Abstract
A holistic approach to understanding the relationship between diet, lifestyle and obesity is a better approach than studying single factors. This study presents the clustering of dietary and lifestyle behaviours to determine the association of these dietary-lifestyle patterns (DLPs) with adiposity, nutrition knowledge, gender and sociodemographic factors in teenagers. The research was designed as a cross-sectional study with convenience sampling. The sample consisted of 1549 Polish students aged 11–13 years. DLPs were identified with cluster analysis. Logistic regression modelling with adjustment for confounders was applied. Three dietary-lifestyle patterns were identified: Prudent-Active (29.3% of the sample), Fast-food-Sedentary (13.8%) and notPrudent-notFast-food-lowActive (56.9%). Adherence to Prudent-Active pattern (reference: notPrudent-notFast-food-lowActive) was 29% or 49% lower in 12-year-old or 13-year-old teenagers than in 11-year-old teenagers, respectively, and higher by 57% or 2.4 times in the middle or the upper tertile than the bottom tertile of the nutrition knowledge score. To the contrary, adherence to Fast-food-Sedentary (reference: notPrudent-notFast-food-lowActive) was lower by 41% or 58% in the middle or the upper tertile than the bottom tertile of the nutrition knowledge score, respectively. In Prudent-Active, the chance of central obesity (waist-to-height ratio ≥0.5) was lower by 47% and overweight/obesity was lower by 38% or 33% (depending on which standard was used: International Obesity Task Force, 2012: BMI (body mass index)-for-age ≥ 25 kg/m2 or Polish standards, 2010: BMI-for-age ≥ 85th percentile) when compared with the notPrudent-notFast-food-lowActive pattern. In Fast-food-Sedentary, the chance of central obesity was 2.22 times higher than the Prudent-Active pattern. The study identified a set of characteristics that decreased the risk of general and central adiposity in teenagers, which includes health-promoting behaviours related to food, meal consumption and lifestyle. Avoiding high-energy dense foods is insufficient to prevent obesity, if physical activity and the consumption frequency of health-promoting foods are low and breakfast and a school meal are frequently skipped. The results highlight the importance of the nutrition knowledge of teenagers in shaping their health-promoting dietary habits and active lifestyle to decrease adiposity risk and negative aspects of lower family affluence which promotes unhealthy behaviours, both related to diet and lifestyle.
Keywords: adolescent, cluster analysis, dietary patterns, food frequency questionnaire, nutrition knowledge, physical activity, screen time, sedentary behaviour, socioeconomic factors
1. Introduction
Adolescence is a period of important changes in physical, mental and social development. The awareness of one’s own sexuality and gender differences arises with regard to nutritional and caloric needs as well as physical abilities. The precise indication of the age at which changes start in the perception of oneself as an independent individual and food consumer is difficult, but the age of 10–12 years old is considered a breakthrough [1]. In general, girls tend to be more knowledgeable about food, nutrition and health and they exhibit more positive health- and food-related beliefs than boys [2,3,4]. On the other hand, boys spend more time being active, while girls spend more time socializing [5,6,7]. In this period, the establishment of health-promoting dietary and lifestyle habits plays a crucial role for achieving full growth potential and preventing diet-related diseases throughout the whole lifespan [8,9].
Progressive globalization, rapid changes in the ways of spending leisure time and increasing access to food create an adiposity-promoting environment with two main factors affecting the positive energy balance and obesity—sedentary lifestyle and an unhealthy diet rich in food whose consumption should be limited [9]. In real life, there is no single factor responsible for obesity. Moreover, adiposity-promoting behaviours can exist together with health-promoting behaviours because young people can engage in a variety of behaviours. It was reported by Gubbels et al. [10] that some boys combined unhealthy with health-promoting dietary and lifestyle behaviours. The pattern labelled as ‘Sports-Computer’ was characterized by a lower frequency of take-out meals and higher frequency of eating meals together, spending more time sitting and using a computer and also being physically active. A comprehensive approach, combining many environmental exposures is a better way to study the causes of obesity rather than to consider single behaviours influencing health [11]. Furthermore, by identifying factors associated with behavioural patterns, high-risk groups can be found for preventive interventions to stop the growth of obesity-related non-communicable diseases [12,13].
There have been several studies focused on the clustering of dietary-related and lifestyle-related behaviours in teenagers [2,10,13,14,15,16,17,18,19,20,21,22,23,24]. Two main patterns, one described as an ‘active and healthy lifestyle’ and the opposite as a ‘high screen time and unhealthy lifestyle’, were reported in school-age children from Spain [14], Finland [15] and nine European countries [25]. Some differences were reported between these patterns, depending on the region and the most characteristic dietary habit for the population under study. To date, few studies have considered selected dietary and/or lifestyle variables in relation to overweight or obesity [14,15,16,17,19,20,25]. The variables mainly referred to time spent in front of the screen, sleep duration, sleep quality, smoking, chosen physical activities, meal consumption or accompanying circumstances [10,14,15,17]. For dietary characteristics, only the consumption of fruit, vegetables and fruit juices was considered [17,18]. Thus, the dietary component of dietary-lifestyle patterns is weakly known in teenagers, especially in relation to obesity.
The aim of the study was the clustering of dietary and lifestyle behaviours to determine the association of these dietary-lifestyle patterns (DLPs) with adiposity, nutrition knowledge, gender and sociodemographic factors in teenagers.
2. Methods
2.1. Study Design and Participants
The analyses related to this paper were designed as a cross-sectional study with convenience sampling. Analyses were carried out on data from the ABC of Healthy Eating national multicentre project and the research was carried out in parallel with the project by academic researchers. The data was collected (2015–2016) by well-trained researchers from nine Polish universities, in ten locations covering the entire territory of Poland. More details on the study protocol, sample collection, sample size calculation and methods have been described previously [26].
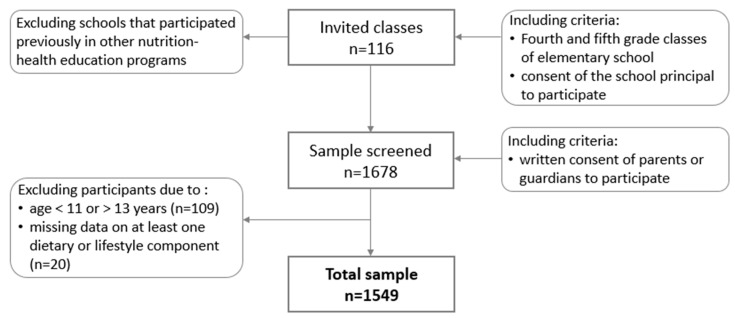
Recruitment was conducted in elementary schools from urban, sub-urban and rural areas. Students from fourth and fifth grade classes were invited to attend. In total, 116 classes were selected from across Poland (Figure 1). Initially, 1678 students were recruited. One hundred and twenty-nine participants were excluded from analyses: 109 participants because of an age below 11 years or above 13 years and 20 participants due to missing data on at least one dietary or lifestyle component. Finally, the study included 1549 teenagers 11–13 years old (48.5% boys).
Figure 1.
Sample collection.
2.2. Data Collection
Data related to diet, lifestyle, nutrition knowledge and socio-demographic factors were collected using a 50-item, short form of the food frequency questionnaire (SF-FFQ4PolishChildren) developed by Kowalkowska, Wadolowska and Hamulka for the ‘ABC of Healthy Eating’ project. The reproducibility of the short form of the FFQ was carried out in cooperation with researchers from 12 universities covering the entire territory of Poland (data not published, paper in preparation). In brief, the internal compatibility of the questionnaire was tested by 630 teenagers (11–15 years old). The questionnaire was completed by teenagers twice (test and retest after 2 weeks). For the measures under study, Fleiss’ Kappa was 0.30 to 0.89 and compatible classification of subjects (into the same category in test and retest) was 42.9% to 95.8%. Thus, the internal compatibility of the short form of the FFQ dedicated for teenagers was considered acceptable to very good.
The questionnaire was self-administered by teenagers in the classroom and supervised by well-trained researchers. Explanations were given if necessary. More details on this questionnaire were previously provided [26].
2.3. Dietary Data
Respondents specified their usual frequency of consumption within the 12 last months of: breakfast, a school meal and nine food items: dairy products, fish, vegetables, fruit, fruit or vegetable juices, fast foods, sweetened drinks, energy drinks and sweets. Breakfast and a school meal were both defined as consuming solid foods with or without beverages: breakfast—the first eating episode per day; a school meal—the second eating episode of the day while at school [27]. Drinking only beverages was not considered as breakfast or a school meal. More details on dietary data were previously provided [26]. In brief, respondents could choose one of the following:
four categories of breakfast consumption (number of days/week): 0/week, 1–3/week, 4–6/week, 7/week (every day);
four categories of school meal consumption (number of days/week): 0/week, 1–3/week, 3–4/week, 5/week (every school day);
seven categories for food frequency consumption: never or almost never, less than once a week, once a week, 2–4 times/week, 5–6 times/week, every day, several times a day; for further analysis, all frequencies of food consumption were converted into daily frequency (details in Table S1).
