ABSTRACT
Introduction
This guideline was developed to present the evidence and provide clinical recommendations on prosthetic knee selection for unilateral amputation at the knee disarticulation or transfemoral level.
Methods
The guideline is based upon the best available evidence as it relates to prosthetic knee selection after unilateral knee disarticulation or transfemoral amputation. Recommendations are drawn from systematic review, meta-analysis, and additional published practice guidelines.
Results
Recommendation 1. Fluid knee benefits and indications: Knees with hydraulic or pneumatic swing resistance are indicated for active walkers, permitting increased walking comfort, speed, and symmetry.
Recommendation 2. Microprocessor knee benefits: Compared with nonmicroprocessor knees:
a) With respect to self-report indices and measures, microprocessor knees are indicated to reduce stumbles, falls, and associated frustrations as well as the cognitive demands of ambulation.
b) With respect to self-report indices and measures, microprocessor knees are indicated to increase confidence while walking, self-reported mobility, satisfaction, well-being, and quality of life.
c) With respect to physical performance indices and measures, microprocessor knees are indicated to increase self-selected walking speed, walking speed on uneven terrain, and metabolic efficiency during gait.
Recommendation 3. Microprocessor knee equivalence: Given the comparable values observed with the use of microprocessor and nonmicroprocessor knees with regard to daily step counts, temporal and spatial gait symmetry, self-reported general health, and total costs of prosthetic rehabilitation, these parameters may not be primary indications in prosthetic knee joint selection.
Recommendation 4. Microprocessor knees for limited community ambulators: Among limited community ambulators, microprocessor knees are indicated to enable increases in level ground walking speed and walking speed on uneven terrain while substantially reducing uncontrolled falls and increasing both measured and perceived balance.
Conclusions
These clinical practice guidelines summarize the available evidence related to prosthetic knee selection for individuals with unilateral knee disarticulation or transfemoral amputation. The noted clinical practice guidelines are meant to serve on as "guides." They may not apply to all patients and clinical situations.
KEY INDEXING TERMS: amputation, prosthesis, transfemoral, knee, microprocessor knee, Clinical Practice Guideline
Of the 1.6 million persons living in the United States with limb loss in 2005, approximately 600,000 (40%) had a major lower-limb amputation.1 These individuals vary tremendously with respect to their age, sex, amputation level and etiology, comorbid health conditions, physical presentation, ambulatory potential, and daily activity levels. Accordingly, a range of prosthetic components have been developed to reflect this variation, allowing for the appropriate pairing of component to end user.
Among those individuals with knee disarticulation and transfemoral amputation, the choice of prosthetic knee mechanism is of tremendous importance. Sawers and Hafner2 have cited the existence of over 220 different knee designs, all of which represent an attempt to balance the contrasting needs at the knee for situational stability and agility.
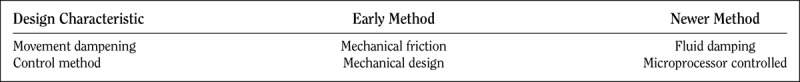
Generic classes of knee mechanisms include single axis/constant friction, stance-control, polycentric, manual locking, and fluid controlled with and without microprocessor regulation, with each of these variants associated with their basic functions, primary indications, major advantages, and chief limitations.3 However, from the standpoint of the current body of evidence, systematic review has separated these knee mechanisms according to a narrower set of design characteristics (Table 1). Specifically, the literature has drawn distinctions according to methods of dampening movement (mechanical friction vs. fluid damping) and method of control (mechanical design vs. microprocessor regulation).
Table 1.
