Abstract
Background:
To conduct an economic evaluation of the clinic for Specialized Treatment Early in Psychosis (STEP), a Coordinated Specialty Care service (CSC) based in a U.S. State-funded community mental health center, relative to usual treatment (UT).
Methods:
Eligible patients were within 5 years of psychosis onset and had no more than 12 weeks of lifetime antipsychotic exposure. Participants were randomized to STEP or UT. The annual per-patient cost of the STEP intervention per se was estimated assuming a steady-state caseload of 30 patients. A cost-offset analysis was conducted to estimate the net value of STEP from a third-party payer perspective. Participant healthcare service utilization was evaluated at 6 months and over the entire 12 months post randomization. Generalized linear model multivariable regressions were used to estimate the effect of STEP on healthcare costs over time, and generate predicted mean costs, which were combined with the per-patient cost of STEP.
Results:
The annual per-patient cost of STEP was $1,984. STEP participants were significantly less likely to have any inpatient or ED visits; among individuals who did use such services in a given period, the associated costs were significantly lower for STEP participants at month 12. We did not observe a similar effect with regard to other healthcare services. The predicted average total costs were lower for STEP than UT, indicating a net benefit for STEP of $1,029 at month 6 and $2,991 at month 12; however, the differences were not statistically significant.
Conclusions:
Our findings are promising with regard to the value of STEP to third-party payers.
Keywords: cost-offset, early psychosis, coordinated specialty care
BACKGROUND
Schizophrenia spectrum disorders exert a large and disproportionate economic impact. In 2013, the total economic costs associated with schizophrenia in the U.S. were estimated to be $155.7 billion, about a quarter of which ($37.7 billion) were attributed to direct healthcare costs, while 72% were attributed to unemployment ($59.2 billion) and productivity losses resulting from caregiving ($52.9 billion).1 Other costs associated with schizophrenia include reduced workplace productivity, caregiver burden, increased use of criminal justice related resources, and premature mortality. This reflects the chronic and pervasive impact of psychotic illnesses, which usually manifest in early adulthood.
Early intervention services can interrupt this accumulating burden of suffering and disability, and deliver economic value. Specialized teams that deliver evidence-based treatments for ‘first episode psychosis’2 have demonstrated such an impact in diverse, international settings.3 Two recent U.S. randomized controlled trials have strengthened the argument for wider national deployment of such Coordinated Specialty Care services (CSC).4,5 However, longstanding constraints on mental healthcare spending place such innovations under fiscal scrutiny.6
Economic analyses of observational studies have supported investments in specialized team-based care for early psychosis.6-11 In addition, randomized trials in Denmark,12 England,13 and the U.S.14 have added compelling experimental support for the economic value of such programs. However, the models of care evaluated in these studies vary widely, as do the healthcare systems within which they were implemented. Consequently, questions remain regarding the economic viability of first-episode services in the fragmented U.S. healthcare system.
The clinic for Specialized Treatment Early in Psychosis (STEP) was established in 2006, to explicitly model a nationally-relevant U.S. public-sector early intervention service. 15 STEP’s clinical services were staffed and resourced by the Connecticut Mental Health Center (CMHC). This Center is a Public-Academic collaboration between Connecticut’s State Mental Health Agency or Authority (SMHA), the Department of Mental Health and Addiction Services, and Yale University’s School of Medicine. We have argued that the 50-state network of SMHAs, initially set up in the 1960s to reintegrate previously institutionalized populations,16 is a de facto national mental health system that can be leveraged towards early intervention.15 The objective of this study was to conduct an economic evaluation of the STEP program from a third-party payer perspective, alongside the recent randomized controlled trial testing the effectiveness of STEP relative to usual treatment (UT) in reducing hospitalizations and improving vocational functioning.5
METHODS
Design
A cost-offset analysis was conducted from a third-party payer perspective, according to established guidelines.17-19 The third-party payer perspective includes all formal (medical) costs incurred by the payer on behalf of participants meeting inclusion criteria in both arms. We determined, and valued, the resources required to manage the STEP program on a day-to-day basis. Other healthcare services utilized by participants were valued using a resource-costing method. The resource costing method entails determining a price weight for each type of resource unit consumed and multiplying the weights by the respective units of service.17,18 We modeled the person period for two 6-month periods following randomization, and conducted all analyses by intent-to-treat. The effect of STEP on healthcare costs over time was estimated using multivariable generalized linear model (GLM) regressions; predicted mean costs were then generated and used to calculate the net value of STEP to third-party payers. The net value was calculated as the difference between the average total cost associated with the STEP arm (including the per-participant cost of STEP), and the average total cost of the UT arm. An average total cost differential favoring STEP would be considered a net benefit for STEP. Finally, we evaluated the uncertainty around the net value point estimate.
