received the vaccine based on a recommendation from their family. A total of 7.9% of the participants stated that the reason for receiving the vaccination was that it was recommended by their doctor (Figure 2A).
Figure 2.
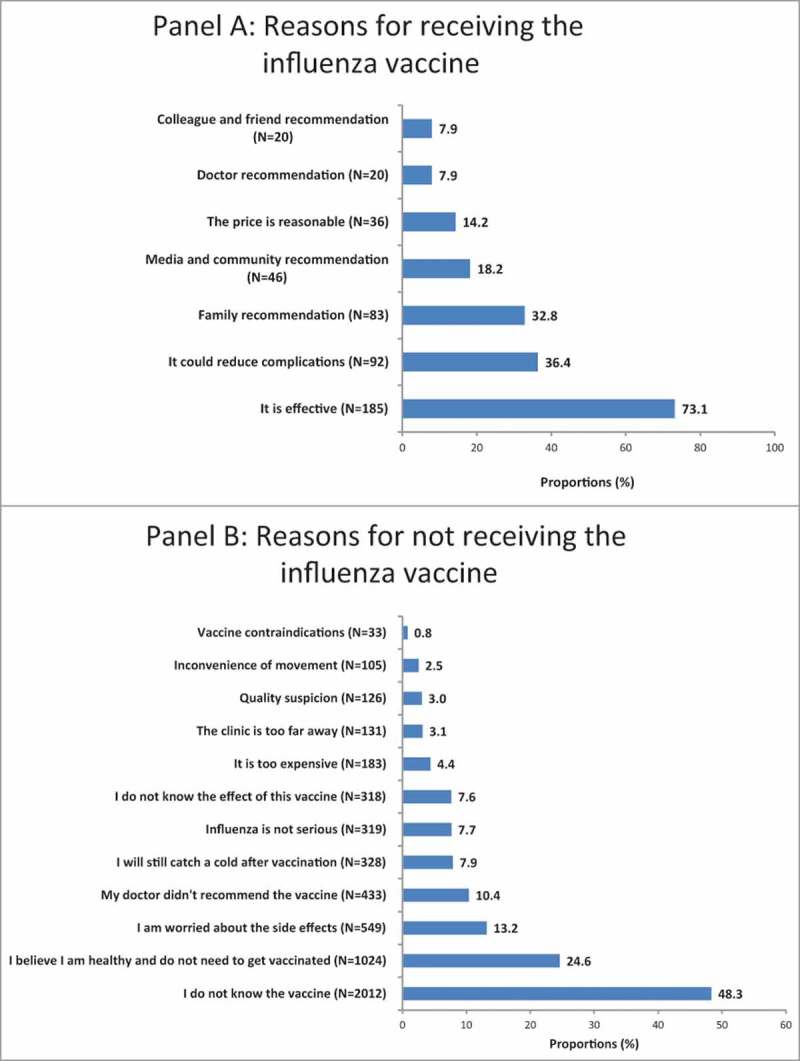
Reasons for receiving or not receiving the influenza vaccine among older people in Pudong during the 2016–17 influenza season.
The main explanations for not being vaccinated were lack of awareness of the influenza vaccine (48.3%, n = 2012), followed by the belief of being healthy enough and not needing to be vaccinated (24.6%, n = 1024), worry regarding the side effects (13.2%, n = 549), lack of a doctor recommendation (10.4%, n = 433), and believing that it was still possible to catch a cold after vaccination (7.9%, n = 328). A total of 0.8% (n = 33) of the unvaccinated respondents claimed that they had contraindications for vaccinations, among whom 87.9% (n = 29) and 12.1% (n = 4) considered COPD or diabetes to be contraindications, respectively (Figure 2B).
We also compared the reasons for not receiving the vaccine in different subgroups. The proportion of respondents who were worried about the quality of the vaccine was significantly higher among women (3.7%; n = 83) than among men (2.2%, n = 43, p = 0.005).. Similarly, that proportions were significantly higher among those older than 80 years of age (4.3%, n = 43) than the other two younger age groups (p = 0.013). The proportion of respondents who reported having a vaccine contraindication was much higher in the group with at least a bachelor's degree (the highest educational level in this survey) than that in the other education subgroups (2.9% vs 0.7%, p = 0.006).
