Abstract
Posttraumatic Stress Disorder (PTSD) is a primary mental health concern of veterans. In clinical settings, efforts to improve broad facets beyond symptom amelioration and consideration of moderators of treatment effectiveness in this population are needed for continued improvement in care. General self-efficacy (GSE) has been indicated as a useful treatment target because of its association with positive outcomes such as increased positive health behaviors. Both race and educational attainment represent potential moderators of treatment response that are relevant for a veteran PTSD population. This study aimed to determine whether a PTSD Recovery Group Therapy Program resulted in improvement in GSE and whether racial and educational differences moderated GSE outcomes. Archival data was examined from male veterans (N = 450) receiving mental health services at a Veteran’s Affair Medical Center using multilevel modeling to examine change in GSE over the course of treatment as well as moderation of change in GSE as a function of race and educational attainment. After completion of group therapy, results indicated there was significant improvement in GSE, with significantly different improvement based on education. Higher levels of education were associated with greater increases in GSE post-treatment. Improvement in GSE did not differ by participant race. In clinical settings, efforts to increase GSE and attending to moderators such as educational attainment may be useful for improving PTSD treatment approaches.
Keywords: veterans, PTSD, general self-efficacy, group therapy, treatment moderators
Posttraumatic Stress Disorder (PTSD) is one of the primary mental health concerns of veterans following combat (Steenkamp, Litz, Hoge, & Marmar, 2015). Estimates of lifetime prevalence of PTSD in Vietnam combat veterans have ranged from 18–19% (Dohrenwend et al., 2007) to 30% (Weiss et al., 1992); a nationally representative survey of veterans from more recent conflicts estimated rates at 20% (Elbogen et al., 2013). Compared to lifetime prevalence rates of approximately 8% in epidemiological surveys in the U.S. (Kilpatrick et al., 2013), the prevalence of PTSD in veterans is notably higher than in civilians. These rates, the chronic nature of PTSD, and the association of PTSD with functional impairment, high psychiatric comorbidity, and reduced quality of life (Richardson et al., 2010), highlight PTSD as an important and costly disorder, illustrating the need for continued treatment efforts.
Cognitive behavioral therapy (CBT) is considered a “gold standard” treatment for PTSD (Koucky, Dickstein, & Chard, 2013), which consists of structured sessions focused on altering cognitions and behaviors. It includes specific manualized treatments and less standardized applications; variations of CBT have been implemented in the Department of Veterans Affairs. There have been a growing number of CBT-based therapy groups for PTSD with literature supporting positive outcomes (i.e., decreases in PTSD symptoms; see meta-analysis by Sloan, Bovin, & Schnurr, 2012). However, in clinical settings, goals of successful group treatment also include broader outcomes beyond PTSD symptom improvement and thus warrant further research efforts.
Increased self-efficacy (SE) is a useful treatment goal given its association with a wide range of positive outcomes. SE is a broad construct, with general self-efficacy (GSE) more specifically conceptualized as a sense of one’s perceived ability to influence functioning across domains (Schwarzer & Jerusalem, 1995). GSE may be particularly meaningful in individuals with long-standing or chronic symptoms, as repeated perceptions that they lack capabilities (i.e., to cope with symptoms) can result in avoidance of challenges and tendency to give up in the face of difficulties (Bandura, 1994). Thus, it would be expected that CBT, with its focus on teaching and practicing new skills, may influence GSE. This represents an important outcome variable in the treatment of PTSD, as it has been shown to influence reactions to trauma (Cyniak-Cieciura, Popiel, & Zawadzki, 2015; Łuszczyńska, Benight & Cieślak, 2009) and been associated with positive health behaviors (e.g., exercise) and decreases in maladaptive coping strategies (e.g., substance use; Schnurr et al., 2007) more generally. As such, the present study aimed to identify whether GSE levels increased over the course of a group treatment for PTSD, implemented in a VA clinic setting.
A second aim of this study was to examine moderators of the PTSD treatment group in improving GSE, given their potential relevance for group participants’ treatment experience and outcomes. Both educational performance (Fenning & May, 2013) and ethnic minority status (Pajares & Schunk, 2001) have been associated with SE, and both represent factors previously examined as treatment moderators, although the literature is limited and mixed. While it has been proposed that patients with higher intelligence benefit more from CBT (e.g., Garfield, 1986), empirical evidence to support this theory is sparse. A limited literature has suggested education is a significant indicator of treatment outcome (Ehlers, Clark, Hackmann, McManus, & Fennell, 2005; Fournier et al., 2009), although others have found that treatment outcomes for a range of psychopathologies (e.g., depression, PTSD) are not impacted by intelligence or education (e.g., Andersson, Carlbring, & Grimlund, 2008). Additionally, a limited research has demonstrated that racial minority veterans are less likely to engage in psychotherapy and to receive adequate care (Doran, Pietrzak, Hoff, & Harpaz-Rotem, 2017), but less is known about the association of minority status with treatment response. Given the generally smaller sample sizes of the existent literature examining these moderators, these studies may not have been powered to detect potential interaction effects. In summary, the associations of education level and racial differences with mental health outcomes, such as GSE, in a treatment setting remains unclear. As such, more work is needed to clarify the role of these moderators.
