Abstract
Background
To prevent and control dementia, many scholars have focused on the transition stage between normal ageing and dementia, mild cognitive impairment (MCI) which is a key interventional target for dementia. Studies have shown that non-invasive brain stimulation (NIBS) is beneficial to improve cognitive function of MCI patients. However, whether NIBS is conducive to the protection of cognitive ability in MCI patients remains unknown due to limited evidence. The aim of the study was to systematically evaluate the modulation effect of NIBS on cognitive function (global cognitive ability and specific domains of cognition) in patients with MCI.
Results
A total of 11 RCTs comprising a total of 367 MCI participants. Meta-analysis showed that NIBS can significantly improve global cognition (n = 271, SMD = 0.94, 95% CI 0.47–1.41, p < 0.0001) and verbal fluency (n = 72, MD = 2.03, 95% CI 0.17–3.88, p = 0.03). However, there was no significant improvement in other domains of cognition.
Conclusions
NIBS has a positive effect on improving global cognitive function and verbal fluency. At the same time, it has a small positive effect on improving executive function. However, these findings should be interpreted carefully due to the limitations of the study.
Electronic supplementary material
The online version of this article (10.1186/s12868-018-0484-2) contains supplementary material, which is available to authorized users.
Keywords: Non-invasive brain stimulation, Mild cognitive impairment, Cognitive function, Meta-analysis
Background
With age increasing, the risk of Alzheimer’s disease (AD) is on the rise [1], however, the treatment of dementia is far from satisfactory [2, 3]. To prevent and control dementia, many scholars have focused on the transition stage between normal ageing and dementia, mild cognitive impairment (MCI) which is a key interventional target for dementia [4]. The main characteristics of MCI are objective memory impairment and other cognitive deficits; however, aspects of daily living are not significantly affected [5]. The incidence of MCI in people over 65 years of age is 10–20%, and more than half of them will progress into dementia within 5 years [6, 7]. Severe cognitive decline will have a huge impact on the daily lives of patients such as independent living ability losing, lower quality of life, and huge economic burden [8]. Thus, effective and timely interventions that aim to improve cognitive function or delay the process of cognitive decline will significantly benefit patients and their families.
Recently, there has been an increased interesting on the use of non-drug therapy to improve the cognitive function of MCI patients [9]. Studies have shown that as a new type of treatment, non-invasive brain stimulation (NIBS) is beneficial to improve cognitive function of MCI patients [10]. NIBS can alter neuronal activity temporarily and affect behavioural performance [11].
The two most commonly used techniques of NIBS are transcranial magnetic stimulation (TMS) and transcranial direct current stimulation (tDCS). TMS modulates cortical activities by delivering strong magnetic pulses to the cortex through the scalp [12, 13]. Different stimulation frequencies can enhance or inhibit cortical excitability in the target cortical region. Unlike TMS, tDCS delivers a continuous week currents (0.5–2.0 mA) to the scalp to modulate neuronal transmembrane potential toward hyperpolarization or depolarization, thereby altering plasticity in the stimulated brain regions [10, 14]. Although they are different in some respects, both tools can induce long-term after effects on cortical excitability and neuroplasticity.
Many studies [15–18] have reported the treatment effect of tDCS and TMS on cognitive outcomes in various populations, such as AD and healthy adults. For example, a study reported that for older adults, compare to the anodal or placebo (sham) tDCS, anodal tDCS not only strengthened episodic memories, but delayed recall is enhanced after 48 h compared with placebo stimulation [19]. Similarly, another study found up-regulation of the dorsolateral prefrontal cortex (DLPFC) led to improvements of everyday memory after 10-Hz TMS in MCI patients [20].
However, beneficial effects of NIBS are not always observed. A study [21] showed that 2 weeks of tDCS did not show significant group differences in the face-name association task. In addition, Boggio et al. [22] found that tDCS over the prefrontal cortex increases high-risk behaviour in older adults. In particular, a study with a crossover design failed to induce positive or negative behavioral effects following either low- or high-frequency TMS in seven patients with vascular MCI [23]. Therefore, the efficacy of tDCS or TMS as a treatment option remains controversial. Specifically, whether tDCS or TMS is conducive to the protection of cognitive ability in MCI patients remains unknown due to limited evidence.
This study was designed to systematically evaluate the effect of tDCS and TMS as an intervention on cognitive function of MCI patients, including global cognitive ability and specific domains of cognition, such as memory, executive function, attention, verbal fluency.
Methods
Protocol and registration
The protocol of this study was registered with the International Prospective Register of Systematic Review, PROSPERO, under the identification number CRD42018092620, and can be integrally assessed online (http://www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42018092620).
Literature search
We searched a total of seven electronic databases, including PubMed, EMBASE (OVID), SinoMed, China National Knowledge Infrastructure (CNKI), Wanfang degree and conference papers database, Chinese Science and Technology Periodical Database (VIP) from its inception to 31 January 2018, as well as the Cochrane Central Register of Controlled Trials (Cochrane Library, 2018, Issue 1). These databases were searched without language restrictions. Relevant keywords related to non-invasive brain stimulation as Medical Subject Heading terms and text words (e.g., ‘noninvasive brain stimulation’, or ‘transcranial direct current stimulation’, or ‘transcranial magnetic stimulation’) were used in combination with words related to mild cognitive impairment.
Inclusion criteria
The trials selected in the study should met the following inclusion criteria: (1) published or unpublished randomized controlled studies; (2) participants diagnosed with MCI based on any diagnostic criteria, such as Petersen criteria, 2004 MCI Key Symposium criteria or other standards and consensus; participants with vascular cognitive impairment or other neurological disorders resulting from AD, dementia or Parkinson’s disease were excluded; (3) the intervention of the experimental group was NIBS technique, regardless of the type; (4) the control group received basic intervention, sham stimulation, medication or other interventions; (5) outcomes included global cognitive ability and specific domain of cognition, which was measured by neuropsychological tests or other objective measurements. Studies without available data were excluded.
Study identification and data extraction
Eliminate duplicate records with the reference management software (Note Express V.2.0). In the literature screening, the title and abstracts were read first to eliminate irrelevant studies. The studies that potentially met the inclusion criteria were independently screened, extracted, and cross-checked by two reviewers. Disagreements were resolved by discussion with a third reviewer. Extract the following information from eligible studies: study design, sample size, participants’ characteristics, methodological information of research quality, experimental and control intervention, the duration, frequency, intensity and type of NIBS, outcomes, the time of follow-up, and adverse events.