Clinical trial overview
The trial used a pragmatic randomized controlled design20 to estimate the effectiveness of a first-episode service, STEP, versus UT. The pragmatic design allowed for a more generalizable sample of participants, and for the effectiveness of STEP to be tested in a community mental health center environment relative to usual treatment in this environment, using clinically relevant outcomes. The primary study outcome was hospital utilization, given that it accounts for 40% of direct healthcare costs associated with schizophrenia,1 and recent admissions are associated with subsequent clinical relapse.21 Vocational engagement and general functioning were secondary outcomes. U.S. Bureau of Labor Statistics’ categories were used to define: employed (in a full- or part-time job, in school, or filling parental or caregiver roles), unemployed (jobless, looking for a job, available for work, or in supported employment), and not in the labor force (any lack of capability to work or less than frequent attempts at finding work as measured by the Social Functioning Scale – SFS22).23 Those who were employed or unemployed and thus avoided dropping out of the labor force were considered vocationally engaged.
STEP is based in the Connecticut Mental Health Center (CMHC), which is the lead agency for all public-sector eligible patients in the greater New Haven region. STEP was permitted to sample beyond this population (i.e., to accept patients with commercial insurance, under the age of 18, or living outside the Center’s catchment). Thus, all individuals between the ages of 16-45 with a recent onset psychotic illness (i.e., operationally defined as less than 12 weeks of antipsychotic treatment) were offered study enrollment. These broad eligibility criteria resulted in an ecological sample of 117 consenting subjects after random allocation to STEP or referral to care in the community (UT).
STEP includes a tailored approach to treating early psychosis in that patients are allowed to choose among psychotropic medications, family education, cognitive-behavioral therapy (CBT), and case management focused on collaboration with other service providers at the mental health center where STEP is located to provide employment support, or local colleges for educational support. STEP’s model of CSC has been detailed elsewhere.5 Relevant to this analysis, clinicians and psychiatrists were reallocated part-time from CMHC’s ambulatory services. Clinicians were drawn from the disciplines of nursing and social work, and psychology and psychiatry training programs. Weekly team meetings, led by a psychiatrist or senior clinician, emphasized integration and continued tailoring of care components in response to evolving patient and family needs. STEP care included standard (routinely offered at CMHC and received by UT patients) and specialized components (implemented specifically for this CSC): besides the team meetings described above, these included a Cognitive-Behavioral Therapy (CBT) based group for patients24 and family education (provided both in individual family meetings and to groups of families).25 CBT sessions occurred once per week and consisted of 10 participants/session. The family education component consisted of approximately 3 individual sessions, and 24 group sessions (10 participants/group) over the course of 12 months. Research psychologists developed manuals for both treatments and supervised the primary clinicians who initially served as co-therapists and then assumed full leadership. After 12 months of observation, post-randomization, STEP participants experienced fewer hospital inpatient visits (0.33 versus 0.68, p=0.02), better vocational engagement (91.7% versus 66.7%, p<0.01), and positive trends with regard to general functioning according to several measures.5
STEP costs
Specialized psychosocial services provided by STEP (CBT and family education) frequently occurred in group settings, involved multiple clinicians and were staffed regardless of patient attendance. Multidisciplinary team meetings were held weekly regardless of census. We were unable to capture the number of sessions attended by each participant over the course of the trial, therefore, we calculated per-participant costs associated with STEP according to the estimated cost of operating the program on an annual basis, assuming a steady-state caseload of 30 patients. After discussions with providers, we decided to inflate the staff time in STEP care delivery by 30% to account for staff activities required for STEP that occurred outside of direct patient care, such as documentation, case discussion, and ongoing training. Unit costs for clinical providers were derived from 2015 nationally-representative hourly wage estimates from the Bureau of Labor Statistics.26 We added fringe (30%) and Facilities and Administrative (10%) costs to the calculated total clinician time costs by sampling from values typical for public Community Mental Health Centers.