The current study had two primary aims. The first was to assess the ability of a group-based treatment, the PTSD Recovery Program, to increase veterans’ GSE. Improvements in GSE were hypothesized. The second aim was to examine the potential role of race and education, specifically whether racial differences and education were associated with GSE at baseline and with change in GSE over the course of treatment. Based on the limited literature, it was hypothesized that African American group members would report lower baseline GSE compared to Caucasian group members, but that GSE change would not differ by race, based on other findings by our group with regard to PTSD symptom change (Authors et al., under review). We hypothesized that education would impact GSE change over the course of therapy based on the limited existing literature. As an additional, exploratory aim, given the potential relevance of GSE for mental health treatment, we also examined the association between pre-treatment GSE and PTSD symptom change, with higher baseline GSE hypothesized to predict greater PTSD symptom improvement.
Methods and Materials
Participants
The current study used data from a Mid-Atlantic Veteran’s Affairs Medical Center (VAMC) and was approved by the local IRB. Participant data was extracted from electronic medical records, clinical intakes, and program evaluation data from a group therapy program, the PTSD Recovery Program. All participants were patients enrolled in the PTSD clinic, an outpatient clinic for combat veterans with PTSD. Before enrollment in the PTSD clinic, veterans were seen for an intake evaluation during which a provider assessed for PTSD through chart review, clinical interview, and administration of a Posttraumatic Stress Disorder Checklist-Military version (PCL-M). The following were considered as inclusion criteria for the study: combat history, diagnosis of PTSD, and initiation in the PTSD Recovery Program between 2010 and 2014, male sex, non-Hispanic Caucasian or non-Hispanic African American race/ethnicity, and completion of the GSE and PCL-M measures at pre-treatment or post-treatment. Non-Hispanic Caucasian were the only minority group included in this study, in order to clearly explore potential differences between one minority group (i.e., African American veterans) to a non-minority group (i.e., non-Hispanic Caucasian veterans). Further, prevalence of group members from other minority groups was small, thus limiting the power to detect other potential group differences. Data were collected on a total of 521 individuals; the current study consisted of a subgroup of the entire sample that met the above inclusion criteria resulting in a study sample of N = 450.
Measures
Client demographics
Demographic and diagnostic information collected from electronic medical records review and PTSD outpatient clinic intake notes included: age, sex, race, ethnicity (e.g., Hispanic), marital status, education, employment status, period of service (e.g., Vietnam), branch of service, highest enlisted rank, lifetime psychiatric diagnoses (e.g., mood disorder), and previous trauma history. Education was coded into five interval groups: less than 12 years, G.E.D./high school diploma/12 years, 13–15 years, Bachelor’s degree/16 years, and post Bachelor’s degree/over 16 years.
General self efficacy scale (GSE)
The General Self Efficacy Scale (Schwarzer, & Jerusalem, 1995) serves as the primary outcome measure. The original scale consists of 10 items yielding a score between 10 and 40, where higher scores indicate higher levels of GSE. However, instead of four Likert response options, prior to this program evaluation, a clinician in the PTSD clinic was utilizing an alternative response set for the GSE. Thus, for the current study, the item response options were as follows: 1 = Never, 2 = Rarely, 3 = Sometimes, 4 = Most often, 5 = All or almost all of the time, leading to a possible score between 10 and 50. While earlier studies have confirmed high reliability, stability, and construct validity of the original scale (e.g., Leganger, Kraft, & Røysamb, 2000), it is unknown if this alternative response set operates in the same way as the original GSE. In this study the scale continued to show good internal consistency at pre-treatment (α = .90).
Posttraumatic Stress Disorder Checklist-Military Version (PCL-M)
The Posttraumatic Stress Disorder Checklist-Military Version (Weathers et al., 1991) is a 17 item questionnaire that asks respondents to answer questions based on symptoms over the last month using a 5-point Likert scale (1 = Not at all, 5 = Extremely) associated with the Diagnostic and Statistical Manual of Mental Disorders (4th ed.; text rev.; DSM-IV-TR; American Psychiatric Association, 2000) PTSD criteria. Items are summed to create a total score ranging from 17 to 85 where higher scores indicate more severe PTSD. The PCL-M has been shown to be psychometrically strong (1-week test-retest reliability of .87 and internal consistency of .91) and correlate strongly (r = .65) with the CAPS total severity score (Adkins, Weathers, McDevitt-Murphy, & Daniels, 2008). In this study, the Cronbach’s alpha for the total score was .89.
