Abstract
Objective:
Video (indirect) laryngoscopy is used as a primary tracheal intubation device for difficult airways in emergency departments and in adult ICUs. The use and outcomes of video laryngoscopy compared with direct laryngoscopy has not been quantified in PICUs or cardiac ICUs.
Design:
Retrospective review of prospectively collected observational data from a multicenter tracheal intubation database (National Emergency Airway Registry for Children) from July 2010 to June 2015.
Setting:
Thirty-six PICUs/cardiac ICUs across the United States, Canada, Japan, New Zealand, and Singapore.
Patients:
Any patient admitted to a PICU or a pediatric cardiac ICU and undergoing tracheal intubation.
Interventions:
Use of direct laryngoscopy versus video laryngos-copy for tracheal intubation.
Measurements and Main Results:
There were 8,875 tracheal intubations reported in the National Emergency Airway Registry for Children database, including 7,947 (89.5%) tracheal intubations performed using direct laryngoscopy and 928 (10.5%) tracheal intubations performed using video laryngoscopy. Wide variability in video laryngoscopy use exists across PICUs (median, 2.6%; range, 0–55%). Video laryngoscopy was more often used in older children (p < 0.001), in children with history of a difficult airway (p = 0.01), in children intubated for ventilatory failure (p < 0.001), and to facilitate the completion of an elective procedure (p = 0.048). After adjusting for patient-level covariates, a secular trend, and site-level variance, the use of video laryngoscopy significantly increased over a 5-year period compared with fiscal year 2011 (odds ratio, 6.7; 95% Cl, 1.7–26.8 for fiscal year 2014 and odds ratio, 11.2; 95% Cl, 3.2–38.9 for fiscal year 2015). The use of video laryngoscopy was independently associated with a lower occurrence of tracheal intubation adverse events (adjusted odds ratio, 0.57; 95% Cl, 0.42–0.77; p < 0.001) but not with a lower occurrence of severe tracheal intubation adverse events (adjusted odds ratio, 0.86; 95% Cl, 0.56–1.32; p = 0.49) or fewer multiple attempts at endotracheal intubation (adjusted odds ratio, 0.93; 95% Cl, 0.71–1.22; p = 0.59).
Conclusions:
Using National Emergency Airway Registry for Children data, we described patient-centered adverse outcomes associated with video laryngoscopy compared with direct laryngoscopy for tracheal intubation in the largest reported international cohort of children to date. Data from this study may be used to design sufficiently powered prospective studies comparing patient-centered outcomes for video laryngoscopy versus direct laryngoscopy during endotracheal intubation.
Keywords: adverse events, indirect laryngoscopy, pediatric intensive care, tracheal intubation, video laryngoscopy
Tracheal intubations (TIs) of children in PICUs and pediatric cardiac ICUs (CICUs) are risky due to the inherent respiratory and hemodynamic instability and limited physiologic reserve of critically ill children (1, 2). TI is commonly associated with adverse events directly related to the procedure and medications administered to achieve adequate sedation and analgesia required for TI (2, 3). Multiple adult studies on urgent endotracheal intubations in emergency departments and adult medical ICUs have demonstrated the utility of video laryngoscopy (VL) over direct laryngoscopy (DL) to achieve higher first-attempt and ultimate success rates for TI (4–8). DL requires that the laryngoscope operator align the oral, pharyngeal, and laryngeal axes to obtain a clear view of the glottis inlet. In contrast, manipulation of a VL does not require alignment of these three axes in order to achieve a view of the glottic inlet on a video screen due to a magnified and panoramic view projected from a light source and micro-video camera mounted on the end third of the laryngoscope blade (9). Although there are abundant data regarding the use of VL for critically ill adults and for children with difficult airway features in the operating suites, there is significantly less literature on the use of VL for ‘TI of critically ill children in PICUs.
The National Emergency Airway Registry for Children (NEAR4KIDS) is a collaborative venture of 36 international PICUs and CICUs, supported by the Pediatric Acute Lung Injury and Sepsis Investigators network (PALISI), which comprises the largest clinical repository of prospectively collected data on TI of children in PICUs (3). The NEAR4KIDS registry has reported on the process of care and safety outcomes of TI of children in PICUs (10), developed a quality improvement (QI) pediatric airway management bundle (1), described the site-level factors involved in tracheal intubation-associated events (TIAE) and severe TIAE (10, 11), and defined the frequency and associated factors of difficult airway (12). In this article, we report the variation in the rate of use of VL compared with DL over time in multiple PICUs. We further examined the clinical characteristics of children for which VL was chosen over DL for TI. Finally, we compared the TIAE, severe TIAE, and multiple TI attempts between VL versus DL for TI. Our primary hypothesis was that the use of VL increased from inception of the database until present. Our secondary hypothesis was that the use of VL would decrease the rate of TIAE, severe TIAE, and the need for greater than or equal to three attempts at TI compared with DL.
METHODS
Setting
This study was conducted across 36 PICUs/CICUs in the United States, Canada, Japan, New Zealand, and Singapore. Study sites were recruited through the PALISI network (eTable 1, Supplemental Digital Content 1, http://links.lww.com/PCC/A421).
Design
The NEAR4KIDS database is a prospectively collected research database developed by members of the PALISI network in conjunction with the NEAR investigators to study pediatric airway management in PICUs in order to support QI initiatives (1, 8). Development of a data collection form was piloted in a tertiary care PICU and refined for the NEAR4KIDS investigators as previously described (1). Institutional review board’s approval was obtained at each participating site. All 36 sites voluntarily participated in the NEAR4KIDS QI initiative and instituted a site-specific compliance plan to capture greater than 95% of TI encounters.
