Abstract
Rationale:
The kyphosis caused by old osteoporotic vertebral compression fracture usually requires osteotomy to correct it. Various osteotomy techniques have been reported, but each has its own advantages and disadvantages.
Patient concerns:
We reviewed 2 cases of old osteoporotic vertebral compression fractures with kyphosis in our hospital. One patient complained of persistent low-back pain, another patient complained of low-back pain and weakness of both lower extremities.
Diagnosis:
Old osteoporotic vertebral compression fractures with kyphosis were diagnosed based on computer tomography and magnetic resonance imaging.
Interventions:
We performed modified grade 4 osteotomy for 2 patients.
Outcomes:
Both patients said significant improvement in preoperative symptoms, and x-ray showed that the kyphosis was corrected. Both patients were satisfied with the treatment at the last follow-up, and the kyphosis was not aggravated.
Lessons:
Modified grade 4 osteotomy is an effective option for the treatment of old osteoporotic fracture with kyphosis. It can restore the spine sequence and achieve better clinical result.
Keywords: kyphosis, modified grade 4 osteotomy, osteoporotic vertebral compression fracture
1. Introduction
With the aging population increasing, the incidence of osteoporosis is already very high. One osteoporotic fracture occurs every 3 seconds in the world, and one vertebral fracture occurs every 22 seconds.[1] Most patients have no clinical symptoms at onset, and only about one-third of patients see a doctor for pain.[2] Many osteoporotic fractures have evolved into old osteoporotic fractures due to missed diagnosis and undiagnosis.[3] Old osteoporotic fractures often cause kyphosis. The kyphosis deformity is progressively aggravated. Local instability and sagittal imbalance of the spine often lead to intractable low-back pain, which seriously affects the quality of life of the elderly. If conservative treatment is not effective, osteotomy is usually required to correct kyphosis. Many scholars have reported various osteotomy techniques.[4] All these techniques can achieve the purpose of correction kyphosis, but each has its own advantages and disadvantages. Therefore, we propose a modified grade 4 osteotomy with satisfactory orthopedic effect.
2. Case reports
This case report is based on a retrospective design. We reviewed the case data of patients undergoing modified grade 4 osteotomy and collected imaging data from patients. We followed-up the patients for 1 year. The patient's informed consent was obtained for publication of this case report. The study obtained ethics committee approval from The Third Hospital of Shijiazhuang.
2.1. Case 1
A 70-year-old female suffered from back pain after accidental fall over 3 years ago. At that time, the back pain was obvious when turning over and getting out of bed. The x-ray showed: compression fracture of L1. After bed rest and conservative treatment, the back pain was slightly relieved. In the past year, the symptoms of low-back pain gradually worsened. The patient complained of increased low-back pain after walking about 100 meters, standing and sitting about 10 minutes, which seriously affect quality of life. Low-back pain relieved after bed rest. The patient was physically healthy and had no history of hypertension, diabetes, or coronary heart disease.
Physical examination showed that the patient has kyphosis deformity in the standing position. The lumbar vertebrae flexion and extension activities were slightly restricted. There was compression pain in L1 horizontal spinous process and paravertebral and no lower extremity radiation pain. Skin feel and muscle strength were normal. Visual analog scale (VAS) of low-back pain was 6 points, Oswestry Disability Index (ODI) score was 65%.
X-ray, bone density, computer tomography (CT) and magnetic resonance imaging (MRI) were performed after hospitalization. Lateral x-ray showed L1 compression fracture and kyphosis. The Cobb angle was 36°. MRI showed an old compression fracture of L1 vertebral body and no obvious spinal cord compression (Fig. 1). The bone density T value was −2.5. Old osteoporotic vertebral compression fractures with kyphosis and postmenopausal osteoporosis were diagnosed.
Figure 1.
