Abstract
Background: Colorectal cancers (CRC) with brain metastases (BM) are scarcely described. The main objective of this study was to determine the molecular profile of CRC with BM. Methods: We included 82 CRC patients with BM. KRAS, NRAS, BRAF and mismatch repair (MMR) status were investigated on primary tumors (n = 82) and BM (n = 38). ALK, ROS1, cMET, HER-2, PD-1, PD-L1, CD3 and CD8 status were evaluated by immunohistochemistry, and when recommended, by fluorescence in situ hybridization. Results: In primary tumors, KRAS, NRAS and BRAF mutations were observed in 56%, 6%, and 6% of cases, respectively. No ROS1, ALK and cMET rearrangement was detected. Only one tumor presented HER-2 amplification. Molecular profiles were mostly concordant between BM and paired primary tumors, except for 9% of discordances for RAS mutation. CD3, CD8, PD-1 and PD-L1 expressions presented some discordance between primary tumors and BM. In multivariate analysis, multiple BM, lung metastases and PD-L1+ tumor were predictive of poor overall survival. Conclusions: CRCs with BM are associated with high frequency of RAS mutations and significant discordance for RAS mutational status between BM and paired primary tumors. Multiple BM, lung metastases and PD-L1+ have been identified as prognostic factors and can guide therapeutic decisions for CRC patients with BM.
Keywords: brain metastases, colorectal cancer, KRAS mutation, PD-L1, tumor infiltrating lymphocytes
1. Introduction
Brain metastases (BM) from colorectal cancer (CRC) are rare with an incidence ranging from 0.6 to 3.2% and are associated with a poor prognosis with an overall survival (OS) of about 5.0 months [1,2]. Patients with BM from CRC present a specific clinical profile with predominant rectosigmoid primary tumor location and lung metastases [3,4,5,6]. Nevertheless, the molecular profile of BMs from CRC has only been partially explored [7,8]. Some small series have suggested a high rate of KRAS mutation in CRC with BM, but no study has evaluated complete RAS (KRAS and NRAS), BRAF and mismatch repair (MMR) status [1].
In metastatic CRC (mCRC), molecular profiles of liver and lung metastases have already been tested and revealed a high concordance between the metastases and paired primary tumor (PPT) (95–100%) [9]. Brastianos et al., by performing a whole-exome sequencing of 86 BM and PPT from various sites, reported 53% of discordances in genetic profile, and found actionable mutations (EGFR, HER-2 and PI3K/AKT/mTOR pathways) in BM that were not detected in PPT [10]. However, only four CRCs were analyzed. Therefore, it is of major interest to evaluate molecular abnormalities of CRC with BM in a larger cohort.
The main objective of this study was to evaluate the molecular profile of CRC with BM. The secondary objectives were to evaluate the concordance of molecular profiles between BM and their PPT and to determine the prognostic factors of CRC patients with BM.
2. Results
2.1. Patient and Tumor Characteristics
Eighty-two CRC patients with BM were included, mostly radiologically confirmed (n = 44/82), with a median follow-up of 45.1 months (95% Confidence Interval (CI) 26.6–45.5 months). Median age at CRC diagnosis was 64.0 years and most of the patients were male (63%) (Table 1).
Table 1.
Clinical characteristics of patients, primary tumors and brain metastases (BM).
| Characteristics | Patients (n = 82) |
|---|---|
| Age at primary tumor diagnostic, years | |
| Median (range) | 64 (35–85) |
| Gender, n (%) | |
| Male | 52 (63) |
| Female | 30 (37) |
| Site of primary tumor, n (%) | |
| Ascending colon | 19 (23) |
| Descending colon | 24 (29) |
| Rectum | 35 (42) |
| Bifocal tumor | 5 (6) |
| Tumor grade, n (%) | |
| Well or moderately differentiated | 61 (87) |
| Poorly differentiated | 9 (13) |
| Missing | 12 |
| Stage at initial CRC diagnostic, n (%) | |
| I | 4 (5) |
| II | 13 (16) |
| III | 26 (32) |
| IV | 39 (47) |
| Primary tumor resection, n (%) | |
| No | 11 (13) |
| Yes | 71 (87) |
| ECOG performance status at BM diagnosis, n (%) | |
| < 2 | 43 (54) |
| ≥ 2 | 36 (46) |
| Missing | 3 |
| Number of BM, n (%) | |
| Single | 43 (52) |
| Multiple | 39 (48) |
| Site of BM, n (%) | |
| Supratentorial | 46 (56) |
| Subtentorial | 18 (22) |
| Both | 18 (22) |
| Delay between BM and CRC diagnosis, n (%) | |
| Synchronous | 8 (10) |
| Metachronous | 74 (90) |
| ECM at BM diagnosis, n (%) | |
| No | 11 (14) |
| Yes | 70 (86) |
| Missing | 1 |
| Lung metastases at BM diagnosis, n (%) | |
| No | 23 (28) |
| Yes | 58 (72) |
| Missing | 1 |
| Liver metastases at BM diagnosis, n (%) | |
| No | 45 (56) |
| Yes | 36 (44) |
Abbreviations: BM, brain metastasis(es); CRC, colorectal cancer; ECM, extracranial metastasis(es); ECOG, Eastern Cooperative Oncology Group score.
2.2. Molecular and Pathological Profiles of Colorectal Cancer with Brain Metastases
In primary tumors (n = 82), RAS mutations were observed in 62% of cases with 56% of KRAS mutations and 6% of NRAS mutations (Table 2). KRAS mutations in codon 12 of exon 2 were observed in 48% and the most frequent were G12D and G12V. BRAF mutation was observed in 6%. Concerning BM (n = 38), RAS was mutated in 85% of cases (74% of KRAS mutations and 11% of NRAS mutations) and BRAF in 5%. Both primary tumors and BM were mostly MMR-proficient (pMMR) (95%). Four patients had dMMR tumors, one patient had a Lynch syndrome (MSH2 germline mutation) and the three others patients had sporadic dMMR tumors.
Table 2.