PTSD Recovery Program
The PTSD Recovery Program consisted of 10 weekly therapy sessions lasting for 90 minutes each, with an average of 10 veterans per group. Measures were administered at the beginning of session 1 and 10. The group was usually run by two clinicians (e.g., licensed psychologists, licensed social workers, graduate students in psychology, and graduate students in social work) who utilized the PTSD Recovery Program manual (Authors et al., 2010). Veterans had a participant version of the manual. The PTSD Recovery Program includes elements of psychoeducation, CBT, in vivo exposure, stress management, acceptance and commitment therapy, mindfulness, and interpersonal effectiveness skills training.
Data analysis
The data were analyzed using SPSS version 24.0 (Armonk, NY: IBM Corp.) and R version 3.2.4 (R Core Team, 2015) using the psych (Revelle, 2015), nlme (Pinheiro, Bates, DebRoy, Sarkar, & R Core Team, 2016), and ggplot2 packages (Wickham, 2009). Given the nested nature of the data (i.e., time nested in person within group within provider) and a high number of missing data points (131 missing pre-treatment data, 197 missing post-treatment data) due to the nature of clinical treatment, linear mixed effect models (i.e., multilevel modeling) with full information maximum likelihood estimation were used to examine the three research aims. Data was included for individuals who had completed a GSE Scale and PCL-M at either pre-treatment or post-treatment, as our analyses allowed for missing data at one time point.
Intra-class correlation coefficients (ICCs) for each of the four levels (i.e., time, participant, provider, group) were calculated to determine the optimal model for change in GSE. ICCs indicated that 39.58% of the variance in GSE was due to nesting time points within person while less than 2.00% of the variance in GSE was due to nesting time and person within group or provider. 60.42% of the variance remained within person. To further examine whether data were exchangeable with regard to group and provider, we estimated the model for GSE with nesting due to group and provider removed. Model fit was unchanged, Δχ2 (2) = 7.95×10−7, p = 1.00, which indicates that principal analyses should be conducted using a two-level linear mixed effects model to account for nesting of time within person. Time was added to the model to examine aim 1, overall change in GSE symptom severity over the course of treatment. Prior to examining associations with baseline GSE and moderation of change in GSE, intercept and linear slope in GSE were allowed to vary by person.
For aim 2, to test the potential moderators of participant race and education level on GSE, these variables were separately added as main effects and interactions with time. Main effects index the influence of each variable on baseline GSE whereas interaction effects index deviation in change over time as a function of the moderator.
For the exploratory aim, to examine the influence of baseline GSE on change in PTSD symptom severity, similar model determination steps were taken as above to determine the best fitting model for PTSD. ICCs indicated that 43.42% of the variance in PTSD was due to nesting time points within person while 1.04% of the variance in PTSD was due to nesting time and person within group and 3.37% due to nesting time and person within provider. The remainder of the variance (52.17%) was within person. Model fit was not significantly changed with nesting due to group removed, Δχ2 (1) = 0.23, p = 0.63, which indicated that data were exchangeable with regard to therapy group. GSE was then entered as a main effect and interaction with the linear slope that described change in PTSD symptom severity.
Results
Demographics and descriptive statistics
A total of 450 participants were included in the current analyses. The sample was primarily African American (n = 278, 62%) and married (n = 303, 67%) with an average age of 54.56 (SD = 13.65). The sample primarily consisted of veterans from the Persian Gulf War (n = 204, 45%) and/or the Vietnam War (n = 206, 46%). Descriptive statistics are presented in Table 1. A total of twenty different providers lead groups, seventeen of which provided demographic information. Therapy providers were mostly female (75%), non-Hispanic Caucasian (88%), and the majority held a graduate degree (65%).
Table 1.
Descriptive Statistics for Self-Efficacy and PTSD measures
| Non-Hispanic African American |
Non-Hispanic Caucasian |
Total Sample |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| N | M | SD | N | M | SD | N | M | SD | |
| Pre-treatment PCL-M | 241 | 63.24 | 11.74 | 137 | 62.65 | 10.72 | 350 | 63.02 | 11.29 |
| Post-treatment PCL-M | 199 | 56.17 | 12.96 | 108 | 54.30 | 12.68 | 286 | 55.89 | 12.88 |
| Pre-treatment GSE | 235 | 30.78 | 7.13 | 134 | 32.51 | 6.65 | 341 | 31.64 | 6.93 |
| Post-treatment GSE | 198 | 32.67 | 6.05 | 108 | 34.58 | 7.00 | 285 | 33.44 | 6.62 |
Note. PCL-M = Posttraumatic Stress Disorder Checklist-Military Version; GSE = General Self Efficacy Scale.