Inclusion and Exclusion Criteria
All primary TIs in PICUs and CICUs were included. The first course (i.e., one method or approach, explanation to follow) for each encounter was included for the analysis. Existing tracheal tube change was excluded. TIs by nonlaryngoscopy devices (e.g., fiberoptic bronchoscopy) were excluded.
Definitions and Outcome Measures
Three airway management events may occur during TI and include the 1) encounter, 2) course, and 3) attempt. An encounter is defined as one episode of completed advanced airway management, including TI. A course is defined as one method or approach to secure an airway, for example, oral, nasal, or by bronchoscope along with one set of medications including premedication and induction. An attempt is defined as a single advanced airway maneuver that begins with the insertion of a laryngoscope or laryngeal mask into the patients’ mouth or nose and ending when the device is removed. Multiple attempts may be made within an intubation course, and more than one course and multiple attempts may occur during one encounter (10). Successful TI is defined as the placement of an endotracheal tube (ETT) in the trachea confirmed by primary indicators such as chest rise, auscultation, and secondary methods such as end-tidal Co2 detection. Process of care variances are defined as more than two attempts per course or oxygen desaturation to less than 80% during the course when the oxygen saturation was greater than or equal to 90% after preoxygenation and without preexisting cyanotic heart disease. A desaturation less than 80% by itself is not considered to be a TIAE. An oxygen saturation of 80% was chosen as a conservative threshold because of the steep arterial oxyhemoglobin disossiation curve at this value, and our previous study demonstrated the association between adverse events and desaturation with this threshold (3). Patients with saturations below 90% after preoxygenation were included in the study, but desaturations lower than 80% at TI were not counted as desaturation events in these patients.
Undesired events have been previously defined in the NEAR4KIDS database (10) and are separated into two categories: nonsevere TIAE and severe TIAE. Nonsevere TIAE include mainstem bronchial intubation, esophageal intubation with immediate recognition, emesis without aspiration, hypertension requiring therapy, epistaxis, dental or lip trauma, medication error, cardiac dysrhythmia, and pain and/or agitation requiring additional medication that results in a delay in TI. Mainstem bronchial intubation was considered only when it was confirmed on chest radiograph or recognized after the clinical team secured the ETT. Severe TIAE include cardiac arrest, esophageal intubation with delayed recognition, emesis with witnessed aspiration, hypotension requiring fluid and/or vasoactive agent, laryngospasm, malignant hyperthermia, pneumothorax/pneumomediastinum, or direct airway injury.
Statistical Analysis
Statistical analysis was performed using STATA 14.0 (Stata Corp, College Station, TX). Summary statistics were described by mean and sd for parametric variables and by median and 25–75th interquartile range (IQR) for nonparametric variables. For categorical variables with a dichotomous outcome, the contingency table method was used with chi-square or Fisher exact test, as appropriate. Wilcoxon rank sum test was used for comparison of nonparametric variables. Logistic regression was performed for a dichotomous outcome to evaluate the association with exposure variables while adjusting for covariates. Pepe and Anderson (13) showed that substantial bias may occur if generalized estimating equation models with nondiagonal correlation structures are fitted to longitudinal data with time-varying covariates. We, therefore, applied identity working correlation structures, with a sandwich estimator of covariance to account for the correlation within sites. A p value less than 0.05 was considered significant for all hypotheses.
RESULTS
Participating PICU and CICU Characteristics
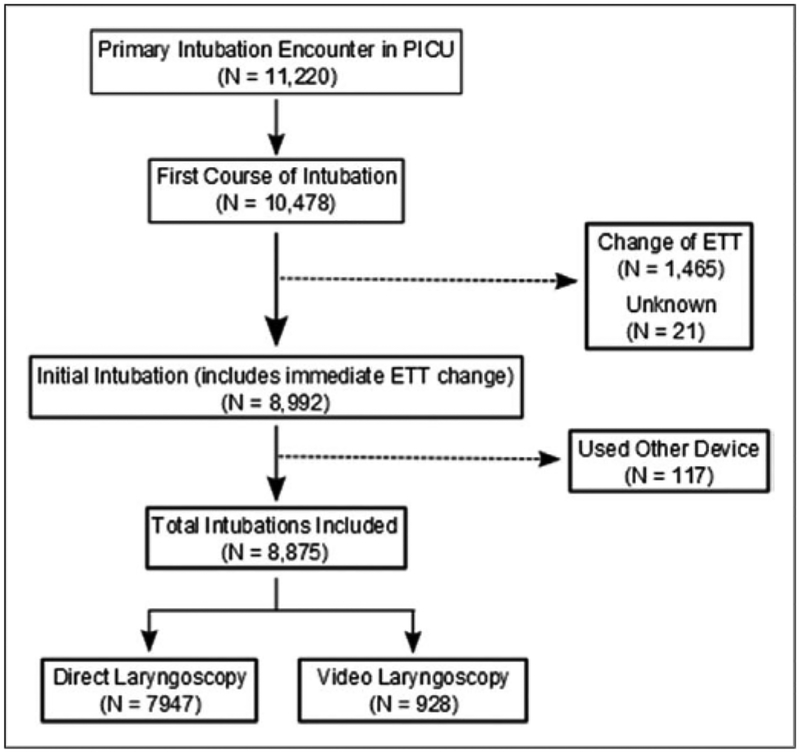
There were 11,220 total intubation encounters in the NEAR-4KIDS database from July 2010 to June 2015, and of all encounters, 10,478 included a first course of TI. Of these first courses of TI, 1,465 were excluded because they involved changing of the ETT, and an additional 21 were excluded because the type of encounter was not reported. There were 8,992 initial courses of TI that could also include an immediate ETT change; however, 117 of these ‘TI were excluded because a device other than a DL or VL was used (e.g., a bronchoscope, a lightwand, or intubation through a tracheostomy). A total of 8,875 TI were included in the analysis with 7,947 via DL and 928 via VL. Figure 1 summarizes the inclusion or exclusion of TI events in this analysis. Of the 928 TI via VL, one of the following VL devices was used to perform TI: Glidescope (Verathon Inc, Bothell, WA) (n = 128; 13.8%), C-MAC (Karl-Storz, Tuttlingen, Germany) (n = 667; 71.9%), Airtraq (Airtraq, LLC, Fenton, MO) (n = 22; 2.4%), and other unspecified VL devices (n = 111; 12.0%).
