Abstract
Rationale:
Mitochondrial encephalopathy, lactic acidosis and stroke-like episodes (MELAS) are thought to be rarely accompanied by macroangiopathy. We reported a case of MELAS that presented right distal internal carotid arterial (ICA) stenosis and reviewed 12 similar previously reported cases involving intracranial large blood vessels.
Patient concerns:
A 38-year-old man suffered from recurrent stroke-like episodes (SE) such as alternating hemiparesis (right lesion 3 years ago and current left lesion), cortical blindness and seizure for 3 years, and was previously misdiagnosed as cerebral infarction. Magnetic Resonance Angiography (MRA) and Digital Subtraction Angiography (DSA) revealed right distal ICA stenosis and sparse cortex blood vessels, which were related to the previous SE.
Diagnoses:
He was diagnosed by genetic screening (a mitochondrial DNA A3243G point mutation) and presence of high lactic acidosis (4.03 mmol/L), which rose to 7.8 mmol/L after exercise.
Intervention:
The patient received Coenzyme Q10, vitamin C, L-arginine for 2 weeks and valproic acid sodium (400 mg bid) to prevent seizures till now.
Outcomes:
He is currently less active and intelligent than his peers, with occasional seizures, and needs family care.
Lessons:
Till date, there are 12 reported cases of MELAS combined with major cerebral arteries abnormalities including stenosis, dissection, occlusion, reversible vasoconstriction, aneurysms, and atherosclerosis. Hence, macroangiopathy in MELAS is not very rare. There is correlation between the affected vessels and the lesions in some cases, but not in others, which may increase the misdiagnosis rate. Hence, mitochondrial diseases cannot be excluded due to concurrent macroangiopathic lesions
Keywords: cerebral infarction, macroangiopathy, MELAS, stroke episode
1. Introduction
Mitochondrial encephalopathy, lactic acidosis, and stroke-like episodes (MELAS) is the most common subtype of mitochondrial encephalopathy. It is most commonly caused by point mutations at the A3243G of the tRNA LEU gene in the mitochondrial DNA (mtDNA). This, in turn, affects mitochondrial protein synthesis and nutrient metabolism, leading to disease. The onset of illness is often in early adulthood. Symptoms include headache, vomiting, hemiplegia, blindness, and epileptic seizures. Patients generally have short stature and low intelligence.[1]
Since stroke-like episodes (SE) are similar to acute cerebral infarction, they are often misdiagnosed.[2] The main point of the differential diagnosis with infarction is that the lesion area and cerebral arterial blood supply area are inconsistent, and the macroangiopathy in MELAS is rarely involved.[3] Herein, we reported a case of MELAS that presented with SE, right distal internal carotid arterial (ICA) stenosis and sparse cortex blood vessels. We also reviewed 12 similar previously reported cases involving intracranial large blood vessels.
2. Case report
2.1. Patient information
A 38-year-old man was admitted to our department due to right hemiparesis, cortical blindness on right half side of both eyes for 1 month. He was diagnosed as cerebral infarction at another hospital and had received aspirin and a statin for 1 month, but his symptoms did not improve significantly. He had haven migraine headache since he was 18 years old. But he had no diabetes mellitus. Three years ago, he had left hemiparesis and left cortical blindness from which he recovered, but had recurrent seizures from than on. His activity endurance decreased during childhood, with progressive bilateral hearing weakness for many years. He had no family history. He was unemployed, with no-toxic contact, alcohol, tobacco or other bad habits.
2.2. Physical examination and diagnostic assessment
His body temperature was 36.5 °C, blood pressure was 123/70 mmHg, and pulse was 68 beats per minute. Physical examination revealed short stature (160 cm height and 45 kg weight), language disability, immature behavior, and biocular visual field defect on right side. The pupil was 4 cm, and the light reflection was normal. Bilateral hearing was weak. Right muscle strength was level 4 and left muscle strength was level 5. Bilateral tendon reflexes were active. The bilateral Babinski sign was negative.
The laboratory data at admission showed high glutamic-pyruvic transaminase (GPT) (52 u/L) and triglyceride (2.3 mmol/L). The patient was suspected as MALES due to elevated lactate (4.03 mmol/L), which rose to 7.8 mmol/L after exercise. He refused muscle biopsy. A genetic study of the patient's peripheral blood leukocytes revealed a mtDNA A3243G point mutation (Fig. 1).
Figure 1.