Healthcare service utilization costs
Per-person costs were calculated by multiplying units of healthcare service utilization (e.g., ED visits) by their respective price weight and summing the relevant values for each resource category. Inpatient and emergency department (ED) service use data were obtained from billing records of the Yale New Haven Hospital system, the dominant provider of such services in the region. This resulted in comprehensive and near complete data for all domains of hospital-based care. The Services Utilization and Resources Form27 was used to query patients and caregivers about non hospital-based healthcare service utilization across four domains: medical, surgical, psychiatric and substance use disorder specialty services. Unit costs for all services were obtained from published reports,14,27 and adjusted to 2015 U.S. dollars using the Consumer Price Index.28 The Services Utilization and Resources Form was administered at 6 and 12 months post-randomization (Bureau of Labor Statistics, 2017).
Analysis
Multivariable generalized linear regression models (GLMs) with clustered standard errors were used to estimate the effect of STEP on healthcare costs over time. Multivariable analyses are recommended for economic evaluations conducted alongside clinical trials in order to control for potentially confounding factors that were not balanced by randomization, or became unbalanced due to loss to follow-up, and because they allow for the incorporation of robust missing data techniques.17 The GLM allows one to choose the most appropriate mean and variance functions according to the fit of the data, which is especially important when analyzing healthcare service utilization data, as it is censored at zero and typically has a heavy tail. Due to the different data generating mechanisms, two separate GLM regressions were performed, one for the inpatient and ED data, and one for the self-reported data from the Services Utilization and Resources Form. The modified Parks test was used to guide the choice for the variance function (i.e., family), while the Pregibon link, the Modified Hosmer and Lemeshow, and the Pearson’s correlation tests were used to help choose the most appropriate mean function (i.e., link).17 Due to the overdispersion of zeros in the data, two-stage GLM regressions were used. In both instances, the tests indicated that a gamma distribution with a log link would be most appropriate.
Because observed inpatient and ED service use were obtained from electronic health records, missing data were not an issue. Of the four healthcare service domains queried by the Services Utilization and Resources Form,27 respondents only reported using outpatient services provided by: psychiatrists, other mental health clinicians, physicians, and nurses (Appendix Table 1). Furthermore, 36% of self-report data was missing at 6 months and 37% was missing at 12 months. The data appear to be missing at random, based on Little’s missing completely at random test and the fact that the missingness is well explained by other variables in the model;29 therefore, inverse probability weighting within the GLM framework was used to address the missingness. Inverse probability weighting has been shown to perform well in terms of addressing missing-data bias when data are missing at random.30
The aforementioned multivariable regressions, and the statistical method of recycled predictions were used to generate the predicted mean values for each resource category, by arm and time period.17 Predicted mean values of a dependent variable that has been transformed (e.g., logarithmically) will be biased if covariate imbalances have not been accounted for in the retransformation; the recycled predictions method avoids such bias.17 The predicted mean values, and the per-patient cost of STEP were then summed to generate total mean costs for each arm at 6 months and over the entire 12 months post randomization. To account for sampling uncertainty, standard errors for the predicted mean values were estimated by performing the analyses within a non-parametric bootstrap, which were then used to calculate p-values.17 The difference in the total mean costs represents the net value of STEP relative to UT. A negative value indicates that STEP is less costly, on average, and therefore would be considered a net benefit.
RESULTS
Table 1 contains baseline participant characteristics relevant to the economic evaluation, by arm. The annual per-patient direct cost of STEP was $1,984 (Table 2). The results from the two-stage GLM regression on inpatient and ED service utilization indicate that STEP participants were significantly less likely to incur any costs for inpatient or ED visits compared to participants assigned to UT (Appendix Table 2). Among individuals who did use inpatient or ED services, the associated costs were significantly lower for STEP participants at month 12, as well as for females, and participants who identified themselves as white or black.