Awareness of the influenza vaccine differed significantly by income level (p = 0.043). The proportion of respondents who answered “I did not know about the influenza vaccine” was highest (51.1%, n = 335) in the subgroup with a monthly household income below 2000 RMB and lowest in the population with the highest income (8000 RMB) (44.0%, n = 158). Among the 445 unvaccinated respondents who lived alone, 283 (63.1%) claimed that they didn't know about influenza vaccine. Meanwhile for the 3719 unvaccinated respondents who lived with their family or friends, only 1729 (46.5%) did not know about this vaccine. This proportion was significantly lower (p < 0.001) than that for the unvaccinated respondents who lived alone.
In contrast, the proportion of respondents who refused vaccination due to a belief that it was unnecessary was highest in the groups with a monthly household income of 5000–7999 RMB (28.2%), followed by the group with the highest household income (8000 RMB, 27.3%). These proportions were 23.0% and 24.1% in the two groups with lower incomes, respectively. This difference was also significant (p = 0.034).
Discussion
The adjusted influenza VCR was approximately 5.2% among older people during the 2016–17 influenza season in Pudong, Shanghai. This rate was not only markedly lower than the rates reported in European countries,15-18 the United States,19-20 Japan,21 Jordan,22 and Korea23 but also lower than the rate reported in Beijing,24 which is a similarly sized domestic city with an influenza vaccination subsidy policy for high risk groups (school-aged children and older adults aged 60 years.5 However, a previous study reported that the mean influenza VCR of urban older people in four selected provinces without a vaccination subsidy policy was 4.1%,25 which was similar to our finding.
The influenza VCRs among the different subgroups were similar, with the exception of the rates among older people living alone and the rates among individuals suffering from chronic respiratory diseases, which were significantly lower than the VCRs obtained for the other groups. A previous study indicated that older people living alone in mainland China rated social relationships and financial circumstances as sources of low satisfaction within their quality of life.26 As suggested by our survey, the proportion of respondents not aware of the influenza vaccine was significantly higher among older adults who lived alone than those who lived with others. Living alone might lead to a narrower range of social contacts, making these individuals less likely to receive vaccine-related information from family or friends. The China CDC has recommended that individuals with chronic underlying conditions, such as chronic respiratory diseases, cardiovascular disease or diabetes, be treated as priority groups for seasonal influenza vaccination2; however, the results from our study revealed a significant gap between reality and this target.
In our study, 48.3% of the unvaccinated respondents were unaware of the vaccine. A recent survey in Nanjing also showed that only one in five older adults was aware of the influenza virus (21%) or vaccine (20%).10 A total of 7.9% of the 253 vaccinated respondents stated that they received the vaccine due to a doctor's recommendation. According to prior studies, healthcare workers in China rarely recommend seasonal influenza vaccination to their patients, even those who are at high risk of developing severe illness from influenza infection.11 Thus, it is likely that few respondents in our study received a recommendation from a healthcare worker for vaccination. Numerous studies have indicated the critical role that healthcare workers play in promoting influenza vaccination. A previous study in Europe indicated that the strongest motivation for receiving vaccination was advice from a family doctor.27 A recent study in Ningbo showed that 78% of older adults stated that they would become vaccinated if a health care worker (HCW) recommended vaccination.11 A study in China further found that, after intervention by educating HCWs, the VCR of older adults increased from 0.3% to 19%.12 We also found that 24.6% of the respondents believed that vaccination was unnecessary because influenza was not a serious disease. In contrast, only 4.4% of the respondents were concerned about the vaccination fee in our study, suggesting that the cost of vaccination was not a substantial obstacle. Similar conclusions were also obtained in a previous study in Ningbo, China. Only 9% of the 150 unvaccinated older adults stated that the reasons for not getting vaccinated were not wanting to pay.12 We also found that some of the respondents considered COPD or diabetes to be a contraindication for influenza vaccine and refused to recive the vaccine based on this reason. The misunderstanding about vaccine contraindication might be an influencing factor of lower VCR among older adults with chronic respiratory diseases.
Therefore, being vaccinated might be not only influenced by local policy but also strongly affected by knowledge and attitudes toward the vaccine. Interventions should concentrate on strategies to inform older adults that vaccination is the most powerful protective measure for influenza. This information could provide a substantial benefit by increasing vaccination coverage, which would, in turn, decrease severe outcomes from influenza infection. and might reduce the likelihood of severe outcomes, such as hospitalization and death.28 Our study also demonstrated that awareness and attitudes could vary by age, gender, household income, and education level. This finding suggests that publicity strategies should be adopted according to the characteristics of the target population to achieve the best effect.
