Endoscopic submucosal dissection (ESD) theoretically allows the en bloc resection of colorectal lesions, irrespective of size. Both increasing lesion size and rectosigmoid location have been identified as independent risk factors for submucosal invasion.1 In these select lesions, en bloc resection is desirable because it facilitates accurate histopathologic assessment.2, 3 However, ESD is a technically complex procedure with the potential for serious adverse events. Adequate countertraction during ESD is essential for visualization and exposure of the dissecting plane for safe and effective dissection.
A novel tissue retractor system (HybridKnife-I; Erbe, Marietta, Ga, USA) was recently approved by the U.S. Food and Drug Administration (Fig. 1). The tissue retractor system consists of an expandable nitinol cage mounted onto a flexible overtube to facilitate stabilization of the working field around the target lesion. Two articulating channels through the overtube permit the passage of grasping devices to facilitate tissue manipulation and traction independent of the endoscope, further enhancing visualization of the dissecting plane. In this video, we present a case of ESD of a large rectal lesion by use of this novel tissue retractor system.
Figure 1.
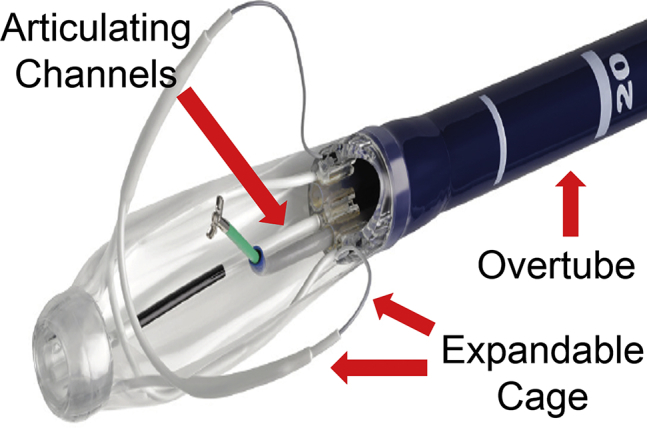
The tissue retractor system consists of an expandable nitinol cage with retractor wires mounted onto a flexible overtube. The expandable cage can be configured to stabilize the working field and grasping devices can be inserted through the articulating channels for tissue manipulation and countertraction during endoscopic resection.
A 55-year-old woman with no significant comorbidities underwent screening colonoscopy. A large rectal mass involving nearly the entire circumference was identified 12 cm from the anal verge (Fig. 2). On the basis of these findings, the patient was referred to our institution for possible ESD. On endoscopy, a lateral spreading granular nodular mixed lesion was identified in the rectum. There were no gross morphologic or pit/vessel patterns to suggest deep invasion. Hence, preparations were made for ESD (Video 1, available online at www.VideoGIE.org). Cautery marks were placed along the outer margins of the lesion. A lifting solution (methylene blue admixed with saline solution) was injected into the submucosa at the anal aspect of the target lesion, followed by a circumferential incision into the submucosa with an electrosurgical knife, capable of simultaneous high-pressure needle-free injection and dissection. After this, the tissue retractor system was front-loaded onto the endoscope and advanced into the rectum. Once the target lesion was visualized, the retractable cage was expanded and configured to provide an adequate working field (Fig. 3). Grasping forceps were then advanced through the articulating channels of the retractor system for tissue manipulation and traction during ESD (Fig. 4). The tissue retractor system facilitated visualization of the dissecting plane and completion of the ESD (Fig. 5). The resected specimen (82 mm × 66 mm) was retrieved en bloc and fixed in formalin (Fig. 6). Histopathologic examination revealed the lesion to be a tubulovillous adenoma with focal serrated features. Both the lateral and deep margins were determined to be free of neoplasm. There were no intraprocedural adverse events, and the patient continued to do well 4 weeks after the procedure.