Table 1:
Baseline characteristics of patients randomly assigned to STEP or to usual treatment - adapted from Srihari, Tek, Kucukgoncu, Phutane, Breitborde, Pollard, Ozkan, Saksa, Walsh, Woods 5
| Total | STEPa | TAU | ||||
|---|---|---|---|---|---|---|
| N | N | % | N | N | % | |
| Socio-demographic characteristics | ||||||
| Age (M±SD) | 60 | 22.4±4.5 | 57 | 22.6 ±5.3 | ||
| Men | 60 | 49 | 82 | 57 | 46 | 81 |
| Ethnicity | ||||||
| Black | 60 | 22 | 37 | 57 | 19 | 33 |
| Hispanic | 60 | 7 | 12 | 57 | 10 | 18 |
| Caucasian | 60 | 27 | 45 | 57 | 26 | 46 |
| Other | 60 | 4 | 6 | 57 | 1 | 2 |
| Years of education (M±SD) | 60 | 12.76±2 | 12.68±2 | |||
| Hospital & ED costs, 6mos prior to enrollment (M±SD) | 60 | $8,824±7,803 | 57 | $11,061±11,289 | ||
| General functioning | ||||||
| GAF (M±SD) | 60 | 36.22 ±12.89 | 57 | 34.42±10.43 | ||
| SFS Global Score (M±SD) | 60 | 114.37±22.15 | 57 | 125.05±26.35 | ||
| Vocational status | ||||||
| Vocationally engaged | 60 | 41 | 68.3 | 54 | 36 | 66.7 |
| Employed/In school | 60 | 32 | 53.3 | 54 | 33 | 61.1 |
| Unemployed, looking for job | 60 | 9 | 15 | 54 | 3 | 5.6 |
| Not in the Labor Force | 60 | 19 | 31.7 | 54 | 18 | 33.3 |
| Clinical Status | ||||||
| DUP in months (M±SD) | 52 | 10.0±16.0 | 47 | 10.0±13.0 | ||
| Schizophrenia or Schizoaffective disorder | 57 | 15 | 26 | 57 | 18 | 32 |
| Co-morbidity | ||||||
| Substance use disorder | 57 | 26 | 46 | 59 | 25 | 45 |
| Anxiety disorder | 51 | 6 | 12 | 38 | 4 | 11 |
| PANSSc | ||||||
| Positive dimension (M±SD) | 60 | 20.75±6.74 | 57 | 19.60±5.90 | ||
| Negative dimension (M±SD) | 60 | 17.82±6.42 | 57 | 17.01±5.40 | ||
| General symptoms (M±SD) | 60 | 33.42±8.62 | 57 | 33.70±8.56 | ||
| Total (M±SD) | 60 | 72.0±16.76 | 57 | 70.33±15.52 | ||
Notes: No statistically significant differences were found between STEP and UT.
STEP, Specialized Treatment Early in Psychosis.
GAF, Global Assessment of Functioning (Possible scores range from 1 to 100, with higher score indicating superior functioning in a range of activities); SFS, Social Functioning Scale (Possible scores on the SFS (Social Functioning Scale) range from 8 to 198, with higher score indicating better social functioning.); DUP, duration of untreated psychosis.
PANSS, Positive and Negative Syndrome Scale (Possible scores for general symptoms range from 16 to 112, with higher scores indicating worse general psychopathology. Possible total scores range from 30 to 210, with higher score indicating worse overall symptomatology).