Participants with incomplete data (n = 219) did not significantly differ from those with complete pre- and post-treatment data (n = 231) on education level, rank, service connection, or baseline self-efficacy (ps > .06). However, missing data was significantly associated with age; participants who were missing data (M = 52.33) were, on average, younger than those who were not (M = 56.44), t(272.55) = 2.88, p = 0.004. Due to the association with missing data, subsequent analyses were also computed adjusting for participant age; results were unchanged. The following results present estimates without adjustment.
Multilevel modeling
Aim 1, change in GSE
There was a significant effect of time with person for the GSE slope, B = 1.75, 95% CI [0.89, 2.62], p < .001, (see Table 2). Participants’ GSE total scores significantly improved from pre-treatment to post-treatment.
Table 2.
Change in GSE over time and across educational levels
|
|
||
|---|---|---|
| Estimate (95% CI) | p | |
|
|
||
| Step 1 | ||
| Intercept | 31.64 (30.92–32.36) | <0.001 |
| Linear Slope (Time) | 1.79 (0.93–2.66) | <0.001 |
| Step 2 | ||
| Intercept | 34.28 (29.35–39.21) | <0.001 |
| Linear Slope (Time) | −5.54 (−11.55–0.47) | 0.07 |
| 12 years education | −3.09 (−8.13–1.95) | 0.23 |
| 13–15 years education | −2.55 (−7.82–2.71) | 0.35 |
| 16 years education | −2.16 (−7.28–2.95) | 0.41 |
| Over 16 years education | −1.45 (−7.03–4.14) | 0.61 |
| 12 years education*Time | 6.66 (0.52–12.81) | 0.04 |
| 13–15 years education*Time | 7.64 (1.28–14.00) | 0.02 |
| 16 years education*Time | 8.14 (1.92–14.35) | 0.01 |
| Over 16 years education*Time | 8.79 (2.00–15.58) | 0.01 |
Note. The reference category for education is less than 12 years of education. Models were estimated with random effects for intercept and slope (i.e., time); estimates are available from the authors upon request.
Aim 2, the role of education and race in change in GSE
Education was not associated with baseline GSE. However, high educational attainment was associated with greater increases in GSE over time (see Table 2, step 2, and Figure 1). Furthermore, inspection of interaction terms indicated a greater linear slope, which suggested greater increases in GSE for each increase in educational attainment (see Figure 1). Participant race showed no evidence of an association with baseline GSE (i.e., a main effect), B = −1.34, 95% CI [−2.80, .13], p = .07. Additionally, there was no evidence to support a cross-level interaction effect wherein race would moderate change in GSE, B = −.41, 95% CI [−2.19, 1.36, p = .65. Given that GSE improved overall, this suggested that both races demonstrated improvement in GSE at similar rates.
Figure 1.
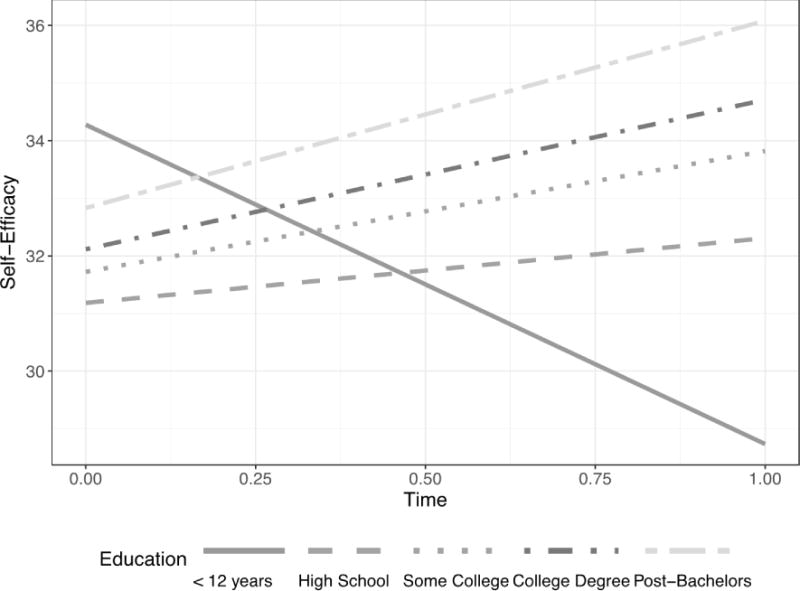
Relationship between GSE increase and educational attainment
Exploratory aim, the role of GSE in PTSD symptom severity improvement
Elevated baseline GSE was associated with lower baseline PTSD symptom severity, B = −.21, 95% CI [−.38, −.04], p = .02. While there was evidence that PTSD symptomology decreased over time, B = −7.17, 95% CI [−8.55, 5.79], p < .001, GSE did not moderate this change, B = −.19, 95% CI [−.28, .13], p = .48.
