Abstract
Objective:
To test the effects of weekly SMS for improving infant feeding practices and infant weight.
Methods:
This was a multi-site randomized clinical trial in a convenience sample of 202 caregivers of healthy term infants 0-2 months participating in the WIC program in Puerto Rico and Hawaii. Participants were randomized to receive SMS about infant’s general health issues (control) or SMS for improving feeding practices (intervention) for four months. Weight, length and infant feeding practices were assessed at baseline and four months later.
Results:
A total of 170 participants completed the study (n=86 control and n=84 intervention). Baseline characteristics were similar between groups. At the end, exclusive breastfeeding rates were similar between groups (67.4% control and 59.1% intervention). Introduction of other foods and beverages, addition of foods to the bottle, placing infants to sleep with milk bottles, caregiver’s method and response to feeding infants and distractions while feeding infants were similar between groups. Also, weight status or rate of weight gain was similar between groups.
Conclusion:
There were no significant improvements in feeding practices or in weight with the intervention. The timeline of the messages in relation to the targeted behavior may have affected the effectiveness of the intervention. Earlier dissemination of messages, higher level of intensity, longer intervention, additional contacts and inclusion of other caregivers may be needed to achieve the desired effects.
Keywords: infant, mobile messages, feeding practices, weight, intervention
Introduction
Infant obesity is higher among Hispanics (14.8%) and Native Hawaiians (11.4%) compared to any other group (Blacks 8.7% and Whites 8.4%) (1). In addition, compared to White infants, Hispanic infants experience rapid weight gain in infancy (2,3). These trends among these minority infants are of great concern, as the first 1,000 days of life (conception-24 months) are crucial for healthy growth and development (4). Infant rapid weight gain increases the risk of obesity later in life (5–7), particularly if the rapid weight gain occurs in the first 6 months (8). In addition, Puerto Rico (PR) and Hawaii (HI) lead the US in several chronic diseases, such as diabetes and hypertension (9). Unhealthful lifestyles and poor health education may underlie many of these chronic diseases (i.e. obesity, diabetes, hypertension) as evidenced by the low intake of fruits, vegetables, low-fat dairy products and fiber in these populations (10–13) and the low diet quality, even among infants (10,14).
Certain infant feeding practices are related to adequate weight gain, such as exclusive breastfeeding for 6 months (8), which is very low (18%) among both Hispanics and Native Hawaiians (15,16). Responsive feeding, which refers to the parent’s ability to identify and appropriately respond to infant hunger cues, also appears to be associated with infant weight, as reported in a systematic review (17). In this review, three out of nine studies provided strong support for response feeding, evaluated as maternal responses to satiety cues and/or bottle-emptying behaviors, with infant growth. Therefore, more studies are needed to understand this. Other factors include early introduction of solid foods, quality and quantity of foods being offered (18–21), formula feeding and feeding on schedule (22).
The few behavioral interventions conducted to date among caregivers have found significant improvements in breastfeeding (23), introduction of solid foods (23), general diet quality (24) and response feeding (25) but none have found significant improvements in infant weight gain (24–28). This lack of impact on weight could be due to the low number of participants, low compliance and adherence and the focus on increasing knowledge without increasing skills (29). Also, most interventions include group-based sessions or home visits, which are resource intensive with high burden for participants and researchers and not easily translatable. These barriers may be addressed with interventions using Short Message Service (SMS), which could be cost-effective, sustained over time and embedded into programs such as the Women, Infants and Children (WIC).
To our knowledge, there are only two SMS based interventions for improving infant feeding patterns and/or weight (30,31) and none have been conducted among US minorities. One such intervention used weekly SMS about infant feeding from late pregnancy until 12 months’ postpartum among mothers in China, with a significant positive impact in breastfeeding duration and in the introduction of solid foods compared to the control group (30). The other study sent weekly SMS for 8 weeks to mothers of infants younger than 3 months in Australia with significant impact in exclusive breastfeeding compared to the control group (31). SMS based intervention can be effective among low-income new mothers (32), a group with poor infant outcomes and more difficult to reach with traditional methods, but also more likely to use SMS. However, several limitations have been identified in studies using SMS, such as a lack of behavioral theories guiding their messages, use of informational instead of motivational messages, delivery of SMS at the same time of day, lack of alignment between content and research outcomes and lack of a control group (32,33). Therefore, to address these limitations, we conducted a feasibility trial to test weekly SMS sent to caregivers of infants for improving feeding practices and weight. For this trial, we used a behavioral theory for informing the messages, aligned the messages with the research outcomes, sent the SMS at different times, included a control group and included groups at high risk of obesity, such as Hispanics and Native Hawaiians, as the target.
