Abstract
This retrospective study aimed to investigate the feasible effectiveness of acupuncture at pain acupoints for the treatment of patients with cervical cancer pain (CCP). A total of 64 cases were analyzed. All these cases were assigned to an acupuncture group or a control group according to the different therapies they received. The cases in the acupuncture group received acupuncture treatment at pain acupoints, while the subjects in the control group underwent acupuncture at regular acupoints. The primary endpoint was CCP, assessed by numeric rating scale (NRS). The secondary endpoints were evaluated by the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire-Core 30 (EORTC QLQ-C30), and Karnofsky Performance Status (KPS). In addition, adverse events were also recorded during the treatment period. After treatment, patients in the acupuncture group exerted greater outcomes in CCP reduction when compared with patients in the control group (P < .01). In addition, no adverse events were recorded in either group. The results of this study showed that acupuncture at pain acupoints might be efficacious in patients with CCP after 14-day treatment.
Keywords: acupuncture, adverse event, cancer pain, cervical cancer, effectiveness
1. Introduction
Cervical cancer (CC) is the second most common cancer among female population worldwide.[1,2] It is also the primary causes of death in women with CC.[3,4] It has been estimated that it is responsible for about 85% of total new cases (more than 530,000 cases) around the world, and about 7.5% deaths of all women cancer (more than 275,000 mortality) annually.[5–7]
Persistent human papilloma virus (HPV) infection and subsequent malignant transformation are supposed to cause CC in more than 95% cases.[8,9] Additionally, other factors can also account for CC, such as precocious intercourse, multiple sexual partners, high parity, smoking, or human immunodeficiency virus HIV.[8,9] Of those, persistent infection of HPV is the most common cause of CC.[9] Therefore, the most effective prevention of CC is the screening and HPV vaccination by utilizing bivalent or quadrivalent vaccine.[1]
Cancer pain is one of the most distressing and intractable conditions in patients with cancer.[10–13] It has been reported that about 20% to 30% of cancer patients who bear a variety of levels of cancer pain.[14,15] Although various pain medications have been utilized for pain relief in many cancer patients, the efficacy is still not satisfied, especially in patients with advanced cancer pain.[16–18] Although analgesics, such as opioids has been widely used for cancer pain management, serious side effects are often accompanied, including constipation, respiratory inhibition, nausea, vomiting, sleep disorder, hallucinations, and drug resistance.[19,20]
Acupuncture is recommended as one of the most potential candidates for cancer pain control.[21–23] Previous studies have reported that it not only has beneficial efficacy for cancer pain management, but also almost has no adverse events for patients with cancer pain.[22] Moreover, few data are available for acupuncture for treating patients with cervical cancer pain (CCP). Additionally, no study specifically explored the effectiveness of acupuncture at pain acupoints for CCP. Therefore, this study explored the effectiveness of acupuncture at pain acupoints for the management of patients with CCP.
2. Patients and methods
2.1. Ethical consideration
This pilot study was approved by the Medical Ethics Committee of The Second Affiliated Hospital of Shaanxi University of Chinese Medicine.
2.2. Design
This pilot study was designed as a retrospective study. The written informed consent from each case was waived because all the data were collected from completed medical records. All the cases were collected between February 2017 and January 2018 at gynecology department of Second Affiliated Hospital of Shaanxi University of Chinese Medicine. A total of 64 cases were analyzed, and were assigned to an acupuncture group, and a control group according to the different treatments they received. Each group analyzed 32 cases. The cases in the acupuncture group received acupuncture at pain acupoints, while the subjects in the control group underwent acupuncture at regular acupoints. All patients in both groups were treated for a total of 14 days.
2.3. Subjects
All patients with confirmed diagnosed of CC at Stage II, III, or IV by the tests of cervical scraping smear and biopsy. Additionally, All subjects were included if they mainly complained CCP, more than 18 years old, at least had 3 months life expectancy, and had normal hearing and communication skills, as well as had ability to evaluate outcomes independently. However, patients were excluded if they suffered from unrelated cancer pain, mental illness, pregnancy, or lactating subjects. In addition, if the patients previously had received acupuncture or similar therapy 1 month before the treatment was also excluded.
2.4. Treatment schedules
Patients in the acupuncture group received acupuncture treatment at local pain acupoints. Sterile disposable acupuncture needles (40 mm in length and 0.30 mm in diameter; Andy brand) were utilized to treat patients with CCP. It was manufactured by Guizhou Andy Medical Instrument Co. It was administered for 30 min each session, with 1 session daily for a total of 14 days. All cases were reported to achieve deqi during the period of their treatments.