Knee Classification Matrix, Adapted from Michaels and Stevens, 2015
Clinical Practice Guidelines (CPGs) are increasingly common in health care, with the Federal Agency for Healthcare Research and Quality (AHRQ) now housing over 1700 practice guidelines in its National Guideline Clearinghouse.4 Yet, the field of orthotics and prosthetics is underrepresented in this area, with only a single CPG listed in the AHRQ database. Encouragingly, the field has begun to develop and publish practice guidelines across a range of care episodes including the management of plagiocephaly,5 postoperative care after transtibial amputation,6 prosthetic foot selection for individuals with lower-limb amputation,7 transtibial socket design, interface and suspension,8 prescribing guidelines for microprocessor-controlled prosthetic knees in the South East England,9 and a two part, “Dutch Evidence-Based Guidelines of Amputation and Prosthetics of the Lower Extremity.”10,11
The scope and depth of CPGs are variable, with direct implications on their resultant clinical relevance and ultimate incorporation into practice. The current effort is modeled after the CPGs of the American College of Physicians,12 with necessary adaptations to accommodate the emerging evidence base of orthotic and prosthetic care. The stated goals of this approach are to “provide clinicians with clinical-based guidelines based upon the best available evidence; to make recommendations on the basis of that evidence; to inform clinicians of when there is no evidence; and finally, to help clinicians deliver the best health care possible.”12(pp 194)
Clinical utility is of paramount importance in this effort, culminating in small number of succinct, actionable evidence-based recommendations.13 Notably, within this framework, although the resultant CPGs represents a comprehensive overview of available literature, deficits in the available literature preclude CPGs within this framework from providing comprehensive clinical guidance. Thus, although CPGs can inform and supplement clinical decision making, they are not intended to direct or replace clinical judgment.
The purpose of these guidelines is to present the highest level of available evidence on prosthetic knee joint selection. In doing so, the guidelines are confined to those knee types represented in systematic review, meta-analysis, and published prescription guidelines. Specifically, this entails comparison of fluid dampening versus mechanical friction, and microprocessor-regulated knees (MPKs) versus nonmicroprocessor-regulated knees (NMPKs) or strictly mechanical knees. Of note, although historic literature has referenced the performance of “swing-only” MPKs, this technology was transitional and has largely been abandoned with the development of swing and stance MPKs. Unless specifically noted otherwise, the term MPK refers to swing and stance MPKs through the balance of this guideline.
The target audience for this guideline includes prosthetists, referring surgeons and physicians, treating physical therapists, and policy makers. The target patient population comprises those individuals with unilateral lower-limb absence, whether congenital or acquired as a result of dysvascular, traumatic, or other etiology.
METHODS
A Medline search was conducted through April 2017 to locate published secondary knowledge sources of evidence statements within the published literature. The following search terms were used: “transfemoral” AND “amputation” AND “prosth*,” AND (“knee” OR “microprocessor knee”) AND (“systematic review” OR “meta-analysis”). This search yielded 17 abstracts. Of these, six papers were identified as secondary knowledge sources (i.e., meta-analysis, systematic review, or evidence-based guidelines) that synthesized published findings of primary knowledge related to the performance characteristics of prosthetic knee types.2,8,14–17 These publications included five systematic reviews2,14–17 and a published set of prescribing guidelines.9 Three additional publications that met inclusion criteria were also identified. These included an additional systematic review,18 a set of national evidence-based guidelines,11 and a literature review that had been published but not yet indexed.19
In more recent publications, where authors provided explicit evidence statements, these were extracted for subsequent synthesis. If explicit evidence statements were not provided, well-supported narrative statements were extracted. Extracted statements are summarized in Table 2. Statements addressed the following key considerations:
Table 2.