Molecular profile of primary tumors and brain metastases.
| Molecular Status | Primary Tumors (n = 82) | BM (n = 38) |
|---|---|---|
| KRAS status | ||
| Wild-type, n (%) | 35 (44) | 10 (26) |
| Mutant, n (%) | 44 (56) | 28 (74) |
| KRAS exon 2 at codon 12 | ||
| G12D | 14 (18) | 9 (23) |
| G12V | 14 (18) | 8 (21) |
| G12A | 5 (6) | 3 (8) |
| G12S | 3 (4) | 0 |
| G12C | 1 (1) | 1 (3) |
| G12R | 1 (1) | 1 (3) |
| KRAS exon 2 at codon 13 | ||
| G13D | 2 (3) | 3 (8) |
| G13R | 1 (1) | 1 (3) |
| KRAS exon 3 at codon 61 | 3 (4) | 2 (5) |
| KRAS exon 4 at codon 146 | 0 | 0 |
| Missing, n | 3 | 0 |
| NRAS status | ||
| Wild-type, n (%) | 74 (94) | 34 (89) |
| Mutant, n (%) | 5 (6) | 4 (11) |
| NRAS exon 2 at codon 12 or 13 | 1 (1) | 1 (3) |
| NRAS exon 3 at codon 61 | 4 (5) | 3 (8) |
| Missing, n | 3 | 0 |
| BRAF exon 15 at codon 600 | ||
| Wild-type, n (%) | 74 (94) | 36 (95) |
| Mutant, n (%) | 5 (6) | 2 (5) |
| Missing, n (%) | 3 | 0 |
| MMR status | ||
| pMMR, n (%) | 70 (95) | 36 (95) |
| dMMR, n (%) | 4 (5) | 2 (5) |
| Missing, n | 8 | 0 |
| cMET expression | ||
| Negative (0, 1+, 2+/3+ with FISH negative), n (%) | 76 (100) | 37 (100) |
| Positive (2+, 3+ with FISH positive), n (%) | 0 | 0 |
| Missing, n | 6 | 1 |
| HER-2 expression | ||
| Negative (0, 1+, 2+ with FISH negative), n (%) | 74 (99) | 37 (100) |
| Positive (2+ with FISH positive, 3+), n (%) | 1 (1) | 0 |
| Missing, n | 7 | 1 |
| ALK expression | ||
| Negative (0, 1+/2+/3+ with FISH negative), n (%) | 76 (100) | 37 (100) |
| Positive (1+/2+/3+ with FISH positive), n (%) | 0 | 0 |
| Missing, n (%) | 6 | 1 |
| ROS1 expression | ||
| Negative (0, 1+/2+/3+ with FISH negative), n (%) | 74 (100) | 37 (100) |
| Positive (1+/2+/3+ with FISH positive), n (%) | 0 | 0 |
| Missing, n | 8 | 1 |
| PD-1 expression | ||
| Negative, n (%) | 64 (86) | 37 (100) |
| Positive, n (%) | 10 (14) | 0 |
| Missing, n | 8 | 1 |
| PD-L1 expression | ||
| Negative, n (%) | 68 (93) | 35 (95) |
| Positive, n (%) | 5 (7) | 2 (5) |
| Missing, n | 9 | 1 |
| CD3 expression | ||
| Median rate, % (range) | 30 (0–80) | 11 (0–60) |
| Missing, n | 11 | 1 |
| CD8 expression | ||
| Median rate, % (range) | 11 (0–70) | 3 (0–50) |
| Missing, n | 7 | 2 |
Abbreviations: IHC, Immunohistochemistry; FISH, Fluorescence in situ hybridization; MMR, Mismatch repair; pMMR, Proficient Mismatch Repair; dMMR, Deficient Mismatch Repair.
No primary tumor overexpressed ROS1 protein according to immunohistochemistry (IHC) analysis. ALK IHC 1+ was detected in six primary tumors, but was negative by Fluorescence in situ hybridization (FISH) analysis. Concerning HER-2 IHC, three primary tumors were positive, but HER-2 amplification was confirmed by FISH only for one sample. cMET positive staining was detected by IHC in 61% of primary CRC, but none was confirmed by FISH. Concerning BM, ROS1, ALK and HER-2 staining were all negative (score 0). cMET positive staining was detected in 84% of BM, but none was confirmed by FISH.
Ten primary tumors (14%) were programmed death-1 positive (PD-1+), but no BM. Five primary tumors (7%) and two BMs (5%) were programmed death-ligand 1 positive (PD-L1+). Among the five PD-L1+ primary tumors, three were MMR-deficient (dMMR) and two were pMMR. The median percentage of CD3 and CD8 lymphocyte infiltrates were 30% and 11% in primary tumors, 11% and 3% in BM respectively. The mean percentages of CD3 and CD8 lymphocyte infiltrates in primary tumors were 46% and 38% in dMMR tumors and 33% and 11% in pMMR tumors (p = 0.23 for CD3 and p < 0.01 for CD8) respectively. The mean percentages of CD3 and CD8 lymphocyte infiltrates in primary tumors were 49% and 41% in PD-L1+ tumors and 33% and 12% in PD-L1- tumors (p = 0.09 for CD3 and p < 0.01 for CD8), respectively.
2.3. Concordance of Molecular and Pathological Profiles between Brain Metastases and Their Paired Primary Tumors
The molecular profiles of BM were compared with their PPT (Table 3), when available (n = 35). Discordances in RAS and BRAF status were observed in four patients (11%), three for RAS and one for BRAF. In each case, PPT was wild-type and BM was mutated. According to IHC evaluation, PPT and BM were discordant for cMET in nine cases (28%). However, all cases were negative according to FISH analyses.
Table 3.