2.4. Lifestyle
Three measures of lifestyle were established—screen time, physical activity at school and physical activity at leisure time.
Screen time was assessed using the question ‘How much time do you spend watching TV or on the computer or in front of a computer on an average day of the week?’ The respondents could choose one of six answers: <2 h/day, 2 to <4 h/day, 4 to <6 h/day, 6 to <8 h/day, 8 to <10 h/day, ≥10 h/day. To express screen time in points, answers were converted into scores (1 to 6 points) (Table S1).
To describe physical activity at school or leisure time, the participants could choose one of three answers (low, moderate, vigorous). Many examples for each answer were given (Table S1). To express both physical activities in points, answers were converted into scores (both 1 to 3 points).
2.5. Dietary-Lifestyle Patterns
Dietary-lifestyle patterns were derived using cluster analysis. The input variables were 11 dietary (in times/day) and 3 lifestyle (in scores) components of DLPs. All input variables were standardized, using our own database, to achieve a mean equal to 0 and a standard deviation equal to 1. To identify the optimal number of clusters, the analysis was conducted several times. The K-means clustering algorithm was used and subjects were grouped based on the Euclidean distances. Finally, three clusters were selected (Table S1). The correctness of cluster identification and labelling was verified by comparing the components of DLPs between clusters with a one-way analysis of variance.
2.6. Nutrition Knowledge
Nutrition knowledge score was determined on the basis of eighteen questions. The respondents were asked about nutrition based on questions developed by Whati et al. [28] and adapted to Polish conditions and education. The correct answer was scored with 1 point, wrong or “I don’t know” answers or missing data were scored with 0 points. Points were summed up for each respondent (range 0 to 18 points). Based on tertile distribution, the respondents were divided into three nutrition knowledge categories: bottom (0–4 points), middle (5–7 points) and upper tertile (8–18 points).
2.7. Socioeconomic Status
Socioeconomic status was determined by the Family Affluence Scale (FAS). The FAS is a measure of material affluence derived from household characteristics. The scale is composed of four questions and was described by the Polish team of the Health Behaviour of School-aged Children (HBSC) study [29]. Answers were scored with 0 to 2 points. Some of the answers were scored with the same number of points, according to the points given below in brackets:
Question: ‘Does your family own a car, van or truck?’ Answers: no (0 points); yes, one (1 point); yes, two or more (2 points).
Question: ‘In recent years, how many times per year did you go away on holiday with your family?’ (necessary examples were given) Answers: not at all (0 points); once (1 point); twice (2 points); more than twice (2 points).
Question: ‘Do you have your own bedroom for yourself?’ Answers: no (0 points); yes (1 point).
Question: ‘How many computers or laptops or tablets does your family own?’ Answers: none (0 points); one (1 point); two (2 points); more than two (2 points).
The points were summed up for each respondent (range 0 to 7 points). Based on quartile distribution, the respondents were divided into three FAS categories: low (0–4 points; <25th quartiles), moderate (5–6 points) and high (7 points; ≥75th quartiles).
2.8. Adiposity Measures
The measurements of body weight (kg), height (cm) and waist circumference (WC, cm) were taken according to International Standards for Anthropometric Assessment (2001), all recoded with a precision of 0.1 kg or 0.1 cm, respectively. Professional devices and measuring tape were used (the same type across all research centres): for height—a portable telescopic measuring rod (SECA 220, Hamburg, Germany), for weight—an electronic digital scale (SECA 799, Hamburg, Germany), for waist circumference—a stretch-resistant tape that provides a constant 100 g tension (SECA 201, Hamburg, Germany). All measurements were taken in light clothing and without shoes. Body mass index (BMI, kg/m2) and waist-to-height ratio (WHtR) were calculated. To identify overweight/obesity (general adiposity), two standards were applied to categorize BMI-for-age with sex-specific cut-offs according to: (1) international standards (International Obesity Task Force, IOTF), 2012 (BMI ≥ 25 kg/m2) [30]; (2) Polish standards, 2010 (BMI ≥ 85th percentiles) [31]. As a central obesity measure (central adiposity), the waist-to-height ratio ≥ 0.5 was used [32].
2.9. Ethical Approval
This study was approved by the Bioethics Committee of the Faculty of Medical Sciences, University of Warmia and Mazury in Olsztyn in 2010, Resolution No. 20/2010. Informed consent was provided by teenagers’ parents or legal guardians.
2.10. Statistical Analysis
Categorical variables were presented as a sample percentage (%) and continuous variables as medians with an interquartile range. The differences between groups were verified with a chi-square test (categorical variables) or a Mann-Whitney test (continuous variables). Before statistical analysis, the normality of the distribution of the variables was checked with a Kolmogorov-Smirnov test.
Logistic regression modelling was applied to assess:
-
(i)
the adherence to chosen a DLP by sociodemographic factors and nutrition knowledge in respect to a referent DLP—the following categorical variables were used as predictors (independent variables): gender (girls, reference: boys), age (12 or 13 years, reference: 11 years), residence (urban, reference: rural), Family Affluence Scale (moderate or high, reference: low), nutrition knowledge score (middle or upper tertile, reference: bottom tertile);
-
(ii)
the chance to fall in the adiposity category (central obesity or overweight)—two opposite DPLs were used as predictors while others were used as a referent (i.e., in total, three various pairs of DPLs were analysed).
The odds ratios (ORs) and 95% confidence intervals (95% CIs) were calculated. Crude and adjusted models were created. Confounders included gender, age (years), residence (rural, urban), FAS (points) and nutrition knowledge score (points), excluding the modelled variable from confounders set, respectively. The significance of ORs was assessed by Wald’s statistics. For all tests, p < 0.05 was considered as significant. Analyses were performed using Statistica software (version 13.1 PL; StatSoft Inc., Tulsa, OK, USA; StatSoft, Krakow, Poland).
3. Results
3.1. Dietary-Lifestyle Patterns Characteristic
Three DLPs were identified, labelled as a Prudent-Active, Fast-food-Sedentary and notPrudent-notFast-food-lowActive (Table S1). Teenagers from the Prudent-Active pattern (29.3% of the sample) were characterised by the highest frequency consumption of vegetables, fruits, fruit or vegetable juices, dairy products and fish. Most of them consumed a breakfast or a school meal every day, had vigorous physical activity at school or leisure time and screen time <2 h/day (Table 1). This pattern was considered as health-promoting due to a diet consisting of foods recommended for consumption, regularity of meals consumption and active lifestyle. In contrast, teenagers from the Fast-food-Sedentary pattern (13.8%) were characterised by the highest frequency consumption of fast foods, sweetened beverages, energy drinks and sweets, and most of them skipped breakfast or a school meal and had screen time ≥10 h/day. This pattern was considered as adiposity-promoting due to a diet consisting of food recommended to be limited with irregular meals consumption and non-active lifestyle. The notPrudent-notFast-food-lowActive pattern was represented by most of the teenagers (56.9%) and did not have any special characteristics, although to some extent it was similar to two DPLs. The notPrudent-notFast-food-lowActive pattern was similar to the Fast-food-Sedentary pattern with a low frequency consumption of vegetables, fruits, fruit or vegetable juices and fish, frequent skipping of breakfast or a school meal as well as low physical activity at school or leisure time and was similar to the Prudent-Active pattern with a low frequency consumption of fast foods, sweetened beverages, energy drinks and sweets.
Table 1.
Sample characteristics by dietary-lifestyle patterns (% of the sample or median (interquartile range)).