Assessment of risk of bias in individual studies
Two reviewers independently evaluated the scientific quality of the study according to the JADAD scoring manual [24]. Evaluation content included description of random sequence generation, description of the double-blind procedure, and description of withdrawals and dropouts. The total score was 5 points, where a score of 1–2 points was associated with low quality and a score of 3–5 points was deemed as high quality.
Data analysis
A meta-analysis of outcomes for each study was performed using Review Manager 5.3 software and a two-sided p < 0.05 was considered statistically significant. Data were summarized using relative risk with 95% CI for binary outcomes. The measurement data used the MD or standardized MD and the 95% CI as the effect amount. The meta-analysis used the I2 test to observe the degree of statistical heterogeneity between studies. When I2 ≤ 50%, a fixed-effect model was used, while a random-effects model was used when I2 > 50%. A parallel sensitivity analysis was used to find the source of heterogeneity. Studies with different interventions were divided into subgroups for subgroup analysis according to different factors, such as design options, treatment duration, and specific interventions. For studies with significant clinical and methodological heterogeneity, the outcome meta-analysis was not performed, and only general statistical descriptions were performed. Statistical heterogeneity among the included studies was assessed using a χ2 test and Higgins I2 value, with I2 > 75% suggesting high statistical heterogeneity [25].
Results
Study identification
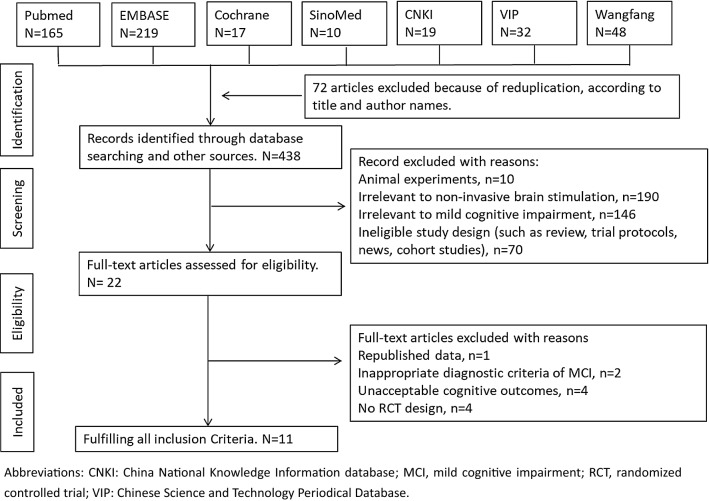
According to the original search strategy, 510 studies were retrieved, and 72 repetitive studies were excluded. After reading titles and abstracts, two independent reviewers excluded 416 articles that did not meet the inclusion criteria. A total of 22 studies were further evaluated, excluding 1 repeated publication, while 2 did not meet the MCI diagnostic criteria, 4 had unacceptable cognitive outcomes, and 4 were non-RCT studies. A total of 11 studies [20, 26–35] were included in the meta-analysis finally.
The detailed screening flow used to find eligible studies is presented in Fig. 1.
Fig. 1.
Flow diagram for searching and selection of the included studies
Characteristics of included studies
This review included 11 RCT studies involving 367 MCI participants (175 males and 192 females, average age 66.52 years) and Table 1 shows the characteristics of each study. Six studies [28–33] were conducted in China, two [26] in Italy, one [27] in Brazil, one [34] in South Korea and one [35] in the US. All studies reported clear diagnostic, inclusion, and exclusion criteria.
Table 1.
Characteristics of included studies in this systematic review
| Author, year | Mean age | Participants (M/F) | Intervention | Stimulation site | Frequency, duration and intensity | Outcomes |
|---|---|---|---|---|---|---|
| Han, 2013 | 66.59 | 40 (14/26) | T: active rTMS C: sham rTMS |
Left/right DLPFC | 20 Hz, 80% RMT, 30 min/day, 5 days/week, 8 weeks | Global cognitive function/MoCA; Linguistic function/VFT; Executive function/WCST; Attention/TMT-A, DSST |
| Zhang, 2014 | 65.75 | 50 (25/25) | T: active rTMS C: oral Piracetam |
Bilateral frontal area | 5 Hz, 100% RMT, 800 pulses/day, 6 days/week, 16 weeks | Global cognitive function/MoCA; ERP |
| Yang, 2014 | 66.00 | 33 (15/18) | T: active rTMS C: sham rTMS |
Bilateral DLPFC | 20 Hz, 80% RMT, 30 min/day, 5 days/week, 8 weeks | Global cognitive function/MMSE; ERP |
| Rosa, 2015 | 69.05 | 20 (11/9) | T: anode tDCS + PT C: sham tDCS + PT |
Left DLPFC | 2 mA, 25 min/day, 5 days/week, 2 weeks | Global cognitive function/MMSE, PD-CRS; Memory/PAL; Attention/TMT; Executive function/Semantic fluency |
| Sun, 2015 | 64.40 | 80 (43/37) | T: active rTMS + cognitive training C: cognitive training |
Left DLPFC and left PC | 15 Hz, 80%-110%RMT, 30 min/day, 6 days/week, 8 weeks | Global cognitive function/MoCA; ERP |
| Hellen, 2015 | 65.16 | 34 (12/22) | T: active rTMS C: sham rTMS |
Left DLPFC | 10 Hz, 110% RMT, 2000 pulses/session, 1 session/day, 10 days | Memory/RBMT, WMS, RAVLT, WAIS-III; Executive function/TMT-B, VFT |
| Kyongsik, 2016 | 73.94 | 16 (5/11) | T: anode tDCS C: sham tDCS |
Anodal: left DLPFC; Cathode: right DLPFC |
2 mA, 30 min/day, 3 days/week, 3 weeks | Memory/MMQ, HVLT; Visuospatial function/RCFT; Linguistic function/BNT; PET |
| Long, 2016 | 66.95 | 30 (14/16) | T: active rTMS C: sham rTMS |
Left DLPFC | 15 Hz, 90% RMT, once a day, 10 days | Global cognitive function/MoCA; Memory/CMS |
| Wu, 2017 | 67.61 | 41 (21/20) | T: active rTMS + oral paroxetine C: oral paroxetine |
Left DLPFC | 20 Hz, 80% RMT, 15 min/day, 5 days/week, 4 weeks | Global cognitive function/MMSE; ERP |
| Giacomo, 2017 | 70.00 | 14 (7/7) | T: active rTMS C: sham rTMS |
PC | 20 Hz, 100% RMT, 20 min/day, 5 days/week, 6 weeks | Global cognitive function/MMSE, Memory/RAVLT; Executive functions/FAB; Attention/DSST |
| Prasad, 2018 | 65.60 | 9 (8/1) | T: active rTMS C: sham rTMS |
Left DLPFC | 10 Hz, 120% RMT, 45 min/day, 5 days/week, 8 weeks | Apathy/AES-C; Global cognitive function/MMSE; Executive functions/TMT A&B; Functional status/IADL; Impression/CGI |