Discussion
The primary aims of this study were to determine if 1) a PTSD group treatment program was effective in improving veterans’ self-efficacy and 2) if race and educational attainment were associated with baseline and moderated change in GSE. Results will be discussed in the context of relevant clinical implications.
Improvement in GSE
This study found significant improvements in GSE from pre- to post-treatment as hypothesized; however, the effect size was small. While SE may not be considered a primary treatment target in comparison to symptom reduction, in clinical settings it is often apparent that goals beyond symptom reduction are particularly meaningful to patients. Given the other positive outcomes associated with increased GSE (e.g., Schnurr et al., 2007) it may be that such increases further support continued improvement over time, after completion of group treatment, stemming from patient increases in sense of mastery. Indeed, GSE represents a self-confident view of one’s capability to deal with life stressors (Warner, Schwarzer, Schüz, Wurm, & Tesch-Römer, 2012) and focusing on this point may be useful in aiding generalization and maintenance following completion of treatment. The group treatment modality may be particularly effective in increasing SE, given that one way to increase SE is through exposure to vicarious experiences through social modeling (Bandura, 1994), and it is suggested that this social modeling is specifically highlighted in group treatment approaches (e.g., leader modeling; Burlingame, Fuhriman, & Johnson, 2001). In the group setting, veterans are able to see other veterans succeeding at therapeutic tasks, and thus, may experience an increase in their own SE.
The role of race and education as moderators of GSE change
For aim two, contrary to our hypothesis, there were no racial differences in pre-treatment GSE, but in line with expectations, African American group members were as likely to show improvements in GSE as compared to Caucasian group members. The finding of no racial differences in improvement in GSE adds to the literature with regard to identifying and understanding racial differences in treatment utilization, retention, and benefit. The group treatment modality may have a positive impact and be in part responsible for the lack of racial differences in GSE improvement, which is potentially important from a service delivery perspective. For example, racially diverse groups may allow all members the opportunity to have vicarious learning experiences from group members they are able to relate to as well as ones with different backgrounds and life experiences. It is promising that extant studies have suggested there is little evidence of clinically significant differences by racial/ethnic minority status on positive treatment expectancies for PTSD (Koo, Tiet, & Rosen, 2016).
Educational level was not associated with baseline GSE in the current study, but was associated with change over time, as hypothesized, in that participants with higher levels of education showed greater increases in GSE. These findings are consistent with previous literature that demonstrates the prognostic effects of education on treatment response, wherein higher education levels predicted lower depression scores at week 16 of a treatment (Fournier et al., 2009) and were associated with being asymptomatic upon completion of a depression treatment protocol (Gelhart, Hand-Ronga, & King, 2002). In the current study, GSE levels did not improve as much in participants with lower education levels. Low educational attainment may thus represent an important moderator wherein low levels of educational attainment may negatively impact success in CBT and warrant clinical attention when designing or tailoring treatment protocols. In clinical settings, such as the present study sample primarily of Vietnam veterans, a wide range of educational history is to be expected, and should be considered. From a service delivery perspective, findings suggest that individuals with lower levels of education may need additional sessions to master certain skills, may benefit more from a different type of treatment approach that is more individualized to allow for mastery experiences, or, may benefit from sessions aimed at increasing sense of self-efficacy prior to initiating group sessions for PTSD to increase likelihood of success during treatment. Future studies of educational attainment as a moderator of treatment response in this population would benefit from more specific and nuanced examination than what was available in the present study.
Pre-treatment GSE and PTSD symptom change
Contrary to the hypothesis for the exploratory aim, baseline GSE did not impact PTSD symptom improvement over time. Although our primary goal was to examine GSE as an outcome, it is associated with PTSD; thus, we were interested in its association with PTSD symptoms in a treatment setting as an effort to expand on our prior work with this data showing improvements in PTSD symptoms (Author et al., under review). Given that baseline GSE was associated with lower PTSD symptoms at the outset, but not change over time, an important goal of treatment for PTSD may be to address GSE at early stages of intervention efforts.
