Depression and anxiety have been considered to influence disease activity and with great interest we read the recently published report by Michelsen et al.[1] In this large prospective multicentre observational study, depression and anxiety reduced the likelihood of joint-remission based on composite scores, in RA after 3 and 6 months. Differences were predominantly caused by subjective markers of disease activity rather than by CRP or ESR. The study cannot prove causality, however their findings imply that baseline depression/anxiety can impair the fulfilment of remission criteria during follow-up, influencing important treatment decisions.
As replication is a keystone in research, we aimed to validate their findings in an independent cohort, the Leiden Early Arthritis Clinic (EAC), to assess generalizability of the results. The EAC is a population-based inception cohort of patients with newly diagnosed arthritis that started in 1993; from 2010 onwards patients completed the Short Form-36 (SF-36) at baseline.[2] We studied patients included between 2010-2014 that fulfilled the 2010-criteria for RA (n=343) and selected patients that completed the SF-36 (n=293). RA-patients were treated according to the insight of the treating rheumatologist: standard therapy regimen consists of early initiation with methotrexate, in case of failure a second synthetic DMARD was prescribed and in case of failure a biologic DMARD was allowed.[3] Outcome of joint-remission was 44-joint Disease Activity Score (DAS44≤2.4) after 1-year.[4, 5] Similar as Michelsen et al we identified depression/anxiety by the SF-36 Mental Health subscale (MH≤56) and SF-36 Mental Component Summary (MCS≤38).
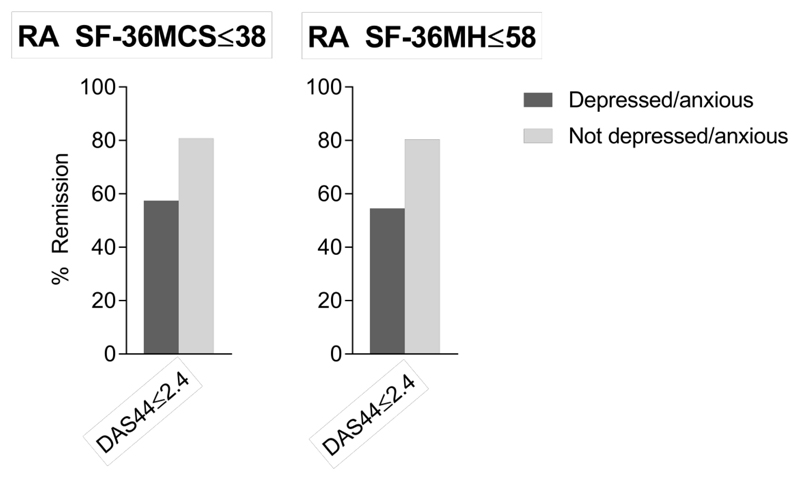
Baseline characteristics are shown in Table 1. The percentage of depressed/anxious RA-patients was 20% according to the SF-36MCS≤38, and 23% according to the SF-36MH≤56. Anxious/depressed patients were significantly younger and had a higher patient global (Table 1). Anxiety and depression was negatively associated with achieving DAS-remission after 1-year, analysed with logistic regression models corrected for age, gender and symptom duration (OR, 95%CI=0.21, 0.09-0.46 for MCS; 0.24, 0.11-0.51 for MH, p-values <0.001; Figure 1). Analyses with additional correction for baseline DAS showed similar results (MCS p<0.001; MH p=0.001). Further analyses on features of disease activity at year 1 showed that anxiety/depression was associated with more pain (β=12.1, p<0.001 for MCS; β=11.1, p=0.03 for MH) and a trend for a higher patient‘s global assessment (β=9.0, p=0.07 for MCS).
Table 1.
