Abstract
OBJECTIVE:
Suicide is a major public health problem and the 10th leading cause of death in the United States. The identification of modifiable risk factors is essential for reducing the prevalence of suicide. Recently, it has been shown that insomnia and nightmares significantly increase the risk for suicidal ideation, attempted suicide, and death by suicide. While both forms of sleep disturbance may independently confer risk, and potentially be modifiable risk factors, it is also possible that simply being awake at night represents a specific vulnerability for suicide. The present analysis evaluates the frequency of completed suicide per hour while taking into account the percent of individuals awake at each hour.
METHODS:
Archival analyses were conducted estimating the time of fatal injury using the National Violent Death Reporting System (NVDRS) and the proportion of the American population awake per hour across the 24 hour day using the American Time Use Survey (ATUS). The initial evaluation of the data took place from September 2013 to December 2014.
RESULTS:
The mean incident rate from 06:00-23:59 was 2.2% +/−0.7%, while the mean incident rate from 24:00-05:59 was 10.3% +/− 4.9%. The maximum incident rate was at 2:00-2:59 (16.3%). Hour-by-hour observed values differed from those that would be expected by chance (p<0.001), and when 6-hour blocks were examined, the observed frequency at night was 3.6 times higher than would be expected by chance (p<0.001).
CONCLUSIONS:
Being awake at night confers greater risk for suicide than being awake at other times of the day, suggesting disturbances of sleep or circadian neurobiology may potentiate suicide risk.
INTRODUCTION
Suicide occurs in both men and women, in most age groups, and in all socioeconomic groups and races1. The population trends suggest that completed suicide occurs most often in Non-Hispanic White men and among those aged 45-64, with an annual population prevalence of approximately 12 per 100,000 individuals1. The effort to understand why people die by suicide, and why so many others attempt suicide, requires the identification of risk factors that are associated with such behaviors. Recently, sleep disturbance has been identified as an indicator of risk for suicidal ideation, suicide attempts, and suicide. To date, there have been at least 40 studies that have evaluated the association of sleep disturbance and suicide(e.g., 2-12). Pigeon et al.5 recently conducted a meta-analysis of these studies and found that sleep disturbance was associated with an overall increased risk across suicide outcomes (RR=2.79, 95% CI=2.44-3.19). Insomnia, nightmares, and “other sleep disturbances” were found to have comparable risk ratios, overall (2.84, 2.61, and 2.72 respectively). Several recent epidemiologic studies add to the existing evidence base by providing information about how the specific subtypes of insomnia and sleep duration are associated with suicide. For example, Wojnar et al.11 found that difficulty initiating sleep and difficulty maintaining sleep predicted suicidal ideation and planning, and difficulty maintaining sleep was associated with suicide attempts. Short sleep duration, while not an insomnia subtype per se, has also been found to be associated with suicidal ideation across several studies(e.g., 13).
It is possible that the association between sleep disturbance and suicide can be explained by factors independent of sleep. For example, variance accounted for by sleep disturbance may simply represent the effects of physiological, psychological, and/or social stressors that may not otherwise be adequately captured5. Yet another possibility is that sleep disturbance results in being awake at night, and it is the fact of being awake at night itself that confers risk. If this is the case, it would be expected that the incidence of suicide attempts and/or completed suicides should be elevated at night (during the circadian phase for sleep). To date, eight studies14-21 have investigated the temporal patterning of suicide across the 24 hour day and found that the peak frequency for completed suicide occurs during the day. Although seminal, the above studies did not adjust for the proportion of the population awake at each time interval. Since suicide represents an intentional behavior that can only be performed when awake, the population that is at risk of suicide varies by time of day. The present analysis evaluates the incidence of suicide by clock time while accounting for the proportion of the population that is likely awake at each given hour. The hypothesis for the present analysis is that, after accounting for the proportion of the population likely to be awake, suicide disproportionately occurs at night.
METHODS
Data Source
Two databases were used to evaluate the study hypothesis. The National Violent Death Reporting System (NVDRS, www.cdc.gov/violenceprevention/nvdrs/)22 was used to investigate deaths by suicide by clock hour. The American Time Use Survey (ATUS, www.bls.gov/tus/data.htm)23 was used to assess the proportion of the population that is awake by clock hour. Both databases are available to public access. The archival analysis project conducted here was reviewed by the University of Pennsylvania’s Internal Review Board (IRB 815690).