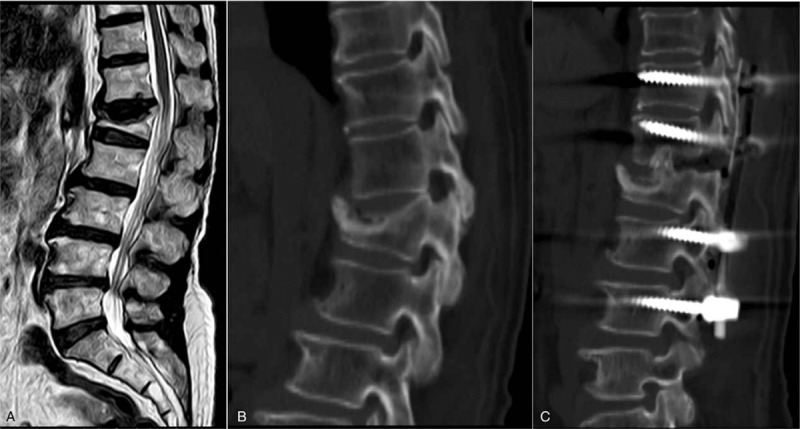
A 70-year-old female presented with an old L1 fracture and low-back pain. The preoperative MRI and CT showed no obvious spinal cord compression (A, B). She was treated with a posterior fusion from T11-L3 with L1 partial pedicular and upper disc subtraction (C).
After the general anesthesia was successful, the neurological monitor was connected and the patient was placed in a prone position. The median longitudinal incision was taken to expose the T11-L3 spinous process, lamina and articular processes. Pedicle screws were implanted through bilateral pedicles of T11, T12, L2, and L3. Completely resect spinous processes of T12 and L1. Burr drill was used to resect part of lamina and bilateral inferior articular processes of T12. Rongeur was used to resect bilateral superior articular process of L1. Remove the ligamentum flavum and reveal the dural sac. A short rod was connected on one side for temporary fixation. With the bilateral nerve roots of T12 were protected, the T12/L1 disc was removed. Burr and osteotome were used to resect the upper 1/3 of the bilateral pedicle of L1. The superior edge of the L1 vertebral body was removed with osteotome. Small bone particles were implanted in the anterior column through the bilateral gap. Blocky spinous processes were implanted in the middle column and serve as a fulcrum. The connecting rods were installed on both sides. Alternating pressure on both sides to close the osteotomy gap and ensure the spinal cord and nerves without compression. X-ray fluoroscopy was satisfactory for correction of kyphosis. Grinding the bilateral T11/T12, L1/L2, L2/L3 joint spaces and implanting small bone particles. Place 2 drainage tubes and suture the incision layer by layer. The vital signs were stable during operation and no abnormalities were observed in the neurological monitoring. The intraoperative blood loss was about 600 mL and the operation time was 4 hours.
The patients were treated with antibiotics for 3 days. The drainage tube was removed when the drainage volume was less than 50 mL/24 h after 3 days. Patient was allowed out of bed with a custom-made plastic orthosis at 5 days after operation. The plastic orthosis was kept for at least 3 months. The suture was removed 12 days after the operation and the patient was discharged. The symptoms of low-back pain were significantly relieved.
The VAS scores at 1 month, 4 months, and 1 year after surgery were 3 points, 1 point, and 0 points, respectively. The ODI scores at 1 month, 4 months, and 1 year after surgery were 40%, 15%, and 5%, respectively. The kyphosis Cobb angles at 1 week, 4 months, and 1 year after surgery were 6°, 7°, and 7°, respectively (Fig. 2). Both clinical efficacy and orthopedic effects were very satisfactory.
Figure 2.