Limitations and future directions
Although this study expands the limited literature with regard to racial and educational differences in GSE, it is not without limitations. The study used program evaluation data from a manualized treatment implemented in a PTSD clinic within the VA. Thus, there are inherent limitations with regard to number of measurements, controlling for comorbidity, likely greater variability in the administration of the manual, as well as the lack of a clinical comparison and lack of documentation regarding reasons for treatment dropout. Future studies would benefit from examination of other important moderators (e.g., stigma, comorbid conditions). It is important to note that the current study used an adapted version of the SE scale with an extra response option, and thus, scores cannot be compared to GSE scores across populations. However, improvement in GSE does seem important for outcomes after experiencing a trauma; in a non-veteran trauma survivor population, higher SE was associated with lower PTSD and depressive symptoms (Luszczynska, Benight, & Cieslak, 2009).
Future studies should link improvements in GSE to adaptive and functional outcomes often associated with PTSD such as marital concerns (Jordan et al., 1992), job instability (Smith, Schnurr, & Rosenheck, 2005), and physical health problems (Boscarino, 2004). Follow-up data was not available in the present study, but given the chronic nature of PTSD, examination of the long-term maintenance of effects is needed. Finally, based on the nature of the clinic demographics, this study examined racial/ethnic minority status with regard to African Americans only. Findings cannot speak to broader minority differences in outcomes. Future work in this area is warranted given evidence of high prevalence of PTSD among American-Indian veterans (Frueh, Brady, & de Arellano, 1998) and Asian-American veterans (Loo, Fairbank, & Chemtob, 2005). It is also unknown whether the present findings would expand to female veterans; given evidence that patterns of treatment utilization, engagement, and benefit differ in males and females (e.g., Doran et al., 2017), research is this area is needed. Lastly, although combat exposure and combat trauma exposure were inclusion criteria, it is not confirmed that combat trauma is the trauma linked to the development of PTSD addressed in treatment. Indeed, childhood abuse history is common in veterans with PTSD, as was seen in this sample (18.4%). Additional and more detailed information regarding participants’ traumas would be useful in confirming the capability of the PTSD group treatment to improve GSE levels in combat trauma exposed veterans.
Conclusions
Despite these limitations, findings of this study suggest GSE increased over the course of the PTSD Recovery group. This increase occurred regardless of racial status, but was impacted by educational attainment, such that those with greater education levels experienced greater treatment gains. From a service delivery perspective, the finding suggesting the benefit of treatment for PTSD implemented by a range of providers in a clinical VA setting is important, as is the potential relevance of attending to treatment moderators such as educational attainment in tailoring treatment to increase success.
Acknowledgments
This material is the result of work supported with resources and the use of facilities at the Hunter Holmes McGuire VA Medical Center, Richmond, VA. The contents of this do not represent the views of the U.S. Department of Veterans Affairs or the United States Government. We would also like to thank Dr. John Lynch for his contributions to this study.
Funding: Drs. Sheerin and Rappaport’s time is supported by NIH grant T32 MH020030.
Project Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Adkins JW, Weathers FW, McDevitt-Murphy M, Daniels JB. Psychometric properties of seven self-report measures of posttraumatic stress disorder in college students with mixed civilian trauma exposure. Journal of Anxiety Disorders. 2008;22:1393–1402. doi: 10.1016/j.janxdis.2008.02.002. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 2000. text rev. [Google Scholar]
- Andersson G, Carlbring P, Grimlund A. Predicting treatment outcome in internet versus face to face treatment of panic disorder. Computers in Human Behavior. 2008;24:1790–1801. doi: 10.1016/j.chb.2008.02.003. [DOI] [Google Scholar]
- Author et al. PTSD recovery program: Treatment manual. 2010 Retrieved from http://www.mirecc.va.gov/docs/visn6/PTSD_Recovery_Group_Client_Manual.pdf.