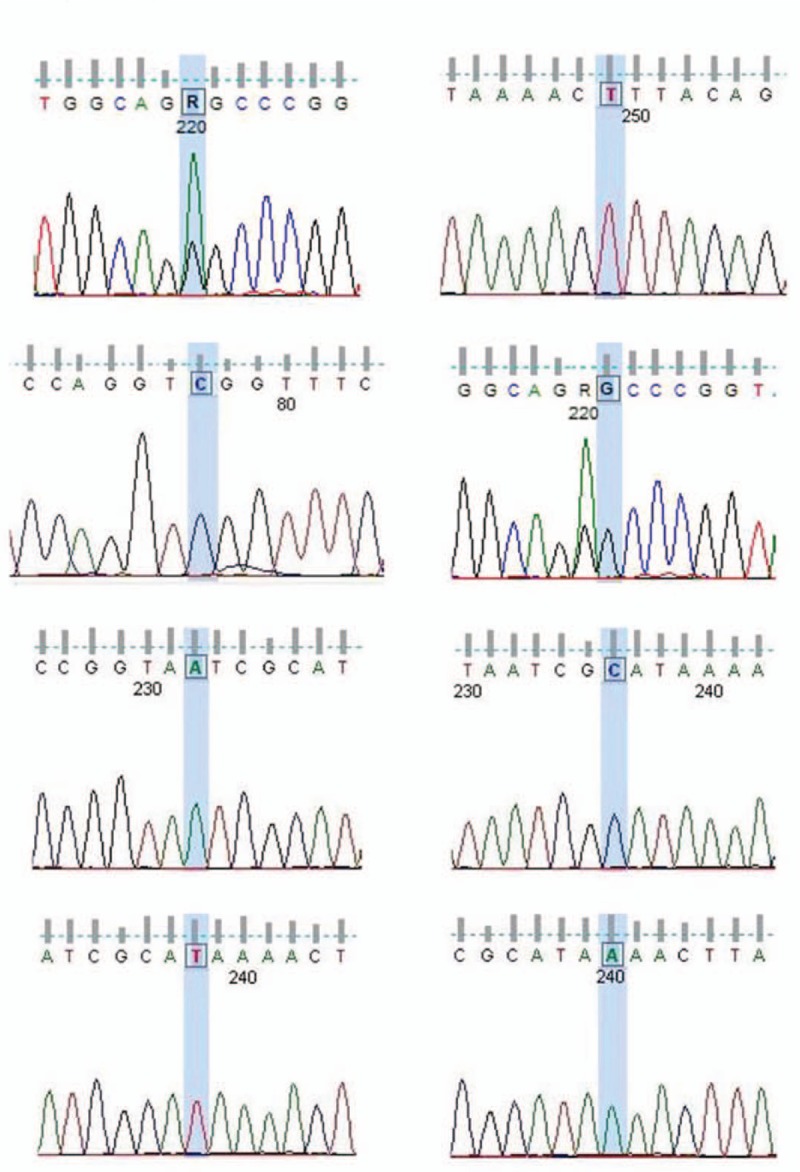
Genetic screening showed a mitochondrial DNA A3243G point mutation.
Brain MRI (3.0 Tesla) at admission revealed a hyperintense lesion in the left occipital lobe in DWI and T2, and right occipital lobe atrophy (Fig. 2). MR angiography (MRA) revealed segmental stenosis at the C7 and M1 junctions, and sparse cortex blood vessels (Fig. 3). The same lesion was persistent and confirmed by digital subtraction angiography (DSA) (Fig. 4) after 20 days. It was a pity that he only received plain CT scanning 3 years ago, without CT angiography (CTA) or MRA.
Figure 2.