Evidence Statements Extracted from Secondary Knowledge Sources
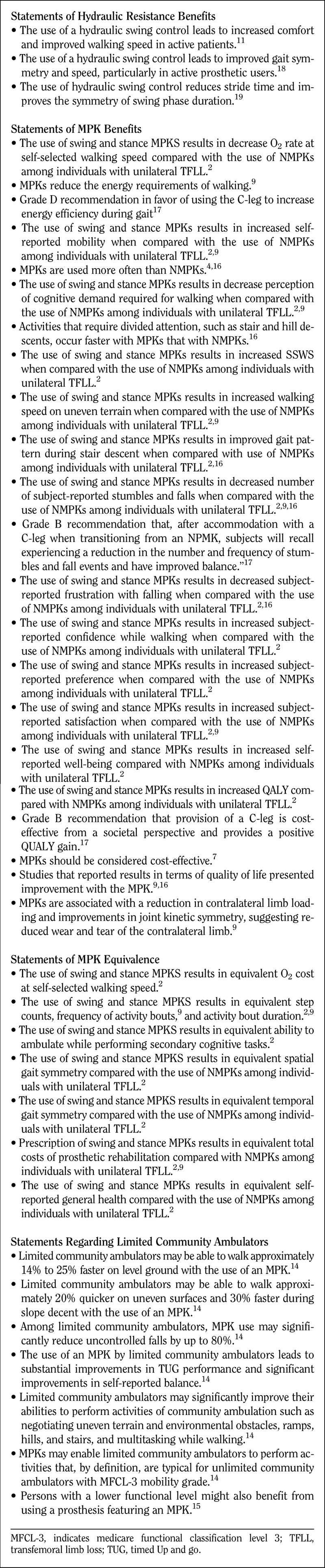
Comparative effectiveness: Where available, statements related to the comparative efficacy of various knee mechanisms were extracted from secondary knowledge sources. These statements related to fluid dampened resistance versus mechanical friction resistance mechanisms, and MPKs versus NMPKs.
Benefits of treatments: Benefits described in the evidence base included such considerations as gait speed, symmetry and comfort, decreased incidence of self-reported falls and stumbles, decreased cognitive demands associated with ambulation, increases in confidence during ambulation, self-reported mobility, satisfaction, well-being, and quality of life.
Harms of treatments: The only harms described in the evidence base included initial prosthetic procurement costs and any associated economic burden. Other potential harms might include a failure to realize the known benefits identified with a given course of treatment, such as decreases in falls and stumbles or increased in ambulatory confidence.
COMPARATIVE EFFECTIVENESS
Several evidence sources included statements related to the comparative benefits associated with fluid damping resistance mechanisms compared with mechanical friction resistance mechanisms.11,18,19 However, consistent with the relative prevalence of clinical trials on MPKs, statements comparing the relative effectiveness of MPKs relative to NMPKs were predominant.2,9,14–17
BENEFITS
With regard to resistance mechanisms, several statements confirmed improved comfort, walking speed, and symmetry with viscous damping mechanisms over friction mechanisms for active patients. With regard to MPKs, benefits can be reasonably categorized into areas of subjective decreases, subjective increases, and objectively observed improvements. Areas of beneficial subjective decreases include self-reported prevalence of stumbles and falls and associated frustrations, as well as the perceived cognitive demands of ambulation. Areas of beneficial subjective increases include self-reported confidence during ambulation, self-reported mobility, satisfaction, mobility, and quality of life. Areas of beneficial, objectively observed improvements included self-selected walking speeds, walking speeds over uneven terrain, and metabolic efficiency. Among limited community ambulators, the use of MPKs was associated with increased walking speeds, reduced falls and improved balance.
EQUIVALENCE
Several statements of equivalence between MPKs and NMPKs were identified. These were noted in daily step counts, frequency and duration of activity bouts, temporal and spatial gait symmetry, self-reported general health, and equivalent total costs of rehabilitation.
HARMS
The higher costs of initial procurement associated with MPKs is considered a potential harm or additional cost associated with this intervention. Additional harms might be seen as any failure of a patient to realize known benefits associated with a given knee mechanism.
RECOMMENDATIONS
Recommendation 1. Fluid knee benefits and indications: Knees with pneumatic or hydraulic swing resistance are indicated for active walkers, permitting increased walking comfort, speed, and symmetry.
Several reviews described the benefits observed by Boonstra et al.20 in their analysis of questionnaires completed by individuals walking with knee units with pneumatic dampening and a purely mechanical knee with mechanical friction based dampening along with those of Murray et al.21 in their analysis of individuals walking with both hydraulic swing control and constant mechanical friction knee mechanisms. These included statements of improved gait symmetry, smoothness, and speed for active walkers, largely due to a reduced prosthetic stride time.11,18,19
Recommendation 2. Microprocessor knee benefits: Compared with nonmicroprocessor knees:
Recommendation 2A: With respect to self-report indices and measures, microprocessor knees are indicated to reduce stumbles, falls, and associated frustrations as well as the cognitive demands of ambulation.