Baseline characteristics for Rheumatoid Arthritis patients with versus without baseline depression/anxiety according to the MCS≤38 or MH≤56
| All patients (n=293) |
Depressed/anxious (n=81) |
Not depressed/anxious (n=212) |
p Value | |
|---|---|---|---|---|
| Age, mean (SD) | 57 (15) | 54 (15) | 58 (14) | 0.02 |
| Female, n (%) | 193 (66) | 58 (72) | 135 (64) | 0.20 |
| Symptom duration in months, median (IQR) | 3 (1-8) | 3 (1-7) | 3 (1-8) | 0.72 |
| Currently smoking, n (%) | 65 (23) | 25 (33) | 40 (20) | 0.08 |
| ACPA positive, n (%) | 162 (55) | 43 (53) | 119 (56) | 0.64 |
| ESR (mm/h) median (IQR) | 28 (14-41) | 28 (14-42) | 28 (14-41) | 0.85 |
| CRP (mg/L), median (IQR) | 10 (3-22) | 7 (3-26) | 10 (3-20) | 0.76 |
| EGA, mean (SD) | 49 (20) | 49 (24) | 49 (19) | 0.44 |
| PGA, mean (SD) | 45 (27) | 54 (27) | 42 (26) | 0.001 |
| Pain, mean (SD) | 60 (25) | 63 (24) | 58 (25) | 0.92 |
| 68-TJC, median (IQR) | 10 (5-17) | 11 (6-19) | 10 (5-16) | 0.18 |
| 66-SJC, median (IQR) | 5 (2-11) | 5 (2-10) | 6 (2-11) | 0.14 |
| DAS44, mean (SD) | 2.9 (0.8) | 3.0 (0.8) | 2.9 (0.8) | 0.45 |
Pain measured by a 0-100 Visual Analogue Scale (VAS); ACPA, anti-citrullinated peptide antibody; 68-TJC, 68 tender joint counts; 66-SJC, 66 swollen joint counts; EGA, evaluator’s global assessment by a 0-100 VAS; PGA, patient’s global assessment by a 0-100 VAS; 44-joint Disease Activity Score; ESR, erythrocyte sedimentation rate; CRP, c-reactive protein; SD, standard deviation; IQR, Inter quartile range.
Figure 1. Percentages of rheumatoid arthritis patients in remission at 1-year (DAS44≤2.4) for RA patients that did or did not have depression/anxiety at the time of diagnosis.
DAS44, 44-joint Disease Activity Score; RA, rheumatoid arthritis; SF-36MCS, Medical Outcomes Survey Short Form-36 Mental Component Summary; SF-36MH, Medical Outcomes Survey Short Form-36 Mental Health subscale.
Thus, our study on the association of baseline anxiety and depression with remission after 1-year validated the findings from Michelsen et al. We observed higher percentages of RA-patients in DAS-remission, which could be caused by the longer duration of treatment (evaluation of remission at 1-year, instead of 3 and 6 months by Michelsen et al).
Concluding, baseline depression and anxiety are associated with a lower chance to achieve DAS-remission, which was mostly reflected by associations with subjective features of disease activity. Also our study cannot prove causality. Though the association between the mental state and DAS-components suggest that efforts to improve the psychological wellbeing early in the disease course may prevent higher DAS-scores later on. This could potentially prevent increased medical costs due to more intensified treatment strategies.
Funding
The research leading to these results has received funding from a Vidi-grant of the Netherlands Organization for Health Research and Development and from the European Research Council (ERC) under the European Union’s Horizon 2020 research and innovation programme (Starting grant, agreement No 714312).
The funding source had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Footnotes
Disclosure statement: There are no conflicts of interest.
References
- 1.Michelsen B, Kristianslund EK, Sexton J, Hammer HB, Fagerli KM, et al. Do depression and anxiety reduce the likelihood of remission in rheumatoid arthritis and psoriatic arthritis? Data from the prospective multicentre NOR-DMARD study. Ann Rheum Dis. 2017;76(11):1906–1910. doi: 10.1136/annrheumdis-2017-211284. [DOI] [PubMed] [Google Scholar]
- 2.de Rooy DP, van der Linden MP, Knevel R, Huizinga TW, van der Helm-van Mil AH. Predicting arthritis outcomes--what can be learned from the Leiden Early Arthritis Clinic? Rheumatology (Oxford) 2011;50(1):93–100. doi: 10.1093/rheumatology/keq230. [DOI] [PubMed] [Google Scholar]
- 3.Ajeganova S, van Steenbergen HW, van Nies JA, Burgers LE, Huizinga TW, et al. Disease-modifying antirheumatic drug-free sustained remission in rheumatoid arthritis: an increasingly achievable outcome with subsidence of disease symptoms. Ann Rheum Dis. 2016;75(5):867–73. doi: 10.1136/annrheumdis-2014-207080. [DOI] [PubMed] [Google Scholar]
- 4.Combe B, Landewe R, Lukas C, Bolosiu HD, Breedveld F, et al. EULAR recommendations for the management of early arthritis: report of a task force of the European Standing Committee for International Clinical Studies Including Therapeutics (ESCISIT) Ann Rheum Dis. 2007;66(1):34–45. doi: 10.1136/ard.2005.044354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goekoop-Ruiterman YP, de Vries-Bouwstra JK, Allaart CF, van Zeben D, Kerstens LJ, et al. Clinical and radiographic outcomes of four different treatment strategies in patients with early rheumatoid arthritis (the BeSt study): a randomized, controlled trial. Arthritis Rheum. 2005;52(11):3381–90. doi: 10.1002/art.21405. [DOI] [PubMed] [Google Scholar]