The NVDRS dataset, compiled by the Centers for Disease Control and Prevention (CDC), includes details on violent deaths from 18 participating US states22. The data for the present study included the years 2003-2010. The four major sources of data include death certificates, reports from the coroner and/or medical examiner, reports from law enforcement agencies, and reports from crime laboratories. For the present analyses, all the available data regarding estimated time of fatal injury data were obtained from the database, regardless of method or situational factors. In addition to estimated time of fatal injury, several other variables were extracted from the NVDRS database including: estimated time of fatal injury, age, sex, race/ethnicity (Non-Hispanic White, Black/African-American, Hispanic/Latino, Asian, and Other), and mood status (“current depressed mood”)22. Estimated time of fatal injury was binned in 1-hour segments (0:00-0:59, 1:00-1:59, 2:00-2:59, etc.) and also arrayed in six hour bins categorized as “night” (0:00-5:59), “morning” (6:00-11:59), “afternoon” (12:00-17:59), and “evening” (18:00-23:59). Age was categorized by 10-year groupings (15-24, 25-34, 35-44, 45-54, 55-64, 65-74, and ≥75).
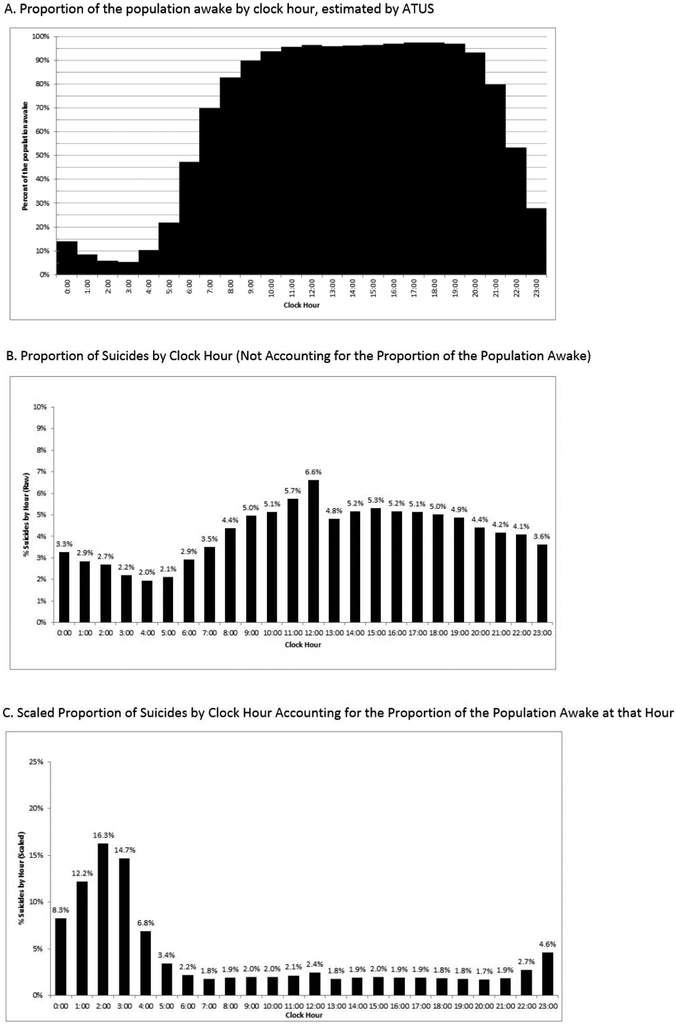
The ATUS is a database maintained by the US Bureau of Labor Statistics (BLS) and is an annual survey that assesses a range of activities across the 24-hour day in a representative sample of Americans23. The survey is conducted by phone and requires respondents to retrospectively profile their activities hour by hour for the last 24 hours. Responses are coded into standardized categories. The primary variable of interest was the report of “sleep.” Percent of the population asleep per hour is represented in Figure 1, panel A. Additional data were also gathered on age, sex, and race/ethnicity. The data for the present analysis were acquired from 2003-2011, and represent population-weighted values for the weekdays (vs. weekends). In supplementary analyses stratified by age, sex, and race/ethnicity, weighted population estimates were separately computed for each category.
Figure 1.
Proportion of the Population Awake and Completed Suicides by Clock Hour
Conceptual Approach
If an analysis aims to discern the temporal patterning of a behavior by hour over the 24-hour day, it follows that: (1) the null hypothesis would be that time1=time2=time3 and so on (i.e., the behavior of interest occurs with similar frequency across all time intervals) and (2) a significant finding would entail the observation that one or more time points would be associated with more or less occurrences of the behavior than expected based on the null hypothesis. In both cases, the underlying assumption is that there is an equal probability of the suicidal behavior occurring across all time intervals. This is not, however, likely to be the case. Since the behavior of interest is volitional and requires wakefulness, the calculation must take into account the probability of being awake across the 24-hour day. Put differently, the question may be better phrased as, “How common is suicide at each hour of the day, given how many people tend to be awake at that hour?” Asked and operationalized in this manner, it may be possible to observe an effect that has been previously masked: That suicide occurs disproportionately at night.