BNT, Boston Naming Test; CMS, Clinical Memory Scale; CGI, Clinical Global Impression; DLPFC, dorsolateral prefrontal cortex; DSST, Digit Symbol Substitution Test; ERP, Event-related Potentials; FAB, Frontal Assessment Battery; HVLT, Hopkins Verbal Learning Test; IADL, Instrumental Activities of Daily Living; MMSE, Mini-mental State Examination; MMQ, Multifactorial Memory Questionnaire; MoCA, Montreal Cognitive Assessment; PAL, Paired Associated Learning; PC, Precuneus; PD-CRS, Parkinson’s Disease Cognitive Rating Scale; PET, Positron Emission Tomography; PT, Physical Therapy; RAVLT, Rey Auditory Verbal Learning Test; RBMT, Rivermead Behavioral Memory Test; RCFT, Rey Complex Figure Test; RMT, Resting Motor Threshold; rTMS, repetitive Transcranial Magnetic Stimulation; TMT, Trial Making Tests; tDCS, transcranial Direct Current Stimulation; VFT, Verbal Fluency Test; WAIS-III, Wechsler Adult Intelligence Scale III; WCST, Wisconsin Card Sorting Test; WMS, Wechsler Memory Scale
The types of NIBS included tDCS [26, 27] and TMS [20, 28–35]. For tDCS, the frequency varied from three to five sessions weekly and 25–30 min per session. The duration of the intervention lasted 2–3 weeks. The stimulation site was in the dorsolateral prefrontal cortex (DLPFC), and the intensity was 2 mA. For TMS, the frequency varied from five to six sessions weekly and 15–45 min per session. The duration of the intervention lasted 2–16 weeks. The stimulation site was in the DLPFC, bilateral frontal area, and precuneus, with an intensity from 80 to 120% resting motor threshold (RMT). Of these 11 studies, 3 were followed up from 1 to 3 months [20, 26, 33]. Two studies compared TMS with drug therapy [29, 33]. Two studies combined TMS/tDCS with physical therapy (PT) or cognitive training to compare the effects of combination therapy with PT or cognitive training alone [26, 31]. Other studies performed comparisons between true and shame-stimuli. There was a wide variety of cognitive measurement tools used in these studies, including Mini-mental state examination (MMSE), Montreal Cognitive Assessment (MoCA), Parkinson’s Disease Cognitive Rating Scale (PD-CRS), Wechsler Memory Scale (WMS), Trial Making Tests-A and B (TMT-A&B), and verbal fluency test (VFT), with different tools applied to evaluate the same cognitive domain within a study or among studies.
Risk of bias of included studies
The risks of bias for all studies are shown in Table 2. In these studies, 3 studies described the use of a random number table and Matlab software to generate random sequences [30, 33, 34]. One study used the covariate adaptive randomization method for random assignment [26]. The rest of the studies mentioned random grouping but did not describe the generation method of random sequences, and there was a potential risk of high selection bias. Five studies used a double-blind design for blindness to subjects and assessors [20, 26, 30, 34, 35]; therefore, their risk of detection bias was judged as low. A single-blind design was used in one other study [33]. However, none of the other studies mentioned blindness, and thus have a potentially high risk of implementation bias and high detection bias. Four studies reported shedding and described the data processing method [20, 26, 30, 34, 35]; therefore, the risk of loss bias was deemed as low. Overall, most of the included studies were judged to have a high risk of bias with low methodological quality.
Table 2.
Risk of bias summary: review authors’ judgements about each risk of bias item for each included study
| Author, year | Randomization sequence generation | Blinding method | Withdrawals and dropouts | Jadad score |
|---|---|---|---|---|
| Han, 2013 | Not described in detail | Not mentioned | 2 Drop out of family reason | 2 |
| Zhang, 2014 | Not described in detail | Not mentioned | Not mentioned | 1 |
| Yang, 2014 | Random number table | Double-blind manner | Not mentioned | 4 |
| Rosa, 2015 | Covariate adaptive randomization method | Double-blind manner | Not mentioned | 4 |
| Sun, 2015 | Not described in detail | Not mentioned | Not mentioned | 1 |
| Hellen, 2015 | Not described in detail | Double-blind manner | 2 Drop out of personal reason | 4 |
| Kyongsik, 2016 | Random number generator from the Matlab software | Double-blind manner | Not mentioned | 4 |
| Long, 2016 | Not described in detail | Not mentioned | Not mentioned | 1 |
| Wu, 2017 | Random number table | Single-blind manner | 7 Drop out of a change in condition or other reasons | 3 |
| Giacomo, 2017 | Not described in detail | Not mentioned | Not mentioned | 3 |
| Prasad, 2018 | Not described in detail | Double-blind manner | 1 Did not tolerate the treatment | 4 |
CNKI: China National Knowledge Information database; MCI, mild cognitive impairment; RCT, randomized controlled trial; VIP: Chinese Science and Technology Periodical Database
Effect of interventions
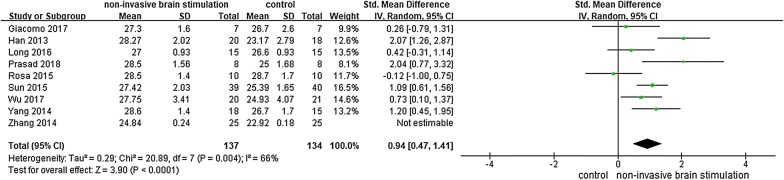
Global cognitive function
Nine studies [26, 28–34] reported the effects of NIBS on global cognitive ability in participants with MCI by using MMSE, MoCA and Parkinson’s Disease Cognitive Rating Scale (PD-CRS). The results showed that NIBS had a significant effect on improving global cognitive ability among participants with MCI, as demonstrated by significantly increased MMSE scores and MoCA scores (n = 301, SMD = 1.82, 95% CI 0.86–2.78, p < 0.0002, I2 = 91%, the random-effect model; Fig. 2). One study [26] reported that tDCS participants had higher PD-CRS scores than those in the control group, the difference was significant (p = 0.041).