Figure 1.
Diagram describing inclusion and exclusion of patients in the study. ETT = endotracheal tube.
Thirty-six PICUs participated in the NEAR4KIDS registry. Table 1 denotes the characteristics of ICUs by size with large defined at greater than 30 beds (n = 7). Small- (< 12 beds; n = 1) and medium-sized PICUs (12–30 beds; n = 28) are grouped together. An academic PICU is defined by the presence of either a residency and/or fellowship program, and 92% of the PICUs in NEAR4KIDS are considered academic. Large PICUs tend to use VL to a greater extent than small- or medium-sized PICUs (large PICU, 18.3% vs small/medium PICU, 5.5%; p < 0.001). Academic PICUs use VL less often than nonacademic PICUs (academic, 9.4% vs nonacademic, 25.1%; p < 0.001). The majority of intubations were performed by Pediatric Critical Care fellows (42.0%), Pediatric or Emergency Medicine residents (19.5%), Pediatric Critical Care attending physicians (16.3%), and nurse practitioners (8.6%) performing most of the remaining TIs.
table 1.
ICU Characteristics and Demographics of Patients
| Characteristics | Number, n = 36 (%) | Direct Laryngoscopy, n = 7,947 (89.5%) | Video Laryngoscopy, n = 928 (10.5%) | Total, n = 8,875 (100%) | P |
|---|---|---|---|---|---|
| ICU size, n (%) | 7,945 | 928 | 8,873 | ||
| Large (> 30 beds) | 7(19) | 2,805(81.7) | 628(18.3) | 3,433 (38.7) | <0.001 |
| Small/medium (≤ 30 beds) | 29(81) | 5,140(94.5) | 300 (5.5) | 5,440 (61.3) | |
| Academic | 33 (92) | 7,516(90.6) | 784 (9.4) | 8,300 (93.5) | <0.001 |
| Nonacademic | 3(8) | 429 (74.9) | 144 (25.1) | 573 (6.5) | |
| First-attempt provider | 7,947 | 928 | 8,875 | <0.001 | |
| PCCM fellow | 3,273 (41.2) | 451 (48.6) | 3,724 (42.0) | ||
| Pediatric/emergency medicine resident | 1,603 (20.2) | 123(13.3) | 1,726(19.5) | ||
| PCCM attending | 1,262(15.9) | 182(19.6) | 1,444(16.3) | ||
| Nurse practitioner | 674 (8.5) | 89 (9.6) | 763 (8.6) | ||
| Subspecialist | 421 (5.3) | 47 (5.0) | 468 (5.3) | ||
| Respiratory therapist | 86(1.1) | 6 (0.7) | 92(1.0) | ||
| Hospitalist | 28 (0.3) | 1 (0.1) | 29 (0.3) | ||
| Other | 600 (7.5) | 29(3.1) | 629 (7.1) | ||
| Age (yr) | <0.001 | ||||
| Infant (< 1) | 3,472 (43.7) | 321 (34.6) | 3,793 (42.3) | ||
| Young child (1–7) | 2,575 (32.4) | 328 (35.3) | 2,903 (32.7) | ||
| Child (8–17) | 1,560(19.6) | 229 (24.7) | 1,789 (20.2) | ||
| Adult (≥ 18) | 340 (4.28) | 50 (5.4) | 390 (4.4) | ||
| Weight (kg), median (IQR) | 10(5–23.2) | 12.5 (6.1–31.5) | <0.001 | ||
| Gender, n (%)a | 7,937 | 928 | 8,865 | 0.785 | |
| Male | 4,470 (56.3) | 526 (56.7) | 4,996 (56.4) | ||
| Female | 3,465 (43.7) | 400 (43.1) | 3,865 (43.6) | ||
| Unknown | 2 (0.03) | 2 (0.22) | 4 (0.05) | ||
| Diagnostic categorya | 7,770 | 926 | 8,696 | <0.001 | |
| Upper respiratory | 724 (9.3) | 141 (15.2) | 865 (9.9) | ||
| Lower respiratory | 2,530 (32.6) | 374 (40.4) | 2,904 (33.4) | ||
| Cardiac (surgical) | 780(10.0) | 36 (3.9) | 816(9.4) | ||
| Cardiac (medical) | 512(6.6) | 14(1.5) | 526 (6.1) | ||
| Sepsis/shock | 591 (7.6) | 51 (5.5) | 642 (7.4) | ||
| Neurologic | 1,386(17.8) | 182(19.7) | 1,568(18.0) | ||
| Trauma | 154(1.9) | 30 (3.2) | 184 (2.1) | ||
| Other | 1,093(14.1) | 98(10.6) | 1,191 (13.7) | ||
| Pediatric Index of Mortality 2b | |||||
| Predicted mortality (%) | 2.1 (0.89–5.8) | 4.2(1.2–14.8) | 2.4 (0.9–6.5) | <0.0001 |
IQR = interquartile range, PCCM = Pediatric Critical Care Medicine.