For example, a data set of 100 individuals who perform a behavior is collected, and the cumulative occurrences of the behavior are arrayed by hour for each hour of the 24-hour day. Assuming equal probability of performing the behavior for each hour (e.g., 100/24 = 4.17 per hour), if it is observed that 10 individuals performed the behavior at 13:00 (1pm) and 2 individuals performed the behavior and at 1:00 (1am), then it would be concluded that the behavior occurred disproportionately more frequently higher at 1pm (10 vs. 2). If, however, approximately 95% of the population is awake at 1pm and only 10% of the population is awake at 1am, and if the behavior estimates were weighted to take this into account, then the adjusted incidents would be 10.5% at 1pm and 20% at 1am (10/[100*0.95] and 2/[100*0.10]). Assessed in this manner, it would be concluded that behavior occurred disproportionately at 1:00am. This approach was used for the present study.
Statistical Analyses
Time of fatal injury was categorized by hour (24 bins, one hour per bin) or by general time of day (4 bins, 6 hours per bin). The proportion of the population awake by hour was determined using ATUS. These proportions were used to compute the expected number of suicides per hour to compare to observed values. These computations resulted in raw and adjusted percentages of suicides by clock hour, relative to the complete sample, as well as relative to the proportion of the population awake at each hour. In addition, these computations resulted in observed and expected frequencies for each clock hour.
Based on these values, the null hypothesis that time1=time2=time3 etc. was tested (taking into account appropriate weighting) using a chi square goodness-of-fit test. This test served as an omnibus evaluation of whether there are differences in the observed versus expected percentages across clock hours. A significant result would indicate that at least 1 hour was different from the rest. To evaluate the degree to which the prevalence at each hour deviated from what would be expected, a series of standardized incidence ratios (SIRs) were computed by dividing the number of observed suicides per hour by the number of suicides expected based on ATUS estimates. By taking this approach, a 95% confidence interval around the SIR was obtained. Because of the large sample size and high statistical power for detecting very small effects, a phi statistic was calculated to estimate effect size. Phi is roughly equivalent to the commonly-used Cohen’s d statistic, modified for use with chi square. Phi is calculated by taking the square root of the result of dividing the chi square statistic by the sample size. As with Cohen’s d, typical rules of thumb suggest that effects of 0.2 are small, effects of 0.5 are medium, and effects of 0.8 are large. Post-hoc hour-by-hour pairwise comparisons were not performed. A similar process was followed to obtain weighted percentages and both observed and expected values for the 4 time of day categories. Similarly, chi-square goodness of fit tests were used to detect whether there were differences among the times of day and phi statistics were computed to estimate effect size. Finally, post-hoc pairwise tests compared night-morning, night-afternoon, night-evening, morning-afternoon, morning-evening, and afternoon-evening periods. To evaluate whether this pattern was consistent across demographic groups, this analytic approach was repeated in analyses stratified by sex, race/ethnicity, and 10-year age groups. Separate ATUS values were extracted for each group. Also, separate analyses were performed for individuals with or without known depression (collected by NVDRS), using the overall sample values from ATUS.
RESULTS
Characteristics of the Overall Sample (Unadjusted Data).
A total of n=35,332 records out of the 71,282 documented suicides had time of fatal injury data and were included in analyses. The first evaluation was undertaken without any adjustment for the proportion of the population that is likely awake at each given hour. As can be seen in Table 1, the two subsets of data (records with and without time of fatal injury) did not differ with respect to demographics, education, or mood status (depression). In the unadjusted data (see Table 2, Column 7 and Figure 1, Panel B.), the majority of suicides were committed during the day with a peak frequency at noon (6.6%) and a trough frequency at 4am (2.0%). The overall distribution was roughly sinusoidal with suicide at night (midnight to 6am) occurring in 18.1% of the sample.
Table 1.