Fig. 2.
NIBS versus other intervention: global cognitive ability
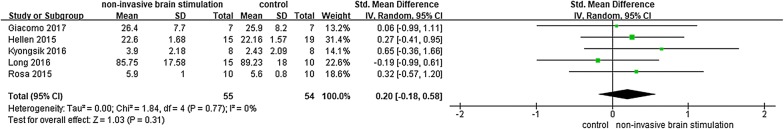
Memory
Five studies [20, 26, 27, 32, 34] involving 109 participants reported the effects of NIBS on memory ability by using the Rivermead Behavioural Memory Test (RBMT), Rey Auditory-Verbal Learning Test (RAVLT), Digit Symbol Substitution Test (DSST), Multifactorial Memory Questionnaire (MMQ), and Clinical memory scale (CMS). Three of the studies compared the effects of TMS stimulation and sham TMS stimulation. The other two articles compare the difference between anode tDCS stimulation and PT/sham stimulation. The results of meta-analysis showed no significant difference between the NIBS group and control groups (n = 109, SMD = 0.20, 95% CI − 0.18 to 0.58, p = 0.31, I2 = 0%, the random-effect model; Fig. 3).
Fig. 3.
NIBS versus other intervention: memory
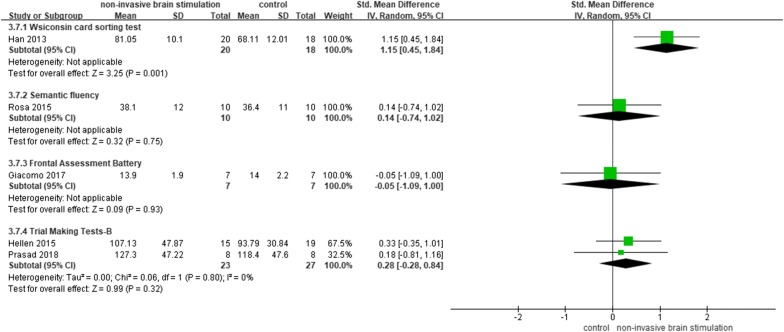
Executive function
The effects of NIBS on executive function were evaluated in five studies [20, 26, 28, 34, 35] using the Wisconsin card sorting test (WCST), Semantic fluency and Frontal Assessment Battery (FAB), and TMT part B (ms). Due to the use of these different tools, we performed a subgroup analysis. One study showed that TMS significantly improved executive ability by increasing WCST scores (SMD = 1.15, 95% CI 0.45–1.84, p = 0.001), while another reported no significant changes (Fig. 4).
Fig. 4.
NIBS versus other intervention: executive ability
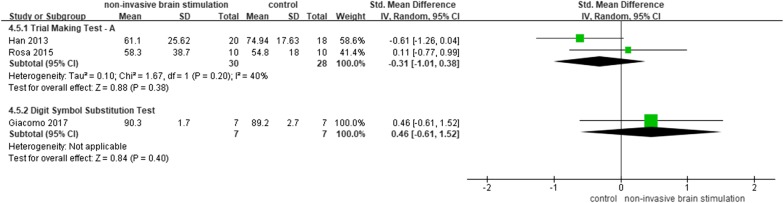
Attention
Three studies [26, 28, 34] reported the effects of NIBS on attention ability by using TMT part A (ms) and Digit Symbol Substitution Test (DSST). The results of meta-analysis showed no significant difference between the NIBS group and control groups on reaction time of TMT part A (n = 58, SMD = − 0.31, 95% CI − 1.01 to 0.38, p = 0.38, I2 = 40%, the random-effect model). Regarding the DSST score, NIBS had no significant effect on improving attention ability (n = 14, MD = 0.46, 95% CI − 0.61 to 1.52, p = 0.40; Fig. 5).
Fig. 5.
NIBS versus other intervention: attention
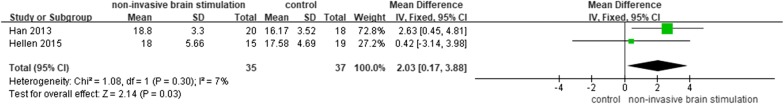
Verbal fluency
Two studies [20, 28] reported the effects of NIBS on verbal fluency ability. The results of meta-analysis showed a significant difference between NIBS and control group (n = 72, MD = 2.03, 95% CI 0.17–3.88, p = 0.03, I2 = 7%, the fixed-effect model; Fig. 6).
Fig. 6.
NIBS versus other intervention: verbal fluency
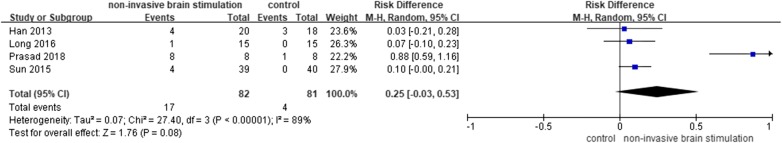
Adverse effects
Adverse effects were reported in 4 studies [28, 31, 32, 35], where the main symptoms were dizziness, pain, and facial twitching. The results of meta-analysis showed no significant difference between the NIBS group and control groups on adverse event rate (RD = 0.25, 95% CI − 0.03 to 0.53, p = 0.08, I2 = 89%, the random-effect model; Fig. 7). Notably, two participants experienced severe pain during TMS stimulation, while one participant quit treatment.
Fig. 7.