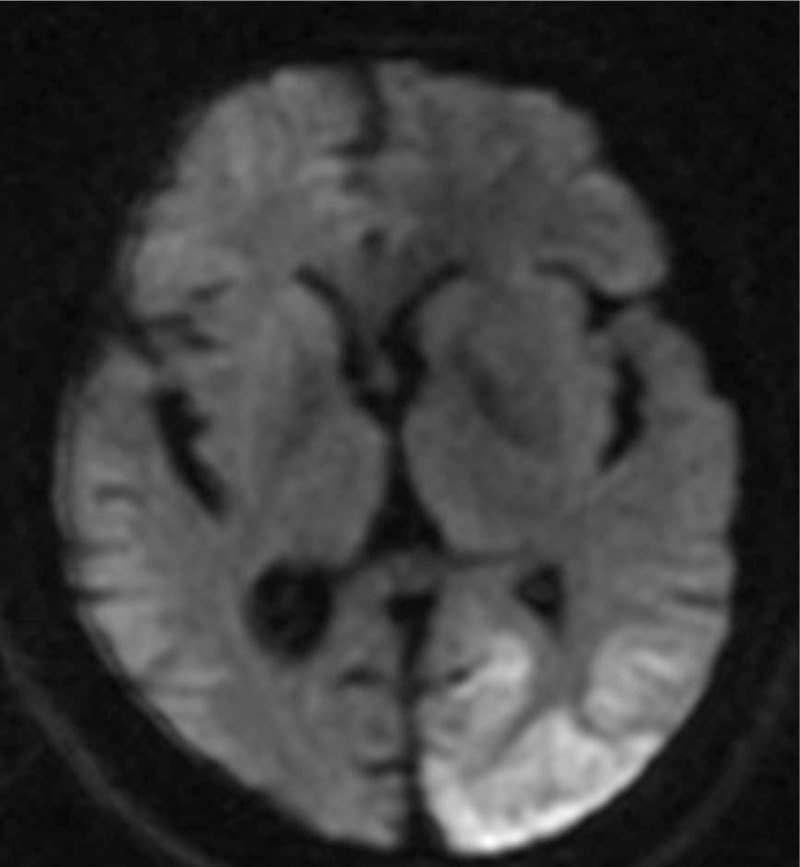
New lesion in the left occipital lobe and atrophy in the right occipital lobe.
Figure 3.
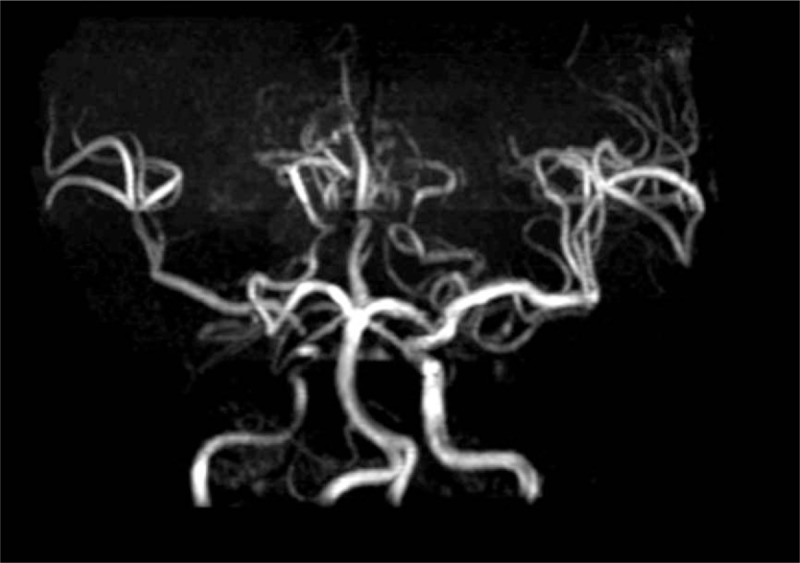
MRA showed stenosis of right ICA. ICA = internal carotid artery, MRA = Magnetic Resonance Angiography.
Figure 4.
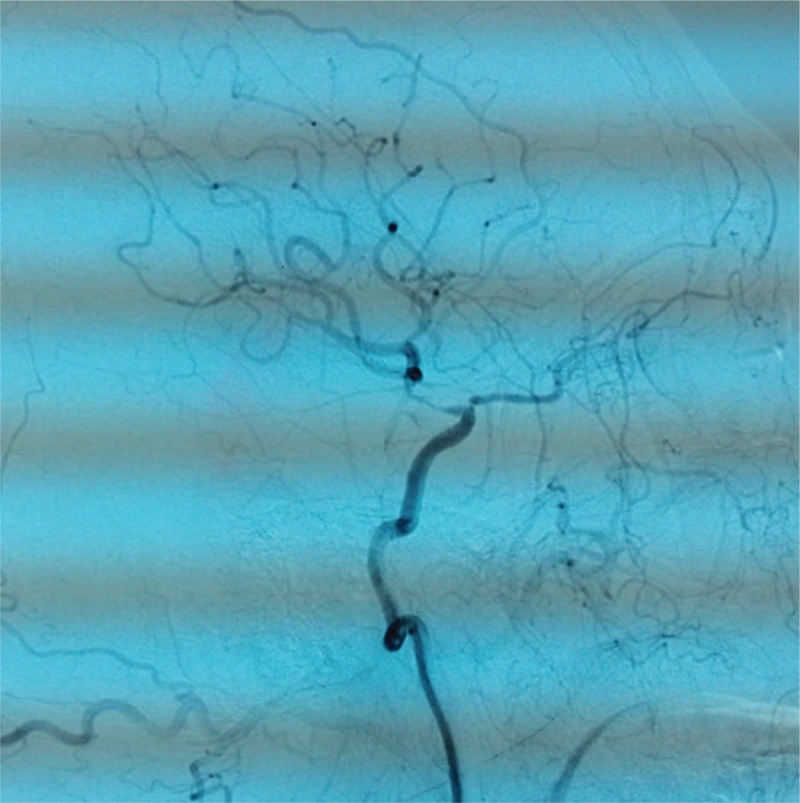
DSA showed stenosis of right ICA. DSA = digital subtraction angiography, ICA = internal carotid artery.