Molecular and pathological profiles of brain metastases and paired primary tumors.
| Brain Metastases | |||
|---|---|---|---|
| RAS status | |||
| Primary tumors | Wild-type | Mutant | Total |
| Wild-type, n (%) | 6 (17) | 3 (9) | 9 (26) |
| Mutant, n (%) | 0 | 26 (74) | 26 (74) |
| Total, n (%) | 6 (17) | 29 (83) | 35 |
| BRAF status | |||
| Primary tumors | Wild-type | Mutant | Total |
| Wild-type, n (%) | 33 (94) | 1 (3) | 34 (97) |
| Mutant, n (%) | 0 | 1 (3) | 1 (3) |
| Total, n (%) | 33 (94) | 2 (6) | 35 |
| MMR status | |||
| Primary tumors | pMMR | dMMR | Total |
| pMMR, n (%) | 30 (94) | 0 | 30 (94) |
| dMMR, n (%) | 0 | 2 (6) | 2 (6) |
| Total, n (%) | 30 (94) | 2 (6) | 32 |
| HER-2 expression | |||
| Primary tumors | Negative | Positive | Total |
| Negative, n (%) | 35 (100) | 0 | 35 (100) |
| Positive, n (%) | 0 | 0 | 0 (0) |
| Total, n (%) | 35 (100) | 0 (0) | 35 |
| cMET expression (IHC) | |||
| Primary tumors | Negative | Positive | Total |
| Negative, n (%) | 4 (13) | 7 (22) | 11 (34) |
| Positive, n (%) | 2 (6) | 19 (59) | 21 (66) |
| Total, n (%) | 6 (19) | 26 (81) | 32 |
| PD-1 expression | |||
| Primary tumors | Negative | Positive | Total |
| Negative, n (%) | 30 (94) | 0 | 30 (94) |
| Positive, n (%) | 2 (6) | 0 | 2 (6) |
| Total, n (%) | 32 (100) | 0 | 32 |
| PD-L1 expression | |||
| Primary tumors | Negative | Positive | Total |
| Negative, n (%) | 29 (91) | 2 (6) | 31 (97) |
| Positive, n (%) | 1 (3) | 0 | 1 (3) |
| Total, n (%) | 30 (94) | 2 (6) | 32 |
| CD3 expression | Primary tumor | Brain metastases | |
| Median rate, % (range) | 34 (0–80) | 15 (0–60) | |
| CD8 expression | Primary tumor | Brain metastases | |
| Median rate, % (range) | 10 (0–70) | 3 (0–50) | |
Abbreviations: IHC, immunohistochemistry; MMR, Mismatch repair; pMMR, Proficient Mismatch Repair; dMMR, Deficient Mismatch Repair.
Concerning PD-1+ tumor, discordance was observed in two paired samples (6%). We found three discordances for PD-L1 status (9%). Median percentages of CD3+ and CD8+ lymphocytes were significantly more important in PPT (34% and 10%) compared to BM (15% and 3%) (both p < 0.01). In addition, there was a positive correlation between levels of CD8+ infiltrates in BM and PTT (p = 0.01), but not for CD3+ infiltrates (p = 0.40).
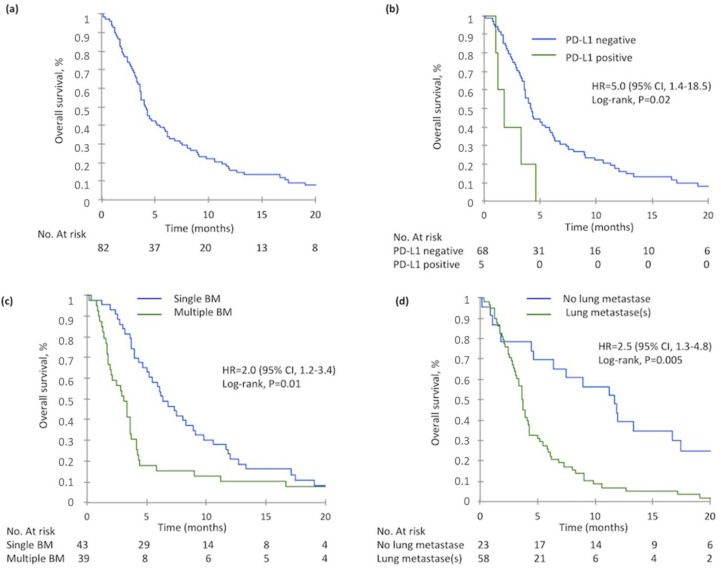
2.4. Overall Survival
79 patients died at the time of data analysis. Median Overall Survival (OS) from BM diagnosis was 4.1 months (95%CI 3.6–5.4 months) (Figure 1). Median OS from diagnosis of metastatic disease was 28.6 months (95%CI 18.0–35.5 months). Age, BRAF mutation, PD-L1+ tumors, Eastern cooperative oncology group (ECOG) performance status ≥ 2, multiple BM and lung metastases were significantly associated with poor OS in univariate analysis (Table 4). In multivariate analysis, PD-L1+ primary tumors, multiple BM and lung metastases were significantly associated with poor OS.
Figure 1.
Overall Survival at brain metastasis(es) diagnosis in the whole population and according to PD-L1 expression, number of brain metastasis(es) and the presence of lung metastasis(es): (a) Overall survival of 82 patients at BM diagnosis, (b) Overall survival according to PD-L1 expression in primary tumor, (c) Overall survival according to the BM number, (d) Overall survival according to the presence of lung metastasis(es) at BM diagnosis.
Table 4.
Univariate and multivariate analysis of overall survival in patients with brain metastases from colorectal cancer.