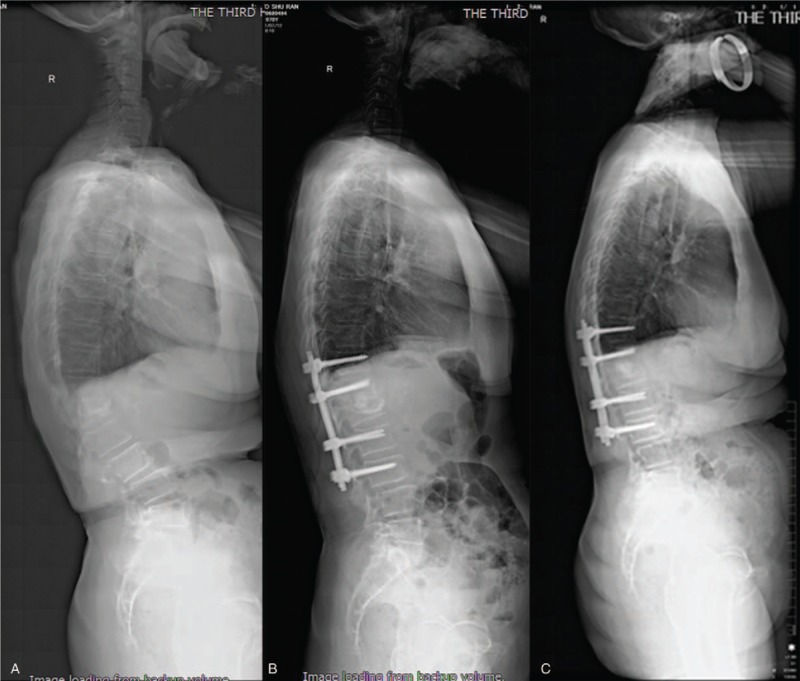
The preoperative Cobb angle is 36° (A). The Cobb angle is 6° at 1 week after operation (B). One year of follow-up revealed a Cobb angle of 7° and solid fusion at the osteotomy site.
2.2. Case 2
A 74-year-old male suffered from low-back pain and limited mobility after accidental fall at 3 months ago. When he turned over and got up, the back pain was obvious. He did not go to the hospital for treatment. After taking painkillers and bed rest, low-back pain relieved, but there are still symptoms of back pain and discomfort when standing and walking. He complained back pain increased after falling again at 20 days ago, accompanied by pain in the front side of the thighs. Gradually he complained weak in both lower limbs and unable to stand and walk. He complained of hypertension and diabetes, but both were stable with the drug control.
Physical examination showed skin pressure sore at bilateral hips. There was compression pain in L1 horizontal spinous processes and paravertebral. Bilateral iliopsoas muscle strength was grade II and bilateral quadriceps muscle strength was grade III. VAS score of low-back pain was 7 points and ODI score was 85%.
X-ray, bone density, CT and MRI were performed after hospitalization. Lateral x-ray showed compression fracture of L1 and kyphosis Cobb angle was 27°. MRI showed disc herniation in L1/L2 level and L1 vertebral body compression fracture (Fig. 3). The bone density T value was −1.9. Old osteoporotic vertebral compression fractures with kyphosis and disc herniation were diagnosed.
Figure 3.
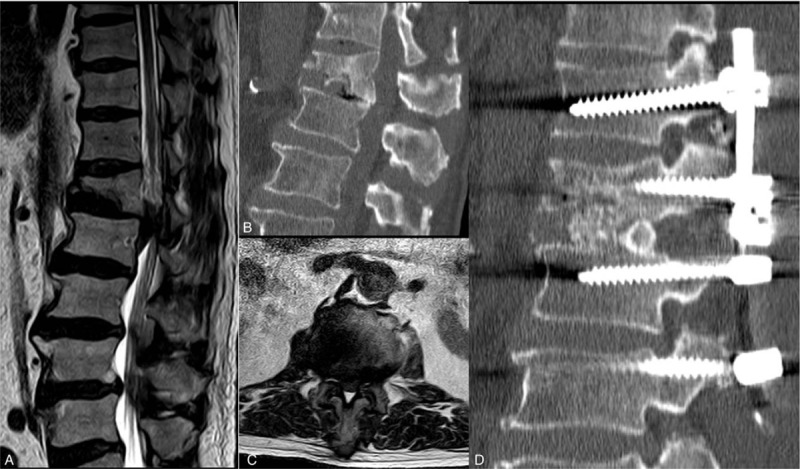
A 74-year-old male with an old L1 fracture, presented with low-back pain and weakness of both lower extremities. The preoperative MRI and CT showed lumbar disc herniation at L1/2 level (A–C). He was treated with a posterior fusion from T12-L3 with L1 partial vertebra and lower disc subtraction (D).