| Variables | Total Sample | Prudent-Active | Fast-Food-Sedentary | notPrudent-notFast-Food-LowActive | p-Value |
|---|---|---|---|---|---|
| Sample size | 1549 | 454 | 214 | 881 | |
| Sample percentage | 100.0 | 29.3 | 13.8 | 56.9 | |
| Gender | *** | ||||
| boys | 48.5 | 41.9 | 59.3 | 49.3 | |
| girls | 51.5 | 58.1 | 40.7 | 50.7 | |
| Age (years) | * | ||||
| 11 | 16.6 | 20.0 | 13.6 | 15.6 | |
| 12 | 73.5 | 72.3 | 73.3 | 74.2 | |
| 13 | 9.9 | 7.7 | 13.1 | 10.2 | |
| Residence | ns | ||||
| rural | 40.4 | 43.6 | 39.7 | 38.9 | |
| urban | 59.6 | 56.4 | 60.3 | 61.1 | |
| Family Affluence Scale (points) | 6.0 (5.0–7.0) | 6.0 (5.0–7.0) | 5.0 (4.0–6.0) | 6.0 (5.0–6.0) | *** |
| Family Affluence Scale | *** | ||||
| low | 24.4 | 24.0 | 35.0 | 20.4 | |
| moderate | 49.9 | 52.0 | 43.5 | 48.6 | |
| high | 25.7 | 24.0 | 21.5 | 31.0 | |
| Nutrition knowledge score (points) | 6.0 (4.0–8.0) | 7.0 (5.0–9.0) | 5.0 (3.0–7.0) | 6.0 (4.0–8.0) | **** |
| Nutrition knowledge score (tertiles) | **** | ||||
| bottom | 30.9 | 32.3 | 49.1 | 19.6 | |
| middle | 39.2 | 40.5 | 35.5 | 38.3 | |
| upper | 29.9 | 27.2 | 15.4 | 42.1 | |
| Central obesity a | 12.1 | 7.8 | 15.2 | 13.6 | ** |
| BMI-for-age by international standards, 2012 b | * | ||||
| thinness | 9.4 | 8.3 | 9.1 | 10.1 | |
| normal weight | 66.0 | 72.4 | 66.5 | 62.6 | |
| overweight/obesity | 24.6 | 19.3 | 24.4 | 27.4 | |
| BMI-for-age by Polish standards, 2010 c | ns | ||||
| thinness | 3.7 | 3.9 | 4.6 | 3.3 | |
| normal weight | 74.5 | 78.6 | 73.1 | 72.6 | |
| overweight/obesity | 21.9 | 17.5 | 22.3 | 24.1 | |
| Components of dietary-lifestyle patterns | |||||
| Breakfast consumption (days/week) | **** | ||||
| <1 | 5.7 | 3.1 | 15.0 | 4.9 | |
| 1 to 3 | 11.8 | 8.6 | 18.7 | 11.8 | |
| 4 to 6 | 12.6 | 7.5 | 14.5 | 14.6 | |
| every day | 69.9 | 80.8 | 51.8 | 68.7 | |
| School meal consumption (days/week) | **** | ||||
| <1 | 5.7 | 1.1 | 10.7 | 6.8 | |
| 1 to 2 | 7.3 | 1.1 | 18.7 | 7.7 | |
| 3 to 4 | 18.1 | 12.1 | 19.2 | 20.9 | |
| every school day | 68.9 | 85.7 | 51.4 | 64.6 | |
| Frequency of consumption of (times/day) | |||||
| vegetables | 0.43 (0.43–1.00) | 1.00 (0.79–1.00) | 0.43 (0.14–0.79) | 0.43 (0.14–0.79) | **** |
| fruits | 0.79 (0.14–1.00) | 1.00 (0.79–2.00) | 0.43 (0.14–0.79) | 0.43 (0.14–0.79) | **** |
| fruit or vegetable juices | 0.43 (0.14–1.00) | 1.00 (0.43–1.00) | 0.43 (0.14–0.79) | 0.43 (0.14–0.79) | **** |
| dairy products | 0.79 (0.43–1.00) | 1.00 (0.79–1.00) | 0.79 (0.43–1.00) | 0.43 (0.43–0.79) | **** |
| fish | 0.06 (0.06–0.14) | 0.14 (0.06–0.43) | 0.06 (0.00–0.14) | 0.06 (0.06–0.14) | **** |
| fast foods | 0.06 (0.06–0.14) | 0.06 (0.00–0.06) | 0.43 (0.06–0.43) | 0.06 (0.06–0.06) | **** |
| sweetened beverages | 0.43 (0.06–0.43) | 0.14 (0.06–0.43) | 1.00 (0.43–2.00) | 0.14 (0.06–0.43) | **** |
| energy drinks | 0.00 (0.00–0.00) | 0.00 (0.00–0.00) | 0.06 (0.00–0.43) | 0.00 (0.00–0.00) | **** |
| sweets | 0.43 (0.14–0.79) | 0.43 (0.14–0.79) | 1.00 (0.43–1.00) | 0.43 (0.14–0.43) | **** |
| Screen time (h/day) | **** | ||||
| <2 | 46.2 | 59.3 | 15.4 | 46.9 | |
| 2 to <4 | 34.5 | 31.9 | 26.7 | 37.7 | |
| 4 to <6 | 11.5 | 5.9 | 26.6 | 10.7 | |
| 6 to <8 | 4.3 | 2.0 | 11.7 | 3.6 | |
| 8 to <10 | 1.4 | 0.7 | 7.0 | 0.5 | |
| ≥10 | 2.1 | 0.2 | 12.6 | 0.6 | |
| Physical activity at school d | **** | ||||
| low | 5.6 | 1.1 | 10.3 | 6.7 | |
| moderate | 48.7 | 36.1 | 50.0 | 54.9 | |
| high | 45.7 | 62.8 | 39.7 | 38.4 | |
| Physical activity at leisure time e | **** | ||||
| low | 9.6 | 2.2 | 21.5 | 10.4 | |
| moderate | 40.4 | 26.4 | 40.2 | 47.7 | |
| high | 50.0 | 71.4 | 38.3 | 41.9 |
Sample size may vary in variables due to missing data. a Central obesity identified as waist-to-height ratio ≥0.5 [32]. BMI: body mass index. BMI-for-age categorized with sex-specific cut-offs according to: b international standards (International Obesity Task Force, IOTF), 2012 [30] as follows: thinness BMI < 18.5 kg/m2; normal weight BMI = 18.5 to 24.9 kg/m2; overweight/obesity BMI ≥ 25 kg/m2, c Polish standards, 2010 [31] as follows: thinness BMI<5th percentiles; normal weight BMI = 5 to <85th percentiles; overweight/obesity BMI ≥ 85th percentiles. d Physical activity at school: low (most of the time in a sitting position, in class or on breaks), moderate (half the time in a sitting position and half the time in motion), vigorous (most of the time on the move or in classes related to high physical exertion). e Physical activity at leisure time: low (more time spent sitting, watching TV, in front of a computer, reading, light housework, short walks totalling up to 2 h a week), moderate (walking, cycling, gymnastics, working at home or other light physical activity performed 2–3 h/week), vigorous (cycling, running, working at home or other sports activities requiring physical effort over 3 h/week). Statistically significant: * p < 0.05, ** p < 0.01, *** p < 0.001, **** p < 0.0001; ns—not significant.
3.2. Association between Dietary-Lifestyle Patterns, Sociodemographic Factors and Nutrition Knowledge
The Prudent-Active pattern had the highest percentage of girls (58.1%) and 11-year-old teenagers (20.0%) and a higher nutrition knowledge score (median 7.0 points). In contrast, the Fast-food-Sedentary pattern had the highest percentage of boys (59.3%) and 13-year-old teenagers (13.1%), and the lowest nutrition knowledge score (median 5.0 points) and FAS (median 5.0 points) (Table 1). The notPrudent-notFast-food-lowActive pattern was represented by students with relatively higher nutrition knowledge scores (median 6.0 points) and FAS (median 6.0) and a similar percentage of girls (50.7%) and boys (49.3%).
The adherence to the Prudent-Active (adjusted models), when compared to the notPrudent-notFast-food-lowActive pattern, was lower by 29% (OR = 0.71, 95% CI: 0.52–0.96; p < 0.05) in 12-year-old and 49% (OR = 0.51, 95% CI: 0.31–0.84; p < 0.01) in 13-year-old than 11-year-old teenagers, and higher by 57% (OR = 1.57, 95% CI: 1.16–2.13; p < 0.01) in the middle and 2.4 times higher (OR = 2.40, 95% CI: 1.76–3.29; p < 0.0001) in the upper than the bottom tertile of the nutrition knowledge score (Table 2). The adherence to the Fast-food-Sedentary (adjusted models), when compared to the notPrudent-notFast-food-lowActive pattern, was lower by 40% (OR = 0.60, 95% CI: 0.42–0.86; p < 0.01) in moderate than low FAS, and lower by 41% (OR = 0.59, 95% CI: 0.42–0.82; p < 0.01) in the middle and 58% (OR = 0.42, 95% CI: 0.27–0.65; p < 0.001) in the upper than the bottom tertile of the nutrition knowledge score.
Table 2.
Odds ratios (95% confidence interval) for dietary-lifestyle patterns by sociodemographic factors and nutrition knowledge.