Table 2:
Annual costs of specialized psychosocial services of STEP
| Specialized service | Total sessions required to treat 30 patients |
Total annual costs | Per-patient cost |
|---|---|---|---|
| Weekly multidisciplinary rounds | 52 | 52 sessions × 1 hour × [$22.70 (social worker) + $34.10 (RN) + $36.60 (Psychologist) + $93.10 (Psychiatrist)] = $9,698 | $323 |
| CBT groups | 3 groups × 52 sessions = 156 | 156 sessions × 1 hour × [$28.40 (clinician)a + $36.60 (psychologist)] = $10,140 | $ 338 |
| Family education - individual | 90 | 90 sessions × 1 hour × $36.60 (psychologist) = $3,294 | $110 |
| Family education – group | 3 groups × 24 sessions = 72 | 72 sessions × 1.5 hours × [$28.40 (clinician)a + $36.60 (psychologist)] = $7,020 | $234 |
| Supervision | 52 | 52 sessions × $36.60 (psychologist) = $1,903 | $63 |
| Direct patient care, total | Sum of all staff time spent in delivering specialized services to STEP patients | $1,068 | |
| Activities outside direct patient care (e.g., case review, consultation) | Assumed to be 30% of staff time in direct patient care = $1,068*30% | $320 | |
| Total wage costs | $1,068 + $320 | $1,388 | |
| Total wage + fringe (30%) | $1,388 × (1+30%) | $1,804 | |
| Total wage + fringe + Facilities and Administrative costs (10%) | $1,804 × (1+10%) | $1,984 | |
Notes: CBT – Cognitive behavioral therapy
Clinician time is based on study documentation.
Clinician wage rates are based on the May 2015 National Occupational Employment and Wage Estimates from the Bureau of Labor Statistics (https://www.bls.gov/oes/current/oes_nat.htm). Specifically, the hourly wage rates we used in our calculation are: psychiatrists - $93.10, registered nurses - $34.14, mental health and substance abuse social workers - $22.70, clinical, counseling and school psychologists – $36.60.
This role was shared by a social worker and an RN; average wage rate of these two professions is used to calculate cost of clinician time
The results from the two-stage GLM regression on self-reported healthcare service utilization other than inpatient and ED services (i.e., visits reported via the Services Utilization and Resources Form – psychiatrists, other mental health clinicians, physicians, and nurses) indicate that STEP was not a statistically significant determinant of whether or not participants received these “other” healthcare services, nor was it associated with the cost of those services among individuals who did receive them (Appendix Table 3). Participants with a high school diploma were slightly more likely to use other healthcare services, and among those who did use services, females incurred significantly fewer costs than males.
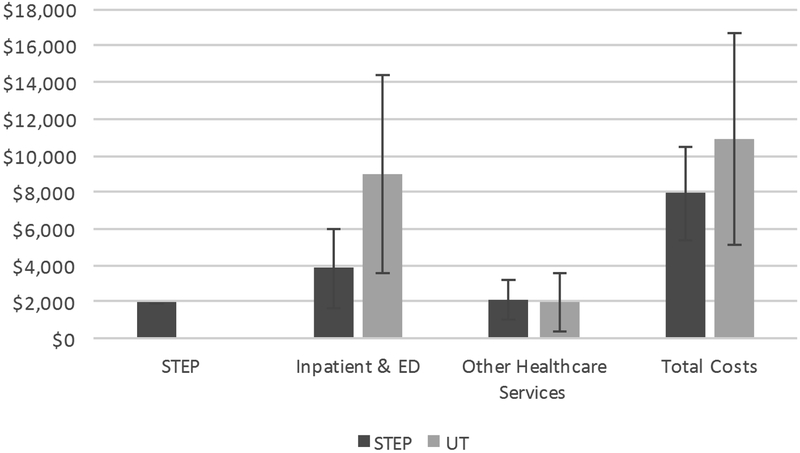
The predicted mean cost and net value of STEP at months 6 and 12 are presented in Table 3. At 6 months following randomization, the predicted mean costs for both inpatient and ED utilization, and other healthcare service utilization are lower for STEP than UT. Even after adding in the estimated per-participant cost of STEP, there is a mean net benefit of $1,029 for STEP. However, none of the cost differentials are statistically significant. At 12 months, the mean cost for inpatient and ED use remains lower for STEP than UT, while the average cost associated with other healthcare service use is slightly higher for UT (Table 3 and Figure 1). Summing these figures and the per-participant cost for STEP results in a $2,991 net benefit for STEP. However, once again, none of the cost differentials are statistically significant.