Characteristics of the Overall Sample
| Time of Fatal Injury Data | |||
|---|---|---|---|
| Variable | Category | No | Yes |
| N | 35998 | 35284 | |
| Age | 46.029 ± 16.940 | 45.359 ± 18.280 | |
| Sex | Female | 24.77% | 18.76% |
| Race/Ethnicity | White | 86.47% | 84.26% |
| Black/African-American | 5.80% | 7.56% | |
| Hispanic/Latino | 4.06% | 4.57% | |
| Asian/Pacific Islander | 1.85% | 1.47% | |
| Native American | 1.56% | 1.91% | |
| Other | 0.27% | 0.24% | |
| Education | Less than High School | 20.86% | 27.18% |
| High School | 39.64% | 39.53% | |
| Some College | 15.63% | 13.56% | |
| College | 18.36% | 14.94% | |
| Postgraduate | 5.51% | 4.80% | |
| Known Depression | Yes | 39.20% | 36.56% |
Table 2.
Calculating Expected Frequenices Per Clock Hour
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Hour | ATUS % Awake1 |
Scaled % Awake2 |
Expected # Awake3 |
Scaled Expected Awake4 |
Observed Frequency5 |
Observed %6 |
Adjusted %7 |
Scaled %8 |
Standardized Incidence Ratio (SIR)9 |
95% CI for SIR | P value |
| 0:00 | 14.47% | 0.89% | 4971.74 | 316.22 | 1153 | 3.26% | 23.19% | 8.27% | 3.65 | (3.43, 3.86) | <0.001 |
| 1:00 | 8.36% | 0.53% | 2954.17 | 187.89 | 1007 | 2.85% | 34.09% | 12.16% | 5.36 | (5.03, 5.70) | <0.001 |
| 2:00 | 5.89% | 0.37% | 2080.76 | 132.34 | 949 | 2.69% | 45.61% | 16.27% | 7.17 | (6.72, 7.64) | <0.001 |
| 3:00 | 5.34% | 0.34% | 1886.76 | 120.00 | 777 | 2.20% | 41.18% | 14.69% | 6.47 | (6.02, 6.94) | <0.001 |
| 4:00 | 10.19% | 0.65% | 3600.73 | 229.02 | 690 | 1.95% | 19.16% | 6.83% | 3.01 | (2.79, 3.24) | <0.001 |
| 5:00 | 21.89% | 1.39% | 7735.18 | 491.98 | 746 | 2.11% | 9.64% | 3.44% | 1.52 | (1.40, 1.62) | <0.001 |
| 6:00 | 47.40% | 3.01% | 16746.51 | 1065.13 | 1030 | 2.92% | 6.15% | 2.19% | 0.97 | 0.90, 1.02) | 0.2918 |
| 7:00 | 69.92% | 4.45% | 24704.73 | 1571.29 | 1241 | 3.51% | 5.02% | 1.79% | 0.79 | (0.74, 0.83) | <0.001 |
| 8:00 | 82.66% | 5.26% | 29206.87 | 1857.64 | 1548 | 4.38% | 5.30% | 1.89% | 0.83 | (0.79, 0.87) | <0.001 |
| 9:00 | 89.80% | 5.71% | 31728.35 | 2018.01 | 1748 | 4.95% | 5.51% | 1.96% | 0.87 | (0.82, 0.90) | <0.001 |
| 10:00 | 93.82% | 5.97% | 33149.08 | 2108.38 | 1814 | 5.13% | 5.47% | 1.95% | 0.86 | (0.82, 0.90) | <0.001 |
| 11:00 | 95.63% | 6.08% | 33787.45 | 2148.98 | 2027 | 5.74% | 6.00% | 2.14% | 0.94 | (0.90, 0.98) | 0.0081 |
| 12:00 | 96.34% | 6.13% | 34039.95 | 2165.04 | 2334 | 6.61% | 6.86% | 2.45% | 1.08 | (1.03, 1.12) | 0.001 |
| 13:00 | 95.92% | 6.10% | 33891.12 | 2155.57 | 1701 | 4.81% | 5.02% | 1.79% | 0.79 | (0.75, 0.82) | <0.001 |
| 14:00 | 96.01% | 6.11% | 33922.25 | 2157.55 | 1825 | 5.17% | 5.38% | 1.92% | 0.85 | (0.80, 0.88) | <0.001 |
| 15:00 | 96.46% | 6.13% | 34079.52 | 2167.55 | 1871 | 5.30% | 5.49% | 1.96% | 0.86 | (0.82, 0.90) | <0.001 |
| 16:00 | 96.81% | 6.16% | 34204.99 | 2175.53 | 1828 | 5.17% | 5.34% | 1.91% | 0.84 | (0.80, 0.87) | <0.001 |
| 17:00 | 97.26% | 6.19% | 34365.28 | 2185.73 | 1816 | 5.14% | 5.28% | 1.88% | 0.83 | (0.79, 0.86) | <0.001 |
| 18:00 | 97.43% | 6.20% | 34424.29 | 2189.48 | 1768 | 5.00% | 5.14% | 1.83% | 0.81 | (0.77, 0.84) | <0.001 |
| 19:00 | 96.80% | 6.16% | 34200.01 | 2175.22 | 1718 | 4.86% | 5.02% | 1.79% | 0.79 | (0.75, 0.82) | <0.001 |
| 20:00 | 93.09% | 5.92% | 32891.02 | 2091.96 | 1551 | 4.39% | 4.72% | 1.68% | 0.74 | (0.70, 0.77) | <0.001 |
| 21:00 | 79.91% | 5.08% | 28234.86 | 1795.82 | 1469 | 4.16% | 5.20% | 1.86% | 0.82 | (0.77, 0.86) | <0.001 |
| 22:00 | 53.28% | 3.39% | 18824.30 | 1197.28 | 1444 | 4.09% | 7.67% | 2.74% | 1.21 | (1.14, 1.26) | <0.001 |
| 23:00 | 27.96% | 1.78% | 9879.86 | 628.39 | 1277 | 3.61% | 12.93% | 4.61% | 2.03 | (1.92, 2.14) | <0.001 |
| SUM: | 1572.24% | 100.00% | 555509.83 | 35332 | 35332 | 100.00% | 280.37% | 100.00% |
The proportion of the population awake at each hour based on ATUS.