In a trial of 17 subjects transitioning from an NMPK to an MPK, Hafner and Smith22 reported a significant decrease in the number of stumbles, semicontrolled falls, and uncontrolled falls. These findings are consistent with those of Kahle et al.,23 who reported upon 19 individuals who experienced fewer stumbles and falls with an MPK compared with an NMPK. The related variable of frustration with falls has also been found to decrease with the use of an MPK.22,24 In their systematic review on the topic, Highsmith et al.17 summarized the findings of seven studies that collectively supported the grade “B” recommendation that, after accommodation from an NMPK to a C-leg, subjects will recall experiencing a reduction in the number and frequency of stumble and fall events and have improved balance.
In addition, patients have consistently reported significant reductions in their perceived cognitive burden during ambulation with an MPK.22,24,25 Furthermore, summarizing within their systematic review, Samuelsson et al.16 have observed that activities that require divided attention, such as stair and hill descents, occur more quickly with the use of an MPK compared with an NMPK, further supporting the observations from patient reports.
Recommendation 2B: With respect to self-report indices and measures, microprocessor knees are indicated to increase confidence while walking, self-reported mobility, satisfaction, well-being, and quality of life.
Berry et al.,26 reporting on a cohort of 368 MPK users who had transitioned from NMPKs, found that users had significantly higher confidence in their MPKs. This finding reinforced similar observations from earlier, smaller trials.22,24
Self-reported mobility has been reported using both the Prosthetic Evaluation Questionnaire (PEQ)22,23,27 and the physical function scale of the SF-36.28,29 Both indices have shown significant improvements with the use of an MPK. Other reviewers have summarized these collective findings simply as “increased use” with the application of an MPK.16 These observations are consistent with the findings of Kaufman et al.27 who noted an increase in energy burned over the course of an entire day with the use of an MPK despite a nonsignificant decrease in oxygen consumption rates during ambulation in this condition.
Satisfaction and preference have both been addressed in two similar clinical trials where study participants were allowed to select their intervention of choice after completion of the study, where the demonstrated preference for MPKs over NMPKs was reported at 74% to 82%.23,24 Both of these trials also reported participant responses to the question, “Over the past 4 weeks, how happy have you been with your prosthesis?” and observed significantly higher satisfaction scores with the use of an MPK.23,24
Well-being among individuals with unilateral transfemoral amputation has been reported using the well-being subscale of the PEQ. These scores have been found to increase with the transition from an MPK to an NMPK.24,27 The related construct of quality of life has been assessed as using the EuroQol Five Dimensions Questionnaire (EuroQol EQ-5D) assessing the dimensions of mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. These values have then been converted to the European construct of quality-adjusted life years (QALYs). Those studies examining this construct have found an increase in QALY values associated with the use of MPKs.28,30 Samuelsson et al.16 summarized their observations more directly in asserting that “studies that reported results in terms of QoL presented improvement with [MPKs].”
Recommendation 2C: With respect to physical performance indices and measures, microprocessor knees are indicated to increase self-selected walking speed, walking speed on uneven terrain, and metabolic efficiency during gait.
Self-selected walking speed has been found to increase with the transition from an NMPK to an MPK.23,31–33 Similarly, speed on uneven terrain has been assessed in several trials with elements including grass, rocks, sand, wood chips, cement, and carpet. These trials have also observed increased walking speeds with the use of MPKs.22–24,34 Similarly, increased speed during hill descent with an MPK has been observed.24 In addition to benefits in velocity, authors have reported improved qualities of movements for both stair descent22–24 and hill descent.22,24
Metabolic efficiency has been reported across a number of different metrics including O2 cost (oxygen consumed per distance traveled), O2 rate (oxygen consumed per time interval), physiologic cost index, and self-reported rating of perceived exertion. Two studies have reported no significant differences in O2 cost when transitioning from NMPKs to MPKs,27,32 whereas two others have observed decreased O2 costs with MPKs.34,35 By contrast, O2 rate generally decreases with the use of an MPK.31,34,36 A single study reported reduced perceived exertion with the use of an MPK.27 Evidence statements were found for O2 cost and O2 rate2 and for the more generalized constructs of reduced energy requirements and efficiency with the use of an MPK.9,17
Recommendation 3. Microprocessor knee equivalence: Given the comparable values observed with the use of microprocessor and nonmicroprocessor knees with regard to daily step counts, temporal and spatial gait symmetry, self-reported general health, and total costs of prosthetic rehabilitation, these parameters may not be primary indications in prosthetic knee joint selection.