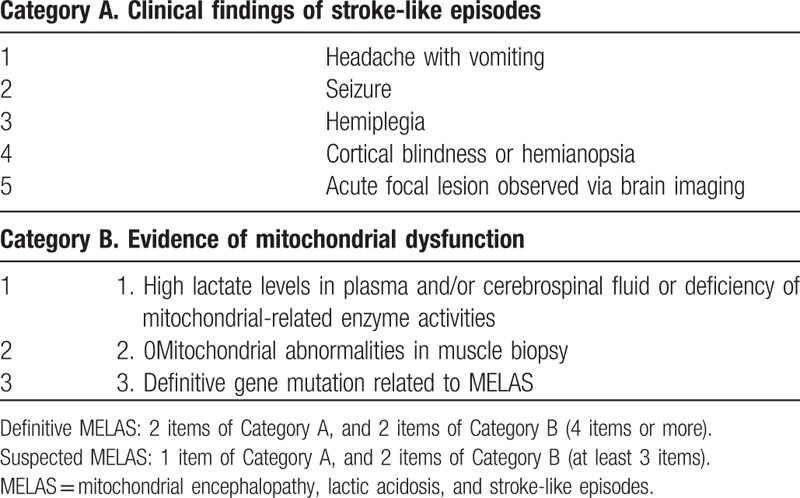
According to the Japanese diagnostic criteria of MELAS developed by Yatsuga[4] (Table 1).The patient met 2, 3, 4, and 5 in Category A, and 1 and 3 in Category B, so he was definitively diagnosed as MELAS.
Table 1.
Japanese diagnostic criteria for MELAS[4].
2.3. Therapeutic interventions
He received Coenzyme Q10 100 mg qd, vitamin C 0.5 tid, L-arginine and valproic acid sodium 0.4 bid from he was in hospital to now nearly 1year.
2.4. Follow-up and outcomes
From he was dismissed from hospital 1year ago to now, he has no SE and his visual field defect improved. He is currently less active and intelligent than his peers, with occasional seizures but less than before, and needs family care now.
3. Discussion
MELAS is a rare genetic, metabolic disease that involves multiple organs. Notably, SEare often misdiagnosed as cerebral infarction.[2] Unlike a stroke that is caused by intracranial vascular disease, SE was thought to be caused by energy metabolic disorders of brain cells and microangiopathy.[5,6] Much of the evidence of microangiopathy came from the patient's peripheral muscle biopsies, which showed abnormal mitochondrial accumulation in the media and endothelium of the small vessels due to lack of energy.[7] The same phenomenon was also found in the tunica media of the walls of pial arterioles and small arteries up to 250 mu in diameter.[8] This impairment of respiratory chain function led to oxidative stress causing a reduction of nitric oxide availability and flow-mediated vasodilatation.[9]
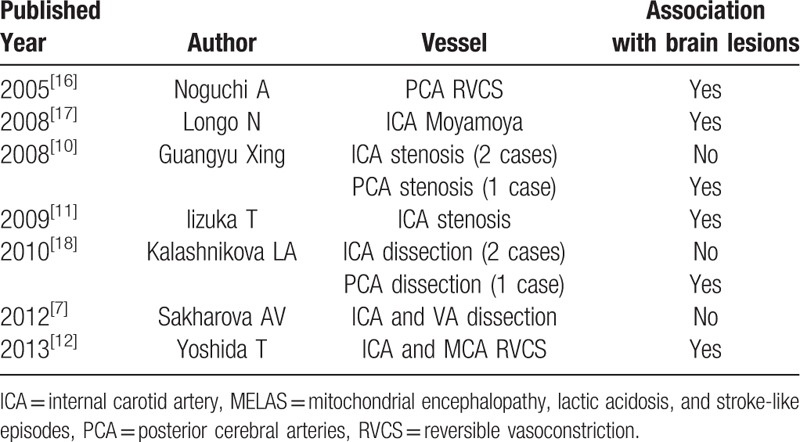
Although both intracranial vascular biopsy[5,7] and nitric oxide-mediated vascular dilatation,[9] showed no serious intracranial vascular disease in MELAS patients. However, the present case provided evidence that the vessel wall was a target of damaged mitochondrial respiration. With the popularization of cerebrovascular imaging, the changes of intracranial and extracranial vessels were observed in some patients with stenosis,[10] Moyamoya syndrome,[11] reversible vasoconstriction,[12] aneurysms,[13] dissection,[7] and atherosclerosis.[14] Some cases may be associated with cerebral lesions, while others may not (Table 2). Since most cases are diagnosed by imaging, there is no evidence of intracranial vascular pathology. Aortic rupture was reported in a case of MELAS harboring A3243G mutation as a phenotype of macroangiopathy, in which marked disarray of the smooth muscle architecture of the aorta was demonstrated.[15] The most important factor is that the mitochondrial abnormality in large cerebral vessels caused vessel wall “weakness” leading to incomplete vascular wall structure.[11] Other relevant factors include mitochondrial disease complicated by diabetes and hyperlipidemia, which may lead to atherosclerotic stenosis,[14] vasospasm caused by nitric oxide insufficiency[9] and vasculitis.