Proportions, divided by the total of all proportions (value from column 2, divided by the sum of all values from column 2). This scales each proportion so that they all sum to 100%.
Values from column 2, multiplied by the total N=35332. This represents the number of individuals from the sample expected to be awake at each hour.
Values from column 4, divided by the total of column 4. This normalizes all values to a 100% scale.
The observed number of suicides at each clock hour, from NVDRS.
The proportion of suicides occurring at each clock hour compared to the entire sample (obtained by dividing each value from column 6 by the total N=35332.
The proportion of suicides occurring at each clock hour compared to the amount of the sample that is estimated to have been awake at that time (obtained by dividing the number of observed suicides from column 6 by the expected # awake in column 4).
Values from column 8, divided by the sum of all values from column 8. This normalizes proportions so they all add up to 100.
SIR computed by dividing the observed frequency from column 6 (i.e., observed) by the scaled number expected awake from column 5 (i.e., expected).
95% Confidence Interval (95%CI) computed around the SIR.
P value for SIR
Characteristics of the Overall Sample (Adjusted Data).
When accounting for the proportion of the population that is likely awake at each given hour (see Table 2, Columns 2 & 9 and Figure 1, Panel C), the majority of suicides were committed at night with a peak frequency at 2am (16.3%) and a mean incident rate from 24:00-05:59 of 10.3% +/− 4.9%. In this model, 63.9% of the suicides occurred between midnight and 6am. The overall distribution, apart from midnight to 6am, was flat with an average incidence of suicide across the remaining 18 hours (6am-midnight) of 2.2% +/−0.7%, per hour. This 24-hour pattern of time of fatal self-injury (hour by hour) deviated from that which would be expected by chance (See Table 2, Columns 12). When the data were categorized in 6-hour bins (night, morning, afternoon, or evening), post-hoc pairwise chi-square tests (See Table 3) showed that the rate of suicide at night was significantly greater than the rate of occurrence during the morning, afternoon, and evening. Further, the differences between morning, afternoon, and evening were nominal.
Table 3.
Pairwise Chi-Square Comparisons among Rates of Night, Morning, Afternoon and Evening, Accounting for the Proportion of the Population Awake
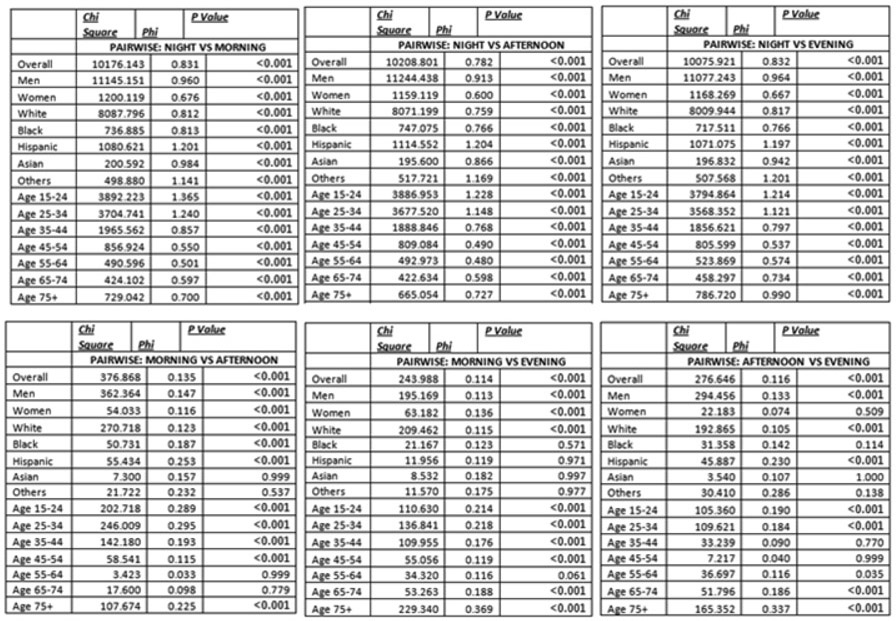 |
Stratified Analyses.