NIBS versus other intervention: adverse effects
Discussion
Epidemiological studies show that 10–15% patients with MCI will transform to dementia [36]. It is very important to provide timely interventions for patients with cognitive impairment in this reversible phase. NIBS has become a potentially useful tool. In particular, NIBS can directly affect the memory mechanisms of young, elderly, and neurotic dysfunction patients, including working memory, episodic memory, and contact memory [37, 38]. However, there is no consistent conclusion regarding whether NIBS can improve the cognitive function of MCI patients.
Eleven studies involving 367 subjects were included in this review. All studies were designed to compare tDCS or TMS with a lack of specific stimuli. The results of the meta-analysis showed that NIBS was beneficial to improve the cognitive function of MCI patients. In terms of global cognitive function, NIBS significantly improved the global cognitive function in MCI patients. Within a specific cognitive domain, NIBS has a slightly significant benefit on executive function and a potentially positive impact on verbal fluency ability. Nevertheless, as verbal fluency was measured only in two studies, the results of this measure should be taken with caution.
With functional magnetic resonance imaging (fMRI), multiple resting state networks such as default mode network, attention network and sensorimotor network have been affected in patients with MCI [39]. Meinzer et al. conducted a double-blind, cross-control study in which brain changes were recorded using task-related and resting fMRI during tDCS stimulation. fMRI data suggest that the low accuracy of semantic flow tests in MCI patients may be related to hyperactivity of bilateral prefrontal area. Anodic-tDCS significantly improved the accuracy of semantic fluency tests in MCI patients, reduced task-related prefrontal hyperactivity and facilitated the normalization of abnormal network structure in resting-state fMRI [40]. Another critical one concerns with modulation of neurotransmitter levels [41, 42]. TMS may affect the regulation of cortical neuronal activity by altering the dynamics of excitation/inhibition of neurotransmitter systems, such as GABA and glutamate [42].
Previous studies and reviews have summarized the main advantages of tDCS and TMS [10, 43]: first, these methods are ideal for exploring brain plasticity throughout the life cycle. Second, they can regulate neurons bidirectionally, not only inhibiting the excitability of neurons but also enhancing the excitability of neurons. Third, these techniques can apply the stimulus only to the position we want without affecting other parts, so that we can treat the disease while avoiding side effects. This is beyond the ability of pharmacology or complementary therapy. In particular, the application of NIBS to dysfunctional neural networks could significantly enhance learning- and memory-related effects. Moreover, repeated use of NIBS for stimulation could make the effect longer lasting.
In terms of safety, there were several mild adverse events in the NIBS group and control group, such as temporary dizziness, pain, and facial twitching. However, these events could be recovered without special treatment. In addition, there was no significant difference in the incidence of adverse events between the two groups. However, it should be noted that there were 2 serious adverse events in the intervention group, of which one participant had severe pain during the treatment, where the pain was relieved after the stimulus was stopped, while the other patient quit treatment due to pain. Although the safety of NIBS has been recognized by most people currently, the individual safety should be monitored, and personal thresholds should be evaluated to determine appropriate parameters for each patient undergoing NIBS treatment [44–46].
This review only included randomized controlled trials, which implied that the included studies had rigorous research design. Regarding the participants, we more force on the patients with MCI. In order to reduce potential confusion and make the generalization of the findings more pertinent, we excluded participants with secondary cognitive impairment (e.g., vascular dementia) or severe cognitive impairment (e.g., AD). All these methods helped to support the NIBS-related causal hypothesis.
There were several limitations in the systematic review. (1) The stimulation parameters used in each study (including stimulation intensity, stimulation rate, stimulation site, and duration) were quite different, and the optimal parameters for NIBS treatment could not be determined. (2) Only three studies were followed up for 1–3 months, suggesting that the effect of NIBS could be maintained for a long time; however, the conclusion should be verified by larger and longer follow-up studies. (3) The control methods adopted in the study were different. Due to the small number of included studies, the systematic review included the results of all the studies together for analysis but did not analyse them separately according to the methodological differences. For example, there are studies that only used drugs as controls, and thus, the placebo effect could not be avoided, which may exaggerate the efficacy of NIBS. Moreover, some studies did not describe whether the subjects were combined with the basic treatment. Therefore, it is unclear whether there was a synergistic effect between the treatments. (4) The overall quality of the research included in this systematic review was not high. Most of the studies did not specifically describe the method of random allocation and did not perform allocation concealment, which may generate selection bias. (5) Eight studies used shame stimuli, but did not test whether the blindness was successful, which may increase measurement bias.
Clinical implications and recommendations for future studies
Meta-analysis showed that in patients with MCI, NIBS seems to improve the overall cognitive function, verbal fluency, and executive function, which suggests that NIBS may be a potential intervention for patients with MCI. Because the quality of the studies is not high, the conclusions should be treated with caution. We also believe that NIBS may offer an exciting novel treatment option in patients with MCI.
Future studies in this field should explore appropriate NIBS treatment parameters (e.g., stimulus type, stimulus intensity, stimulation frequency, stimulation site) for patients with MCI. For example, Ahmed et al. [47] conducted a TMS intervention trial on AD, suggesting that high-frequency stimulation is superior to low-frequency stimulation. Moreover, a more sensitive and objective measurement tool should be used to assess the overall cognitive ability and specific domains of cognition. As memory loss is a major manifestation of MCI, recent studies have concluded that delayed memory and semantic memory tests can better predict whether MCI will progress to AD compared to other memory tests [48].
There are different types of MCI, such as amnestic MCI and non-amnestic MCI as well as single domain impairment or multiple domain impairment [49]. Whether the response of different types of MCI to NIBS treatment is different remains to be discussed. In addition, since the adverse events reported in these studies are mainly transient dizziness and headaches, we believe that the setting of NIBS parameters in future studies should be based on safety guidelines [50–52]. At the same time, follow-up studies are needed to assess the long-term risks and benefits of NIBS treatment. In addition, in order to better assess the quality of the research, the author should follow the CONSORT guidelines [53] when reporting research.
Conclusion
NIBS may benefit the improvement of global cognitive function and verbal fluency in patients with MCI, while it has a slight positive impact on executive function. However, considering the different types of NIBS, and the discrepancies in intensity, frequency, locus, duration of stimulation, as well as the limited number of studies and the small sample size, these findings must be carefully explained. More sample size trials are needed, with more rigorously randomized controlled trial designed and standardized training programmes to draw specific and accurate conclusions.