Missing data.
Pediatric Index of Mortality 2 value is missing in 1,980 cases.
Patient Characteristics
The demographics, physical characteristics, diagnostic category, and indication for ‘TI of patients with TI performed by DL and VL are reported in Tables 1 and 2. An older age (p < 0.001), a history of a difficult airway (p = 0.005), limited neck extension (p < 0.001), and a higher Pediatric Index of Mortality 2 (PIM 2) score (p < 0.0001) were all associated with an increased use of VL compared with DL. Diagnostic categories of upper respiratory (9.3% DL vs 15.2% VL), lower respiratory (32.6% DL vs 40.4% VL), neurologic (17.8% DL vs 19.7% VL), and trauma (1.9% DL vs 3.2% VL) were associated with increased use of VL (p < 0.001). Tl for ventilation failure (odds ratio [OR], 1.28; 95% Cl, 1.12–1.47; p < 0.001) and for an elective procedure (OR, 1.19; 95% Cl, 1.01—1.41; p = 0.048) were also associated with increased VL use compared with DL. In contrast, Tl for unstable hemodynamics (OR, 0.38; 95% Cl, 0.29—0.51; p < 0.001) or therapeutic hyperventilation (OR, 0.28; 95% Cl, 0.12–0.69; p = 0.003) were associated with a lower use of VL compared with DL.
table 2.
Univariate Odds Ratio of Using Video Laryngoscopy Versus Direct Laryngoscopy
| Characteristics | ORa | 95% Cl | p |
|---|---|---|---|
| Difficult airway | |||
| History of a difficult airway | 1.30 | 1.08–1.57 | 0.005 |
| Limited neck extension | 2.34 | 1.85–2.95 | <0.001 |
| Upper airway obstruction | 0.92 | 0.74–1.15 | 0.475 |
| Short thyromental distance < 3 vs ≥ 3 | 0.97 | 0.81–1.16 | 0.729 |
| Midface hypoplasia | 1.09 | 0.72–1.67 | 0.680 |
| Limited mouth opening < 3 vs ≥ 3 | 1.01 | 0.85–1.20 | 0.920 |
| Indication for tracheal intubation | |||
| Oxygen failure | 0.99 | 0.86–1.14 | 0.888 |
| Ventilation failure | 1.28 | 1.12–1.47 | <0.001 |
| Therapeutic hyperventilation | 0.28 | 0.12–0.69 | 0.003 |
| Neuromuscular weakness | 0.93 | 0.62–1.39 | 0.708 |
| Impaired airway reflex | 1.10 | 0.86–1.42 | 0.454 |
| Elective procedure | 1.19 | 1.01–1.41 | 0.048 |
| Upper airway obstruction | 0.92 | 0.74–1.15 | 0.475 |
| Pulmonary hygiene | 0.97 | 0.71–1.32 | 0.823 |
| Unstable hemodynamics | 0.38 | 0.29–0.51 | <0.001 |
| Pediatric Index of Mortality 2b | 1.02 | 1.01–1.02 | <0.001 |
OR = odds ratio.
An odds ratio (OR) > 1 favors the use of video laryngoscopy (VL) over direct laryngoscopy (DL); likewise, an OR < 1 favors the use of DL over VL.
Predicted mortality (%) was used. The calculated OR reflects each 1% increase in Pediatric Index of Mortality 2 predicted mortality. Boldface type denotes statistical significance.
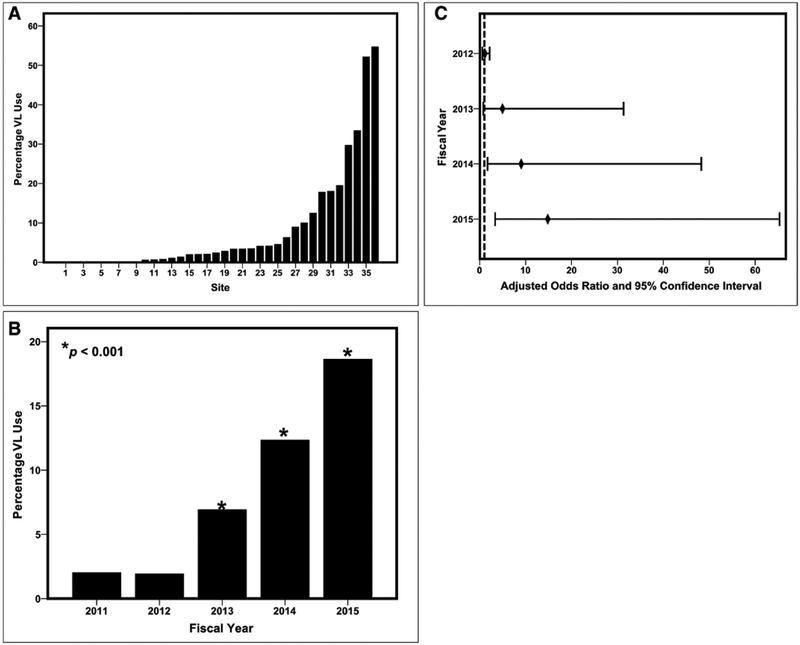
Use of VL by Site and Year
There is a wide variation in VL use among PICUs in the NEAR-4KIDS registry (Fig. 2A). The median use of VL is 2.6% with a range of 0–54.7% (IQR, 0.3–9.5%). The use of VL increased throughout the study period (Fig. 2B). The baseline rate of VL use was 1.97% in fiscal year (FY) 2011 and increased to 12.3% (p < 0.001) and 18.6% (p < 0.001) in FY 2014 and FY 2015, respectively. Multivariable analyses of VL use by academic year while adjusting for patient and provider characteristics demonstrated the gradual increase for VL use over the duration of the study. Figure 2C shows that the adjusted ORs for VL use with FY 2011 as the baseline.