Two studies have reported on the related variables of step count, number of activity bouts, and duration of activity bouts as observed with MPKs and NMPKs using an externally mounted StepWatch activity monitor.24,37 Both reported no significant differences in step-related activity outcomes. Of note, however, is that such activity measures are surrogate indices of the primary construct of daily energy expenditure. However, this construct was measured directly in a separate clinical trial and increased with the use of MPKs despite a nonsignificant decrease in energy costs with the use of the MPK, suggesting increased activity with the use of an MPK.27
Neither temporal nor spatial gait symmetry has been found to consistently and significantly vary with the choice of prosthetic knee mechanism.24,33,38 However, Sedki and Fisher9 summarized, “A reduction in contralateral limb loading and a significant improvement in joint kinetic symmetry suggest reduced wear and tear on the residual limb.”
General health with the use of MPKs and NMPKs has been monitored using the general health subscale of the SF-36.28,29 Both studies observed nonsignificant improvements in this index when subjects were using the MPK compared with the NMPK.
Although MPKs have higher procurement costs than NMPKs, studies that consider overall costs to society, inclusive of prosthetic acquisition costs, inpatient and outpatient care, hospital expenses, housekeeping, transportation, adaptive technology, and lost productivity have found no significant differences between MPKs and NMPKs.28,29 This was summarized in one systematic review as a grade “B” recommendation that MPK provision is cost-effective from a societal perspective.17 When viewed in isolation, the increased initial procurement costs associated with MPKs have been reported in several publications28–30 and are universally recognized.
Recommendation 4. Microprocessor knees for limited community ambulators: Among limited community ambulators, microprocessor knees are indicated to enable increases in level ground walking speed and walking speed on uneven terrain while substantially reducing uncontrolled falls and increasing both measured and perceived balance.
In their review on the effects of MPKs for limited community ambulators, Kannenberg et al.14 reported upon a number of beneficial effects. These include an increased self-selected walking velocity of 14% to 25%,23,39 a 20% increase in ambulation across uneven surfaces,22,39 and a nearly 30% increase in descending slopes and hills.22,40
In addition, Kannenberg et al.14 synthesized the observations of three studies with 27 limited community ambulators in which outcomes related to safety of prosthesis use were reported. These included reports of an 80% reduction in falls within this population with the use of an MPK23 and a significant decrease in the frequency of stumbles, uncontrolled falls, and frustration with falls in a similar population.22
Collectively, Kannenberg identified six articles reporting on the impact of MPKs on limited community ambulators that jointly suggest improved abilities to perform activities of community ambulation with an MPK, such as negotiating uneven terrain and environmental obstacles, ramps, hills, and stairs, and multitasking while walking.14 Further, MPKs may enable limited community ambulators to perform activities that by definition are typical for unlimited community ambulators.14 This premise is further supported by two articles that observed 44% to 50% of the limited community ambulators who transitioned from an NMPK to an MPK improved to unlimited community ambulation.23,24 Theeven et al.15 summarized succinctly that persons with a lower functional level might also benefit from using a prosthesis with an MPK.
AREAS OF DEVELOPING EVIDENCE
The majority of the evidence published on the clinical efficacy of MPKs reports upon early studies of the Otto Bock C-leg. The parity between the function of the early C-leg and the function that observed the current MPKs is underreported. As technological advances precipitate new approaches in MPK functionality, clinicians and manufacturers alike will need to verify the continued efficacy of these novel MPK mechanisms.
Theeven et al.15 observed that the majority of the outcome measures that have been used to study MPKs (67%) assess “body function” within the structure of the International Classification of Functioning, Disability, and Health (ICF). By contrast, only a minority of measures have assessed the constructs of “activity” and “participation.” Future studies may provide additional insight into the impact of knee choice on the individual's ability to perform activities in everyday life and his or her participation in society.