| Univariate Analysis | Multivariate Analysis | |||||
|---|---|---|---|---|---|---|
| Variables | n | Median (Months) | p Value | HR | 95% CI | p Value |
| Gender (n = 82) | 0.79 * | 0.38 | ||||
| Male | 52 | 3.9 | 1 | |||
| Female | 30 | 4.3 | 0.8 | 0.5–1.4 | ||
| Age at BM diagnosis (n = 82) | 82 | 0.02 * | 1.0 | 1.0–1.0 | 0.62 | |
| Site of primary tumor (n = 82) | 0.23 | |||||
| Ascending colon | 20 | 4.5 | ||||
| Descending colon | 24 | 5.9 | ||||
| Rectum | 35 | 2.9 | ||||
| Tumor grade (n = 70) | 0.05 | |||||
| Well or moderately differentiated | 61 | 3.9 | ||||
| Poorly differentiated | 9 | 4.6 | ||||
| RAS status (n = 79) | 0.65 | |||||
| Wild-type | 30 | 3.6 | ||||
| Mutant | 49 | 4.3 | ||||
| BRAF status (n = 79) | 0.03 * | 0.76 | ||||
| Wild-type | 74 | 4.2 | 1 | |||
| Mutant | 5 | 3.3 | 1.2 | 0.3–4.2 | ||
| MMR status (n = 74) | 0.68 | |||||
| pMMR | 70 | 4.1 | ||||
| dMMR | 4 | 4.0 | ||||
| PD-1 expression (n = 74) | 0.79 | |||||
| Negative | 64 | 4.2 | ||||
| Positive | 10 | 3.6 | ||||
| PD-L1 expression (n = 73) | 0.009 * | 0.02 | ||||
| Negative | 68 | 4.2 | 1 | |||
| Positive | 5 | 1.8 | 5.0 | 1.4–18.5 | ||
| CD3 expression (n = 71) | 71 | 0.08 | ||||
| CD8 expression (n = 75) | 75 | 0.45 | ||||
| ECOG performance status (n = 79) | 0.0003 * | 0.07 | ||||
| <2 | 43 | 7.3 | 1 | |||
| ≥2 | 36 | 3.2 | 1.8 | 1.0–3.4 | ||
| Number of BM (n = 82) | 0.003 * | 0.01 | ||||
| Single | 43 | 6.3 | 1 | |||
| Multiple | 39 | 3.1 | 2.0 | 1.2–3.4 | ||
| Lung metastases at BM diagnosis (n = 81) | 0.0003 * | 0.005 | ||||
| No | 23 | 11.7 | 1 | |||
| Yes | 58 | 3.6 | 2.5 | 1.3–4.8 | ||
| Liver metastases at BM diagnosis (n = 81) | ||||||
| No | 45 | 4.3 | 0.31 | |||
| Yes | 36 | 3.7 | ||||
Abbreviations: HR, hazard ratio; BM, brain metastasis(es); 95% CI, 95% confidence interval; ECOG, Eastern Cooperative Oncology Group score. * variables included in multivariate analysis
3. Discussion
In our study, molecular features of CRC with BM were in accordance with rates observed in all-comers mCRC except for RAS mutations that appear to be higher than rates commonly observed in mCRC [11]. Surprisingly, we observed some differences of molecular profiles between BM and PPT, especially for RAS and PD-L1 status. Finally, we identified multiple BM, lung metastases and PD-L1 positivity as prognostic factors in patients with BM from CRC.
As compared to all-comers mCRC patients, in our study, patients with BM from CRC seemed to be younger, with more frequent rectal tumor and lung metastases. Other studies had previously identified frequent lung metastases and young age as particular characteristics of CRC patients with BM [1]. In accordance with the literature, the interval between primary tumor diagnosis and BM diagnosis reached more than 30 months, probably because the brain is a late sanctuary site for chemo-resistant tumor cells [12]. Moreover, the rate of RAS mutation was high (62%) in comparison to what is usually observed in mCRC (≈50%) [11]. This observation is in agreement with other studies, which also showed that KRAS mutations could be a predictive factor of BM [13]. The rates of CD3 and CD8 tumor-infiltrating lymphocytes (TILs) observed in our study were in accordance with the rates observed in other mCRC cohorts [14,15]. Also, our study showed comparable proportions of PD-L1+ and PD-1+ tumors, mostly in dMMR tumors, when compared with other studies in the literature [16,17].
There is a high discrepancy observed between IHC and FISH results for cMET status in our study, as described in the literature. In a recent study using IHC, 57.5% of CRC were found to be positive for MET protein IHC, but only 4.4% were FISH positive [18]. Overexpression of MET has been established in CRC [19], with MET protein levels ranging from 12% to 81% (median, 61%) [20]. Zeng et al. established that MET gene amplification was present in 2% of localized CRC tumors, 9% of tumors with distant metastases, and 18% of liver metastases using the quantitative PCR/ligase detection reaction technique [21]. In our study cMET positive staining was detected by IHC in 61% of primary CRC, but none was confirmed by FISH.
Comparison of BM and PPT has been scarcely explored in mCRC, but discordances have been observed between BM and PPT in lung and breast cancers [10]. In our study, we found a higher rate of RAS mutation in BM (85%) compared to PPT (62%) and three discordant cases (9%). El-Deiry et al. determined KRAS status from 2510 primary CRC and 30 BM from CRC and found significantly higher rates of KRAS mutation in BM (65%) compared to the primary tumor (45%), but the samples were not paired [13]. In another cohort of 41 BM with PPT, two cases presented discordant KRAS status [22]. Discordances between PPT and BM could be explained by intra and/or inter-tumoral heterogeneity, as we recently demonstrated in CRC [23]. Indeed, if CRC patients have had BM surgery, RAS should be evaluated in this sample in order to define treatment (anti-EGFR). BM are more frequently observed in breast and gastric cancers with HER-2 overexpression compared to HER-2 negative tumors [24,25], which does not seem to be the case in mCRC.
To our knowledge, no previous study has compared the expression of PD-1, PD-L1, CD3 and CD8 in paired primary CRC and BM. In BM, we identified low rates of immune infiltrates compared to PPT. These results were concordant with the study by Harter et al., which showed low rates of PD-L1+ and PD-1+ tumors (1%) and low rates of CD3+ (3%) and CD8+ T-cells (2%) in BM samples from CRC [26]. In the literature, whatever the tumor type, less immune infiltrate is observed in BM compared to PPT [27]. Moreover, in our study, there was some discordance between PD-1 and PD-L1 status in BM compared to PPT. Recent studies have identified BM as a sanctuary site for tumor cells to escape immunosurveillance [28]. Up until now, there has been only limited data concerning immune checkpoint inhibitor efficacy in BM, but no clinical evidence of lesser efficacy compared to other metastatic sites [29]. Nevertheless, it is important to consider the spatial heterogeneity of the tumor immune microenvironment in BM compared to PPT, especially PD-L1 expression, when cancer patients are treated with PD-1 or PD-L1 inhibitors.