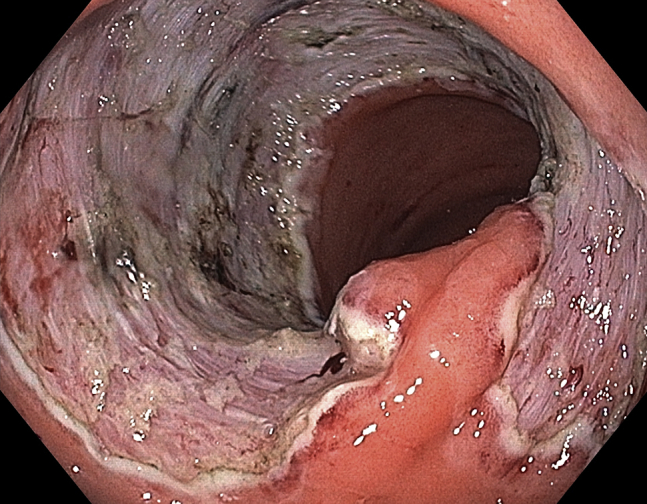
Figure 2.
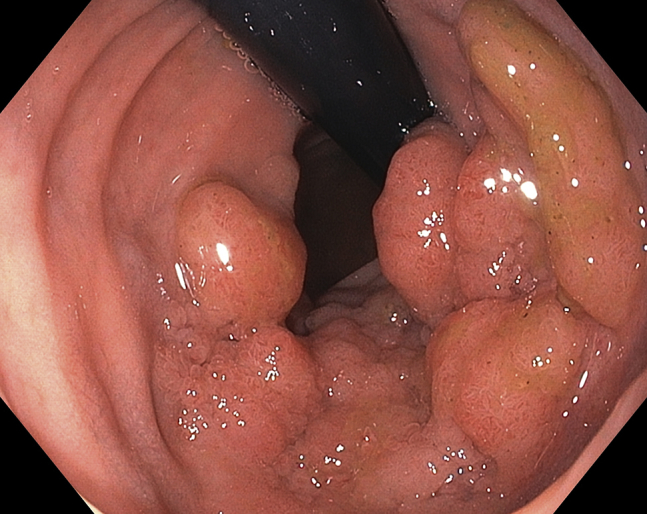
Large lateral spreading granular nodular mixed rectal lesion involving nearly the entire luminal circumference.
Figure 3.
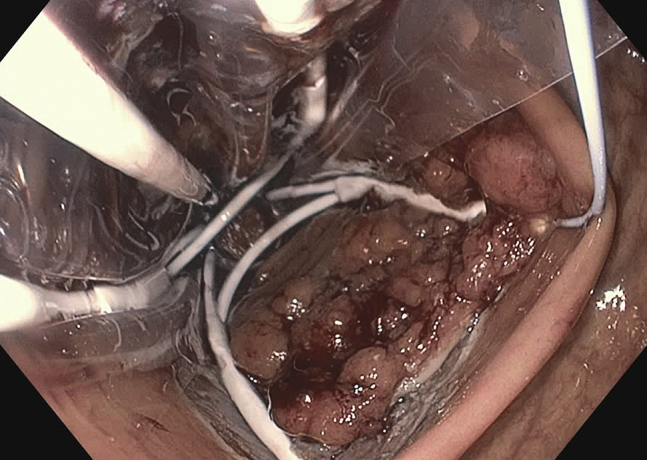
The expandable cage provides stabilization of the working field for endoscopic submucosal dissection.
Figure 4.