After the general anesthesia was successful, the neurological monitor was connected and the patient was placed in a prone position. The median longitudinal incision was taken to expose the T12-L3 spinous process, lamina, and articular processes. Pedicle screws were implanted through bilateral pedicles of T12, L1, L2, and L3. Completely resect spinous processes, part of lamina, and bilateral inferior articular processes of L1 with burr drill. Rongeur was used to resect bilateral superior articular process of L2. Remove the ligamentum flavum and reveal the dural sac. A short rod was connected on one side for temporary fixation. With the bilateral nerve roots of L1 were protected, the L1/L2 disc was removed. The inferior edge of the L1 vertebral body was removed with osteotome. Small bone particles were implanted in the anterior column through the bilateral gap. Blocky spinous processes were implanted in the middle column and serve as a fulcrum. The connecting rods were installed on both sides. Alternating pressure on both sides to close the osteotomy gap and ensure the spinal cord and nerves without compression. X-ray fluoroscopy was satisfactory for correction of kyphosis. Grinding the bilateral T12/L1, L2/L3 joint spaces and implanting small bone particles. Place 2 drainage tubes and suture the incision layer by layer. The vital signs were stable during operation and no abnormalities were observed in the neurological monitoring. The intraoperative blood loss was about 800 mL and the operation time was 5 hours.
The patients were treated with antibiotics for 3 days. The drainage tube was removed when the drainage volume was less than 50 mL/24 h after 5 days. Patient was allowed out of bed with a custom-made plastic orthosis at 7 days after operation. The plastic orthosis was kept for at least 3 months. The suture was removed 12 days after the operation and the patient was discharged. The symptoms of low-back pain were significantly relieved. Bilateral iliopsoas muscle strength was grade III and bilateral quadriceps muscle strength was grade IV at 1 week after surgery. Patients can walk with a walking aid.
The VAS scores at 1 month and 1 year after surgery were 2 points and 0 points respectively. The ODI scores were 50% and 20%, respectively. Bilateral iliopsoas muscle strength was grade IV and bilateral quadriceps muscle strength was grade V at 1 year after surgery. The kyphosis Cobb angles at 1 week and 1 year after surgery were 6° and 7°, respectively (Fig. 4). Both clinical efficacy and orthopedic effects are very satisfactory.
Figure 4.

The preoperative Cobb angle is 27° (A). The Cobb angle is 6° at 1 week after operation (B). One year of follow-up revealed a Cobb angle of 7° and solid fusion at the osteotomy site (C).
3. Discussion
There are 3 explanations for the causes of low-back pain caused by old vertebral fracture and kyphosis: the microcirculation in the fractured vertebral body is destroyed, and the MRI shows the ischemic necrosis and nonunion in the vertebral body, leading to instability in the vertebral body and causing pain; Old vertebral fractures with kyphosis cause instability of the upper and lower adjacent segments of the fractured vertebral body, causing delayed low-back pain; In patients with thoracolumbar kyphosis, excessive compensatory lumbar lordosis often occurs in order to maintain trunk balance. So the facet joint load of the posterior column is aggravated, and the paravertebral muscles are fatigued due to continuous stretching, resulting in severe pain.[5] Surgical indications for old vertebral fractures with kyphosis include: persistent low-back pain after conservative treatment, progressive thoracolumbar kyphosis, spinal or nerve root injury, pseudoarthrosis or nonunion.[6]
Surgical approaches for kyphosis include anterior, posterior, and anterior-posterior combined approaches. Shota Takenaka compared 3 surgical approaches in the treatment of osteoporotic vertebral fractures. The operation time was significantly longer in anterior–posterior combined group than in the other 2 groups. The postoperative correction of kyphosis was significantly greater in posterior group than in anterior group. Better outcomes were obtained in posterior group in back pain relief at the end point, ambulatory ability at the end point, and average loss of correction.[7] Therefore, posterior surgery is the optimal approach. The posterior approach has the following advantages: the approach is more familiar, obtain firmly fixed, with fewer complications, and the anterior column of the vertebral body can also be reconstructed through the posterior approach. So, both cases were treated with posterior surgery.