| Variables | Prudent-Active (Ref.: notPrudent-notFast-Food-LowActive) | Fast-Food-Sedentary (Ref.: notPrudent-notFast-Food-lowActive) | Fast-Food-Sedentary (Ref.: Prudent-Active) | |||
|---|---|---|---|---|---|---|
| Crude Model | Adjusted Model | Crude Model | Adjusted Model | Crude Model | Adjusted Model | |
| Girls (ref.: boys) | 1.35 * | 1.24 | 0.67 ** | 0.73 | 0.49 **** | 0.62 ** |
| (1.07; 1.70) | (0.98; 1.57) | (0.49; 0.90) | (0.54; 1.00) | (0.35; 0.69) | (0.43; 0.89) | |
| Age | ||||||
| 12 years (ref.: 11 years) | 0.76 | 0.71 * | 1.13 | 1.18 | 1.50 | 1.56 |
| (0.56; 1.02) | (0.52; 0.96) | (0.73; 1.75) | (0.75; 1.85) | (0.95; 2.38) | (0.94; 2.59) | |
| 13 years (ref.: 11 years) | 0.59 * | 0.51 ** | 1.47 | 1.56 | 2.51 ** | 3.20 ** |
| (0.37; 0.94) | (0.31; 0.84) | (0.82; 2.64) | (0.84; 2.88) | (1.31; 4.83) | (1.56; 6.54) | |
| Urban residence (ref.: rural) | 0.82 | 0.80 | 0.97 | 0.99 | 1.17 | 1.27 |
| (0.66; 1.04) | (0.63; 1.02) | (0.70; 1.33) | (0.73; 1.35) | (0.84; 1.64) | (0.88; 1.84) | |
| Family Affluence Scale | ||||||
| moderate (ref.: low) | 1.10 | 1.03 | 0.57 ** | 0.60 ** | 0.52 *** | 0.53 ** |
| (0.82; 1.48) | (0.76; 1.40) | (0.40; 0.81) | (0.42; 0.86) | (0.35; 0.77) | (0.34; 0.81) | |
| high (ref.: low) | 1.51 * | 1.32 | 0.61 * | 0.67 | 0.40 **** | 0.49 ** |
| (1.09; 2.10) | (0.94; 1.85) | (0.40; 0.92) | (0.44; 1.02) | (0.26; 0.63) | (0.29; 0.81) | |
| Nutrition knowledge score (tertiles) | ||||||
| middle (ref: bottom) | 1.56 ** | 1.57 ** | 0.58 ** | 0.59 ** | 0.37 **** | 0.38 **** |
| (1.15; 2.10) | (1.16; 2.13) | (0.41; 0.80) | (0.42; 0.82) | (0.25; 0.55) | (0.25; 0.57) | |
| upper (ref: bottom) | 2.55 **** | 2.40 **** | 0.37 ** | 0.42 *** | 0.15 **** | 0.16 **** |
| (1.88; 3.46) | (1.76; 3.29) | (0.18; 0.77) | (0.27; 0.65) | (0.09; 0.23) | (0.10; 0.26) | |
Odds ratios adjusted for confounders: gender, age (years), residence (categorical variable), Family Affluence Scale (points), nutrition knowledge score (points), excluding the modelled variable from confounders set, respectively. Statistically significant: * p < 0.05; ** p < 0.01; *** p < 0.001; **** p < 0.0001.
In the crude model, girls were more likely to adhere to the Prudent-Active pattern (OR = 1.35, 95% CI: 1.07–1.70; p < 0.05) and less likely to adhere to the Fast-food-Sedentary pattern (OR = 0.67, 95% CI: 0.49–0.90; p < 0.05), when compared to the notPrudent-notFast-food-lowActive pattern, but both associations disappeared after the adjustment.
The adherence to the Fast-food-Sedentary (adjusted models), when compared to the Prudent-Active pattern, was lower by 38% (OR = 0.62, 95% CI: 0.43–0.89; p < 0.01) in girls than boys, lower by 47% (OR = 0.53, 95% CI: 0.34–0.81; p < 0.01) in moderate and 51% (OR = 0.49, 95% CI: 0.29–0.81; p < 0.01) in high than low FAS, lower by 62% (OR = 0.38, 95% CI: 0.25–0.57; p < 0.0001) in the middle and 84% (OR = 0.16, 95% CI: 0.10–0.26; p < 0.0001) in the upper than the bottom tertile of the nutrition knowledge score, and 3.2 times higher (OR = 3.20, 95% CI: 1.56–6.54; p < 0.01) in 13-year-old than 11-year-old teenagers.
3.3. Association between Dietary-Lifestyle Patterns and Adiposity Measures
The Prudent-Active pattern had the lowest percentage of students with central obesity (7.8%) or overweight/obesity (17.5% or 19.3% depending on which standard was used) (Table 1). In contrast, the Fast-food-Sedentary pattern had the highest percentage of teenagers with central obesity (15.2%) and a relatively high percentage of overweight/obese students (22.3% or 24.4% depending on standard). The notPrudent-notFast-food-lowActive pattern had a relatively high percentage of students with central obesity (13.6%) and the highest percentage of overweight/obese students (24.1% or 27.4% depending on standard).
In the Prudent-Active adjusted models, when compared to the notPrudent-notFast-food-lowActive pattern, the chance of central obesity was lower by 47% (OR = 0.53, 95% CI: 0.35–0.80; p < 0.01) and overweight/obesity was lower by 33% (OR = 0.67, 95% CI: 0.50–0.91; p < 0.05) or 38% (OR = 0.62, 95% CI: 0.47–0.84; p < 0.01), depending on which standard was used (Table 3). No significant associations were found between adiposity measures and Fast-food-Sedentary, when compared to the notPrudent-notFast-food-lowActive pattern, in either the crude or adjusted models. In the Fast-food-Sedentary adjusted model, when compared to the Prudent-Active pattern, the chance of central obesity was 2.22 times higher (OR = 2.22, 95% CI: 1.24–3.97; p < 0.01).
Table 3.
Odds ratios (95% confidence interval) for adiposity measures by dietary-lifestyle patterns.
| Dietary-Lifestyle Patterns | Central Obesity a (Ref: Lack) | Overweight/Obesity (Ref: Normal Weight) | |
|---|---|---|---|
| International Standards, 2012 b | Polish Standards, 2010 c | ||
| Prudent-Active (ref.: notPrudent-notFast-food-lowActive) | |||
| Crude model | 0.54 ** | 0.61 *** | 0.67 ** |
| (0.36; 0.80) | (0.46; 0.81) | (0.50; 0.90) | |
| Adjusted model | 0.53 ** | 0.62 ** | 0.67 * |
| (0.35; 0.80) | (0.47; 0.84) | (0.50; 0.91) | |
| Fast-food-Sedentary (ref.: notPrudent-notFast-food-lowActive) | |||
| Crude model | 1.14 | 0.84 | 0.92 |
| (0.74; 1.76) | (0.58; 1.21) | (0.64; 1.34) | |
| Adjusted model | 1.08 | 0.82 | 0.92 |
| (0.69; 1.70) | (0.56; 1.19) | (0.63; 1.34) | |
| Fast-food-Sedentary (ref.: Prudent-Active) | |||
| Crude model | 2.12 ** | 1.37 | 1.38 |
| (1.25; 3.58) | (0.91; 2.07) | (0.90; 2.09) | |
| Adjusted model | 2.22 ** | 1.34 | 1.34 |
| (1.24; 3.97) | (0.86; 2.11) | (0.84; 2.13) | |
Odds ratios adjusted for confounders: gender, age (years), residence (categorical variable), Family Affluence Scale (points), nutrition knowledge score (points). a Central obesity identified as waist-to-height ratio ≥0.5 [32]. Overweight/obesity and normal weight identified as BMI-for-age categorized with sex-specific cut-offs according to: b international standards (International Obesity Task Force, IOTF), 2012 [30] as follows: overweight BMI ≥ 25 kg/m2, normal weight BMI = 18.5 to 24.9 kg/m2; c Polish standards, 2010 [31] as follows: overweight/obesity BMI ≥ 85th percentiles, normal weight BMI = 5 to <85th percentiles. Statistically significant: * p < 0.05, ** p < 0.01; *** p < 0.001.
4. Discussion
Among three dietary-lifestyle patterns derived with cluster analysis, two opposite patterns were revealed, Prudent-Active and Fast-food-Sedentary, representing approx. 29% and 14% of the sample, respectively. A lower prevalence of central obesity and overweight/obesity in the Prudent-Active than the notPrudent-notFast-food-lowActive pattern (covering approx. 57% of the sample) was found, as well as a higher prevalence of central obesity in the Fast-food-Sedentary than the Prudent-Active pattern. A higher chance of adherence to the Prudent-Active pattern was shown in teenagers with higher nutrition knowledge. In contrast, a lower chance of adherence to the Fast-food-Sedentary pattern was shown in teenagers with higher nutrition knowledge or higher family affluence. More girls adhered to the Prudent-Active pattern and more boys or older teenagers adhered to the Fast-food-Sedentary pattern. No associations between dietary-lifestyle patterns and residence were found.
We identified the health-promoting dietary-lifestyle pattern (the Prudent-Active) as being clearly associated with a lower risk of obesity. This pattern was multi-component-based, i.e., composed of many dietary and lifestyle factors, as follows: high frequency consumption of health-promoting foods (vegetables, fruits, fruit or vegetable juices, dairy products and fish), regular consumption of breakfast and a meal at school and vigorous physical activity at school and during leisure time. Due to the unique composition of the Prudent-Active pattern, it is not easy to compare our findings with others. For example, in school-age Spanish children a ‘high physical activity, low sedentary behaviour, longer sleep duration, healthier diet’ lifestyle pattern was identified [14]. In 13–15-year-old Finnish adolescents, a ‘healthy lifestyle’ pattern was identified which was related to longer sleep duration, sleep quality, higher physical activity and higher fruit and vegetable consumption [15], while in fourth grade American children an ‘active, healthy eating’ pattern was identified which was characterised by a higher chance of daily fruit and vegetable consumption, participation in team sports and physical activities, weight-loss exercises and a lower consumption of soda and both high-sugar and salty/high-fat snacks [33]. In regard to obesity risk, dietary and/or lifestyle patterns, the results reported previously are not completely compatible [10,19,20,25,34,35,36,37,38]. A meta-analysis by Mu et al. [35] provides evidence that higher adherence to the ‘prudent’ or ‘healthy’ dietary patterns decreased risk of overweight/obesity while a systematic review by Janssen et al. [36] showed that overweight was not associated with fruit and vegetable consumption. In a national sample of 9–13-year-old Greeks, the pattern combining more active lifestyle with more frequent meal consumption was negatively associated with body mass index [39]. Since our study showed a clear association between the Prudent-Active pattern and obesity, it strengthens the evidence that health-promoting dietary habits and more active lifestyle are associated with lower obesity risk. Moreover, the study indicates that preventing excessive adiposity depends on many protective factors existing together as a multi-component dietary-lifestyle pattern. Thus, a holistic approach taking together dietary and lifestyle characteristics is clearly justified. Our findings provide clear evidence that future research should take into account the clustering of dietary and lifestyle behaviours to study the impact of dietary-related and lifestyle-related factors on adiposity risk in teenagers.