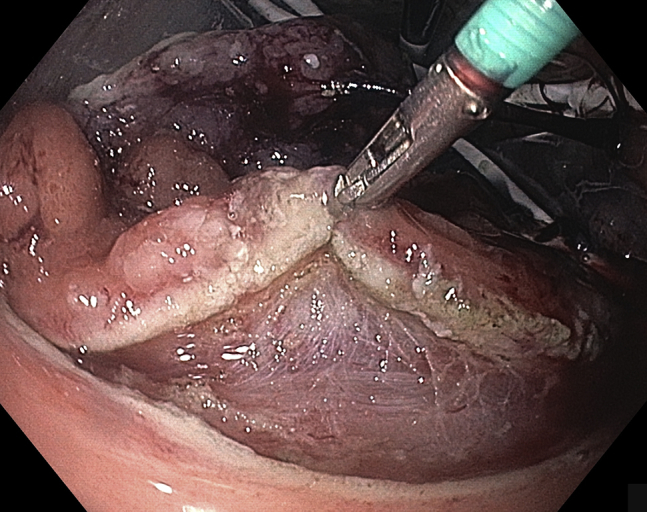
Grasping devices through the tissue retraction system allow for tissue manipulation and countertraction during endoscopic submucosal dissection.
Figure 5.
Endoscopic image after completion of endoscopic submucosal dissection.
Figure 6.
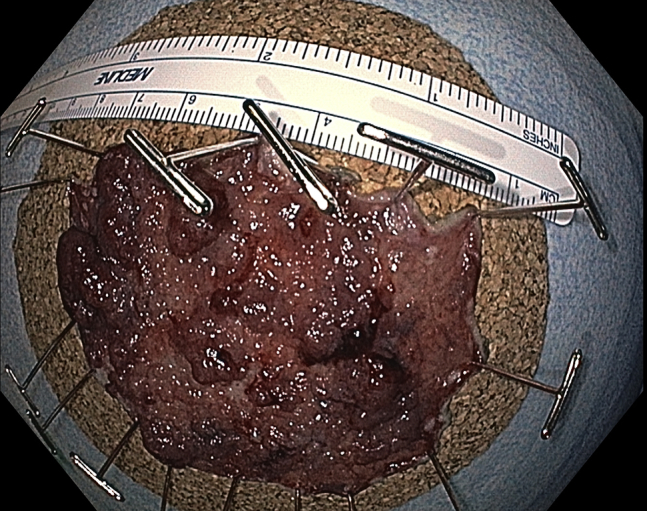
Resected (82-mm × 66-mm) specimen confirmed on histopathologic examination to be a tubulovillous adenoma with focal serrated features; the lateral and deep margins were free of neoplasm.
In conclusion, ESD is a technically demanding procedure with the potential for serious adverse events. With recent advances in endoscopic technology, novel dedicated ESD accessories and devices have begun to emerge, which may facilitate the dissemination of ESD in the West. In this case, ESD of a large rectal lesion was successfully completed with the assistance of a new tissue retractor system, which provided a stable operative field and permitted adequate traction for safe and effective ESD. Future studies are needed to further corroborate the utility of this new tissue retractor platform.
Disclosure
Dr Yang and Dr Draganov are consultants for Boston Scientific. All other authors disclosed no financial relationships relevant to this publication.
Supplementary data
Endoscopic submucosal dissection (ESD) of a large rectal lesion using a novel tissue retractor system.
References
- 1.Burgess N.G., Hourigan L.F., Zanati S.A. Risk stratification for covert invasive cancer among patients referred for colonic endoscopic mucosal resection: a large multi-center cohort. Gastroenterology. 2017;153:732–742. doi: 10.1053/j.gastro.2017.05.047. [DOI] [PubMed] [Google Scholar]
- 2.Pimentel-Nunes P., Dinis-Ribeiro M., Ponchon T. Endoscopic submucosal dissection: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2015;47:829–854. doi: 10.1055/s-0034-1392882. [DOI] [PubMed] [Google Scholar]
- 3.Tanaka S., Kashida H., Saito Y. JGES guidelines for colorectal endoscopic submucosal dissection/endoscopic mucosal resection. Dig Endosc. 2015;27:417–434. doi: 10.1111/den.12456. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Endoscopic submucosal dissection (ESD) of a large rectal lesion using a novel tissue retractor system.