Table 2.
Cases with macroangiopathy in MELAS.
The cause of ICA stenosisin of this patient could be the collapse of blood vessels caused by weak vascular structure due to the following reasons: Right ICA stenosis was found at admission by MRA and persisted for 20 days as confirmed by DSA, which could be related to the previous episode 3 years ago. The sparse cortex blood vessels of right middle cerebral artery (MCA) could be due to ICA stenosis.
3.1. Analysis of previous misdiagnosis of this patient
First: Insufficient knowledge of MELAS. The patient was young, short and immature, with recurrent seizures, multiple intracranial lesions mainly in the occipital lobe cortex. The clinical manifestations of MELAS are typical, although without pathological basis.
Second: Insufficient attention was given to laboratory examination. The absence of GPT/lactic acid elevation after 1 month when the patient recovered is a good indication of MELAS.
Third: The doctor may have considered macroangiopathy as a standard for exclusion of MELAS.
Although MELAS patients with macroangiopathy are uncommon in clinical practice, macrovascular stenosis and other lesions exist in some patients, and the macroangiopathy is partially due to stroke. Hence, mitochondrial diseases cannot be excluded due to concurrent macroangiopathic lesions.
Author contributions
Conceptualization: Xiangrong Sun, Guohui Jiang, Xinyue Ju.
Formal analysis: Xiangrong Sun, Guohui Jiang, Xinyue Ju, Hongmei Fu.
Investigation: Xiangrong Sun, Xinyue Ju, Hongmei Fu.
Methodology: Xiangrong Sun, Guohui Jiang, Hongmei Fu.
Supervision: Xiangrong Sun, Guohui Jiang, Xinyue Ju.
Validation: Hongmei Fu.
Visualization: Xiangrong Sun, Guohui Jiang, Xinyue Ju.
Writing – original draft: Xiangrong Sun.
Writing – review & editing: Xiangrong Sun, Guohui Jiang, Xinyue Ju, Hongmei Fu.
Footnotes
Abbreviations: DSA = digital subtraction angiography, GPT = glutamic pyruvic transaminase, ICA = internal carotid artery, MELAS = mitochondrial encephalopathy, lactic acidosis, and stroke-like episodes, MRA = Magnetic Resonance Angiography, mtDNA = mitochondrial DNA, SE = stroke-like episodes.
This work was supported by North Sichuan Medical College Project [CBY12-A-ZP11].
The authors declare that they have no conflict of interest.
Written informed consent was obtained from the patient.