The temporal pattern effect of suicide was evaluated by age, sex, and race (See Table 4). When the sample was stratified by sex, the overall pattern of incidence of suicide over time, adjusting for likelihood of being awake, was maintained, with significant differences when examining hour-by-hour data and data by 6-hour categories. When examining effect sizes, there was a clear gender difference: the temporal effects for men were larger than for women. When the sample was stratified by race/ethnicity, the same temporal pattern emerged with nominal differences among groups. The largest effect sizes were seen among Hispanic/Latinos and the smallest effect sizes were seen among Black/African-Americans. When the sample was divided into 10-year age groups, the pattern remained, with significant omnibus effects for all groups. It should be noted, however, that effects were largest among the 15-24 and 25-34 age groups, and, to a lesser degree, the 35-44 age group. Analyses stratified by depression also show this pattern, with both depressed and non-depressed individuals showing increased prevalence of suicides at night (p < 0.0001 for both models).
Table 4.
Chi-Square and Phi Values Assessing whether the 24-Hour Distribution of Suicide Differs from Chance, Accounting for the Proportion of the Population Awake, Stratified by Age, Sex, and Ethnoracial Group
| 24 HOURS | NIGHT vs MORNING vs AFTERNOON vs EVENING |
|||||
|---|---|---|---|---|---|---|
| Group | Chi Square | Phi | P Value | Chi Square | Phi | P Value |
| Overall | 17102.757 | 0.696 | <0.001 | 10452.789 | 0.544 | <0.001 |
| Depressed | 4633.666 | 0.599 | <0.001 | 2735.311 | 0.460 | <0.001 |
| Men | 18282.137 | 0.798 | <0.001 | 11439.607 | 0.631 | <0.001 |
| Women | 2138.292 | 0.568 | <0.001 | 1222.302 | 0.430 | <0.001 |
| White | 13999.033 | 0.686 | <0.001 | 8280.661 | 0.527 | <0 001 |
| Black | 1126.573 | 0.649 | <0.001 | 768.242 | 0.536 | <0.001 |
| Hispanic | 2023.212 | 1.119 | <0.001 | 1126.508 | 0.835 | <0.001 |
| Asian | 241.145 | 0.682 | <0.001 | 204.132 | 0.628 | <0.001 |
| Others | 983.282 | 1.140 | <0.001 | 529.291 | 0.837 | <0.001 |
| Age 15-24 | 5460.433 | 1.046 | <0.001 | 3997.583 | 0.895 | <0.001 |
| Age 25-34 | 5797.393 | 1.012 | <0.001 | 3814.361 | 0.821 | <0.001 |
| Age 35-44 | 3960.947 | 0.766 | <0.001 | 1998.801 | 0.544 | <0.001 |
| Age 45-54 | 2061.963 | 0.533 | <0.001 | 864.141 | 0.345 | <0.001 |
| Age 55-64 | 1174.229 | 0.501 | <0.001 | 527.292 | 0.336 | <0.001 |
| Age 65-74 | 703.552 | 0.512 | <0.001 | 475.897 | 0.421 | <0.001 |
| Age 75+ | 1123.741 | 0.618 | <0.001 | 894.394 | 0.552 | <0.001 |
DISCUSSION
Summary of Main Results.
Only a few studies have examined the temporal patterning of suicide across the 24-hour day. The results of all the prior investigations indicated a higher prevalence of suicides during the day than at night. These findings were, however, are based on the assumption that the probability for suicide is equal during each hour of the 24 hour day. This is unlikely because the at-risk population (i.e., the denominator for the suicide rate) changes with time-of-day. In the present analysis, when accounting for the proportion of the population that is awake at each given hour, it was found that suicide is more likely to occur at night then during the morning, afternoon or evening hours. This finding was consistent across age groups, sex, race/ethnicity groups, and for depressed and non-depressed individuals. The effect sizes for the finding was nominally greater for younger individuals, males, and those identified as Hispanic/Latino.