The ability of a knee mechanism to influence activity levels is still unclear. Two studies have reported equivalent step counts, activity bouts, and activity bout durations between MPK and NMPK conditions,24,37 both using an externally mounted activity monitor (StepWatch). However, a separate clinical trial evaluated a more direct measure of activity in the form of doubly labeled water samples that indicated increased physical activity-related energy expenditure with the use of MPKs despite a nonsignificant decrease in O2 cost with the use of an MPK.27 These findings are more consistent with self-reported increases in physical activity with the use of an MPK using measures such as the physical function subscale of the SF-36.28,29
To the extent that the effect of knee mechanisms on objective measures of the cognitive demands of ambulation have been studied, no clear benefits have been observed.22,24,25 These have included measures of head sway and accuracy of cognitive responses during secondary task completion while walking with different knee mechanisms. However, patients have consistently reported significant reductions in their perceived cognitive burden during ambulation with an MPK.22,24,25 The inability of empirical efforts to date to fully substantiate patient-reported benefits within this construct is an area that requires further research and understanding. It may be that the artificial cognitive loads applied in a clinical trial fail to represent the intensity and importance of the cognitive loads patients experience in daily life, or conversely the motor task is too simple or temporally confined. Ultimately, this remains an area where further research and understanding appear needed.
Note: Clinical practice guidelines are “guides” only and may not apply to all patients and all clinical situations. Thus, they are not intended to replace clinical judgment.
Footnotes
Disclosure: The authors are current employees of Hanger Clinic and received no external funding for the purposes of this work.
REFERENCES
- 1.Ziegler-Graham K, MacKenzie EJ, Ephraim PL, et al. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Arch Phys Med Rehabil 2008;89(3):422–429. [DOI] [PubMed] [Google Scholar]
- 2.Sawers AB, Hafner BJ. Outcomes associated with the use of microprocessor-controlled prosthetic knees among individuals with unilateral transfemoral limb loss: a systematic review. J Rehabil Res Dev 2013;50(3):272–314. [DOI] [PubMed] [Google Scholar]
- 3.Michael JW, Stevens PM. Lower limb prosthetic components: updated classification and passive, body-powered components. In: Krajbich JI, Pinzur MS, Potter BK, Stevens PM, eds. Atlas of Amputations and Limb Deficiencies: Surgical, Prosthetic, and Rehabilitation Principles. 4th Ed Rosemont, IL: American Academy of Orthopedic Surgeons; 2015:429–443. [Google Scholar]
- 4.US Department of Health and Human Services; Agency for Healthcare Quality and Research; National Guideline Clearinghouse. Accessed at: https://www.guideline.gov/browse/clinical-specialty. Accessed September 8, 2017.
- 5.Lin RS, Stevens PM, Wininger M, Castiglione CL. Orthotic management of deformational plagiocephaly: consensus clinical standards of care. Cleft Palate Craniofac J 2016;53(4):394–403. [DOI] [PubMed] [Google Scholar]
- 6.Stevens P, Rheinstein J, Campbell J. Acute postoperative care of the residual limb following transtibial amputation: a clinical practice guideline. Arch Phys Med Rehabil 2016;10:e21. [Google Scholar]
- 7.Stevens P, Rheinstein J, Wurdeman S. Prosthetic foot selection for individuals with lower limb amputation: a clinical practice guideline. J Prosthet Orthot 2018;30(4):175–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stevens P, DePalma R, Wurdeman S. Transtibial socket design, suspension and interface: A clinical practice guideline. J Prosthet Orthot. Epub ahead of print. [Google Scholar]