Overall survival of patients with BM from CRC is poor. It is important to identify prognostic factors to help therapeutic decision-making. Some prognostic classifications exist, but most are not designed specifically for patients with mCRC. A recent Italian retrospective study identified age, performance status, BM site and BM number as prognostic factors associated with OS of CRC patients with BM [30]. In our study, we found no association between RAS or BRAF status and OS. However, OS of patients with PD-L1 negative primary tumors was significantly higher than patients with PD-L1+ tumors. This result should be interpreted with caution considering the small number of patients with PDL1+ tumors, the potential tumor heterogeneity and the absence of standard cut-off for this marker. High PD-L1 expression has been associated with longer OS in pMMR mCRC in some studies, but not all [31]. In addition, in lung cancer with BM, PD-L1 expression has been associated with worse OS [32]. Our study highlighted two other prognostic markers, single BM and the absence of lung metastases that had already been reported for patients with BM whatever the primary tumor.
The main limitation of the study is its retrospective nature, but there are few missing data (≈10%). Results concerning the comparison of BM and PPT should be confirmed given the small size of our study, since most patients did not have surgery of BM. Nevertheless, it is the largest study up until now concerning the molecular profile of CRC with BM.
4. Materials and Methods
4.1. Patients
All patients with BM from CRC, diagnosed from 2001 to 2016, were identified in our institution using our clinical report database. All patients with a histologically confirmed CRC and histologically or radiologically confirmed BM by computed tomography scan (CT-scan) and/or magnetic resonance imaging (MRI) were included. BM was defined as synchronous if they occur within three months of mCRC diagnosis. Our institution’s Ethics Committee approved the study (DC-2008-565).
4.2. Molecular Analyses
Genomic DNA from tumor samples was extracted using Maxwell 16 FFPE Plus LEV DNA purification kit© (Promega, Charbonnières-les-Bains, France). KRAS/NRAS codons 12, 13, 61, 146 and BRAF (V600E) were analyzed by pyrosequencing (TheraScreenPyroKit©, Qiagen, Hilden, Germany) using homemade specific primers as previously described [33]. MMR status was determined by microsatellite analysis using MD1641 Promega kit© (Promega).
4.3. Tissue Microarray Construction and Immunohistochemistry
Formalin-fixed paraffin-embedded blocks were used for tissue microarray (TMA) construction using four biopsy cores of 1 mm diameter per tumor in the tumor center (MTA Booster© version 1.01, Alphelys, Paris, France).
IHCwas carried out on paraffin-embedded 3-μm thick TMA sections with antibodies directed against ALK, ROS1, cMet, HER-2, PD-1, PD-L1, CD3 and CD8 according to the manufacturer’s instructions.
IHC is a prescreening test commonly used for the detection of ALK rearrangement in lung carcinoma [34] and the same scoring was used here. Immunostaining scores were assigned from 0 to 3. For ALK cytoplasmic staining, a score of 1+ (weak), 2+ (moderate) or 3+ (strong) in more than 10% of tumor cells and for ROS1 staining, any percentage of tumor cells with cytoplasmic staining intensity of 1+, 2+ or 3+ were considered as IHC-positive and then evaluated by FISH [35]. Indeed, FISH is considered the “gold standard” to confirm IHC results, due to possible false-positive signals with IHC testing [36]. For MET only 2+ or 3+ in more than 10% of tumor cells were defined as positive and subsequently evaluated by FISH [37]. HER-2 IHC positive status was defined as tumors with a 2+ or 3+ staining in more than 10% of the cells and then evaluated by FISH [38].
PD-1 IHC was considered positive when ≥1% of intra-epithelial TILs were stained. PD-L1 immunostaining was considered positive when ≥1% of tumor cells had membranous staining [39]. CD3 and CD8 staining were also analyzed as the percentage of both intra-tumoral and stromal CD3 and CD8 positive lymphocytes over the total immune cells [14,15].
4.4. Fluorescent In Situ Hybridization (FISH)
Vysis ALK Break Apart FISH probes© (Abbott Molecular, Abbott Park, IL, USA), HER-2/CEP17 DNA Probe Kit II probes© (Abbott Molecular) and ZytoLight SPEC MET/CEN 7 Dual Color Probes© (ZytoVision, Bremerhaven, Germany) were used respectively for the detection of ALK rearrangement, HER-2 and cMET amplification.
ALK locus rearrangement was considered translocated if ≥15% of tumor cells showed isolated red signal(s) and/or split red and green signals. ALK appeared amplified and required further verification if an average copy number ≥6 copies per nucleus was detected [40]. HER-2 was considered amplified if average HER-2/CEP17 ratio was higher than 2.0 [38]. Tumors with MET/CEP7 ratio ≥2 or with an average number of MET signals per nucleus >6 were scored as positive for MET amplification [41].
4.5. Statistical Analysis
Survival curves and 95% confidence intervals were determined using the Kaplan-Meier method. Predictive factors of OS were evaluated using the log-rank test for univariate analysis and statistically significant variables were included in multivariate analysis using a Cox regression model. The level of significance was set at a p value of 0.05. Statistical analyses were performed using XLSTAT 2017 software (Addinsoft, New York, NY, USA).
5. Conclusions
Our study provided relevant and specific features of CRC patients with BM, such as frequent lung metastasis, frequent rectal tumor site and high rate of RAS mutation. These results suggest a need for BM screening in this mCRC patients subgroup, but will require further prospective investigations to determine if early identification of BM improves survival and/or quality of life. We have highlighted the usefulness of BM number, the presence of lung metastases and the expression of PD-L1 as prognostic markers. For the first time, we found that PD-L1 expression was associated with poor prognostic in CRC patients with BM. All of these new data can guide therapeutic decision-making in patients with BM from CRC.
Acknowledgments
The authors thank all of the clinical research technicians who participated in DNA extraction. Our original English-language manuscript was reread and revised by Jeffrey Arsham, an American medical translator. Finally, the authors would like to thank Vanessa Le Berre and Laetitia Rouleau for their assistance in preparing the submission of the article.