Table 3:
Predicted Mean Costs (per patient)
| 6-Months | 12-Months | |||||||
|---|---|---|---|---|---|---|---|---|
| Variable | STEP | UT | Diff (SE) | P-value | XRNTX | UT | Diff (SE) | P-value |
| Costs | ||||||||
| STEPa | $992 | 0 | $992 | $1,984 | 0 | $1,984 | ||
| Inpatient & Emergency Department |
$2,771 | $4,576 | −$1,805 (2,860) | 0.53 | $3,870 | $8,942 | −$5,072 (4,719) | 0.28 |
| Other Healthcare Services | $838 | $1,054 | −$216 (440) | 0.62 | $2,084 | $1,987 | $97 (907) | 0.92 |
| Total Costs | $4,601 | $5,630 | −$1,029 (2,938)a | 0.73 | $7,938 | $10,929 | −$2,991 (4,958)a | 0.55 |
The services valued as part of STEP represent those offered in addition to Usual Treatment (UT).
The difference in average total costs between the two arms represents the net value. A negative value indicates that STEP is less costly, on average, and thus represents a net benefit.
Figure 1.
: 12-Month Costs
Note: Error bars represent standard errors. The services valued as part of STEP represent those offered in addition to Usual Treatment (UT). ED = Emergency Department.
DISCUSSION
Our results indicate that STEP participants were significantly less likely to incur inpatient and ED costs over the course of the study, and among those who did, the costs decreased over time. This is a promising finding, as psychiatric hospitalizations are the single largest driver of direct healthcare and non-healthcare costs for schizophrenia in the U.S.,1 and may serve as a proxy for patient well-being since recent hospital admissions have been associated with subsequent clinical relapse.21 We did not observe a similar effect with regard to other healthcare services. Although the predicted average total costs were lower for STEP than UT, even after accounting for the per-patient cost of the intervention, the differences did not achieve statistical significance. This finding is similar to those of prior clinical trials that did not find statistically significant cost savings associated with first-episode psychosis interventions.12-14
The pragmatic randomized design, which limited selection bias while allowing ecologically relevant sampling, is a strength of this analysis; there are also several limitations. We do not have data on STEP services received by individual participants due to the lack of a reliable, centralized service tracking system. Thus, we estimated the per-patient intervention cost based on the assumption that the provider would be able to maintain a patient cohort of 30. The cohort size of 30 was based on STEP’s census over the study period and the guidelines of the Recovery After an Initial Schizophrenia Episode (RAISE) Implementation and Evaluation Study.31 Our sample size may limit our ability to detect significant differences among less frequent types of healthcare service utilization; however, we argue that the results from the economic evaluation remain important and informative, because a) we are estimating the economic impact of the intervention, as opposed to testing a specific hypothesis; b) we calculate and report the uncertainty around the point estimates; and c) nonparametric bootstrapping techniques were used to estimate the standard errors and p-values, which increases the robustness of estimates derived from data that are non-normal and asymmetrical, as is often case with small sample sizes. We were unable to calculate quality-adjusted life-years; therefore, our economic evaluation is limited to exploring direct healthcare cost offsets associated with STEP relative to UT. Missing data among self-reported healthcare service utilization data is a limitation; however, we used an established statistical technique shown to control for missing-variable bias when data are missing at random, which these appear to be.30 Although inpatient and ED service utilization data were obtained from the dominant provider in the area, we cannot be certain that related care was not received elsewhere. Given the chronic nature of psychosis, the 12-month observation period is also a limitation, and likely undervalues the benefit of STEP.
Similarly, although vocational engagement and involvement with the criminal justice system were measured, they were not done in a manner conducive to an economic evaluation conducted from a societal perspective. This is a significant limitation, as a number of the benefits associated with early psychosis intervention programs have ramifications for society; thus, only viewing the economic value from a healthcare sector perspective likely undervalues the true benefit to society. As reported by Srihari et al.,5 STEP participants were more likely to be vocationally engaged. Given that the absence of afflicted individuals from the labor market is a significant driver of the long-term economic burden of psychotic illnesses, small vocational gains in these younger samples can be expected to result in disproportionate benefits that accrue over time.1,32,33 Similarly, even limited involvement with the criminal justice system in early adulthood can cause persistent distortions of social and vocational trajectories.34 Moreover, in addition to the direct costs incurred by the criminal justice system, criminal activity is associated with many tangible and intangible costs to society, such as property damage, and pain and suffering of victims.35
CONCLUSIONS
Overall, our findings are promising with regard to the economic value of STEP to third-party payers, and extend a growing international literature supporting the economic viability of specialized team-based care for early psychosis.