The study revealed no difference in adiposity between the Fast-food-Sedentary and notPrudent-notFast-food-lowActive pattern (used as referent). This may result from some similarity of these patterns. The Fast-food-Sedentary pattern was characterised by the highest frequency consumption of high-energy dense foods (fast foods) and skipping breakfast or a school meal, and the highest screen time, while the notPrudent-notFast-food-lowActive pattern was characterised by the lowest frequency consumption of health-promoting foods and also high-energy dense foods, frequent skipping of breakfast or a school meal and low physical activity.
Firstly, our study is compatible with the evidence that unhealthy dietary habits and/or sedentary lifestyle are associated with higher adiposity [17,37,38,40,41,42,43,44,45]. It has been reported that higher body mass index or overweight/obesity are associated with a ‘westernized’ dietary pattern or a ‘high animal protein and fat’ pattern in Mexican adolescents [42] or an ‘obesogenic’ pattern in Brazilian [43,44] and Spain school-age children [45] or insufficient vigorous physical activity in 11–15-year-old Americans [37]. However, a systematic review by Janssen et al. [36] showed that sweets consumption frequency was lower in overweight youth than normal-weight youth, while overweight was not associated with soft drinks consumption or time spent on the computer. Secondly, the current findings suggest that avoiding foods which favour a positive energy balance (the notPrudent-notFast-food-lowActive pattern) is insufficient to prevent obesity if, at the same time, physical activity and the consumption of health-promoting foods are low and breakfast and school meals are frequently skipped. To our knowledge, this is the first time two adiposity-promoting multi-component dietary-lifestyle patterns were identified (the Fast-food-Sedentary and the notPrudent-notFast-food-lowActive), with both presenting a similar negative association with adiposity risk in teenagers.
Since the present study is the first study investigating the association between lifestyle-dietary patterns and nutrition knowledge in Polish teenagers, a comparison of our results with others is difficult. This study clearly showed that teenagers’ higher nutrition knowledge was strongly associated with higher adherence (by 60–140%) to the Prudent-Active pattern and lower adherence (by 40–60%) to the Fast-food-Sedentary pattern. It documents the wide context of the impact of nutrition knowledge on both dietary and lifestyle behaviours. In some studies, a positive association between parental nutrition knowledge and dietary habits or single lifestyle behaviours of school-age children has been reported [21,46]. Only one study related to school children’s nutrition knowledge showed the same positive relation [47]. Our results are consistent with the previous studies but show a new aspect of teenagers’ nutrition knowledge. It can be assumed that a gain in teenagers’ nutrition knowledge can improve their lifestyle, and dietary-lifestyle education may be addressed directly to teenagers and implemented in school classes. We also note the unique role of schools in implementing diet-related and lifestyle-related education programs and also giving teenagers a chance to participate in school physical education lessons which are well-tailored to their expectations.
The study documents that the Fast-Food-Sedentary pattern was associated with lower family affluence than the Prudent-Active pattern. As we identify patterns combining both dietary and lifestyle components, our results cannot be directly compared to other results, although we can discuss the results separately with reference to dietary patterns or lifestyle characteristics. Our finding supports the view that lower family affluence is a barrier to health-promoting dietary or lifestyle behaviours. For example, a worse diet that was poor in fruits, vegetables and/or rich in highly-processed foods and/or lower breakfast frequency consumption were more frequently identified among adolescents with lower socioeconomic status from different countries, for example, the USA [48], Lithuania [34,49], the Czech Republic [50] and France [51]. It is well-documented across the world that low-energy dense foods (e.g., vegetables and fruits) are more expensive and less affordable for lower income families, resulting in disparities in access to a healthy diet [50,52,53]. High-energy dense foods, such sweets and fast foods, are generally cheaper than low-energy dense foods, so their consumption is higher in children from poorer families, especially with lower parental education [54,55]. In regard to lifestyle, positive aspects of higher family affluence were reported when children were given greater access to extracurricular physical activity and participation in team sports [56,57]. However, one contradictory finding was described. Canadian children 7–11-year-old from less affluent families were less likely to use a computer, but also less likely to participate in vigorous physical activities [58]. We hypothesize that the Fast-Food-Sedentary pattern of Polish teenagers is a result of time spent in front of the TV screen, as a cheap model of spending leisure time [22,59].
We found the clear association of gender with dietary-lifestyle patterns. This result is in line with previously reported results in regard to dietary habits, but inconsistent in regard to lifestyle. Most of the studies reported health-promoting dietary habits, but lower physical activity in girls than boys [2,3,4]. However, one study covering Polish adolescents from less urbanized regions showed that the ‘westernized Polish’ dietary pattern was more often represented by the boys who spent their free time being sedentary [60]. Our study demonstrated that girls had higher adherence to health-promoting dietary habits in combination with having a more active lifestyle (the Prudent-Active pattern) and, in contrast, boys had a higher adherence to the unhealthy dietary habits in combination with having a sedentary lifestyle (the Fast-Food-Sedentary pattern). To our knowledge, for the first time, vigorous physical activity in girls was demonstrated. This can be explained by the clustering of dietary and lifestyle behaviours in one analysis. It allowed new aspects of teenagers’ behaviours to be identified in respect to gender, compared to studies considering only single factors of diet or lifestyle or only focused on dietary patterns or lifestyle patterns [61,62,63]. Our results require further research to confirm these findings across a wide age range of Polish students as well as in other European teenagers.
The study confirmed the relationship between age and behaviours, showing the worse dietary habits (the Fast-food Sedentary pattern) in older teenagers (13-year-olds in comparison to 11-year- olds). Younger teenagers (around the age of 10–12) are still under strong influence from parents and partake in family meals, but this tendency declines as they get older [38]. Older teenagers have a lower preference for fruit, vegetables and other health-promoting foods [64,65], and are at higher risk of unhealthy dietary habits (e.g., often choose to eat fast foods, processed foods and sweets) and their diet migrated with age from a healthy to an industrialized food pattern [25]. This results from greater freedom in making food choices and the greater pressure from multiple sources around themselves, including peers [8,9].
An unexpected finding of the study was the lack of association of dietary-lifestyle patterns with residence. Across the world, rural residence is linked with lower parental education and lower family affluence and all these factors taken together result in lower socioeconomic status [66]. It is well-documented that rural residence was associated with worse dietary habits and lower adherence to dietary recommendations [67,68]. Moreover, more vigorous physical activity in adolescents from the countryside than urban areas has been reported [69]. There are two possible explanations. The clustering of many factors and/or reverse causation of some of them could have caused a lack of significant association between dietary-lifestyle patterns and residence. Secondly, progressive globalization could blur the differences between the city and the countryside through supermarket expansion, increased access to food and a change in the ways of spending leisure time [9]. Such changes could equalize the living conditions of Polish teenagers. This statement has been confirmed by several studies. About ten years ago Lazarou and Kalavana [70] found significant differences between Cypriot children from urban and rural areas due to the consumption of more traditional dishes and less fast-food by rural children. Recently, in Polish adolescents from less urbanized regions, it was shown that rural residence was not a barrier to a well-composed diet [60]. Similarly, no impact of place of residence on dietary patterns in children from public schools in Brazil was observed [24].
Strengths and Limitations
The strength of the study is its relatively large sample (above 1500). Although the sample was not randomly selected, it covers the entire territory of Poland and widely reflects the demographic-social diversity of Poles, thus forming a good basis for generalizations. The ratio of rural/urban area in our sample (40.4/59.6) was similar to the Polish population (39.9/60.1) and the ratio of boys/girls in our sample (48.5/51.5) was also similar to the population of 10–14-year-old Polish adolescents (51.2/48.7) [71]. We applied simple measures of general and central adiposity which are appropriate for a comprehensive assessment of high adiposity levels and are widely used in large epidemiological studies, despite having some interpretative limitations [14,15,32,63].