Additional file
Authors’ contributions
LC, JT conceived and designed the experiments. YX, ZJ, JF performed the experiments. YX, ZJ analysed the data. JL, JS contributed reagents/materials/analysis tools. YX, ZJ, JF wrote the paper. LC, JT revised study and wrote several sections of the manuscript. JL, JS helped to develop the study measures and analyses. All authors contributed to drafting the manuscript and have read and approved the final manuscript. The corresponding author had final responsibility for the decision to submit for publication. All authors read and approved the final manuscript.
Acknowledgements
Not applicable.
Competing interests
The authors declare that they have no competing interests, whether intellectual, financially, or proprietary.
Availability of data and materials
All relevant data are within the paper and its Supporting Information files.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Not applicable.
Funding
This study is supported by the Fujian Collaborative Innovation Center for Rehabilitation Technology (X2017004-XIETONG), and TCM Rehabilitation Research Center of SATCM, and Rehabilitation medical technology Joint National Local Engineering Research Center. The funders had no role in study design, data collection and analysis, interpretation of data, or preparation of the manuscript.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abbreviations
- AD
Alzheimer’s disease
- BNT
Boston Naming Test
- CMS
Clinical Memory Scale
- CNKI
China National Knowledge Infrastructure
- CGI
Clinical Global Impression
- DLPFC
dorsolateral prefrontal cortex
- DSM-IV
diagnostic and statistical manual
- DSST
Digit Symbol Substitution Test
- ERP
event-related potentials
- FAB
frontal assessment battery
- fMRI
functional magnetic resonance imaging
- HVLT
Hopkins Verbal Learning Test
- IADL
instrumental activities of daily living
- MCI
mild cognitive impairment
- MMSE
mini-mental state examination
- MMQ
Multifactorial Memory Questionnaire
- MoCA
Montreal Cognitive Assessment
- NIBS
non-invasive brain stimulation
- PAL
paired associated learning
- PC
Precuneus
- PD-CRS
Parkinson’s Disease Cognitive Rating Scale
- PET
positron emission tomography
- PT
physical therapy
- RAVLT
Rey Auditory Verbal Learning Test
- RBMT
Rivermead Behavioral Memory Test
- RCFT
Rey Complex Figure Test
- RCT
randomized controlled studies
- RMT
resting motor threshold
- TMS
transcranial magnetic stimulation
- TMT
Trial Making Tests
- tDCS
transcranial direct current stimulation
- VFT
Verbal Fluency Test
- VIP
Chinese Science and Technology Periodical Database
- WAIS-III
Wechsler Adult Intelligence Scale III
- WCST
Wisconsin Card Sorting Test
- WMS
Wechsler Memory Scale
Contributor Information
Ying Xu, Email: 13799326706@163.com.
Zhijie Qiu, Email: 346285642@qq.com.
Jingfang Zhu, Email: 346286192@qq.com.
Jiao Liu, Email: 1773903011@qq.com.
Jingsong Wu, Email: 61102547@qq.com.
Jing Tao, Email: 369049101@qq.com.
Lidian Chen, Email: cld@fjtcm.edu.cn.
References
- 1.Ferri CP, Prince M, Brayne C, Brodaty H, Fratiglioni L, Ganguli M, Hall K, Hasegawa K, Hendrie H, Huang YQ, et al. Global prevalence of dementia: a Delphi consensus study. Lancet. 2005;366(9503):2112–2117. doi: 10.1016/S0140-6736(05)67889-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Association A. 2012 Alzheimer’s disease facts and figures. Alzheimers Dement. 2012;8(2):131–168. doi: 10.1016/j.jalz.2012.02.001. [DOI] [PubMed] [Google Scholar]
- 3.Karakaya T, Fusser F, Schroder J, Pantel J. Pharmacological treatment of mild cognitive impairment as a prodromal syndrome of Alzheimer s disease. Curr Neuropharmacol. 2013;11(1):102–108. doi: 10.2174/157015913804999487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jia J, Zhou A, Wei C, Jia X, Wang F, Li F, Wu X, Mok V, Gauthier S, Tang M, et al. The prevalence of mild cognitive impairment and its etiological subtypes in elderly Chinese. Alzheimers Dement. 2014;10(4):439–447. doi: 10.1016/j.jalz.2013.09.008. [DOI] [PubMed] [Google Scholar]
- 5.Petersen RC, Negash S. Mild cognitive impairment: an overview. CNS Spectr. 2008;13(1):45–53. doi: 10.1017/s1092852900016151. [DOI] [PubMed] [Google Scholar]
- 6.Budson AE. Understanding memory dysfunction. Neurologist. 2009;15(2):71–79. doi: 10.1097/NRL.0b013e318188040d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bartley M, Bokde AL, O’Neill D. Mild cognitive impairment. N Engl J Med. 2011;365(14):1357–1359. doi: 10.1056/NEJMc1108238. [DOI] [PubMed] [Google Scholar]
- 8.Lee CY, Cheng SJ, Lin HC, Liao YL, Chen PH. Quality of life in patients with Dementia with Lewy Bodies. Behav Neurol. 2018;2018:8320901. doi: 10.1155/2018/8320901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huckans M, Hutson L, Twamley E, Jak A, Kaye J, Storzbach D. Efficacy of cognitive rehabilitation therapies for mild cognitive impairment (MCI) in older adults: working toward a theoretical model and evidence-based interventions. Neuropsychol Rev. 2013;23(1):63–80. doi: 10.1007/s11065-013-9230-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Birba A, Ibanez A, Sedeno L, Ferrari J, Garcia AM, Zimerman M. Non-invasive brain stimulation: a new strategy in mild cognitive impairment? Front Aging Neurosci. 2017;9:16. doi: 10.3389/fnagi.2017.00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Miniussi C, Harris JA, Ruzzoli M. Modelling non-invasive brain stimulation in cognitive neuroscience. Neurosci Biobehav Rev. 2013;37(8):1702–1712. doi: 10.1016/j.neubiorev.2013.06.014. [DOI] [PubMed] [Google Scholar]