Figure 2.
Percentage of video laryngoscopy (VL) use for tracheal intubation (Tl) by participating PICU or cardiac ICU. A, There is a wide range in use of VL versus direct laryngoscopy (DL) for Tl across PICUs participating in the National Emergency Airway Registry for Children study. The distribution is a non parametric distribution with a right-skew. The median for VL use is 3% with a range of 0–55%. B, The use of VL increased from 1.97% in fiscal year (FY) 2011 to 12.3% (p < 0.001) and 18.6% (p < 0.001) in FY 2014 and FY 2015, respectively. C, Adjusted odds ratio of VL use over study time period compared with FY 2011. The vertical dashed line at 1.0 represents no difference in the use of VL versus DL by FY compared with FY 2011. The percentage of VL increased significantly from FY 2011 to FY 2014 and FY 2015.
Outcomes of VL Versus DL for Tis
A total of 1,501/8,875 TIs (16.9%) were associated with adverse TIAEs; 1,054 TIs (11.9%) were with nonsevere TIAEs and 574 (6.5%) were with severe TIAEs. One hundred twenty-four TIs (1.3%) experienced both severe and nonsevere TIAEs. Adverse TIAEs were observed significantly less often in TIs with VL (60/928; 6.5%) versus TIs with DL (994/7,947; 12.5%) (OR, 0.56; 95% Cl, 0.45–0.70; p < 0.001). The occurrence of severe TIAEs were not significantly different among TIs with VL (47/928; 5.1%) versus TIs with DL (527/7,947; 6.6%) (OR, 0.75; 95% Cl, 0.54–1.02; p = 0.067). The use of VL was significantly associated with lower odds of mainstem bronchial intubation (OR, 0.40; 95% Cl, 0.22–0.74; p = 0.003), esophageal intubation with immediate recognition (OR, 0.49; 95% Cl, 0.34–0.69; p < 0.001), and dysrhythmia (OR, 0.36; 95% Cl, 0.15–0.88; p = 0.019); however, overall severe TIAE, multiple attempts at TI, and desaturation less than 80% were not associated with a difference in percentage of VL versus DL use, as shown in Table 3.
table 3.
Univariate Outcomes of Using Video Laryngoscopy Versus Direct Laryngoscopy
| Outcomea | OR | 95% CI | p |
|---|---|---|---|
| Any TIAE, n (%) | 0.56 | 0.45–0.70 | <0.001 |
| Nonsevere TIAE, n (%) | 0.48 | 0.36–0.63 | <0.001 |
| Mainstem bronchial intubation | 0.40 | 0.20–0.74 | 0.001 |
| Esophageal intubation with immediate recognition | 0.49 | 0.33–0.69 | <0.001 |
| Emesis without aspiration | 0.75 | 0.23–1.86 | 0.68 |
| Hypertension requiring medication | 2.34 | 0.42–8.88 | 0.17 |
| Epistaxis | 1.98 | 0.36–7.22 | 0.23 |
| Lip trauma | 0.52 | 0.10–1.63 | 0.36 |
| Medication error | 0 | 0.00–4.12 | 1.00 |
| Dysrhythmia | 0.36 | 0.11–0.87 | 0.017 |
| Delayed intubation due to pain/agitation requiring additional medication | 0.71 | 0.08–2.88 | 1.00 |
| Severe TIAE, n (%) | 0.75 | 0.54–1.02 | 0.067 |
| Cardiac arrest | |||
| Survived | 0.83 | 0.38–1.60 | 0.76 |
| Death | 0.37 | 0.09–2.29 | 0.51 |
| Esophageal intubation with delayed recognition | 1.14 | 0.29–3.25 | 0.78 |
| Emesis with aspiration | 0.72 | 0.23–1.79 | 0.68 |
| Hypotension requiring intervention | 0.50 | 0.29–0.82 | 0.004 |
| Laryngospasm | 2.26 | 0.66–6.28 | 0.10 |
| Malignant hyperthermiaa | NA | NA | NA |
| Pneumothorax/pneumomediastinum | 0 | 0.00–2.35 | 0.39 |
| Direct airway injury | 0.86 | 0.02–6.03 | 1.00 |
| Dental trauma | 2.23 | 0.82–5.26 | 0.08 |
| ≥ 3 Attempts | 0.87 | 0.70–1.07 | 0.19 |
| Desaturation < 80%b | 0.99 | 0.83–1.19 | 0.94 |
NA = not applicable; OR = odds ratio; TIAE = tracheal intubation adverse event.
There were no episodes of malignant hyperthermia reported.
Desaturation was defined as lowest Spo2 < 80% during the course when the oxygen saturation was ≥ 90% after preoxygenation and without preexisting cyanotic heart disease. See “Methods” section in the article.
Boldface type denotes statistical significance.