The main limitation of the study is the use of a questionnaire to collect dietary and lifestyle data. The questionnaire contained a short list of food items (nine items) and simple questions related to sedentary and active behaviours. There is evidence of many advantages to the use of brief tools, for example, high reproducibility of simple questions, the possibility to rank respondents into categories of habitual food consumption and identify dietary patterns, the possibility to assess compliance with dietary or lifestyle recommendations as well as low cost and quick, easy administration [72]. Future studies should consider the use of a long form of the FFQ (containing more food items) to fully describe the teenagers’ dietary behaviours. However, to date, there has been no validated long form of FFQ developed for Polish children or adolescents. Secondly, the use of a questionnaire causes some uncertainty due to social desirability bias. As females are more likely to provide more socially acceptable answers, it cannot be ruled out that girls under study could have reported their own dietary and lifestyle behaviours as being closer to the recommendations than in reality [73,74,75].
5. Conclusions
Using a holistic approach, the study identified a set of characteristics decreasing the risk of general and central adiposity in teenagers, which includes health-promoting behaviours. Clear benefits in reducing adiposity risk were found in teenagers who frequently consumed health-promoting foods (vegetables, fruits, fruit or vegetable juices, dairy products and fish), regularly consumed breakfast and a meal at school and were vigorously active at school and leisure time (the Prudent-Active pattern). On the other hand, adiposity-promoting was a dietary-lifestyle pattern characterized by lower frequency consumption of both health-promoting foods and fast foods, frequent skipping of breakfast or a school meal and low physical activity. Such a pattern increased obesity risks similarly to another pattern characterized by the frequent consumption of fast foods and a sedentary lifestyle. Therefore, avoiding high-energy dense foods is insufficient to prevent obesity, if physical activity and frequency consumption of health-promoting foods are low and breakfast and a school meal are frequently skipped.
The results highlight the importance of the nutrition knowledge of teenagers in shaping their health-promoting dietary habits and active lifestyle to decrease adiposity risk, and negative aspects of lower family affluence which promotes unhealthy behaviours related to both diet and lifestyle. The study supports evidence that health-promoting activities should be directed to Polish teenagers from less affluent families and should be particularly focused on increasing the consumption of health-promoting foods, improving regular meal consumption and spending more time actively. Further studies may explore gender-related dietary-lifestyle patterns to confirm our result that girls tended to display a complex of health-promoting behaviours related to diet and lifestyle, in contrast to boys who tended to display a complex of unhealthy behaviours by eating more fast foods and spending more sedentary time in front of a screen.
Acknowledgments
Thanks are expressed to the participants for their contributions to the study and the academic researchers from: Warsaw University of Life Sciences (WULS-SGGW), Gdynia Maritime University, Faculty of Health Sciences, Medical University in Bialystok, Faculty of Physical Education and Sport in Biala Podlaska of the Josef Pilsudski University of Physical Education in Warsaw, University of Agriculture in Krakow, University of Life Sciences in Lublin, University of Life Sciences in Poznan, University of Warmia and Mazury in Olsztyn, Wroclaw University of Environmental and Life Sciences.
Supplementary Materials
The following are available online at http://www.mdpi.com/2072-6643/10/12/1988/s1, Table S1. Standardized means of components of dietary-lifestyle patterns identified with cluster analysis.
Author Contributions
L.W., J.H. and J.K. were responsible for the conception and design of the main study. J.H., A.P. and E.C.-S. were involved in the funding acquisition in respect to the project and managing of the project. L.W., J.H. and J.K. were responsible for the design and data interpretation for this particular paper. J.K. was responsible for the data cleaning and statistical analysis for the main study and this particular paper. K.W. was responsible for the statistical analysis related to implementation of BMI-for-age to calculate overweight prevalence. L.W. and M.K. were responsible for data interpretation for this particular paper and for writing the manuscript. J.H., J.K., M.K., R.B.-K., E.C.-S., W.K. and A.P. were responsible for data collection of the main study. J.H. was responsible for revising the manuscript critically for important intellectual content. The manuscript was revised by all co-authors.
Funding
The study was financially supported by Carrefour Foundation (Agreement ABC No.1/2014; Agreement ABC No. 2/2016) and each scientific centre from sources of the Polish Ministry of Sciences and Higher Education.
Conflicts of Interest
The authors declare no conflicts of interest. The funding sponsors had no role in the study design, data collection, analysis or interpretation of the data, the writing of the manuscript or the decision to publish the results.
Data availability statement
Due to ethical restrictions and participant confidentiality, data cannot be made publicly available. However, data from the ABC of Healthy Eating study are available upon request, for researchers who meet the criteria for access to confidential data. Data requests can be sent to ABC of the Healthy Eating study coordinator (Jadwiga Hamulka).
References
- 1.Baxter S.D. Cognitive processes in children’s dietary recalls: Insight from methodological studies. Eur. J. Clin. Nutr. 2009;63:19–32. doi: 10.1038/ejcn.2008.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fitzgerald A.F., Heary C., Nixon E., Kelly C. Gender differences in factors influencing dietary patterns among Irish children and adolescents. Proc. Nutr. Soc. 2010;69:E385. doi: 10.1017/S0029665110002466. [DOI] [Google Scholar]
- 3.Marshall S., Jones D., Ainsworth B., Reis J., Levy S., Macera C. Race/ethnicity, social class, and leisure-time physical inactivity. Med. Sci. Sports Exercise. 2007;39:44–51. doi: 10.1249/01.mss.0000239401.16381.37. [DOI] [PubMed] [Google Scholar]
- 4.Marques A., da Costa F.C. Levels of physical activity of urban adolescents according to age and gender. Int. J. Sports Sci. 2013;3:23–27. [Google Scholar]
- 5.Ferrari K.E., Olds T.S., Walters J.L. All the stereotypes confirmed: Differences in how Australian boys and girls use their time. Health Educ. Behav. 2012;39:589–595. doi: 10.1177/1090198111423942. [DOI] [PubMed] [Google Scholar]
- 6.Klomsten A.T., Marsh H.W., Skaalvik E.M. Adolescents’ perceptions of masculine and feminine values in sport and physical education: A study of gender differences. Sex Roles. 2005;52:625–636. doi: 10.1007/s11199-005-3730-x. [DOI] [Google Scholar]
- 7.Jago R., Fox K.R., Page A.S., Brockman R., Thompson L. Physical activity and sedentary behaviour typologies of 10-11 years old. Int. Behav. Nutr. Phys. Act. 2011;7:8–49. doi: 10.1186/1479-5868-7-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ranjit N., Evans M.H., Byrd-Williams C., Evans A.E., Hoelscher D.M. Dietary and activity correlates of sugar-sweetened beverage consumption among adolescents. Pediatrics. 2010;126:e754–e761. doi: 10.1542/peds.2010-1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Popkin B.M., Adair L.S., Ng S.W. Global nutrition transition and the pandemic of obesity in developing countries. Nutr. Rev. 2012;70:3–21. doi: 10.1111/j.1753-4887.2011.00456.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gubbels J.S., Kremers S.P., Stafleu A., Goldbohm R.A., de Vries N.K., Thijs C. Clustering of energy balance-related behaviors in 5-year-old children: Lifestyle patterns and their longitudinal association with weight status development in early childhood. Int. J. Behav. Nutr. Phys. Act. 2012;9:77–91. doi: 10.1186/1479-5868-9-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.United States Department of Agriculture (USDA) A Series of Systematic Reviews on the Relationship between Dietary Patterns and Health Outcome. [(accessed on 4 July 2018)]; Available online: https://www.cnpp.usda.gov/2014.