- 12.Fregni F, Pascual-Leone A. Technology insight: noninvasive brain stimulation in neurology-perspectives on the therapeutic potential of rTMS and tDCS. Nat Clin Pract Neurol. 2007;3(7):383–393. doi: 10.1038/ncpneuro0530. [DOI] [PubMed] [Google Scholar]
- 13.Rubens MT, Zanto TP. Parameterization of transcranial magnetic stimulation. J Neurophysiol. 2012;107(5):1257–1259. doi: 10.1152/jn.00716.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Prehn K, Flöel A. Potentials and limits to enhance cognitive functions in healthy and pathological aging by tDCS. Front Cell Neurosci. 2015;9:355. doi: 10.3389/fncel.2015.00355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Berryhill ME, Jones KT. tDCS selectively improves working memory in older adults with more education. Neurosci Lett. 2012;521(2):148–151. doi: 10.1016/j.neulet.2012.05.074. [DOI] [PubMed] [Google Scholar]
- 16.Floel A, Suttorp W, Kohl O, Kurten J, Lohmann H, Breitenstein C, Knecht S. Non-invasive brain stimulation improves object-location learning in the elderly. Neurobiol Aging. 2012;33(8):1682–1689. doi: 10.1016/j.neurobiolaging.2011.05.007. [DOI] [PubMed] [Google Scholar]
- 17.Eliasova I, Anderkova L, Marecek R, Rektorova I. Non-invasive brain stimulation of the right inferior frontal gyrus may improve attention in early Alzheimer’s disease: a pilot study. J Neurol Sci. 2014;346(1–2):318–322. doi: 10.1016/j.jns.2014.08.036. [DOI] [PubMed] [Google Scholar]
- 18.Khedr EM, Gamal NF, El-Fetoh NA, Khalifa H, Ahmed EM, Ali AM, Noaman M, El-Baki AA, Karim AA. A double-blind randomized clinical trial on the efficacy of cortical direct current stimulation for the treatment of Alzheimer’s disease. Front Aging Neurosci. 2014;6:275. doi: 10.3389/fnagi.2014.00275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sandrini M, Manenti R, Brambilla M, Cobelli C, Cohen LG, Cotelli M. Older adults get episodic memory boosting from noninvasive stimulation of prefrontal cortex during learning. Neurobiol Aging. 2016;39:210–216. doi: 10.1016/j.neurobiolaging.2015.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Drumond MH, Myczkowski ML, Maia MC, Arnaut D, Leite RP, Sardinha MC, Lancelote AR, Boura BB, Alves FDSA, Tortella G, et al. Transcranial magnetic stimulation to address mild cognitive impairment in the elderly: a randomized controlled study. Behav Neurol. 2015;2015:287843. doi: 10.1155/2015/287843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cotelli M, Manenti R, Brambilla M, Petesi M, Rosini S, Ferrari C, Zanetti O, Miniussi C. Anodal tDCS during face-name associations memory training in Alzheimer’s patients. Front Aging Neurosci. 2014;6:38. doi: 10.3389/fnagi.2014.00038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Boggio PS, Campanha C, Valasek CA, Fecteau S, Pascual-Leone A, Fregni F. Modulation of decision-making in a gambling task in older adults with transcranial direct current stimulation. Eur J Neurosci. 2010;31(3):593–597. doi: 10.1111/j.1460-9568.2010.07080.x. [DOI] [PubMed] [Google Scholar]
- 23.Sedlackova S, Rektorova I, Fanfrdlova Z, Rektor I. Neurocognitive effects of repetitive transcranial magnetic stimulation in patients with cerebrovascular disease without dementia. J Psychophysiol. 2008;22(1):14–19. [Google Scholar]
- 24.Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, McQuay HJ. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17(1):1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 25.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Manenti R, Brambilla M, Benussi A, Rosini S, Cobelli C, Ferrari C, Petesi M, Orizio I, Padovani A, Borroni B, et al. Mild cognitive impairment in Parkinson’s disease is improved by transcranial direct current stimulation combined with physical therapy. Mov Disord. 2016;31(5):715–724. doi: 10.1002/mds.26561. [DOI] [PubMed] [Google Scholar]
- 27.Yun K, Song IU, Chung YA. Changes in cerebral glucose metabolism after 3 weeks of noninvasive electrical stimulation of mild cognitive impairment patients. Alzheimers Res Ther. 2016;8(1):49. doi: 10.1186/s13195-016-0218-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ke-yan HAN, Lu-lu YU, Lan WANG, Na LI, Ke-zhi LIU, Shun-jiang XU, Xue-yi WANG. The case–control study of the effect of repetitive transcranial magnetic stimulation on elderly mild cognitive impairment patients. J Clin Psychiatry. 2013;23(3):156–159. [Google Scholar]
- 29.Zhang L, Yuan L, Wang Y. Effects of repetitive transcranial magnetic stimulation on cognitive function in patients with mild cognitive impairment. J Clin Neurol. 2014;27(3):203–206. [Google Scholar]
- 30.Linlin Y, Keyan H, Xueyi W, Cuixia A, Shunjiang X, Mei S, Lan W, Lulu Y. Preliminary study of high-frequency repetitive transcranial magnetic stimulation in treatment of mild cognitive impairment. Chin J Psychiatry. 2014;47(4):227–231. [Google Scholar]
- 31.Rui S, Yan Ma. Effect of repetitive transcranial magnetic stimulation combined with cognitive training on mild cognitive impairment. Chin J Rehabil. 2015;30(5):355–357. [Google Scholar]
- 32.Shiyu L, Xiaoming W, Cheng L, Xin L, Fei Y, Du H, Lin H, Ming Z. Impacts of repetitive transcranial magnetic stimulation on the brain network regulation and cognitive function of patients with amnesiac mild cognitive impairment. J Epileptol Electroneurophysiol. 2016;25(1):6–11. [Google Scholar]
- 33.Wu Z, Zhou Z, Zhao R, Wang J. Effect of high-frequency repetitive transcranial magnetic stimulation on elderly patients with depression and mild cognitive impairment. J Neurosci Mental Health. 2017;17(8):562–565. [Google Scholar]