Supplementary Material
Acknowledgments and Disclosures:
This work was supported by grants to Dr. Srihari, principal investigator, from the Patrick and Catherine Weldon Donaghue Medical Research Foundation (DF07-014) and the National Institutes of Health (MH088971). The trial is registered at ClinicalTrials.gov (NCT00309452). The views expressed here are those of the authors, and not necessarily those of the National Institute of Mental Health, the National Institutes of Health, or the federal government. This work was funded in part by the State of Connecticut, Department of Mental Health and Addiction Services, but this publication does not express the views of the Department of Mental Health and Addiction Services or the State of Connecticut. The views and opinions expressed are those of the authors.
Footnotes
Conflicts of Interest: The authors declare no competing interests.
Trial registration: www.ClinicalTrials.gov: NCT00309452.
REFERENCES
- 1.Cloutier M, Aigbogun MS, Guerin A, et al. The economic burden of schizophrenia in the United States in 2013. J Clin Psychiatry. 2016;77(6):764–771. [DOI] [PubMed] [Google Scholar]
- 2.Breitborde NJ, Srihari VH, Woods SW. Review of the operational definition for first‐episode psychosis. Early intervention in psychiatry. 2009;3(4):259–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Srihari VH, Shah J, Keshavan MS. Is early intervention for psychosis feasible and effective? Psychiat Clin N Am. 2012;35(3):613–631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kane JM, Robinson DG, Schooler NR, et al. Comprehensive versus usual community care for first-episode psychosis: 2-year outcomes from the NIMH RAISE early treatment program. American Journal of Psychiatry. 2015;173(4):362–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Srihari VH, Tek C, Kucukgoncu S, et al. First-episode services for psychotic disorders in the US public sector: a pragmatic randomized controlled trial. Psychiat Serv. 2015;66(7):705–712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Andrew A, Knapp M, McCrone PR, Parsonage M, Trachtenberg M. Effective interventions in schizophrenia: the economic case. 2012. [Google Scholar]
- 7.Liffick E, Mehdiyoun NF, Vohs JL, Francis MM, Breier A. Utilization and Cost of Health Care Services During the First Episode of Psychosis. Psychiat Serv. 2016;68(2):131–136. [DOI] [PubMed] [Google Scholar]
- 8.Tsiachristas A, Thomas T, Leal J, Lennox BR. Economic impact of early intervention in psychosis services: results from a longitudinal retrospective controlled study in England. BMJ Open. 2016;6(10):e012611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Behan C, Cullinan J, Kennelly B, et al. Estimating the cost and effect of early intervention on in-patient admission in first episode psychosis. The journal of mental health policy and economics. 2015;18:57–61. [PubMed] [Google Scholar]
- 10.Mihalopoulos C, McGorry P, Carter R. Is phase‐specific, community‐oriented treatment of early psychosis‐an economically viable method of improving outcome? Acta Psychiat Scand. 1999;100(1):47–55. [DOI] [PubMed] [Google Scholar]
- 11.Mihalopoulos C, Harris M, Henry L, Harrigan S, McGorry P. Is early intervention in psychosis cost-effective over the long term? Schizophrenia Bull. 2009;35(5):909–918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hastrup LH, Kronborg C, Bertelsen M, et al. Cost-effectiveness of early intervention in first-episode psychosis: economic evaluation of a randomised controlled trial (the OPUS study). The British Journal of Psychiatry. 2013;202(1):35–41. [DOI] [PubMed] [Google Scholar]
- 13.McCrone P, Craig TK, Power P, Garety PA. Cost-effectiveness of an early intervention service for people with psychosis. The British Journal of Psychiatry. 2010;196(5):377–382. [DOI] [PubMed] [Google Scholar]