Frank Schwab comprehensively analyzed the osteotomy methods reported in the literature and divided the osteotomy technique into 6 grades.[4] Xi et al[8] reported pedicle subtraction osteotomy (PSO) in treatment of post-traumatic thoracolumbar kyphosis. PSO,classified in grade 3 osteotomy, is performed by removing the posterior elements and both pedicles, decancellating vertebral body, and closure of the osteotomy gap by hinging on the anterior cortex. An average of 30° to 40° correction can be achieved with one level PSO.[4]
It is important to note that in a PSO, spine surgeons removed all the posterior ligamentous structures and posterior bony elements. Only the anterior longitudinal ligament and adjacent intervertebral discs were remained to maintain the stability of the spine. Poor local stability leads to high risk of spondylolisthesis and rod fracture. According to Smith et al,[9] the rate of rod fracture among cases that included a PSO was 22.0%, and the fracture occurred at or adjacent to the level of PSO. Upadhyaya et al[10] reported a case with spondylolisthesis following PSO.
Jo et al[11] described modified posterior closing wedge osteotomy for the treatment of posttraumatic thoracolumbar kyphosis. This procedure was classified in grade 4 osteotomy which partial body, pedicle, and upper disk were resected. After the osteotomy is completed, only the intervertebral disc was remained between the osteotomy vertebrae and the lower vertebrae. There was still risk of spondylolisthesis and rod fracture. Gao et al[12] reported modified partial pedicle subtraction osteotomy in the treatment of post-traumatic thoracolumbar kyphosis. In the process, upper disc and upper two-third of the pedicle were resected and the lower facet joint were preserved. The mean correction of focal kyphotic deformity was 34°. According to Hu et al,[13] the main advantages of taking down the disc were the added amount of correction provided, and the additional fusion surface. With a large interspace, however, the spinal column will be excessively shortened which may result in buckling of the dura and spinal cord. In their procedure, after removing the upper disc and posterior elements, a cage containing autogenous bone was put at the anterior column between the lower endplate of the upper vertebra and the osteotomy surface to restore the spinal column height and avoid potential spinal cord curving or kinking. However, since the upper endplate of the fractured vertebral body was removed, the intervertebral cage had risk of sinking.
After comprehensive analysis of these osteotomy techniques, we adopted modified grade 4 osteotomy for kyphosis due to osteoporotic vertebral compression fractures. In case 1, upper disc and upper 1/3 of the bilateral pedicle of L1 were resected, and the lower facet joint were preserved. Therefore, the posterior column structure in L1/2 level remains intact, while maintaining the stability of the spine. In case 2, lower disc and lower half of the vertebral were resected.
After the osteotomy was completed, small bone particles were implanted in the anterior column through the bilateral gap. Blocky spinous processes were implanted in the middle column to preserve the spinal column height and avoid potential spinal cord curving or kinking. Autogenous bone grafts can achieve higher fusion rates and reduce the risk of sinking. Like closing–opening wedge osteotomy, blocky spinous processes in the middle column serve as a fulcrum, the correction was achieved by closing the posterior column and creating an open wedge of the anterior column.[14] After 1 year of follow-up, the patient's clinical effect and the correction of kyphosis were satisfactory.
The modified grade 4 osteotomy is not a completely new surgical method. Instead, it only resect upper part of pedicle and vertebral body to keep the lower facet joint intact or resect lower part of the vertebral body to keep the upper facet joint intact, which can preserve the stability of spine. Blocky spinous processes were implanted in the middle column to preserve the spinal column height and avoid potential spinal cord curving or kinking, achieve higher fusion rates and reduce the risk of sinking, add amount of correction of kyphosis. The modified grade 4 osteotomy is an effective treatment option for kyphosis caused by old osteoporotic vertebral compression fracture.
Author contributions
Conceptualization: Xian-Ze Sun.