The limitations of this study are similar to those associated with retrospective survey and cross-sectional study designs, including recall bias and selection bias. Our survey was conducted among only older residents seeking medical services at Community Health Service Centers (CHSCs). Obviously, older adults who pay more attention to their health and who tend to seek primary health care services have a greater opportunity for receiving information about the influenza vaccine and being vaccinated. Such people may have been over-sampled in our study. In contrast, those who seldom or never seek health services at CHSCs might not be recruited for this survey. This selection bias might be the reason for the higher VCR from our study than those from previous studies in China.10,11,25
Conclusions
In this study, for the first time, we quantitatively revealed the influenza VCR in a large sample of older adults in Shanghai, China. Despite the highly recommended influenza vaccine uptake for this population globally, our study found that the overall influenza VCR is extremely low in Shanghai. The poor awareness of this vaccine is the leading barrier to accepting the influenza vaccine among older people; great efforts should be made to enhance the perception of influenza virus and influenza vaccine among this high risk group.
Materials and methods
Ethics statement
Ethics clearance for this research was approval by the Ethical Review Board of Pudong New Area Centers for Disease Control and Prevention (PDCDC). Informed consent was obtained from all respondents surveyed. All potentially identifying factors have been removed to prevent identification of individuals.
Study design
This study consisted of a retrospective cross-sectional survey to assess influenza vaccination coverage and its influencing factors among older people in the Pudong New Area, Shanghai and the related reasons for receiving or not receiving the influenza vaccine.
A sample size of 4561 participants was computed based on an estimated influenza vaccination coverage of 4%, an acceptance rate of 90%, an alpha risk of 5%, a study power of 80%, and a clustering effect of 2 using the following formula for estimating the minimum sample size in a cross-sectional study: N = Z2pq/d2.
In Pudong New Area, 46 CHSCs provide primary medical care services for residents living nearby, and these services include vaccinations, free physical examinations for older residents, and health information. We conducted our study in 24 randomly selected CHSCs and allocated 180–200 questionnaires to each center. Older adults seeking health services in the selected CHSCs would be eligible to participate in the study if he/she were years old or above; and had the ability to give informed consent. Each day during the survey period from September 1st to 30th, 2017; the first 10–15 eligible participants going to the CHSC would be asked if they agreed to be interviewed. The survey ended when the allocated questionnaires were completed by each CHSC.
Data collection
Face-to-face interviews were conducted at each selected CHSC by the staff who were trained by professional investigators at the PDCDC. First, the questionnaire items were explained to the respondents by the interviewers.
Each Points of Vaccination clinic (POV) in Shanghai is required to register the time and receiver's name of each shot of the vaccine into a private dataset. In our study, when a respondent claimed that he/she had received an influenza vaccine at the CHSC where this survey was conducted, the investigator would verify his/her record in this dataset. However, for those who were not sure if they had received influenza vaccine in a POV clinic other than the survey site, their vaccination status would be classified as ‘unknown’.
Multiple checks were performed before the completed questionnaires were submitted to the PDCDC.
Questionnaire
The study tool used in this study was a questionnaire adopted and modified from the US CDC cross-sectional survey (http://www.cdc.gov/flu/fluvaxview/national-flu-survey.htm).
The investigation was conducted via face to face interviews. The questionnaire included questions on socio-demographic variables, the health status, the influenza vaccination status during the latest influenza season, and the reason(s) for being or not being vaccinated. For those participants who had received the influenza vaccine, the list of reasons in our questionnaire was read by the investigator and the respondent were asked to select the important reason(s) that influenced their decision. For those who had not received the influenza vaccine, they would first be asked if they had heard about the influenza vaccine. If the answer was “no”, other reasons for not receiving the influenza vaccination were not be proposed. Otherwise, they could provide multiple reasons for not being vaccinated. For those whose vaccination status had been classified as ‘unknown’, the rest of the questionnaire would not be administered.
The questionnaire was validated in a pilot survey conducted in two communities for two months prior to the formal survey.
Statistical analysis
The VCRs were calculated according to gender, age group, education level, self-evaluation of the health situation, household income, and presence of chronic underlying conditions. We adjusted the raw VCRs according to the gender and age group distributions of the Pudong New Area population, as reported by the 2015 Census of Pudong. Pearson's chi-square test was used to compare the adjusted VCRs among the different subgroups.
Potential factors influencing vaccination uptake were determined by bivariate logistic regression, and adjusted ORs with 95% CIs were calculated to examine the associations.
The proportions of individuals who cited each reason for receiving or not receiving the influenza vaccine were calculated and compared between subgroups of different genders, age groups, education levels, and household income levels using Pearson's chi-square test.