- Author et al. (under review). Effectiveness of the Posttraumatic Stress Disorder (PTSD) Recovery Group Therapy Program for African American and Caucasian combat veterans
- Bandura A. Self-efficacy. In: Ramachaudran VS, editor. Encyclopedia of human behavior. Vol. 4. New York: Academic Press; 1994. pp. 71–81. [Google Scholar]
- Boscarino JA. Posttraumatic stress disorder and physical illness: Results from clinical and epidemiologic studies. Annals of the New York Academy of Sciences. 2004;1032:141–153. doi: 10.1196/annals.1314.011. [DOI] [PubMed] [Google Scholar]
- Burlingame GM, Fuhriman A, Johnson JE. Cohesion in group psychotherapy. Psychotherapy: Theory, Research, Practice, Training. 2001;38:373–379. doi: 10.1037/0033-3204.38.4.373. [DOI] [Google Scholar]
- Cyniak-Cieciura M, Popiel A, Zawadzki B. General self-efficacy level and changes in negative posttraumatic cognitions and posttraumatic stress disorder (PTSD) symptoms among motor vehicle accident survivors after PTSD therapy. Studia Psychologiczne. 2015;53:19–32. doi: 10.2478/v10167-010-0112-3. [DOI] [Google Scholar]
- Dohrenwend BP, Turner JB, Turse NA, Adams BG, Koenen KC, Marshall R. Continuing controversy over the psychological risks of Vietnam for US veterans. Journal of Traumatic Stress. 2007;20:449–465. doi: 10.1002/jts.20296. [DOI] [PubMed] [Google Scholar]
- Doran JM, Pietrzak RH, Hoff R, Harpaz‐Rotem I. Psychotherapy utilization and retention in a national sample of veterans with PTSD. Journal of Clinical Psychology. 2017;73:1–21. doi: 10.1002/jclp.22445. [DOI] [PubMed] [Google Scholar]
- Ehlers A, Clark DM, Hackmann A, McManus F, Fennell M. Cognitive therapy for post-traumatic stress disorder: development and evaluation. Behaviour research and therapy. 2005;43:413–431. doi: 10.1016/j.brat.2004.03.006. [DOI] [PubMed] [Google Scholar]
- Elbogen EB, Wagner HR, Johnson SC, Kinneer P, Kang H, Vasterling JJ, Beckham JC. Are Iraq and Afghanistan veterans using mental health services? New data from a national random-sample survey. Psychiatric Services. 2013;64:134–141. doi: 10.1176/appi.ps.004792011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenning BE, May LN. Where there is a will, there is an A”: examining the roles \ of self-efficacy and self-concept in college students’ current educational attainment and career planning. Social Psychology of Education. 2013;16:635–650. doi: 10.1007/s11218-013-9228-4. [DOI] [Google Scholar]
- Fournier JC, DeRubeis RJ, Shelton RC, Hollon SD, Amsterdam JD, Gallop R. Prediction of response to medication and cognitive therapy in the treatment of moderate to severe depression. Journal of Consulting and Clinical Psychology. 2009;77:775–787. doi: 10.1037/a0015401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frueh BC, Brady KL, de Arellano MA. Racial differences in combat-related PTSD: Empirical findings and conceptual issues. Clinical Psychology Review. 1998;18:287–305. doi: 10.1016/S0272-7358(97)00087-1. [DOI] [PubMed] [Google Scholar]
- Garfield SL. Research on client variables in psychotherapy. In: Garfield SL, Bergin AE, editors. Handbook of psychotherapy and behavior change. 3. New York: Wiley; 1986. [Google Scholar]
- Gelhart RP, Hand-Ronga N, King HL. Group cognitive-behavioral treatment of depression and the interaction of demographic variables. Journal of Cognitive Psychotherapy. 2002;16:469–486. doi: 10.1891/jcop.16.4.469.52525. [DOI] [Google Scholar]
- Jordan BK, Marmar CR, Fairbank JA, Schlenger WE, Kulka RA, Hough RL, Weiss DS. Problems in families of male Vietnam veterans with posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 1992;60:916–926. doi: 10.1037/0022-006X.60.6.916. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, Friedman MJ. National estimates of exposure to traumatic events and PTSD prevalence using DSM‐IV and DSM‐5 criteria. Journal of traumatic stress. 2013;26:537–547. doi: 10.1002/jts.21848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koo KH, Tiet QQ, Rosen CS. Relationships between racial/ethnic minority status, therapeutic alliance, and treatment expectancies among veterans with PTSD. Psychological Services. 2016;13:317–321. doi: 10.1037/ser0000029. [DOI] [PubMed] [Google Scholar]
- Koucky EM, Dickstein BD, Chard KM. Cognitive behavioral treatment for posttraumatic stress disorder: Empirical foundations and new directions. CNS Spectrum. 2013;18:73–81. doi: 10.1017/S1092852912000995. [DOI] [PubMed] [Google Scholar]
- Leganger A, Kraft P, Røysamb E. Perceived self-efficacy in health behavior research: conceptualisation, measurement and correlates. Psychology and Health. 2000;15:51–69. doi: 10.1080/08870440008400288. [DOI] [Google Scholar]
- Loo CM, Fairbank JA, Chemtob CM. Adverse race-related events as a risk factor for posttraumatic stress disorder in Asian American Vietnam veterans. Journal of Nervous and Mental Disease. 2005;193:455–463. doi: 10.1097/01.nmd.0000168239.51714.e6. [DOI] [PubMed] [Google Scholar]
- Luszczynska A, Benight CC, Cieslak R. Self-efficacy and health-related outcomes of collective trauma: A systematic review. European Psychologist. 2009;14:51–62. doi: 10.1027/1016-9040.14.1.51. [DOI] [Google Scholar]
- Pajares F, Schunk DH. Self-beliefs and school success: Self-efficacy, self-concept, and school achievement. In: Riding R, Rayner S, editors. International perspectives on individual differences. London: Ablex Publishing; 2001. pp. 239–265. [Google Scholar]
- Pinheiro J, Bates D, DebRoy S, Sarkar D, R Core Team nlme: Linear and Nonlinear Mixed Effects Models (Version 3.1-124) 2016 Retrieved from http://CRAN.R-project.org/packagenlme.