Multivariable Analyses: VL Versus DL for the Occurrence of TIAEs and Multiple Attempts
Finally, we performed a multivariable analysis that considered all univariate patient characteristics that were associated with the use of VL that included age, a history of a difficult airway, limited neck mobility, ventilation failure, therapeutic hyper-ventilation, unstable hemodynamics, and TI for an elective procedure. Provider characteristics (resident vs nonresident airway provider) and a secular trend were also included in the model. The adjusted OR of any TIAE is lower when comparing the use of VL with DL (OR, 0.57; 95% Cl, 0.42–0.77; p < 0.001). After adjusting for covariates, there was no significant decrease in the odds of severe TIAE (OR, 0.86; 95% Cl, 0.56–1.32; p = 0.49) or multiple attempts (OR, 0.93; 95% Cl, 0.71–1.22; p = 0.59) with the use of VL, as shown in the Supplemental Figure (Supplemental Digital Content 2, http://links.lww.com/PCC/A422; legend, Supplemental Digital Content 3, http://links.lww.com/PCC/A423).
DISCUSSION
This is the largest study to date describing the use of VL compared with DL in 36 international PICUs. Although there is a large range of VL use in critically ill children admitted to ICUs, the use of VL increased over the 5-year study period, and VL was more frequently used in older children, in children with a higher PIM 2 score, or in children with a history of a difficult airway. Consistent with our primary hypothesis, the use of VL increased from inception of the database until present. The use of VL was more common in children with higher severity of illness and with respiratory indications. In addition, the use of VL was associated with a significant decrease in the odds of experiencing any TIAE after we adjusted for differences in patient characteristics. Specifically, the VL use was associated with lower odds of mainstem bronchial intubation, esophageal intubation with immediate recognition, and dysrhythmia. However, we did not detect a decrease in the odds of experiencing a severe TIAE or a decrease in the need for greater than or equal to three attempts at TI when using VL as compared with DL. It is likely that our study was not adequately powered to detect a significant difference in severe TIAE when comparing the use of VL with DL, given the low occurrence rate of severe TIAEs (6.5%) and the baseline differences in patient and provider characteristics between the cohorts for which we needed to account. Results from this study provide the framework for future comparative or quasi-experimental studies on the primary use of VL in diverse PICUs and CICUs. This study results also highlight potential educational opportunities with VL to teach TI to pediatric trainees and frontline clinicians in academic settings.
Results from our study are consistent with literature reported from adult ICUs on the use of VL versus DL. Several single-institution adult studies have demonstrated that VL increases first-attempt success at TI, improves the grade view of the glottis inlet, and increases the ultimate success of TI (5,6,14–22). In a meta-analysis by Su et al (7), in comparison with DL, VL gave a better view of the glottis, had a similar rate of TI success, and decreased the time taken for difficult TI. A second large systematic review and meta-analysis by De Jong et al (4) comparing the use of VL (n = 1,066) with DL (n = 1,067) in adult ICUs demonstrated that VL significantly reduced the odds of difficult oral TI, Cormack grades 3 or 4, and esophageal intubation. The OR of first-attempt success of oral ‘TI was increased in this meta-analysis by De Jong et al (4); however, there was no change in the odds of severe hypoxemia, airway injury, or severe cardiovascular collapse. Silverberg et al (22) reported that use of the Glidescope VL was superior to DL for first-attempt success at urgent Tl and that there was no difference in esophageal intubation, aspiration events, hypotension, or oxygen desaturation events.
In a meta-analysis of the 14 randomized control trials comparing VL with DL in children as performed by anesthesiologists in the operating room, Sun et al (23) report that although VL improved glottis visualization in all children, their analysis indicated that it took longer to intubate using VL and that there was a higher relative risk of failing to intubate. Of note, there was no difference in the first-attempt success or associated complication rates between VL and DL (23). In contrast, Donoghue et al (24) has shown that VL is associated with greater first-attempt success during intubation by pediatric emergency physicians on an adult simulator. Previously, NEAR4KIDS investigators have reported that only 2% of all intubations across the 15 PICUs studied involved the use of indirect laryngoscopy (3). Furthermore, VL use by pediatric critical care physicians has not been compared with the DL with respect to type of VL used, intubation success, time to intubation, quality of glottic exposure (grades of view obtained), TIAE, and trends over time. The current study using the NEAR4KIDS database closes this gap in knowledge regarding the use of VL compared with DL in diverse PICUs.
Although cost is a primary barrier for adoption of indirect laryngoscopy tools such as VL, adult studies have shown that adoption of VL is proceeding more rapidly than predicted based on a typical technology adoption life-cycle (25). Studies in the operating room have shown that anesthesia residents can learn VL quickly and inexperienced anesthesiologists had higher success rates and shorter intubation times using VL (26). Adult studies in the critical care literature indicate that VL decreases the learning curve at performing Tl and closes the gap between less experienced and seasoned physicians at performing urgent endotracheal intubations (27). Importantly, at teaching institutions, VL allows for a supervising physician to direct a learner during the course of Tl and to confirm ETT placement by direct visualization of the ETT passing through the vocal cords on the video monitor. We believe that the rapid adoption of VL in the PICUs across the country may be due to the use of VL as an invaluable teaching tool.