- 12.Hu H.B. Dietary pattern analysis: A new direction in nutrition epidemiology. Curr. Opin. Lipidol. 2002;13:3–9. doi: 10.1097/00041433-200202000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Rachel E., Laxer R.E., Brownson R.C., Dubin J.A., Cooke M., Chaurasia A., Leatherdale S.T. Clustering of risk-related modifiable behaviours and their association with overweight and obesity among a large sample of youth in the COMPASS study. BMC Public Health. 2017;17:102. doi: 10.1186/s12889-017-4034-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pérez-Rodrigo C., Gil A., González-Gross M., Ortega R.M., Serra-Majem L., Varela-Moreiras G., Aranceta-Bartrina J. Clustering of dietary patterns, lifestyles, and overweight among spanish children and adolescents in the ANIBES study. Nutrients. 2016;8:11. doi: 10.3390/nu8010011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nuutinen T., Lehto E., Ray C., Roos E., Villberg J., Tynjälä J. Clustering of energy balance-related behaviours, sleep, and overweight among Finnish adolescents. Int. J. Public Health. 2017;62:929–938. doi: 10.1007/s00038-017-0991-4. [DOI] [PubMed] [Google Scholar]
- 16.Mandic S., Bengoechea E.G., Coppell K.J., Spence J.C. Clustering of (Un)healthy behaviors in adolescents from Dunedin, New Zealand. Am. J. Health Behav. 2017;41:266–275. doi: 10.5993/AJHB.41.3.6. [DOI] [PubMed] [Google Scholar]
- 17.Dupuy M., Godeau E., Vignes C., Ahluwalia N. Socio-demographic and lifestyle factors associated with overweight in a representative sample of 11–15 years old in France: Results from the WHO-Collaborative Health Behaviour in School-aged Children (HBSC) cross-sectional study. BMC Public Health. 2011;11:442. doi: 10.1186/1471-2458-11-442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Eisenburg L.K., Corpeleijn E., van Sluijs E.M.F., Atkin A.J. Clustering and correlates of multiple health behaviours in 9–10 year old children. PLoS ONE. 2014;9:e99498. doi: 10.1371/journal.pone.0099498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lioret S., Touvier M., Lafay L., Volatier J.C., Maire B. Dietary and physical activity patterns in French children are related to overweight and socioeconomic status. J. Nutr. 2008;138:101–107. doi: 10.1093/jn/138.1.101. [DOI] [PubMed] [Google Scholar]
- 20.Ambrosini G.L., Emmett P.M., Northstone K., Howe L.D., Tilling K., Jebb S.A. Identification of a dietary pattern prospectively associated with increased adiposity during childhood and adolescence. Int. J. Obes. 2012;36:1299–1305. doi: 10.1038/ijo.2012.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hinnig P.F., Monteiro J.S., Altenburg de Assis M.A., Levy R.B., Peres M.A., Perazi F.M., Porporatti A.L., De Luca Santo G. Dietary patterns of children and adolescents from high, medium and low human development countries and associated socioeconomic factors: A systematic review. Nutrients. 2018;10:436. doi: 10.3390/nu10040436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jodkowska M., Oblacińska A., Tabak I. Patterns of physical activity and sedentary behaviors among 13-year-olds in Poland. Pediatria Polska. 2013;88:508–513. doi: 10.1016/j.pepo.2013.08.008. [DOI] [Google Scholar]
- 23.Northstone K., Smith A.D.A.C., Newby P.K., Emmett P.M. Longitudinal comparisons of dietary patterns derived by cluster analysis in 7- to 13-year-old children. Br. J. Nutr. 2012;109:1–9. doi: 10.1017/S0007114512004072. [DOI] [PubMed] [Google Scholar]
- 24.Corrêa R.S., Vencato P.H., Rockett F.C., Bosa V.L. Dietary patterns: Are there differences between children and adolescents? Ciênc Saúde Coletiva. 2017;22:553–562. doi: 10.1590/1413-81232017222.09422016. [DOI] [Google Scholar]
- 25.Te Velde S.J., De Bourdeaudhuij I., Thorsdottir I., Rasmussen M., Hagströmer M., Klepp K.I., Brug J. Patterns in sedentary and exercise behaviors and associations with overweight in 9-14-year-old boys and girls—a cross-sectional study. BMC Public Health. 2007;7:16. doi: 10.1186/1471-2458-7-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hamulka J., Wadolowska L., Hoffman M., Kowalkowska J., Gutkowska K. The effect of an education program on nutrition knowledge, attitudes toward nutrition, diet quality, lifestyle, and body composition in Polish teenagers. The ABC of Healthy Eating project: Design, protocol, and methodology. Nutrients. 2018;10:1439. doi: 10.3390/nu10101439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pereira M.A., Erickson E., McKee P., Schrankler K., Raatz S.K., Lytle L.A., Pellegrini A.D. Breakfast frequency and quality may affect glycemia and appetite in adults and children. J. Nutr. 2011;141:163–168. doi: 10.3945/jn.109.114405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Whati L.H., Senekal M., Steyn N.P., Nel J.H., Lombard C., Norris S. Development of a reliable and valid nutritional knowledge questionnaire for urban South African adolescents. Nutrition. 2005;21:76–85. doi: 10.1016/j.nut.2004.09.011. [DOI] [PubMed] [Google Scholar]
- 29.Mazur J. Family affluence scale—validation study and suggested modification. Hygeia Public Health. 2013;48:211–217. [Google Scholar]
- 30.Cole T.J., Lobstein T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatric Obes. 2012;7:284–294. doi: 10.1111/j.2047-6310.2012.00064.x. [DOI] [PubMed] [Google Scholar]
- 31.Kułaga Z., Litwin M., Tkaczyk M., Palczewska I., Zajączkowska M., Zwolińska D., Krynicki T., Wasilewska A., Moczulska A., Morawiec-Knysak A., et al. Polish 2010 growth references for school-aged children and adolescents. Eur. J. Pediatrics. 2011;170:599–609. doi: 10.1007/s00431-010-1329-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ashwell M., Gunn P., Gibson S. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: Systematic review and meta-analysis. Obes. Rev. 2012;13:275–286. doi: 10.1111/j.1467-789X.2011.00952.x. [DOI] [PubMed] [Google Scholar]
- 33.Huh J., Riggs N.R., Spruijt-Metz D., Chou C.P., Huang Z., Pentz M. Identifying patterns of eating and physical activity in children: A latent class analysis of obesity risk. Obesity. 2011;19:652–658. doi: 10.1038/oby.2010.228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Smetanina N., Albaviciute E., Babinska V., Karinauskiene L., Albertsson-Wikland K., Petrauskiene A., Verkauskiene R. Prevalence of overweight/obesity in relation to dietary habits and lifestyle among 7–17 years old children and adolescents in Lithuania. BMC Public Health. 2015;15:1001. doi: 10.1186/s12889-015-2340-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mu M., Xu L.F., Hu D., Wu J., Bai M.J. Dietary Patterns and Overweight/Obesity: A Review Article. Iran. J. Public Health. 2017;46:869–876. [PMC free article] [PubMed] [Google Scholar]
- 36.Janssen I., Katzmarzyk P.T., Boyce W.F., Vereecken C., Mulvihill C., Roberts C., Currie C., Pickett W., Health Behaviour in School-Aged Children Obesity Working Group Comparison of overweight and obesity prevalence in school-aged youth from 34 countries and their relationships with physical activity and dietary patterns. Obes. Rev. 2005;6:123–132. doi: 10.1111/j.1467-789X.2005.00176.x. [DOI] [PubMed] [Google Scholar]
- 37.Patrick K., Norman G.J., Calfas K.J., Sallis J.F., Zabinski M.F., Rupp J., Cella J. Diet, physical activity, and sedentary behaviors as risk factors for overweight in adolescence. Arch. Pediatrics Adolesc. Med. 2004;158:385–390. doi: 10.1001/archpedi.158.4.385. [DOI] [PubMed] [Google Scholar]
- 38.Oellingrath I.M., Svendsen M.V., Brantsaeter A.L. Tracking of eating patterns and overweight – a follow-up study of Norwegian schoolchildren from middle childhood to early adolescence. Nutr. J. 2011;6:106–118. doi: 10.1186/1475-2891-10-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Moschonis G., Kalliora A.C., Costarelli V., Papandreou Ch., Koutoukidis D., Lionis Ch., Chrousos G.P., Manios Y. Identification of lifestyle patterns associated with obesity and fat mass in children: The Healthy Growth Study. Public Health Nutr. 2013;17:614–624. doi: 10.1017/S1368980013000323. on behalf of the Healthy Growth Study Group. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cutler G.J., Flood A., Hannan P.J., Slavin J.L., Neumark-Sztainer D. Association between major patterns of dietary intake and weight status in adolescents. Br. J. Nutr. 2012;108:349–356. doi: 10.1017/S0007114511005435. [DOI] [PubMed] [Google Scholar]
- 41.Wadolowska L., Kowalkowska J., Czarnocinska J., Jezewska-Zychowicz M., Babicz-Zielinska E. Comparing dietary patterns derived by two methods and their associations with obesity in Polish girls aged 13–21 years: The cross-sectional GEBaHealth study. Perspect. Public Health. 2017;137:182–189. doi: 10.1177/1757913916679859. [DOI] [PubMed] [Google Scholar]
- 42.Gutiérrez-Pliego E., del Socorro Camarillo-Romero L., Montenegro-Morales E.P., José L.G. Dietary patterns associated with body mass index (BMI) and lifestyle in Mexican adolescents. BMC Public Health. 2016;16:850. doi: 10.1186/s12889-016-3527-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Santos N.H., Fiaccone R.L., Barreto M.L., Silva L.A., Silva R. Association between eating patterns and body mass index in a sample of children and adolescents in Northeastern Brazil. Cadernos de Saúde Pública. 2014;30:2235–2245. doi: 10.1590/0102-311X00178613. [DOI] [PubMed] [Google Scholar]