Patients in the control group underwent acupuncture therapy at commonly used acupoints of Zusanli (ST36, 3 cun below the lower border of the patella, 1 finger width lateral from the anterior border of the tibia) and Sanyinjiao (SP6, 3 cun directly above the tip of the medial malleoulus on the posterior border of the tibia) according to the previous published studies.[24–26] The acupuncture needles were the same as them in the intervention group used. It also had the same treatment session, as well as the treatment period.
2.5. Endpoint measurements
The primary endpoint was assessed by numeric rating scale (NRS).[27] It ranges from 0, no pain, to 10, the worst pain, with higher score indicating worse pain. The secondary endpoints included European Organization for Research and Treatment of Cancer Quality of Life Questionnaire-Core 30 (EORTC QLQ-C30). The score varies from 0 to 100, with higher score indicating a higher response level.[28] In addition, the tool of Karnofsky Performance Status (KPS) was also used to assess the efficacy.[29] The scores range from 0 to 100. A higher score means the better able to carry out daily activities. All primary and secondary endpoints were measured before and after 14 days of treatment.
2.6. Statistical analysis
All data of characteristic and endpoints were analyzed by using SPSS software (SPSS V.15.0, IBM Corp., Armonk, NY). Fisher exact test was used to analyze dichotomous data, and Mann–Whitney U test was used to perform continuous data. The value of P < .05 was regarded as a statistical significance.
3. Results
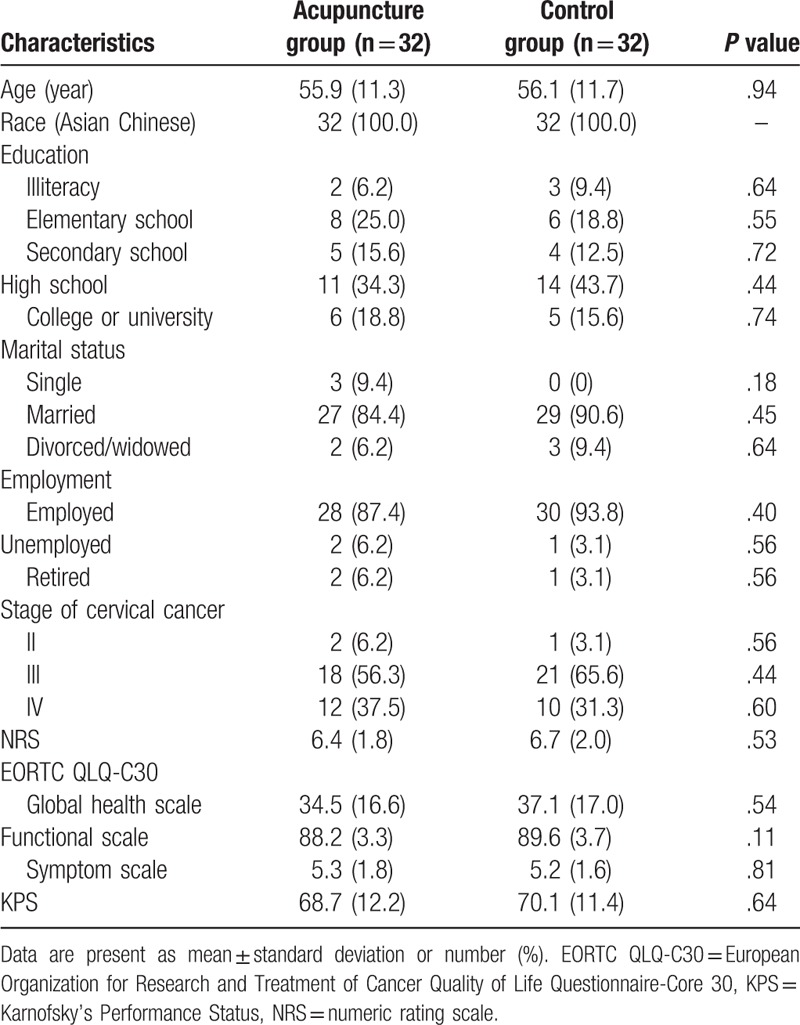
The characteristic values of all included patients are listed in Table 1. There were no significant differences regarding all these values between 2 groups in the present study.
Table 1.
Patient characteristic values before the treatment.
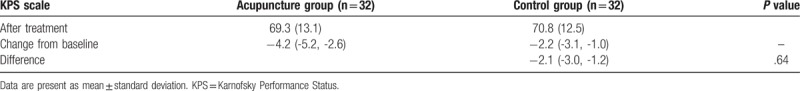
After 14-day treatment, patients in the acupuncture group showed more promising effectiveness in NRS score (P < .01; Table 2), except the EORTC QLQ-C30 scores (Global health scale, P = .20; Functional scale, P = .35; Symptom scale, P = .40; Table 3), and KPS scale (P = .64, Table 4), compared with patients in the control group.