Implications.
If suicide occurs disproportionately at night (as compared to other times during the 24 hour day), the emergent question is, “What about being awake at night confers risk?” One possibility is that being awake may be associated with reduced social support and increased utilization of alcohol and other substances which promote cognitive and behavioral disinhibition (e.g.,24,25). These factors alone, or in combination with other known and unknown factors, may confer increased risk for suicide. Another possibility, in line with current findings, is that insomnia and/or nightmares contribute to suicidal ideation and behavior by making it more likely that an afflicted individual will be awake at night; intensifying the individual’s sense of hopelessness, isolation, and distress relative to inability to sleep. Being awake at night (when one is not biologically predisposed to be awake) also likely results in a decrease in frontal lobe function (i.e., hypo-activation of the frontal lobes due to circadian effects, sleep loss /sleep deprivation, and/or sleep inertia) (e.g.,26). Hypofrontality, in turn, may result in diminished problem solving abilities and increased impulsive behavior, both of which may be expected to increase the risk for suicide. This possibility suggests that one way to reduce the risk of suicide is to ensure that individuals are not awake when they are disproportionately vulnerable. Conceptualized this way, it follows that 1) targeted treatment for insomnia and nightmares and 2) the increased allocation / utilization of psycho-social resources at night (e.g., increased availability of peer and professional support) should have substantial value as preventive strategies for suicide.
Limitations.
The NVDRS data set does not contain data regarding why individuals that die by suicide at night were awake from midnight to 06:00. Although insomnia and awakenings from nightmares seem like reasonable explanations, it is also possible that the individuals who die by suicide at night did so deliberately; that is, they simply stayed awake until a chosen hour. Further, while the given data make it clear that being awake at night is a risk, there are no data to allow for an assessment of which factors (e.g., social isolation, access to weapons, alcohol and substance use, or decreased executive functioning) alone or in combination, undergird the observed finding. Finally, the use of the ATUS data set to estimate proportion of the population awake at each across the 24 hour day may systematically under represent the segment of the population of depressed and/or suicidal individuals that are awake during the traditional sleep period and asleep during the day.
Future Directions.
Several directions seem possible. First, a large scale psychological autopsy study could be undertaken to assess the relative contribution of insomnia and/or nightmares, social isolation, access to substances to the observed finding. Second, within-subject circadian experimental paradigms (with or without QEEG measures of frontal lobe activity) could be used to assess how executive function, suicidal ideation, and/or impulsive behavior vary as a function of time of day, especially in at-risk subjects. Third, large scale studies of circadian effects on decision making and/or impulsive behavior could be conducted in other populations that are more easily tracked (e.g., data sets that have hour by hour data related to on-line gambling, shopping, or social networking). Finally, as suggested above, an indirect assessment of the association, and the importance of, being awake during the normal sleep period (circadian night) could be accomplished by assessing whether treatment for insomnia and/or nightmares or increased nighttime psychosocial support in at risk populations diminishes suicidal ideation and behavior. This last possibility appears to particularly viable given the results from a recent study by Manber and colleagues (2015) which provides the first evidence that Cognitive Behavioral Therapy for Insomnia (CBT-I) can significantly reduce suicidal ideation27.
Footnotes
Conflict of Interest Statement: I/we certify that there is no actual or potential conflict of interest in relation to this article.