The level of significance was set to 0.05 (two-tailed). The data were analyzed using the ‘survey’ package in R version 3.4.2 (R Core Team, R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria).
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
Funding Statement
This work was supported by the Young Medical Talent Training Program of Health System of Pudong New Area, Shanghai [grant number PWRq2017-32].
Acknowledgment
The authors would like to acknowledge the support of the twenty-four community health service centers in conducting this survey.
References
- 1.Thompson WW, Shay DK, Weintraub E, Brammer L, Cox N, Anderson LJ, Fukuda K. Mortality associated with influenza and respiratory syncytial virus in the United States. JAMA. 2003;289(2):179−86. doi: 10.1001/jama.289.2.179. [DOI] [PubMed] [Google Scholar]
- 2.Feng L, Yang P, Zhang T, Yang J, Fu C, Qin Y, Zhang Y, Ma C, Liu Z, Wang Q, et al. . Technical guidelines for the application of seasonal influenza vaccine in China (2014-2015). Hum Vaccin Immunother. 2015;11(8):2077−101. doi: 10.1080/21645515.2015.1027470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO Influenza (Seasonal) fact sheet. 2017. [accessed 12 Jan 2018] http://www.who.int/mediacentre/factsheets/fs211/en/.
- 4.Grohskopf LA, Sokolow LZ, Broder KR, Walter EB, Bresee JS, Fry AM, Jernigan DB. Prevention and control of seasonal influenza with vaccines: recommendations of the advisory committee on immunization practices-United States, 2017–18 influenza season. Am J Transplant. 2017;17(11):2970−82. doi: 10.1111/ajt.14511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lv M, Fang R, Wu J, Pang X, Deng Y, Lei T, Xie Z. The free vaccination policy of influenza in Beijing, China: the vaccine coverage and its associated factors. Vaccine. 2016;34(18):2135−40. doi: 10.1016/j.vaccine.2016.02.032. [DOI] [PubMed] [Google Scholar]
- 6.Government of Kelamayi City Free influenza vaccines for older adults and children. 2013. [accessed 28 Apr 2018] http://www.kelamayi.com.cn/news/news_local/2013-10/21/content_1108354.htm
- 7.Government of Xinxiang County Opinions about influenza vaccination. 2017. [accessed 28 Apr 2018] http://www.xinxiang.gov.cn/sitegroup/root/html/ff80808122c050240122c5d7f2a5000c/20171115163030721.html
- 8.Government of Guizhou Province Vaccines covered by medical insurance.2017. [accessed 28 Apr 2018] http://www.gzgov.gov.cn/xxgk/jdhy/rdhy/201709/t20170929_1070481.html
- 9.Government of Ningbo City Vaccines covered by medical insurance.2015. [accessed 28 Apr 2018] http://nb.people.com.cn/n/2015/0114/c200864-23554533.html
- 10.Wendlandt R, Cowling BJ, Chen Y, Havers F, Shifflet P, Song Y, Zhang R, Iuliano D, Xu C, Yu H, et al. . Knowledge, attitudes and practices related to the influenza virus and vaccine among older adults in Eastern China. Vaccine. 2018;36(19):2673–82. doi: 10.1016/j.vaccine.2018.03.052. [DOI] [PubMed] [Google Scholar]
- 11.Song Y, Zhang T, Chen L, Yi B, Hao X, Zhou S, Zhang R, Greene C. Increasing seasonal influenza vaccination among high risk groups in China: Do community healthcare workers have a role to play? Vaccine. 2017;35(33):4060–3. doi: 10.1016/j.vaccine.2017.06.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yi B, Zhou S, Song Y, Chen E, Lao X, Cai J, Greene C M, Feng L, Zheng J, Yu H, et al. . Innovations in adult influenza vaccination in China, 2014–2015: Leveraging a chronic disease management system in a community-based intervention. Hum Vaccin Immunother. 2018;14(4):947–51. doi: 10.1080/21645515.2017.1403704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shanghai Research Center on Aging Surveillance results among older population in Shanghai. 2016. [accessed 12 Jan 2018] http://www.shrca.org.cn/5779.html.