Participation in the NEAR4KIDS registry is voluntary, and data entered into the database are subject to recall and reporting bias. Because of the possibility of a higher degree of motivation required to participate in a national QI initiative, participating centers may be more proficient at performing TIs. Reporting bias is minimized by the strict compliance required with being a member of the NEAR4KIDS registry. This study is also limited by the retrospective analysis of pro-spectively collected data on the use of VL compared with DL, and the selection of patients to receive VL versus DL is subject to bias. For example, our results show that there is a clear preference toward using DL over VL to intubate more severely ill patients with hemodynamic instability or neurologic deterioration. Although we attempted to account for this selection bias in our multivariable analysis using PIM 2 score and primary diagnostic category, only a future randomized study of patients receiving VL versus DL would be able to control for such selection bias. Although a significant decrease in the odds of having hypotension requiring intervention was associated with VL use in our univariate analysis, DL was used more frequently in TIs in patients with shock. We speculate that this association was confounded by the patient condition. It is likely that the patient preparation and choice/doses of medication might play a larger role in the occurrence of hypotension during TIs rather than the choice of device. However, due to a limited sample size and infrequency of hypotension requiring intervention, we were not able to evaluate this association further. There is a learning curve to use VL, and our study was not able to account for each provider’s experience in VL use, and the lack of capturing the experience of VL use could attenuate the impact of VL to decrease severe TIAEs and multiple attempts. The type of VL device may also impact the Tl outcomes because the intubation technique and learning curve of providers are likely different among various VL devices. Unfortunately, the earliest version of the NEAR4KIDS registry did not include reporting of the type of VL device, resulting in an inability to report this information in 12% of the Tl performed using VL. It is unclear whether the higher use of VL to intubate older children is a consequence of the lack of availability of equipment for infants in some participating sites, since this data point was not collected in the registry. In addition, the C-MAC video laryngoscope (Karl-Storz) may be used to perform DL and/or indirect laryngoscopy. Whether the video image was actually used by the primary airway provider performing the intubation was not prospectively collected until October 2015. Nevertheless, this study is to date the largest, multicenter pediatric study describing the primary use of VL in children admitted to PICUs and CICUs. Future studies should focus on defining patient characteristics that constitute appropriate VL indications and how VL would be best utilized in academic settings, that is, airway provider using the direct view versus supervising physician viewing the video image to coach trainees.
CONCLUSIONS
Analysis of the NEAR4KIDS database has shown that the primary use of VL increased over the time; however, substantial variance in VL use exists across PICUs. The primary use of VL was significantly associated with lower occurrence of any adverse TIAE even after adjusting for patient characteristics. Further studies are needed to evaluate clinical impact of primary VL use in multiple PICUs.
Supplementary Material
ACKNOWLEDGMENT
We thank Hayley Buffman, MPH, and Stephanie Tuttle, MBA, for their administrative support.
Dr. Grunwell is supported by National Institute of Health (NIH) T32G M 095442. The NIH had no role in the design, collection, analysis, and interpretation of data, writing of the article, or the decision to submit this article for publication. Dr. Lee’s institution received funding from Covidien, and he received funding from KK Women’s and Children’s Hospital. Dr. Shults was supported by Agency for Healthcare and Research Quality (AHRQ) R18HS022464, AHRQ R 18H S024511.
Drs. Nadkarni and Nishisaki were supported by AHRQ R03HS021583, AHRQ R18HS022464, AHRQ R 18H S024511, and the Endowed Chair, Critical Care Medicine, The Children’s Hospital of Philadelphia. Dr. Nishi-saki’s institution received funding from AHRQ R03HS021583, AHRQ R18HS022464, and AHRQ R18H S024511. The remaining authors have disclosed that they do not have any potential conflicts of interest.
Footnotes
A full list of the National Emergency Airway Registry for Children (NEAR4KIDS) Network is supplied in eTable 1 (Supplemental Digital Content 1, http://links.lww.com/PCC/A421).
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/pccmjoumal).
REFERENCES
- 1.Li S, Rehder KJ, Giuliano JS Jr, et al. : Development of a quality improvement bundle to reduce tracheal intubation-associated events in pediatric ICUs. Am J Med Qual 2016; 31 :47–55 [DOI] [PubMed] [Google Scholar]
- 2.Nett S, Emeriaud G, Jarvis JD, et al. ; NEAR4KIDS Investigators and Pediatric Acute Lung Injury and Sepsis Investigators (PALISI) Network: Site-level variance for adverse tracheal intubation-associated events across 15 North American PICUs: A report from the national emergency airway registry for children. Pediatr Crit Care Med 2014; 15:306–313 [DOI] [PubMed] [Google Scholar]
- 3.Nishisaki A, Turner DA, Brown CAIII, et al. ; National Emergency Airway Registry for Children (NEAR4KIDS); Pediatric Acute Lung Injury and Sepsis Investigators (PALISI) Network: A National Emergency Airway Registry for children: Landscape of tracheal intubation in 15 PICUs. Crit Care Med 2013; 41 :874–885 [DOI] [PubMed] [Google Scholar]