REFERENCES
- 1.Heron M. Deaths: Leading causes for 2010. National Vital Statistics Reports. 2013;62(6):1–97. [PubMed] [Google Scholar]
- 2.Ribeiro JD, Pease JL, Gutierrez PM, et al. Sleep problems outperform depression and hopelessness as cross-sectional and longitudinal predictors of suicidal ideation and behavior in young adults in the military. J Affect Disord. February 2012;136(3):743–750. [DOI] [PubMed] [Google Scholar]
- 3.Hyman J, Ireland R, Frost L, Cottrell L. Suicide incidence and risk factors in an active duty US military population. Am J Public Health. March 2012;102 Suppl 1:S138–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee YJ, Cho SJ, Cho IH, Kim SJ. Insufficient sleep and suicidality in adolescents. Sleep. April 2012;35(4):455–460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pigeon WR, Pinquart M, Conner K. Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. The Journal of clinical psychiatry. September 2012;73(9):e1160–1167. [DOI] [PubMed] [Google Scholar]
- 6.Bjorngaard JH, Bjerkeset O, Romundstad P, Gunnell D. Sleeping problems and suicide in 75,000 norwegian adults: a 20 year follow-up of the HUNT I study. Sleep. September 2011;34(9):1155–1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McCall WV. Insomnia is a risk factor for suicide-what are the next steps? Sleep. September 2011;34(9):1149–1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pigeon WR, Caine ED. Insomnia and the risk for suicide: Does sleep medicine have interventions that can make a difference? Sleep Med. October 2010;11(9):816–817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McCall WV, Blocker JN, D'Agostino R Jr., et al. Insomnia severity is an indicator of suicidal ideation during a depression clinical trial. Sleep Med. October 2010;11(9):822–827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mahgoub NA. Insomnia and suicide risk. J Neuropsychiatry Clin Neurosci. Spring 2009;21(2):232–233. [DOI] [PubMed] [Google Scholar]
- 11.Wojnar M, Ilgen MA, Wojnar J, McCammon RJ, Valenstein M, Brower KJ. Sleep problems and suicidality in the National Comorbidity Survey Replication. J Psychiatr Res. February 2009;43(5):526–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bernert RA, Joiner TE Jr., Cukrowicz KC, Schmidt NB, Krakow B. Suicidality and sleep disturbances. Sleep. September 2005;28(9):1135–1141. [DOI] [PubMed] [Google Scholar]
- 13.Blasco-Fontecilla H, Alegria AA, Lopez-Castroman J, et al. Short self-reported sleep duration and suicidal behavior: a cross-sectional study. J Affect Disord. September 2011;133(1-2):239–246. [DOI] [PubMed] [Google Scholar]
- 14.van Houwelingen CA, Beersma DG. Seasonal changes in 24-h patterns of suicide rates: a study on train suicides in The Netherlands. Journal of affective disorders. October 2001;66(2-3):215–223. [DOI] [PubMed] [Google Scholar]
- 15.Preti A, Miotto P. Diurnal variations in suicide by age and gender in Italy. Journal of affective disorders. August 2001;65(3):253–261. [DOI] [PubMed] [Google Scholar]
- 16.Altamura C, VanGastel A, Pioli R, Mannu P, Maes M. Seasonal and circadian rhythms in suicide in Cagliari, Italy. Journal of affective disorders. April 1999;53(1):77–85. [DOI] [PubMed] [Google Scholar]
- 17.Gallerani M, Avato FM, Dal Monte D, Caracciolo S, Fersini C, Manfredini R. The time for suicide. Psychological medicine. July 1996;26(4):867–870. [DOI] [PubMed] [Google Scholar]
- 18.Maldonado G, Kraus JF. Variation in suicide occurrence by time of day, day of the week, month, and lunar phase. Suicide & life-threatening behavior. Summer 1991;21(2):174–187. [PubMed] [Google Scholar]
- 19.Williams P, Tansella M. The time for suicide. Acta psychiatrica Scandinavica. May 1987;75(5):532–535. [DOI] [PubMed] [Google Scholar]
- 20.Barraclough BM. Time of day chosen for suicide. Psychological medicine. May 1976;6(2):303–305. [DOI] [PubMed] [Google Scholar]
- 21.Vollen KH, Watson CG. Suicide in relation to time of day and day of week. The American journal of nursing. February 1975;75(2):263. [DOI] [PubMed] [Google Scholar]
- 22.National Center for Injury Prevention and Control. National Violent Death Reporting System (NVDRS). Atlanta, GA: Centers for Disease Control and Prevention; 2013. [Google Scholar]
- 23.Bureau of Labor Statistics. American Time Use Survey Fact Sheet. Washington, DC: Bureau of Labor Statistics; 2013. [Google Scholar]
- 24.You S, Van Orden KA, Conner KR. Social connections and suicidal thoughts and behavior. Psychology of addictive behaviors : journal of the Society of Psychologists in Addictive Behaviors. March 2011;25(1):180–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vijayakumar L, Kumar MS, Vijayakumar V. Substance use and suicide. Current opinion in psychiatry. May 2011;24(3):197–202. [DOI] [PubMed] [Google Scholar]
- 26.Vandewalle G, Archer SN, Wuillaume C, et al. Functional magnetic resonance imaging-assessed brain responses during an executive task depend on interaction of sleep homeostasis, circadian phase, and PER3 genotype. J Neurosci. June 24 2009;29(25):7948–7956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Trockel M, Karlin BE, Taylor CB, Brown GK, Manber R. Effects of cognitive behavioral therapy for insomnia on suicidal ideation in veterans. Sleep. 2015;38(2):259–265. [DOI] [PMC free article] [PubMed] [Google Scholar]