Data curation: Zheng-Qi Zhao.
Methodology: Liang Ren.
Supervision: Feng Li.
Validation: Wen-Yuan Ding.
Visualization: Zhen-Fang Gu.
Writing – original draft: Feng-Yu Liu.
Writing – review & editing: Xian-Ze Sun.
Footnotes
Abbreviations: CT = computer tomography, MRI = magnetic resonance imaging, ODI = Oswestry Disability Index, PSO = pedicle subtraction osteotomy, VAS = visual analog scale.
No funds were received in support of this work.
No relevant financial activities outside the submitted work.
The authors have no conflicts of interest to disclose.
References
- [1].Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 2006;17:1726–33. [DOI] [PubMed] [Google Scholar]
- [2].Prather H, Watson JO, Gilula LA. Nonoperative management of osteoporotic vertebral compression fractures. Injury 2007;38:S40–8. [DOI] [PubMed] [Google Scholar]
- [3].Delmas PD, van de Langerijt L, Watts NB, et al. Underdiagnosis of vertebral fractures is a worldwide problem: the IMPACT study. J Bone Miner Res 2005;20:557–63. [DOI] [PubMed] [Google Scholar]
- [4].Diebo B, Liu S, Lafage V, et al. Osteotomies in the treatment of spinal deformities: indications, classification, and surgical planning. Eur J Orthop Surg Traumatol 2014;24Suppl 1:S11–20. [DOI] [PubMed] [Google Scholar]
- [5].Zeng Y, Chen Z, Sun C, et al. Posterior surgical correction of posttraumatic kyphosis of the thoracolumbar segment. J Spinal Disord Tech 2013;26:37–41. [DOI] [PubMed] [Google Scholar]
- [6].Buchowski JM, Kuhns CA, Bridwell KH, et al. Surgical management of posttraumatic thoracolumbar kyphosis. Spine J 2008;8:666–77. [DOI] [PubMed] [Google Scholar]
- [7].Takenaka S, Mukai Y, Hosono N, et al. Major surgical treatment of osteoporotic vertebral fractures in the elderly: a comparison of anterior spinal fusion, anterior-posterior combined surgery and posterior closing wedge osteotomy. Asian Spine J 2014;8:322–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Xi YM, Pan M, Wang ZJ, et al. Correction of post-traumatic thoracolumbar kyphosis using pedicle subtractionosteotomy. Eur J Orthop Surg Traumatol 2013;23Suppl 1:S59–66. [DOI] [PubMed] [Google Scholar]
- [9].Smith JS, Shaffrey E, Klineberg E, et al. Prospective multicenter assessment of risk factors for rod fracture following surgery for adultspinal deformity. J Neurosurg Spine 2014;21:994–1003. [DOI] [PubMed] [Google Scholar]
- [10].Upadhyaya CD, Berven S, Mumaneni PV. Spondylolisthesis following a pedicle subtraction osteotomy. Case report. Neurosurg Focus 2010;28:E16. [DOI] [PubMed] [Google Scholar]
- [11].Jo DJ, Kim YS, Kim SM, et al. Clinical and radiological outcomes of modified posterior closing wedge osteotomy for the treatment of posttraumatic thoracolumbar kyphosis. J Neurosurg Spine 2015;23:510–7. [DOI] [PubMed] [Google Scholar]
- [12].Gao R, Wu J, Yuan W, et al. Modified partial pedicle subtraction osteotomy for the correction of post-traumatic thoracolumbar kyphosis. Spine J 2015;15:2009–15. [DOI] [PubMed] [Google Scholar]
- [13].Hu W, Wang B, Run H, et al. Pedicle subtraction osteotomy and disc resection with cage placement in post-traumatic thoracolumbar kyphosis, a retrospective study. J Orthop Surg Res 2016;11:112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Chang KW, Cheng CW, Chen HC, et al. Closing-opening wedge osteotomy for the treatment of sagittal imbalance. Spine (Phila Pa 1976) 2008;33:1470–7. [DOI] [PubMed] [Google Scholar]