- R Core Team. R: A language and environment for statistical computing. Vienna, Austria: 2015. Retrieved from https://www.R-project.org/ [Google Scholar]
- Revelle W. psych: Procedures for Personality and Psychological Research (Version 1,5,8) Evanston, IL: Northwestern University; 2015. Retrieved from http://CRAN.R-project.org/packagepsych. [Google Scholar]
- Richardson LK, Frueh BC, Acierno R. Prevalence estimates of combat-related post-traumatic stress disorder: critical review. Australian & New Zealand Journal of Psychiatry. 2010;44:4–19. doi: 10.3109/00048670903393597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnurr PP, Friedman MJ, Engel CC, Foa EB, Shea MT, Chow BK, Turner C. Cognitive behavioral therapy for posttraumatic stress disorder in women: A randomized controlled trial. Jama. 2007;297(8):820–830. doi: 10.1001/jama.297.8.820. [DOI] [PubMed] [Google Scholar]
- Schwarzer R, Jerusalem M. Generalized Self-Efficacy scale. In: Weinman J, Wright S, Johnston M, editors. Measures in health psychology: A user’s portfolio Causal and control beliefs. Windsor, England: NFER-NELSON; 1995. pp. 35–37. [Google Scholar]
- Schwarzer R, Jerusalem M. Optimistic self-beliefs as a resource factor in coping with stress. In: Hobfoll SE, de Vries MW, editors. Extreme stress and communities: Impact and intervention. Netherlands: Springer; 1995. pp. 159–177. [Google Scholar]
- Sloan DM, Bovin MJ, Schnurr PP. Review of group treatment for PTSD. Journal of Rehabilitation Research & Development. 2012;49:689–702. doi: 10.1682/JRRD.2011.07.0123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith MW, Schnurr PP, Rosenheck RA. Employment outcomes and PTSD symptom severity. Mental Health Services Research. 2005;7:89–101. doi: 10.1007/s11020-005-3780-2. [DOI] [PubMed] [Google Scholar]
- Steenkamp MM, Litz BT, Hoge CW, Marmar CR. Psychotherapy for military-related PTSD: A review of randomized clinical trials. JAMA. 2015;314:489–500. doi: 10.1001/jama.2015.8370. [DOI] [PubMed] [Google Scholar]
- Walling SM, Suvak MK, Howard JM, Taft CT, Murphy CM. Race/ethnicity as a predictor of change in working alliance during cognitive behavioral therapy for intimate partner violence perpetrators. Psychotherapy. 2012;49:180. doi: 10.1037/a0025751. [DOI] [PubMed] [Google Scholar]
- Warner LM, Schwarzer R, Schüz B, Wurm S, Tesch-Römer C. Health-specific optimism mediates between objective and perceived physical functioning in older adults. Journal of behavioral medicine. 2012;35:400–406. doi: 10.1007/s10865-011-9368-y. [DOI] [PubMed] [Google Scholar]
- Weiss DS, Marmar CR, Schlenger WE, Fairbank JA, Jordan BK, Hough RL, Kulka RA. The prevalence of lifetime and partial post-traumatic stress disorder in Vietnam theater veterans. Journal of Trauma Stress. 1992;5:365–376. doi: 10.1007/BF00977234. [DOI] [Google Scholar]
- Wickham H. ggplot2: Elegant graphics for data analysis. New York, NY: Springer-Verlag; 2009. [Google Scholar]
- Wisco BE, Marx BP, Wolf EJ, Miller MW, Southwick SM, Pietrzak RH. Posttraumatic stress disorder in the US veteran population: results from the National Health and Resilience in Veterans Study. Journal of Clinical Psychiatry. 2014;75:1338–1346. doi: 10.4088/JCP.14m09328. [DOI] [PMC free article] [PubMed] [Google Scholar]