- 9.Sedki I, Fisher K. Developing prescribing guidelines for microprocessor-controlled prosthetic knees in the South East England. Prosthet Orthot Int 2015;39(3):250–254. [DOI] [PubMed] [Google Scholar]
- 10.Geertzen J, van der Linde H, Rosenbrand K, et al. Dutch evidence-based guidelines for amputation and prosthetics of the lower extremity: amputation surgery and postoperative management. Part 1. Prosthet Orthot Int 2015;39(5):351–360. [DOI] [PubMed] [Google Scholar]
- 11.Geertzen J, van der Linde H, Rosenbrand K, et al. Dutch evidence-based guidelines for amputation and prosthetics of the lower extremity: Rehabilitation process and prosthetics. Part 2. Prosthet Orthot Int 2015;39(5):361–371. [DOI] [PubMed] [Google Scholar]
- 12.Qaseem A, Snow V, Owens DK, et al. The development of clinical practice guidelines and guidance statements of the American College of Physicians: summary of methods. Ann Intern Med 2010;153:194–199. [DOI] [PubMed] [Google Scholar]
- 13.Qaseem A, Humphrey LL, Forciea MA, et al. Treatment of pressure ulcers: a clinical practice guideline from the American College of Physicians. Ann Intern Med 2015;162:370–379. [DOI] [PubMed] [Google Scholar]
- 14.Kannenberg A, Zacharias B, Pröbsting E. Benefits of microprocessor-controlled prosthetic knees to limited community ambulators: Systematic review. J Rehabil Res Dev 2014;51(10):1469–1496. [DOI] [PubMed] [Google Scholar]
- 15.Theeven PJ, Hemmen B, Brink PR, et al. Measures and procedures utilized to determine the added value of microprocessor-controlled prosthetic knee joints: a systematic review. BMC Musculoskelet Disord 2013;14(1):333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Samuelsson KA, Töytäri O, Salminen AL, Brandt Å. Effects of lower limb prosthesis on activity, participation, and quality of life: a systematic review. Prosthet Orthot Int 2012;36(2):145–158. [DOI] [PubMed] [Google Scholar]
- 17.Highsmith MJ, Kahle JT, Bongiorni DR, et al. Safety, energy efficiency, and cost efficacy of the C-Leg for transfemoral amputees: a review of the literature. Prosthet Orthot Int 2010;34(4):362–377. [DOI] [PubMed] [Google Scholar]
- 18.van der Linde H, Hofstad CJ, Geurts AC, et al. A systematic literature review of the effect of different prosthetic components on human functioning with a lower-limb prosthesis. J Rehabil Res Dev 2004;41(4):555–570. [DOI] [PubMed] [Google Scholar]
- 19.Safaeepour Z, Eshraghi A, Geil M. The effect of damping in prosthetic ankle and knee joints on the biomechanical outcomes: a literature review. Prosthet Orthot Int 2017;41(4):336–344. [DOI] [PubMed] [Google Scholar]
- 20.Boonstra AM, Schrama JM, Eisma WH, et al. Gait analysis of transfemoral amputee patients using prostheses with two different knee joints. Arch Phys Med Rehabil 1996;77(5):515–520. [DOI] [PubMed] [Google Scholar]
- 21.Murray MP, Mollinger LA, Sepic SB, et al. Gait patterns in above-knee amputee patients: hydraulic swing control vs. constant-friction knee components. Arch Phys Med Rehabil 1983;64(8):339–345. [PubMed] [Google Scholar]
- 22.Hafner BJ, Smith DG. Differences in function and safety between Medicare Functional Classification Level-2 and −3 transfemoral amputees and influence of prosthetic knee joint control. J Rehabil Res Dev 2009;46(3):417–433. [PubMed] [Google Scholar]
- 23.Kahle JT, Highsmith MJ, Hubbard SL. Comparison of nonmicroprocessor knee mechanism versus C-Leg on Prosthesis Evaluation Questionnaire, stumbles, falls, walking tests, stair descent, and knee preference. J Rehabil Res Dev 2008;45(1):1–14. [DOI] [PubMed] [Google Scholar]
- 24.Hafner BJ, Willingham LL, Buell NC, et al. Evaluation of function, performance and preference as transfemoral amputees transition from mechanical to microprocessor control of the prosthetic knee. Arch Phys Med Rehabil 2007;88(2):207–217. [DOI] [PubMed] [Google Scholar]