- 14.Ye C, Zhu W, Yu J, Li Z, Fu Y, Lan Y, Lai S, Wang Y, Pan L, Sun Q, et al. . Viral pathogens among elderly people with acute respiratory infections in Shanghai, China: preliminary results from a laboratory-based surveillance, 2012–2015. J Med Virol. 2017;89(10):1700−6. doi: 10.1002/jmv.24751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Loerbroks A, Stock C, Bosch JA, Litaker DG, Apfelbacher CJ. Influenza vaccination coverage among high-risk groups in 11 European countries. Eur J Public Health. 2012;22(4):562−8. doi: 10.1093/eurpub/ckr094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ganczak M, Gil K, Korzeń M, Bażydło M. Coverage and influencing determinants of influenza vaccination in elderly patients in a country with a poor vaccination implementation. Int J Environ Res Public Health. 2017;14(6):665. doi: 10.3390/ijerph14060665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Spruijt IT, de Lange MMA, Dijkstra F, Donker GA, van der Hoek W. Long-term correlation between influenza vaccination coverage and incidence of influenza-like illness in 14 European countries. PLoS One. 2016;11(9):e0163508. doi: 10.1371/journal.pone.0163508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Blank PR, Schwenkglenks M, Szucs TD. Vaccination coverage rates in eleven European countries during two consecutive influenza seasons. J Infect. 2009;58(6):446−58. doi: 10.1016/j.jinf.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 19.Chiu APY, Dushoff J, Yu D, He D. Patterns of influenza vaccination coverage in the United States from 2009 to 2015. Int J Infect Dis. 2017;65:122−7. doi: 10.1016/j.ijid.2017.10.004. [DOI] [PubMed] [Google Scholar]
- 20.Biggerstaff M, Reed C, Swerdlow DL, Gambhir M, Graitcer S, Finelli L, Borse RH, Rasmussen SA, Meltzer MI, Bridges CB. Estimating the potential effects of a vaccine program against an emerging influenza pandemic–United States. Clin Infect Dis. 2015;60(Suppl 1):S20−9. doi: 10.1093/cid/ciu1175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Saito N, Komori K, Suzuki M, Morimoto K, Kishikawa T, Yasaka T, Ariyoshi K. Negative impact of prior influenza vaccination on current influenza vaccination among people infected and not infected in prior season: a test-negative case-control study in Japan. Vaccine. 2017;35(4):687−93. doi: 10.1016/j.vaccine.2016.11.024. [DOI] [PubMed] [Google Scholar]
- 22.Assaf AM, Hammad EA, Haddadin RN. Influenza vaccination coverage rates, knowledge, attitudes, and beliefs in Jordan: a comprehensive study. Viral Immunol. 2016;29(9):516−25. doi: 10.1089/vim.2015.0135. [DOI] [PubMed] [Google Scholar]
- 23.Cha S-H, Paik J-H, Lee M-R, Yang H, Park S-G, Jeon Y-J, Yoo S. Influenza vaccination coverage rate according to the pulmonary function of Korean adults aged 40 years and over: analysis of the fifth Korean national health and nutrition examination survey. J Korean Med Sci. 2016;31(5):709−14. doi: 10.3346/jkms.2016.31.5.709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wu S, Yang P, Li H, Ma C, Zhang Y, Wang Q. Influenza vaccination coverage rates among adults before and after the 2009 influenza pandemic and the reasons for non-vaccination in Beijing, China: a cross-sectional study. BMC Public Health. 2013;13:636. doi: 10.1186/1471-2458-13-636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhou L, Su Q, Xu Z, Feng A, Jin H, Wang S, Feng Z. Seasonal influenza vaccination coverage rate of target groups in selected cities and provinces in China by season (2009/10 to 2011/12). PLoS One. 2013;8(9):e73724. doi: 10.1371/journal.pone.0073724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen Y, Hicks A, While AE. Quality of life and related factors: a questionnaire survey of older people living alone in Mainland China. Qual Life Res. 2014;23(5):1593−602. doi: 10.1007/s11136-013-0587-2. [DOI] [PubMed] [Google Scholar]
- 27.Nitsch-Osuch A, Korzeniewski K, Gyrczuk E, Zielonka T, Zycinska K, Wardyn K, Kuchar E. Stagnating low influenza vaccine coverage rates in the polish elderly population in 2008–2013. Adv Exp Med Biol. 2015;857:39−44. doi: 10.1007/5584_2015_120. [DOI] [PubMed] [Google Scholar]
- 28.Dugan VG, Blanton L, Elal AIA, Alabi N, Barnes J, Brammer L, Burns E, Cummings CN, Davis T, Flannery B, et al. . Update: influenza activity — United States, October 1–November 25, 2017. MMWR Morb Mortal Wkly Rep. 2017;66(48):1318−26. doi: 10.15585/mmwr.mm6648a2. [DOI] [PMC free article] [PubMed] [Google Scholar]