- 34.Koch G, Bonni S, Pellicciari MC, Casula EP, Mancini M, Esposito R, Ponzo V, Picazio S, Di Lorenzo F, Serra L, et al. Transcranial magnetic stimulation of the precuneus enhances memory and neural activity in prodromal Alzheimer’s disease. Neuroimage. 2018;169:302–311. doi: 10.1016/j.neuroimage.2017.12.048. [DOI] [PubMed] [Google Scholar]
- 35.Padala PR, Padala KP, Lensing SY, Jackson AN, Hunter CR, Parkes CM, Dennis RA, Bopp MM, Caceda R, Mennemeier MS, et al. Repetitive transcranial magnetic stimulation for apathy in mild cognitive impairment: a double-blind, randomized, sham-controlled, cross-over pilot study. Psychiatry Res. 2018;261:312–318. doi: 10.1016/j.psychres.2017.12.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Grober E, Lipton RB, Hall C, Crystal H. Memory impairment on free and cued selective reminding predicts dementia. Neurology. 2000;54(4):827–832. doi: 10.1212/wnl.54.4.827. [DOI] [PubMed] [Google Scholar]
- 37.Manenti R, Cotelli M, Robertson IH, Miniussi C. Transcranial brain stimulation studies of episodic memory in young adults, elderly adults and individuals with memory dysfunction: a review. Brain Stimul. 2012;5(2):103–109. doi: 10.1016/j.brs.2012.03.004. [DOI] [PubMed] [Google Scholar]
- 38.Elder GJ, Taylor JP. Transcranial magnetic stimulation and transcranial direct current stimulation: treatments for cognitive and neuropsychiatric symptoms in the neurodegenerative dementias? Alzheimers Res Ther. 2014;6(9):74. doi: 10.1186/s13195-014-0074-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Brier MR, Thomas JB, Snyder AZ, Benzinger TL, Zhang D, Raichle ME, Holtzman DM, Morris JC, Ances BM. Loss of intranetwork and internetwork resting state functional connections with Alzheimer’s disease progression. J Neurosci. 2012;32(26):8890–8899. doi: 10.1523/JNEUROSCI.5698-11.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Meinzer M, Lindenberg R, Phan MT, Ulm L, Volk C, Floel A. Transcranial direct current stimulation in mild cognitive impairment: behavioral effects and neural mechanisms. Alzheimers Dement. 2015;11(9):1032–1040. doi: 10.1016/j.jalz.2014.07.159. [DOI] [PubMed] [Google Scholar]
- 41.Ridding MC, Ziemann U. Determinants of the induction of cortical plasticity by non-invasive brain stimulation in healthy subjects. J Physiol. 2010;588(Pt 13):2291–2304. doi: 10.1113/jphysiol.2010.190314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Reis J, John D, Heimeroth A, Mueller HH, Oertel WH, Arndt T, Rosenow F. Modulation of human motor cortex excitability by single doses of amantadine. Neuropsychopharmacol. 2006;31(12):2758–2766. doi: 10.1038/sj.npp.1301122. [DOI] [PubMed] [Google Scholar]
- 43.Heise KF, Niehoff M, Feldheim JF, Liuzzi G, Gerloff C, Hummel FC. Differential behavioral and physiological effects of anodal transcranial direct current stimulation in healthy adults of younger and older age. Front Aging Neurosci. 2014;6:146. doi: 10.3389/fnagi.2014.00146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.McClintock SM, Reti IM, Carpenter LL, McDonald WM, Dubin M, Taylor SF, Cook IA, O’Reardon J, Husain MM, Wall C, et al. Consensus recommendations for the clinical application of repetitive transcranial magnetic stimulation (rTMS) in the treatment of depression. J Clin Psychiatry. 2018 doi: 10.4088/JCP.16cs10905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Aleman A. Use of repetitive transcranial magnetic stimulation for treatment in psychiatry. Clin Psychopharm Neurosci. 2013;11(2):53–59. doi: 10.9758/cpn.2013.11.2.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Brunoni AR, Amadera J, Berbel B, Volz MS, Rizzerio BG, Fregni F. A systematic review on reporting and assessment of adverse effects associated with transcranial direct current stimulation. Int J Neuropsychopharmacol. 2011;14(8):1133–1145. doi: 10.1017/S1461145710001690. [DOI] [PubMed] [Google Scholar]
- 47.Ahmed MA, Darwish ES, Khedr EM, El SY, Ali AM. Effects of low versus high frequencies of repetitive transcranial magnetic stimulation on cognitive function and cortical excitability in Alzheimer’s dementia. J Neurol. 2012;259(1):83–92. doi: 10.1007/s00415-011-6128-4. [DOI] [PubMed] [Google Scholar]
- 48.Gainotti G, Quaranta D, Vita MG, Marra C. Neuropsychological predictors of conversion from mild cognitive impairment to Alzheimer’s disease. J Alzheimers Dis. 2014;38(3):481–495. doi: 10.3233/JAD-130881. [DOI] [PubMed] [Google Scholar]
- 49.Petersen RC. Mild cognitive impairment. Lancet. 2006;367(9527):1979. doi: 10.1016/S0140-6736(06)68881-8. [DOI] [PubMed] [Google Scholar]
- 50.Rossi S, Hallett M, Rossini PM, Pascual-Leone A. Safety, ethical considerations, and application guidelines for the use of transcranial magnetic stimulation in clinical practice and research. Clin Neurophysiol. 2009;120(12):2008–2039. doi: 10.1016/j.clinph.2009.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rossini PM, Burke D, Chen R, Cohen LG, Daskalakis Z, Di Iorio R, Di Lazzaro V, Ferreri F, Fitzgerald PB, George MS, et al. Non-invasive electrical and magnetic stimulation of the brain, spinal cord, roots and peripheral nerves: basic principles and procedures for routine clinical and research application. An updated report from an I.F.C.N. Committee. Clin Neurophysiol. 2015;126(6):1071–1107. doi: 10.1016/j.clinph.2015.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Woods AJ, Antal A, Bikson M, Boggio PS, Brunoni AR, Celnik P, Cohen LG, Fregni F, Herrmann CS, Kappenman ES, et al. A technical guide to tDCS, and related non-invasive brain stimulation tools. Clin Neurophysiol. 2016;127(2):1031–1048. doi: 10.1016/j.clinph.2015.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340:c332. doi: 10.1136/bmj.c332. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.