- 4.De Jong A, Molinari N, Conseil M, et al. : Video laryngoscopy versus direct laryngoscopy for orotracheal intubation in the intensive care unit: A systematic review and meta-analysis. Intensive Care Med 2014. ;40 :629–639 [DOI] [PubMed] [Google Scholar]
- 5.Jones BM, Agrawal A, Schulte TE: Assessing the efficacy of video versus direct laryngoscopy through retrospective comparison of 436 emergency intubation cases. J Anesth 2013; 27:927–930 [DOI] [PubMed] [Google Scholar]
- 6.Sakles JC, Mosier J, Chiu S, et al. : A comparison of the C-MAC video laryngoscope to the Macintosh direct laryngoscope for intubation in the emergency department. Ann Emerg Med 2012; 60:739–748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Su YC, Chen CC, Lee YK, et al. : Comparison of video laryngoscopes with direct laryngoscopy for tracheal intubation: A meta-analysis of randomised trials. Eur J Anaesthesiol 2011. ; 28:788–795 [DOI] [PubMed] [Google Scholar]
- 8.Brown CA III, Bair AE, Pallin DJ, et al. ; NEAR III Investigators: Techniques, success, and adverse events of emergency department adult intubations. Ann Emerg Med 2015; 65:363–370.e1 [DOI] [PubMed] [Google Scholar]
- 9.Kaplan MB, Hagberg CA, Ward DS, et al. : Comparison of direct and video-assisted views of the larynx during routine intubation. J Clin Anesth 2006; 18:357–362 [DOI] [PubMed] [Google Scholar]
- 10.Nishisaki A, Ferry S, Colborn S, et al. ; National Emergency Airway Registry (NEAR); National Emergency Airway Registry for kids (NEAR4KIDS) Investigators: Characterization of tracheal intubation process of care and safety outcomes in a tertiary pediatric intensive care unit. Pediatr Crit Care Med 2012; 13:e5–e10 [DOI] [PubMed] [Google Scholar]
- 11.Nishisaki A, Marwaha N, Kasinathan V, et al. : Airway management in pediatric patients at referring hospitals compared to a receiving tertiary pediatric ICU. Resuscitation 2011; 82:386–390 [DOI] [PubMed] [Google Scholar]
- 12.Graciano AL, Tamburro R, Thompson AE, et al. : Incidence and associated factors of difficult tracheal intubations in pediatric ICUs: A report from National Emergency Airway Registry for Children: NEAR4KIDS. Intensive Care Med 2014; 40:1659–1669 [DOI] [PubMed] [Google Scholar]
- 13.Pepe MS, Anderson GL: A cautionary note on inference for marginal regression models with longitudinal data and general correlated response data. Commun Stat Simul Comput 1994; 23:939–951 [Google Scholar]
- 14.Aziz MF, Dillman D, Fu R, et al. : Comparative effectiveness of the C-MAC video laryngoscope versus direct laryngoscopy in the setting of the predicted difficult airway. Anesthesiology 2012; 116:629–636 [DOI] [PubMed] [Google Scholar]
- 15.Jungbauer A, Schumann M, Brunkhorst V, et al. : Expected difficult tracheal intubation: A prospective comparison of direct laryngoscopy and video laryngoscopy in 200 patients. Br J Anaesth 2009; 102:546–550 [DOI] [PubMed] [Google Scholar]
- 16.Mort TC, Braffett BH: Conventional versus video laryngoscopy for tracheal tube exchange: G lottic visualization, success rates, complications, and rescue alternatives in the high-risk difficult airway patient. Anesth Analg 2015; 121:440–448 [DOI] [PubMed] [Google Scholar]
- 17.Lee DH, Han M, An JY, et al. : Video laryngoscopy versus direct laryngoscopy for tracheal intubation during in-hospital cardiopulmonary resuscitation. Resuscitation 2015; 89 :195–199 [DOI] [PubMed] [Google Scholar]
- 18.Noppens RR, Geimer S, Eisel N, et al. : Endotracheal intubation using the C-MAC® video laryngoscope or the Macintosh laryngoscope: A prospective, comparative study in the ICU. Crit Care 2012; 16:R103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kory P, Guevarra K, Mathew JP, et al. : The impact of video laryngos-copy use during urgent endotracheal intubation in the critically ill. Anesth Analg 2013; 117:144–149 [DOI] [PubMed] [Google Scholar]
- 20.Sakles JC, Mosier JM, Chiu S, et al. : Tracheal intubation in the emergency department: A comparison of GlideScope® video laryngos-copy to direct laryngoscopy in 822 intubations. J Emerg Med 2012; 42:400–405 [DOI] [PubMed] [Google Scholar]
- 21.Sakles JC, Patanwala AE, Mosier JM, et al. : Comparison of video laryngoscopy to direct laryngoscopy for intubation of patients with difficult airway characteristics in the emergency department. Intern Emerg Med 2014; 9:93–98 [DOI] [PubMed] [Google Scholar]
- 22.Silverberg MJ, Li N, Acquah SO, et al. : Comparison of video laryngos-copy versus direct laryngoscopy during urgent endotracheal intubation: A randomized controlled trial. Crit Care Med 2015; 43:636–641 [DOI] [PubMed] [Google Scholar]
- 23.Sun Y, Lu Y, Huang Y, et al. : Pediatric video laryngoscope versus direct laryngoscope: A meta-analysis of randomized controlled trials. Paediatr Anaesth 2014; 24:1056–1065 [DOI] [PubMed] [Google Scholar]
- 24.Donoghue AJ, Ades AM, Nishisaki A, et al. : Videolaryngoscopy versus direct laryngoscopy in simulated pediatric intubation. Ann Emerg Med 2013; 61:271–277 [DOI] [PubMed] [Google Scholar]
- 25.Raja AS, Sullivan AF, Pallin DJ, et al. : Adoption of video laryngoscopy in Massachusetts emergency departments. J Emerg Med 2012; 42:233–237 [DOI] [PubMed] [Google Scholar]
- 26.Howard-Quijano KJ, Huang YM, Matevosian R, et al. : Video-assisted instruction improves the success rate for tracheal intubation by novices. Br J Anaesth 2008; 101:568–572 [DOI] [PubMed] [Google Scholar]
- 27.Paolini JB, Donati F, Drolet P: Review article: Video-laryngoscopy: Another tool for difficult intubation or a new paradigm in airway management? Can J Anaesth 2013; 60:184–191 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.