- 44.Pinho M.G.M., Aadami F., Benedet J., Vasconcelos F. Association between screen time and dietary patterns and overweight/obesity among adolescents. Rev. Nutr. 2017;30:377–389. doi: 10.1590/1678-98652017000300010. [DOI] [Google Scholar]
- 45.Aranceta J., Perez-Rodrigo C., Ribas L., Serra-Majem L. Sociodemographic and lifestyle determinants of food patterns in Spanish children and adolescents: The enKid study. Eur. J. Clin. Nutr. 2003;57:40–44. doi: 10.1038/sj.ejcn.1601813. [DOI] [PubMed] [Google Scholar]
- 46.Grosso G., Mistretta A., Turconi G., Cena H., Roggi C., Galvano F. Nutrition knowledge and other determinants of food intake and lifestyle habits in children and young adolescents living in a rural area of Sicily, South Italy. Public Health Nutr. 2012;16:1–10. doi: 10.1017/S1368980012003965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gower J.R., Moyer-Mileur L.J., Wilkinson R.D., Slater H., Jordan K.C. Validity and reliability of a nutrition knowledge survey for assessment in elementary school children. J. Am. Diet Assoc. 2010;110:452–456. doi: 10.1016/j.jada.2009.11.017. [DOI] [PubMed] [Google Scholar]
- 48.Cutler G.J., Flood A., Hannan P., Neumark-Sztainer D. Multiple sociodemographic and socioenvironmental characteristics are correlated with major patterns of dietary intake in adolescents. J. Am. Diet Assoc. 2011;111:230–240. doi: 10.1016/j.jada.2010.10.052. [DOI] [PubMed] [Google Scholar]
- 49.Petrauskienė A., Žaltauskė V., Albavičiūtė E. Family socioeconomic status and nutrition habits of 7–8 year old children: Cross-sectional Lithuanian COSI study. Ital. J. Pediatrics. 2015;41:34. doi: 10.1186/s13052-015-0139-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Voráčová J., Sigmund E., Sigmundová D., Kalman M. Family affluence and the eating habits of 11- to 15-year-old Czech adolescents: HBSC 2002 and 2014. Int. J. Environ. Res. Public Health. 2016;13:1034. doi: 10.3390/ijerph13101034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Darmon N., Drewnowski A. Contribution of food prices and diet cost to socioeconomic disparities in diet quality and health: A systematic review and analysis. Nutr. Rev. 2015;73:643–660. doi: 10.1093/nutrit/nuv027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Darmon N., Drewnowski A. Does social class predict diet quality? Am. J. Clin. Nutr. 2008;87:1107–1117. doi: 10.1093/ajcn/87.5.1107. [DOI] [PubMed] [Google Scholar]
- 53.Fismen A.S., Samdal O., Torsheim T. Family affluence and cultural capital as indicators of social inequalities in adolescent’s eating behaviours: A population-based survey. BMC Public Health. 2012;12:1036. doi: 10.1186/1471-2458-12-1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Anzman S.L., Rollins B.Y., Birch L.L. Parental influence on children’s early eating environments and obesity risk: Implications for prevention. Int. J. Obes. 2010;34:1116–1124. doi: 10.1038/ijo.2010.43. [DOI] [PubMed] [Google Scholar]
- 55.Fielding-Singh P., Wan J. Table talk: How mothers and adolescents across socioeconomic status discuss food. Soc. Sci. Med. 2017;187:49–57. doi: 10.1016/j.socscimed.2017.06.016. [DOI] [PubMed] [Google Scholar]
- 56.Kantomaa M.T., Tammelin T.H., Näyhä S., Taanila A.M. Adolescents’ physical activity in relation to family income and parents’ education. Prev. Med. 2007;44:410–415. doi: 10.1016/j.ypmed.2007.01.008. [DOI] [PubMed] [Google Scholar]
- 57.Drenowatz C.D., Eisenmann J.C., Pfeiffer K.A., Welk G., Heelan K., Gentile D., Walsh D. Influence of socio-economic status on habitual physical activity and sedentary behavior in 8- to 11-year old children. BMC Public Health. 2010;10:214. doi: 10.1186/1471-2458-10-214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.McCormack G.R., Hawe P., Perry R., Blackstaffe A. Associations between familial affluence and obesity risk behaviours among children. Paediatrics Child Health. 2011;16:19–24. doi: 10.1093/pch/16.1.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sas-Nowosielski K., Ogrodnik J. Stages of exercise change and screen time in adolescents. New Educ. Rev. 2012;30:281–291. [Google Scholar]
- 60.Długosz A. Wzory żywienia, niepożądane skutki zdrowotne, sytuacja społeczno-ekonomiczna i styl życia młodzieży z mniej zurbanizowanych regionów Polski (Dietary Patterns, Adverse Health Outcomes, Socioeconomic Situation and Lifestyle of Adolescents from Less Urbanized Regions of Poland) UWM; Olsztyn, Poland: 2017. pp. 1–108. [Google Scholar]
- 61.Vašíčková J., Groffik D., Frömel K., Chmelík F., Wasowicz W. Determining gender differences in adolescent physical activity levels using IPAQ long form and pedometers. Ann. Agric. Environ. Med. 2013;20:749–755. [PubMed] [Google Scholar]
- 62.Spencer R.A., Rehman L., Kirk S.F.L. Understanding gender norms, nutrition, and physical activity in adolescent girls: A scoping review. Int. J. Behav. Nutr. Phys. Act. 2015;12:6–16. doi: 10.1186/s12966-015-0166-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wadolowska L., Kowalkowska J., Lonnie M., Czarnocinska J., Jezewska-Zychowicz M., Babicz-Zielinska E. Associations between physical activity patterns and dietary patterns in a representative sample of Polish girls aged 13–21 years: A cross-sectional study (GEBaHealth Project) BMC Public Health. 2016;16:698. doi: 10.1186/s12889-016-3367-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ball K., MacFarlane A., Crawford D., Savige G., Andrianopoulos N., Worsley A. Can social cognitive theory constructs explain socio-economic variations in adolescent eating behaviours? A mediation analysis. Health Educ. Res. 2009;24:496–506. doi: 10.1093/her/cyn048. [DOI] [PubMed] [Google Scholar]
- 65.Larson N.I., Neumark-Sztainer D.R., Story M.T., Wall M.M., Harnack L.J., Eisenberg M.E. Fast food intake: Longitudinal trends during the transition to young adulthood and correlates of intake. J. Adolesc. Health. 2008;43:79–86. doi: 10.1016/j.jadohealth.2007.12.005. [DOI] [PubMed] [Google Scholar]
- 66.Blakely F., Dunnagan T., Haynes G., Moore S., Pelicane S. Moderate physical activity and its relationship to select measures of a healthy. Diet J. Rural Health. 2004;20:160–165. doi: 10.1111/j.1748-0361.2004.tb00023.x. [DOI] [PubMed] [Google Scholar]
- 67.Liu H., Jones S.J., Sun H., Probst J.C., Merchant A., Cavicchia P. Diet, physical activity, and sedentary behaviors as risk factors for childhood obesity: An urban and rural comparison. Child Obes. 2012;8:440–448. doi: 10.1089/chi.2011.0090. [DOI] [PubMed] [Google Scholar]
- 68.Ettienne-Gittens R., McKyer E.L., Odum M. Rural versus urban Texas WIC participants’ fruit and vegetable consumption. Am. J. Health Behav. 2013;37:130–140. doi: 10.5993/AJHB.37.1.15. [DOI] [PubMed] [Google Scholar]
- 69.Regis M.F., de Oliveira L.M.F.T., dos Santos A.R.M., Leonidio A.C.R., Diniz P.R.B., de Freitas C.M.S.M. Urban versus rural lifestyle in adolescents: Associations between environment, physical activity levels and sedentary behavior. Einstein. 2016;14:461–467. doi: 10.1590/s1679-45082016ao3788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lazarou C., Kalavana T. Urbanization influences dietary habits of Cypriot children: The CYKIDS study. Int. J. Public Health. 2009;54:69–77. doi: 10.1007/s00038-009-8054-0. [DOI] [PubMed] [Google Scholar]
- 71.GUS, Area and Population in Territorial Cross-Section in 2018. [(accessed on 10 November 2018)]; Available online: https://stat.gov.pl/download/gfx/portalinformacyjny/en/defaultaktualnosci/3286/3/23/1/population_size_and_structure_and_vital_statistics_in_poland_31-12-2017.pdf.
- 72.Dietary assessment FAO 2018 Food and Agriculture Organization Dietary Assessment: A Resource Guide to Method Selection and Application in Low Resource Settings. [(accessed on 15 November 2018)]; Available online: http://203.187.160.134:9011/www.fao.org/c3pr90ntc0td/3/i9940en/I9940EN.pdf.
- 73.Kaminska O., Foulsham T. Understanding Sources of Social Desirability Bias in Different Modes: Evidence from Eye-tracking. [(accessed on 15 November 2018)];2013 Available online: https://www.iser.essex.ac.uk/research/publications/working-papers/iser/2013-04.pdf.
- 74.Klesges L.M., Baranowski T., Beech B., Cullen K., Murray D.M., Rochon J., Pratt C. Social desirability bias in self-reported dietary, physical activity and weight concerns measures in 8- to 10-year-old African-American girls: Results from the Girls Health Enrichment Multisite Studies (GEMS) Prev. Med. 2004;38:78–87. doi: 10.1016/j.ypmed.2003.07.003. [DOI] [PubMed] [Google Scholar]
- 75.Novotny J.A., Rumpler W.V., Judd J.T., Riddick H.W., Rhodes D., McDowell M., Briefel R. Diet interviews of subject pairs: How different persons recall eating the same foods. J. Am. Diet Assoc. 2001;101:1189–1193. doi: 10.1016/S0002-8223(01)00291-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Due to ethical restrictions and participant confidentiality, data cannot be made publicly available. However, data from the ABC of Healthy Eating study are available upon request, for researchers who meet the criteria for access to confidential data. Data requests can be sent to ABC of the Healthy Eating study coordinator (Jadwiga Hamulka).