Abbreviations
| BM | Brain Metastases |
| CI | Confidence Interval |
| CT-scan | Computed Tomography scan |
| CRC | Colorectal Cancer |
| ECM | Extracranial Metastasis(es) |
| ECOG | Eastern Cooperative Oncology Group score |
| FISH | Fluorescence In Situ Hybridization |
| HR | Hazard Ratio |
| IHC | Immunohistochemistry |
| OS | Overall Survival |
| mCRC | Metastatic Colorectal Cancer |
| MMR | Mismatch Repair |
| MRI | Magnetic Resonance Imaging |
| pMMR | Proficient Mismatch Repair |
| dMMR | Deficient Mismatch Repair |
| PPT | Paired Primary Tumor |
| TMA | Tissue Microarray |
| TILs | Tumor-Infiltrating Lymphocytes |
Author Contributions
Conceptualization, P.R., L.K.-T. and D.T.; methodology, P.R., G.T., C.V., S.M., E.F., L.K.-T. and D.T.; validation, P.R., L.K.-T. and D.T.; formal analysis, P.R., G.T., C.V., S.M., E.F., J.G., A.B., S.E., C.P., M.W., L.K.-T. and D.T.; investigation, P.R., G.T., L.K.-T. and D.T.; data curation, P.R., L.K.-T. and D.T.; writing—original draft preparation, P.R., G.T., L.K.-T. and D.T.; writing—review and editing, P.R., G.T., C.V., S.M., E.F., J.G., A.B., S.E., C.P., M.W., L.K.-T. and D.T.; supervision, L.K.-T. and D.T.; project administration, L.K.-T. and D.T.
Funding
This work was supported by a grant from the associations “Sport et Collection” and “Ligue Contre le Cancer, Comités départementaux de la Vienne, Charente et Charente-Maritime”.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Christensen T.D., Spindler K.-L.G., Palshof J.A., Nielsen D.L. Systematic review: Brain metastases from colorectal cancer—Incidence and patient characteristics. BMC Cancer. 2016;16:260. doi: 10.1186/s12885-016-2290-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jung M., Ahn J.B., Chang J.H., Suh C.O., Hong S., Roh J.K., Shin S.J., Rha S.Y. Brain metastases from colorectal carcinoma: Prognostic factors and outcome. J. Neurooncol. 2011;101:49–55. doi: 10.1007/s11060-010-0214-9. [DOI] [PubMed] [Google Scholar]
- 3.Tanriverdi O., Kaytan-Saglam E., Ulger S., Bayoglu I.V., Turker I., Ozturk-Topcu T., Cokmert S., Turhal S., Oktay E., Karabulut B., et al. The clinical and pathological features of 133 colorectal cancer patients with brain metastasis: A multicenter retrospective analysis of the Gastrointestinal Tumors Working Committee of the Turkish Oncology Group (TOG) Med. Oncol. 2014;31:152. doi: 10.1007/s12032-014-0152-z. [DOI] [PubMed] [Google Scholar]
- 4.Yaeger R., Cowell E., Chou J.F., Gewirtz A.N., Borsu L., Vakiani E., Solit D.B., Rosen N., Capanu M., Ladanyi M., et al. RAS mutations affect pattern of metastatic spread and increase propensity for brain metastasis in colorectal cancer. Cancer. 2015;121:1195–1203. doi: 10.1002/cncr.29196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Christensen T.D., Palshof J.A., Larsen F.O., Høgdall E., Poulsen T.S., Pfeiffer P., Jensen B.V., Yilmaz M.K., Christensen I.J., Nielsen D. Risk factors for brain metastases in patients with metastatic colorectal cancer. Acta Oncol. 2017;56:639–645. doi: 10.1080/0284186X.2017.1290272. [DOI] [PubMed] [Google Scholar]
- 6.Michl M., Thurmaier J., Schubert-Fritschle G., Wiedemann M., Laubender R.P., Nüssler N.C., Ruppert R., Kleeff J., Schepp W., Reuter C., et al. Brain Metastasis in Colorectal Cancer Patients: Survival and Analysis of Prognostic Factors. Clin. Colorectal. Cancer. 2015;14:281–290. doi: 10.1016/j.clcc.2015.05.009. [DOI] [PubMed] [Google Scholar]
- 7.Liu J., Zeng W., Huang C., Wang J., Yang D., Ma D. Predictive and Prognostic Implications of Mutation Profiling and Microsatellite Instability Status in Patients with Metastatic Colorectal Carcinoma. [(accessed on 27 November 2018)]; doi: 10.1155/2018/4585802. Available online: https://www.hindawi.com/journals/grp/2018/4585802/abs/ [DOI] [PMC free article] [PubMed]
- 8.Prasanna T., Karapetis C.S., Roder D., Tie J., Padbury R., Price T., Wong R., Shapiro J., Nott L., Lee M., et al. The survival outcome of patients with metastatic colorectal cancer based on the site of metastases and the impact of molecular markers and site of primary cancer on metastatic pattern. Acta Oncol. 2018;57:1438–1444. doi: 10.1080/0284186X.2018.1487581. [DOI] [PubMed] [Google Scholar]
- 9.Vakiani E., Janakiraman M., Shen R., Sinha R., Zeng Z., Shia J., Cercek A., Kemeny N., D’Angelica M., Viale A., et al. Comparative genomic analysis of primary versus metastatic colorectal carcinomas. J. Clin. Oncol. 2012;30:2956–2962. doi: 10.1200/JCO.2011.38.2994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brastianos P.K., Carter S.L., Santagata S., Cahill D.P., Taylor-Weiner A., Jones R.T., Van Allen E.M., Lawrence M.S., Horowitz P.M., Cibulskis K., et al. Genomic Characterization of Brain Metastases Reveals Branched Evolution and Potential Therapeutic Targets. Cancer Discov. 2015;5:1164–1177. doi: 10.1158/2159-8290.CD-15-0369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Douillard J.-Y., Oliner K.S., Siena S., Tabernero J., Burkes R., Barugel M., Humblet Y., Bodoky G., Cunningham D., Jassem J., et al. Panitumumab-FOLFOX4 treatment and RAS mutations in colorectal cancer. N. Engl. J. Med. 2013;369:1023–1034. doi: 10.1056/NEJMoa1305275. [DOI] [PubMed] [Google Scholar]