- 14.Rosenheck R, Leslie D, Sint K, et al. Cost-effectiveness of comprehensive, integrated care for first episode psychosis in the NIMH RAISE early treatment program. Schizophrenia Bull. 2016;42(4):896–906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Srihari VH, Breitborde NJ, Pollard J, et al. Public-academic partnerships: early intervention for psychotic disorders in a community mental health center. Psychiat Serv. 2009;60(11):1426–1428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Frank RG. Better but not well: Mental health policy in the United States since 1950. JHU Press; 2006. [Google Scholar]
- 17.Glick HA, Doshi JA, Sonnad SS, Polsky D. Economic Evaluation in Clinical Trials. Oxford University Press; 2014. [Google Scholar]
- 18.Neumann PJ, Sanders GD, Russell LB, Siegel JE, Ganiats TG. Cost-Effectiveness in Health and Medicine. 2nd ed. New York, NY: Oxford University Press; 2017. [Google Scholar]
- 19.Drummond MF, Schulpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the Economic Evaluation of Health Care Programmes. Fourth ed: Oxford university press; 2015. [Google Scholar]
- 20.Hotopf M, Churchill R, Lewis G. Pragmatic randomised controlled trials in psychiatry. The British Journal of Psychiatry. 1999;175(3):217–223. [DOI] [PubMed] [Google Scholar]
- 21.Almond S, Knapp M, Francois C, Toumi M, Brugha T. Relapse in schizophrenia: costs, clinical outcomes and quality of life. The British Journal of Psychiatry. 2004;184(4):346–351. [DOI] [PubMed] [Google Scholar]
- 22.Birchwood M, Smith J, Cochrane R, Wetton S, Copestake S. The Social Functioning Scale. The development and validation of a new scale of social adjustment for use in family intervention programmes with schizophrenic patients. Brit J Psychiatry. 1990;157(6):853–859. [DOI] [PubMed] [Google Scholar]
- 23.Bureau of Labor Statistics. How the Government Measures Unemployment. 2015; https://www.bls.gov/cps/cps_htgm.htm. Accessed 01/08/2018.
- 24.Saksa JR, Cohen SJ, Srihari VH, Woods SW. Cognitive behavior therapy for early psychosis: A comprehensive review of individual vs. group treatment studies. International journal of group psychotherapy. 2009;59(3):357–383. [DOI] [PubMed] [Google Scholar]
- 25.Breitborde NJ, Srihari VH. Family work for first-episode psychosis: A service delivery protocol In: Psychosis: Causes, diagnosis and treatment. Nova Science Publishers, Inc; 2012. [Google Scholar]
- 26.Bureau of Labor Statistics. Occupational Outlook Handbook. 2017; http://www.bls.gov/ooh/home.htm.
- 27.Rosenheck RA, Leslie DL, Sindelar J, et al. Cost-effectiveness of second-generation antipsychotics and perphenazine in a randomized trial of treatment for chronic schizophrenia. American Journal of Psychiatry. 2006;163(12):2080–2089. [DOI] [PubMed] [Google Scholar]
- 28.U.S. Department of Labor Bureau of Labor Statistics - Consumer Price Index. http://www.bls.gov/cpi/. Accessed 12/18/18.
- 29.Little RJ, Rubin DB. Statistical analysis with missing data. John Wiley & Sons; 2014. [Google Scholar]
- 30.Seaman SR, White IR. Review of inverse probability weighting for dealing with missing data. Statistical Methods in Medical Research. 2013;22(3):278–295. [DOI] [PubMed] [Google Scholar]
- 31.Bennett M, Piscitelli S, Goldman H, Essock S, Dixon L. Coordinated Specialty Care for First Episode Psychosis Manual II: Implementation. National Institute of Mental Health;2014. [Google Scholar]
- 32.Esch P, Bocquet V, Pull C, et al. The downward spiral of mental disorders and educational attainment: a systematic review on early school leaving. BMC psychiatry. 2014;14(1):237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kessler RC, Foster CL, Saunders WB, Stang PE. Social consequences of psychiatric disorders, I: Educational attainment. Am J Psychiatry. 1995;152(7):1026. [DOI] [PubMed] [Google Scholar]
- 34.Travis J, Western B, Redburn FS. The growth of incarceration in the United States: Exploring causes and consequences. 2014. [Google Scholar]
- 35.McCollister KE, French MT, Fang H. The cost of crime to society: new crime-specific estimates for policy and program evaluation. Drug Alcohol Depen. 2010;108(1-2):98–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.