- 25.Williams RM, Turner AP, Orendurff M, et al. Does having a computerized prosthetic knee influence cognitive performance during amputee walking? Arch Phys Med Rehabil 2006;87(7):989–994. [DOI] [PubMed] [Google Scholar]
- 26.Berry D, Olson MD, Larntz K. Perceived stability, function and satisfaction among transfemoral amputees using microprocessor and nonmicroprocessor controlled prosthetic knees: a multicenter survey. J Prosthet Orthot 2009;21(1):32–42. [Google Scholar]
- 27.Kaufman KR, Levine JA, Brey RH, et al. Energy expenditure and activity of transfemoral amputees using mechanical and microprocessor-controlled prosthetic knees. Arch Phys Med Rehabil 2008;89(7):1380–1385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gerzeli S, Torbica A, Fattore G. Cost utility analysis of knee prosthesis with complete microprocessor control (C-leg) compared with mechanical technology in trans-femoral amputee. Eur J Health Econ 2009;10(1):47–55. [DOI] [PubMed] [Google Scholar]
- 29.Seelen HAM, Hemmen B, Schmeets AJ, et al. Cost and consequences of a prosthesis with an electronically stance and swing phase controlled knee joint. Technol Disabil 2009;21:25–34. [Google Scholar]
- 30.Brodtkorb TH, Henriksson M, Johannesen-Munk K, et al. Cost-effectiveness of C-leg compared with non-microprocessor-controlled knees: a modeling approach. Arch Phys Med Rehabil 2008;89(1):24–30. [DOI] [PubMed] [Google Scholar]
- 31.Johansson JL, Sherrill DM, Riley PO, et al. A clinical comparison of variable dampening and mechanically passive prosthetic knee devices. Am J Phys Med Rehabil 2005;84(8):563–575. [DOI] [PubMed] [Google Scholar]
- 32.Orendurff MS, Segal AD, Klute GK, et al. Gait efficiency using the C-Leg. J Rehabil Res Dev 2006;43(2):239–246. [DOI] [PubMed] [Google Scholar]
- 33.Segal AD, Orendurff MS, Klute GK, et al. Kinematic and kinetic comparisons of transfemoral amputee gait using C-leg and Mouch SNS prosthetic knees. J Rehabil Res Dev 2006;42(7):857–870. [DOI] [PubMed] [Google Scholar]
- 34.Seymour R, Engbretson B, Kott K, et al. Comparison between the C-leg microprocessor-controlled prosthetic knee and non-microprocessor control prosthetic knees: a preliminary study of energy expenditure, obstacle course performance and quality of life survey. Prosthet Orthot Int 2007;31(1):51–61. [DOI] [PubMed] [Google Scholar]
- 35.Datta D, Heller B, Howitt J. A comparative evaluation of oxygen consumption and gait pattern in amputees using intelligent prostheses and conventionally damped knee swing-phase control. Clin Rehabil 2005;19(4):398–403. [DOI] [PubMed] [Google Scholar]
- 36.Schmalz T, Blumentritt S, Jarasch R. Energy expenditure and biomechanical characteristics of lower limb amputee gait: the influence of prosthetic alignment and different prosthetic components. Gait Posture 2002;16(3):255–263. [DOI] [PubMed] [Google Scholar]
- 37.Klute GK, Berge JS, Orendurff MS, et al. Prosthetic intervention effects on activity of lower-extremity amputees. Arch Phys Med Rehabil 2006;87(5):717–722. [DOI] [PubMed] [Google Scholar]
- 38.Jepson F, Datta D, Harris I, et al. A comparative evaluation of the adaptive knee and catech knee joints: a preliminary study. Prosthet Orthot Int 2008;32(1):84–92. [DOI] [PubMed] [Google Scholar]
- 39.Eberly VJ, Mulroy SJ, Gronley JK, et al. Impact of a stance phase microprocessor controlled knee porsthesis on level walking in lower functioning individuals with a transfemoral amputation. Prosthet Orthot Int 2014;38(6):447–455. [DOI] [PubMed] [Google Scholar]
- 40.Burnfield JM, Eberly VJ, Gronely JK, et al. Impact of stance phase microprocessor controlled knee prosthesis on ramp negotiation and community walking function in K2 level transfemoral amputees. Prosthet Orthot Int 2012;36(1):95–104. [DOI] [PubMed] [Google Scholar]