- 12.Berghoff A.S., Schur S., Füreder L.M., Gatterbauer B., Dieckmann K., Widhalm G., Hainfellner J., Zielinski C.C., Birner P., Bartsch R., et al. Descriptive statistical analysis of a real life cohort of 2419 patients with brain metastases of solid cancers. ESMO Open. 2016;1:e000024. doi: 10.1136/esmoopen-2015-000024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.El-Deiry W.S., Vijayvergia N., Xiu J., Scicchitano A., Lim B., Yee N.S., Harvey H.A., Gatalica Z., Reddy S. Molecular profiling of 6,892 colorectal cancer samples suggests different possible treatment options specific to metastatic sites. Cancer Biol. Ther. 2015;16:1726–1737. doi: 10.1080/15384047.2015.1113356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tougeron D., Fauquembergue E., Rouquette A., Le Pessot F., Sesboüé R., Laurent M., Berthet P., Mauillon J., Di Fiore F., Sabourin J.-C., et al. Tumor-infiltrating lymphocytes in colorectal cancers with microsatellite instability are correlated with the number and spectrum of frameshift mutations. Mod. Pathol. 2009;22:1186–1195. doi: 10.1038/modpathol.2009.80. [DOI] [PubMed] [Google Scholar]
- 15.Maby P., Tougeron D., Hamieh M., Mlecnik B., Kora H., Bindea G., Angell H.K., Fredriksen T., Elie N., Fauquembergue E., et al. Correlation between Density of CD8+ T-cell Infiltrate in Microsatellite Unstable Colorectal Cancers and Frameshift Mutations: A Rationale for Personalized Immunotherapy. Cancer Res. 2015;75:3446–3455. doi: 10.1158/0008-5472.CAN-14-3051. [DOI] [PubMed] [Google Scholar]
- 16.Gatalica Z., Snyder C., Maney T., Ghazalpour A., Holterman D.A., Xiao N., Overberg P., Rose I., Basu G.D., Vranic S., et al. Programmed cell death 1 (PD-1) and its ligand (PD-L1) in common cancers and their correlation with molecular cancer type. Cancer Epidemiol. Biomark. Prev. 2014;23:2965–2970. doi: 10.1158/1055-9965.EPI-14-0654. [DOI] [PubMed] [Google Scholar]
- 17.Lee L.H., Cavalcanti M.S., Segal N.H., Hechtman J.F., Weiser M.R., Smith J.J., Garcia-Aguilar J., Sadot E., Ntiamoah P., Markowitz A.J., et al. Patterns and prognostic relevance of PD-1 and PD-L1 expression in colorectal carcinoma. Mod. Pathol. 2016;29:1433–1442. doi: 10.1038/modpathol.2016.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang M., Li G., Sun X., Ni S., Tan C., Xu M., Huang D., Ren F., Li D., Wei P., et al. MET amplification, expression, and exon 14 mutations in colorectal adenocarcinoma. Hum. Pathol. 2018;77:108–115. doi: 10.1016/j.humpath.2018.03.024. [DOI] [PubMed] [Google Scholar]
- 19.Abou-Bakr A.A., Elbasmi A. c-MET overexpression as a prognostic biomarker in colorectal adenocarcinoma. Gulf. J. Oncol. 2013;1:28–34. [PubMed] [Google Scholar]
- 20.Liu Y., Yu X.-F., Zou J., Luo Z.-H. Prognostic value of c-Met in colorectal cancer: A meta-analysis. World J. Gastroenterol. 2015;21:3706–3710. doi: 10.3748/wjg.v21.i12.3706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zeng Z.-S., Weiser M.R., Kuntz E., Chen C.-T., Khan S.A., Forslund A., Nash G.M., Gimbel M., Yamaguchi Y., Culliford A.T., et al. c-Met gene amplification is associated with advanced stage colorectal cancer and liver metastases. Cancer Lett. 2008;265:258–269. doi: 10.1016/j.canlet.2008.02.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Aprile G., Casagrande M., De Maglio G., Fontanella C., Rihawi K., Bonotto M., Pisa F.E., Tuniz F., Pizzolitto S., Fasola G. Comparison of the molecular profile of brain metastases from colorectal cancer and corresponding primary tumors. Future Oncol. 2017;13:135–144. doi: 10.2217/fon-2016-0196. [DOI] [PubMed] [Google Scholar]
- 23.Jeantet M., Tougeron D., Tachon G., Cortes U., Archambaut C., Fromont G., Karayan-Tapon L. High Intra- and Inter-Tumoral Heterogeneity of RAS Mutations in Colorectal Cancer. Int. J. Mol. Sci. 2016;17:2015. doi: 10.3390/ijms17122015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Feilchenfeldt J., Varga Z., Siano M., Grabsch H.I., Held U., Schuknecht B., Trip A., Hamaguchi T., Gut P., Balague O., et al. Brain metastases in gastro-oesophageal adenocarcinoma: Insights into the role of the human epidermal growth factor receptor 2 (HER2) Br. J. Cancer. 2015;113:716–721. doi: 10.1038/bjc.2015.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gabos Z., Sinha R., Hanson J., Chauhan N., Hugh J., Mackey J.R., Abdulkarim B. Prognostic significance of human epidermal growth factor receptor positivity for the development of brain metastasis after newly diagnosed breast cancer. J. Clin. Oncol. 2006;24:5658–5663. doi: 10.1200/JCO.2006.07.0250. [DOI] [PubMed] [Google Scholar]