Table 2.
Comparison of NRS scores between 2 groups.
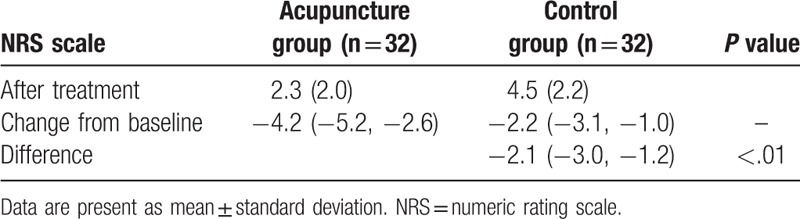
Table 3.
Comparison of EORTC QLQ-C30 scores between 2 groups (Change from baseline).

Table 4.
Comparison of KPS scores between 2 groups.
No adverse events were documented in both groups during the 14-day treatment period.
4. Discussion
A previous study reported the effectiveness of acupuncture for cancer pain and related symptoms.[30] It did not only explore the effectiveness of acupuncture for cancer pain, but also for the nausea, vomiting, constipation, pruritus, neuropathy, and joint pain.[30] Although no conclusion of acupuncture management on cancer pain was made in that study, it provided clinical clues for the further studies.
Presently, no study investigated the effectiveness of acupuncture at pain acupoints for CCP. To our best knowledge, this pilot study firstly conducted the feasible effectiveness of acupuncture at pain acupoints for CCP among Chinese female population. Although it is still a pilot study, it may provide more helpful information for either the clinical therapists, or for the searchers of future clinical trials to further investigate the effectiveness of acupuncture at pain acupoints for patients with CCP.
The results of this study demonstrated that patients who received acupuncture treatment at pain acupoints for CCP had more promising effectiveness than patients who underwent acupuncture management at regular acupoint, although patients did not differ significantly at other outcome measurements of EORTC QLQ-C30 and KPS scores. It indicated that acupuncture at pain acupoints for CCP may be efficacious among female CC population.
This study has several limitations. First, the sample size was relatively small, which just investigated the feasible effectiveness of acupuncture at pain acupoints for CCP. Second, it only included the treatment period of 14 days, thus, it may still not long enough to exert positive results for other outcome measurements, except the pain evaluation. Third, lacking randomization application may increase the selection risk. Fourth, follow-up assessments should still be considered in future studies.
5. Conclusion
This study showed that acupuncture at pain acupoints might be effective for patients with CCP after 14-days treatment.
Author contributions
Conceptualization: Fan-feng Meng, Yan-hong Feng.
Data curation: Fan-feng Meng, Yan-hong Feng.
Formal analysis: Yan-hong Feng.
Investigation: Yan-hong Feng.
Methodology: Yan-hong Feng.
Project administration: Fan-feng Meng.
Resources: Fan-feng Meng, Yan-hong Feng.
Software: Yan-hong Feng.
Supervision: Fan-feng Meng.
Validation: Fan-feng Meng, Yan-hong Feng.
Visualization: Fan-feng Meng, Yan-hong Feng.
Writing – original draft: Fan-feng Meng, Yan-hong Feng.
Writing – review & editing: Fan-feng Meng, Yan-hong Feng.
Footnotes
Abbreviations: CCP = cervical cancer pain, EORTC QLQ-C30 = European Organization for Research and Treatment of Cancer Quality of Life Questionnaire-Core 30, KPS = Karnofsky performance status, NRS = numeric rating scale.
The authors have no conflicts of interest to disclose.