References
- [1].El-Hattab AW, Adesina AM, Jones J, et al. MELAS syndrome: clinical manifestations, pathogenesis, and treatment options. Mol Genet Metab 2015;116:4–12. [DOI] [PubMed] [Google Scholar]
- [2].Xiao Z, Li Y, Wang H. Mitochondrial myopathy, encephalopathy, lactic acidosis and stroke-like episodes (MELAS):were misdiagnosed as cerebral infarction. Clin Misdianosis Misther 2014;27:22–4. [Google Scholar]
- [3].Danks RA, Dorevitch M, Cummins JT, et al. Mitochondrial myopathy, encephalopathy, lactic acidosis and stroke-like episodes (MELAS): adolescent onset with severe cerebral edema. Aust N Z J Med 1988;18:69–72. [DOI] [PubMed] [Google Scholar]
- [4].Yatsuga S, Povalko N, Nishioka J, et al. MELAS: a nationwide prospective cohort study of 96 patients in Japan. Biochim Biophys Acta 2012;1820:619–24. [DOI] [PubMed] [Google Scholar]
- [5].Gilchrist JM, Sikirica M, Stopa E, et al. Adult-onset MELAS. Evidence for involvement of neurons as well as cerebral vasculature in strokelike episodes. Stroke 1996;27:1420–3. [DOI] [PubMed] [Google Scholar]
- [6].Sarnat HB, Flores-Sarnat L, Casey R, et al. Endothelial ultrastructural alterations of intramuscular capillaries in infantile mitochondrial cytopathies: “mitochondrial angiopathy”. Neuropathology 2012;32:617–27. [DOI] [PubMed] [Google Scholar]
- [7].Sakharova AV, Kalashnikova LA, Chaikovskaia RP, et al. Morphological signs of mitochondrial cytopathy in skeletal muscles and micro-vessel walls in a patient with cerebral artery dissection associated with MELAS syndrome. Arkh Patol 2012;74:51–6. [PubMed] [Google Scholar]
- [8].Ohama E, Ohara S, Ikuta F, et al. Mitochondrial angiopathy in the cerebral blood vessels of MELAS (mitochondrial myopathy, encephalopathy, lactic acidosis and strokelike episodes). No To Shinkei 1988;40:109–18. [PubMed] [Google Scholar]
- [9].Vattemi G, Mechref Y, Marini M, et al. Increased protein nitration in mitochondrial diseases: evidence for vessel wall involvement. Mol Cell Proteomics 2011;10:M110.002964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Guangyu Xing, Chuan-Qiang PU, Wei-Ping WU. Radiological features of cerebral artery in patients with mitochondrial encephalomyopathy. J Brain Nervous Dis 2008;12:123–5. [Google Scholar]
- [11].Iizuka T, Goto Y, Miyakawa S, et al. Progressive carotid artery stenosis with a novel tRNA phenylalanine mitochondrial DNA mutation. J Neurol Sci 2009;278:35–40. [DOI] [PubMed] [Google Scholar]
- [12].Yoshida T, Ouchi A, Miura D, et al. MELAS and reversible vasoconstriction of the major cerebral arteries. Intern Med 2013;52:1389–92. [DOI] [PubMed] [Google Scholar]
- [13].Zhu K, Li S, Chen H, et al. Late onset MELAS with m.3243A >G mutation and its association with aneurysm formation. Metab Brain Dis 2017;32:1069–72. [DOI] [PubMed] [Google Scholar]
- [14].Racaru V, Righez C, Chachati A. A clinical case of mitochondrial diabetes. Revue Médicale De Liège 2014;69:12–5. [PubMed] [Google Scholar]
- [15].Tay SH, Nordli DR, Jr, Bonilla E, et al. Aortic rupture in mitochondrial encephalopathy, lactic acidosis, and stroke-like episodes. Arch Neurol 2006;63:281–3. [DOI] [PubMed] [Google Scholar]
- [16].Noguchi A(1), Shoji Y, Matsumori M, et al. Stroke-like episode involving a cerebral artery in a patient with MELAS. Pediatr Neurol 2005;33:70–1. [DOI] [PubMed] [Google Scholar]
- [17].Longo N1, Schrijver I, Vogel H, et al. Progressive cerebral vascular degeneration with mitochondrial encephalopathy. Am J Med Genet A 2008;146:361–7. [DOI] [PubMed] [Google Scholar]
- [18].Kalashnikova LA, Sakharova AV, Dobrynina LA, et al. Mitochondrial arteriopathy as a cause of spontaneous dissection of cerebral arteries. Zh Nevrol Psikhiatr Im S S Korsakova 2010;110:3–11. [PubMed] [Google Scholar]