- 26.Harter P.N., Bernatz S., Scholz A., Zeiner P.S., Zinke J., Kiyose M., Blasel S., Beschorner R., Senft C., Bender B., et al. Distribution and prognostic relevance of tumor-infiltrating lymphocytes (TILs) and PD-1/PD-L1 immune checkpoints in human brain metastases. Oncotarget. 2015;6:40836–40849. doi: 10.18632/oncotarget.5696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mansfield A.S., Aubry M.C., Moser J.C., Harrington S.M., Dronca R.S., Park S.S., Dong H. Temporal and spatial discordance of programmed cell death-ligand 1 expression and lymphocyte tumor infiltration between paired primary lesions and brain metastases in lung cancer. Ann. Oncol. 2016;27:1953–1958. doi: 10.1093/annonc/mdw289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Puhalla S., Elmquist W., Freyer D., Kleinberg L., Adkins C., Lockman P., McGregor J., Muldoon L., Nesbit G., Peereboom D., et al. Unsanctifying the sanctuary: Challenges and opportunities with brain metastases. Neuro-Oncology. 2015;17:639–651. doi: 10.1093/neuonc/nov023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Goldberg S.B., Gettinger S.N., Mahajan A., Chiang A.C., Herbst R.S., Sznol M., Tsiouris A.J., Cohen J., Vortmeyer A., Jilaveanu L., et al. Pembrolizumab for patients with melanoma or non-small-cell lung cancer and untreated brain metastases: Early analysis of a non-randomised, open-label, phase 2 trial. Lancet Oncol. 2016;17:976–983. doi: 10.1016/S1470-2045(16)30053-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pietrantonio F., Aprile G., Rimassa L., Franco P., Lonardi S., Cremolini C., Biondani P., Sbicego E.L., Pasqualetti F., Tomasello G., et al. A new nomogram for estimating survival in patients with brain metastases secondary to colorectal cancer. Radiother. Oncol. 2015;117:315–321. doi: 10.1016/j.radonc.2015.08.023. [DOI] [PubMed] [Google Scholar]
- 31.Droeser R.A., Hirt C., Viehl C.T., Frey D.M., Nebiker C., Huber X., Zlobec I., Eppenberger-Castori S., Tzankov A., Rosso R., et al. Clinical impact of programmed cell death ligand 1 expression in colorectal cancer. Eur. J. Cancer. 2013;49:2233–2242. doi: 10.1016/j.ejca.2013.02.015. [DOI] [PubMed] [Google Scholar]
- 32.Téglási V., Reiniger L., Fábián K., Pipek O., Csala I., Bagó A.G., Várallyai P., Vízkeleti L., Rojkó L., Tímár J., et al. Evaluating the significance of density, localization, and PD-1/PD-L1 immunopositivity of mononuclear cells in the clinical course of lung adenocarcinoma patients with brain metastasis. Neuro-Oncology. 2017;19:1058–1067. doi: 10.1093/neuonc/now309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cortes U., Guilloteau K., Rouvreau M., Archaimbault C., Villalva C., Karayan-Tapon L. Development of pyrosequencing methods for the rapid detection of RAS mutations in clinical samples. Exp. Mol. Pathol. 2015;99:207–211. doi: 10.1016/j.yexmp.2015.07.003. [DOI] [PubMed] [Google Scholar]
- 34.Lindeman N.I., Cagle P.T., Beasley M.B., Chitale D.A., Dacic S., Giaccone G., Jenkins R.B., Kwiatkowski D.J., Saldivar J.-S., Squire J., et al. Molecular testing guideline for selection of lung cancer patients for EGFR and ALK tyrosine kinase inhibitors: Guideline from the College of American Pathologists, International Association for the Study of Lung Cancer, and Association for Molecular Pathology. J. Mol. Diagn. 2013;15:415–453. doi: 10.1016/j.jmoldx.2013.03.001. [DOI] [PubMed] [Google Scholar]
- 35.Houang M., Toon C.W., Clarkson A., Sioson L., de Silva K., Watson N., Singh N.R., Chou A., Gill A.J. ALK and ROS1 overexpression is very rare in colorectal adenocarcinoma. Appl. Immunohistochem. Mol. Morphol. 2015;23:134–138. doi: 10.1097/PAI.0000000000000025. [DOI] [PubMed] [Google Scholar]
- 36.Yatabe Y. ALK FISH and IHC: You cannot have one without the other. J. Thorac. Oncol. 2015;10:548–550. doi: 10.1097/JTO.0000000000000461. [DOI] [PubMed] [Google Scholar]
- 37.Bardelli A., Corso S., Bertotti A., Hobor S., Valtorta E., Siravegna G., Sartore-Bianchi A., Scala E., Cassingena A., Zecchin D., et al. Amplification of the MET receptor drives resistance to anti-EGFR therapies in colorectal cancer. Cancer Discov. 2013;3:658–673. doi: 10.1158/2159-8290.CD-12-0558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Valtorta E., Martino C., Sartore-Bianchi A., Penaullt-Llorca F., Viale G., Risio M., Rugge M., Grigioni W., Bencardino K., Lonardi S., et al. Assessment of a HER2 scoring system for colorectal cancer: Results from a validation study. Mod. Pathol. 2015;28:1481–1491. doi: 10.1038/modpathol.2015.98. [DOI] [PubMed] [Google Scholar]
- 39.Overman M.J., McDermott R., Leach J.L., Lonardi S., Lenz H.-J., Morse M.A., Desai J., Hill A., Axelson M., Moss R.A., et al. Nivolumab in patients with metastatic DNA mismatch repair-deficient or microsatellite instability-high colorectal cancer (CheckMate 142): An open-label, multicentre, phase 2 study. Lancet Oncol. 2017;18:1182–1191. doi: 10.1016/S1470-2045(17)30422-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zito Marino F., Rocco G., Morabito A., Mignogna C., Intartaglia M., Liguori G., Botti G., Franco R. A new look at the ALK gene in cancer: Copy number gain and amplification. Expert Rev. Anticancer Ther. 2016;16:493–502. doi: 10.1586/14737140.2016.1162098. [DOI] [PubMed] [Google Scholar]
- 41.Pietrantonio F., Oddo D., Gloghini A., Valtorta E., Berenato R., Barault L., Caporale M., Busico A., Morano F., Gualeni A.V., et al. MET-Driven Resistance to Dual EGFR and BRAF Blockade May Be Overcome by Switching from EGFR to MET Inhibition in BRAF-Mutated Colorectal Cancer. Cancer Discov. 2016;6:963–971. doi: 10.1158/2159-8290.CD-16-0297. [DOI] [PubMed] [Google Scholar]