References
- [1].Alber JM, Brewer NT, Melvin C, et al. Reducing overuse of cervical cancer screening: a systematic review. Prev Med 2018;116:51–9. [DOI] [PubMed] [Google Scholar]
- [2].Yang H, Zhang X, Hao Z. The diagnostic accuracy of a real-time optoelectronic device in cervical cancer screening: a PRISMA-compliant systematic review and meta-analysis. Medicine (Baltimore) 2018;97:e11439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Krakow M, Yale RN, Perez Torres D, et al. Death narratives and cervical cancer: Impact of character death on narrative processing and HPV vaccination. Health Psychol 2017;36:1173–80. [DOI] [PubMed] [Google Scholar]
- [4].de Freitas LM, Serafim RB, de Sousa JF, et al. Photodynamic therapy combined to cisplatin potentiates cell death responses of cervical cancer cells. BMC Cancer 2017;17:123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Jemal A, Bray F, Center MM, et al. Global cancer statistics. CA Cancer J Clin 2011;61:69–90. [DOI] [PubMed] [Google Scholar]
- [6].Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin 2012;62:10–29. [DOI] [PubMed] [Google Scholar]
- [7].Sharma M, Bruni L, Diaz M, et al. Using HPV prevalence to predict cervical cancer incidence. Int J Cancer 2013;132:1895–900. [DOI] [PubMed] [Google Scholar]
- [8].Hang D, Yin Y, Han J, et al. Analysis of human papillomavirus 16 variants and risk for cervical cancer in Chinese population. Virology 2016;488:156–61. [DOI] [PubMed] [Google Scholar]
- [9].Lorin L, Bertaut A, Hudry D, et al. About invasive cervical cancer: A French population based study between 1998 and 2010. Eur J Obstet Gynecol Reprod Biol 2015;191:1–6. [DOI] [PubMed] [Google Scholar]
- [10].Yamanaka M. A concept analysis of self-management of cancer pain. Asia Pac J Oncol Nurs 2018;5:254–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Brant JM. Assessment and management of cancer pain in older adults: strategies for success. Asia Pac J Oncol Nurs 2018;5:248–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Portenoy RK, Ahmed E. Cancer pain syndromes. Hematol Oncol Clin North Am 2018;32:371–86. [DOI] [PubMed] [Google Scholar]
- [13].Fink RM, Brant JM. Complex cancer pain assessment. Hematol Oncol Clin North Am 2018;32:353–69. [DOI] [PubMed] [Google Scholar]
- [14].Vellucci R, Mediati RD, Gasperoni S, et al. Assessment and treatment of breakthrough cancer pain: from theory to clinical practice. J Pain Res 2017;10:2147–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Georgesen J, Dungan JM. Managing spiritual distress in patients with advanced cancer pain. Cancer Nurs 1996;19:376–83. [DOI] [PubMed] [Google Scholar]
- [16].Lema MJ. Invasive analgesia techniques for advanced cancer pain. Surg Oncol Clin N Am 2001;10:127–36. [PubMed] [Google Scholar]
- [17].Marinangeli F, Ciccozzi A, Leonardis M, et al. Use of strong opioids in advanced cancer pain: a randomized trial. J Pain Symptom Manage 2004;27:409–16. [DOI] [PubMed] [Google Scholar]
- [18].Toscani F, Gallucci M, Scaricabarozzi I. Nimesulide in the treatment of advanced cancer pain. Double-blind comparison with naproxen. Drugs 1993;156–8. [DOI] [PubMed] [Google Scholar]
- [19].Klaschik E, Clemens KE. Opioids for cancer pain treatment. Efficacy and side effects. Schmerz 2005;19:395–400. [DOI] [PubMed] [Google Scholar]
- [20].Wiffen PJ, Wee B, Derry S, et al. Opioids for cancer pain - an overview of Cochrane reviews. Cochrane Database Syst Rev 2017;7:CD012592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Deng G, Bao T, Mao JJ. Understanding the benefits of acupuncture treatment for cancer pain management. Oncology (Williston Park) 2018;32:310–6. [PubMed] [Google Scholar]
- [22].Paley CA, Johnson MI, Tashani OA, et al. Acupuncture for cancer pain in adults. Cochrane Database Syst Rev 2015;10:CD007753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Choi TY, Lee MS, Kim TH, et al. Acupuncture for the treatment of cancer pain: a systematic review of randomised clinical trials. Support Care Cancer 2012;20:1147–58. [DOI] [PubMed] [Google Scholar]
- [24].Lee H, Schmidt K, Ernst E. Acupuncture for the relief of cancer-related pain: a systematic review. Eur J Pain 2005;9:437–44. [DOI] [PubMed] [Google Scholar]
- [25].Peng H, Peng FD, Xu L, et al. Efficacy of acupuncture in treatment of cancer pain: a systematic review. Chin J Integr Med 2010;8:501–9. [DOI] [PubMed] [Google Scholar]
- [26].Yu D. The clinical study of acupuncture of analgesic effect on cancer pain. Chin Acupuncture Moxibusti 1998;1:17. [Google Scholar]
- [27].Farrar JT, Young JP, Jr, LaMoreaux L, et al. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain 2001;94:149–58. [DOI] [PubMed] [Google Scholar]
- [28].Nunes NA. The quality of life of Brazilian patients in palliative care: validation of the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire Core 15 PAL (EORTC QLQ-C15-PAL). Support Care Cancer 2014;22:1595–600. [DOI] [PubMed] [Google Scholar]
- [29].Sachsenheimer W, Piotrowski W, Bimmler T. Quality of life in patients with intracranial tumors on the basis of Karnofsky's performance status. J Neurooncol 1992;13:177–81. [DOI] [PubMed] [Google Scholar]
- [30].Lu W, Rosenthal DS. Acupuncture for cancer pain and related symptoms. Curr Pain Headache Rep 2013;17:321. [DOI] [PMC free article] [PubMed] [Google Scholar]