Materials and Methods
Design
This was a multi-site feasibility trial to pilot test weekly SMS sent to caregivers of infant’s participants of the WIC program in PR and HI for improving feeding practices and preventing excessive weight gain in infants for 4 months. All activities occurred at the WIC clinics in both sites. Details of study methods have been previously published (34).
Setting and Participants
A total of 202 caregivers of infants 0-2 months old participating in the WIC program in PR (n=100) and HI (n=102) were recruited in 2017. Eligibility criteria included: caregiver must be 18 years or older, owner of a mobile phone with unrestricted SMS capability, responsible for infant care, and willing to participate for the full study duration. Exclusion criteria included: infants with special diets, infants with limited mobility, pre-term birth (<37 weeks), small or large for gestational age (birthweight <10th or >90th percentile), inability to consent to participate, unwillingness to be randomized and not being able to read. The institutional review boards at the University of Puerto Rico, Medical Sciences Campus and University of Hawaii in Manoa approved study procedures and participants signed an informed consent form.
Randomization
Participants were recruited from 2 WIC clinics in PR and 4 WIC clinics in HI (34). WIC clinics were selected based on availability and accessibility to the investigators, with the help of the WIC program in each site. Equal numbers of caregivers were randomized to the control arm (SMS about general infant’s health issues) or to the intervention arm (SMS for improving feeding practices) using random block sizes (2, 4 or 6) with 26 total blocks. A computer-generated list of randomization numbers and corresponding ID was created; participants were allocated an ID sequentially as they were recruited and this ID was matched with the randomized group. Among those randomized to the intervention arm, participants were assigned either to the lactation or formula intervention group, based on their initial feeding status.
Delivery of Intervention
Intervention SMS were created based on the TransTheoretical Model (TTM) of health behavior change (35) and focused on reinforcing WIC messages on breastfeeding, preventing overfeeding, delaying introduction of solid foods, and delaying and reducing baby juice consumption. Messages presented in WIC regarding infant feeding practices are produced by the United States Department of Agriculture’s Food and Nutrition Service. Messages undergo a peer-reviewed process and are consistent with population-based approaches and recommendations from expert organizations, such as the American Academy of Pediatrics. According to the TTM, individuals undertaking changes in health behaviors progress through a series of stages, from pre-contemplation to maintenance (35). Constructs in the TTM were used to address key determinants of behavioral change to ensure relevance to the audience, and targeted individuals both at the earlier and later stages of change. For example, barriers to change may prevent individuals in the earlier stages of change from breastfeeding; thus, messages provided both information on the benefits of performing the behavior, such as “Breastfeeding is the best way to feed your baby, but it may be hard. Put your baby to your breast and you will have more milk”, and simple, practical suggestions for initiating the behavior, such as “When breastfeeding, make sure the nipple and the area around is inside baby’s mouth. If baby eats from the tip, they will break. Always correct the position”.
Control SMS were related to general infant’s health issues related to sleeping, bathing, teething, traveling in a car, medications, handling baby, and smoking, information related to immunization, and care of common illnesses.
SMS were sent automatically using a web-based SMS messaging platform from the time the participant enrolled in the study until the end (4 months later). A total of 18 messages (1 per week for 4 months) were sent. All messages were written at a grade 5-level in Spanish for PR or English for HI. Each message was about 35-50 words long and sent on different days and times of the week to help prevent the participants from ignoring the messages over time. As messages were sent, a record of the message and time sent for each participant appeared on the study website. It was also possible to view the status of messages sent to each participant through a delivery report showing whether a message bounced or was delivered. Also, to learn if messages were being read, we sent 7 short questions via SMS about the intervention every 2 weeks. These responses were recorded. A more detailed description of the intervention is published elsewhere (34).
Both groups received the WIC standard of care, which includes a certification visit when infants first start the program (usually around 0-2 months) and re-certification visits at 6 months and 12 months (36). During these certification visits, the Value Enhanced Nutrition Assessment (VENA) platform (USDA, 2006)(37) is completed to evaluate each participant in a standardized way in all states. Based on the answers to the different questions required as part of VENA, the system uses an algorithm to detect nutritional and self-care risks that require individualized nutritional intervention through the program or referral to other services (i.e., Social Work). Those identified as high risk may need to complete additional visits to follow their progress. In addition to these visits, each state must follow the 7 CFR 246.11 - Nutrition education WIC Regulation (38), in which participants are required to complete at least 2 nutrition education sessions within every 6 months’ re-certification period.
Measures
All measures were completed at baseline and at the end of the trial at the WIC clinics.
-Infant feeding practices.
A trained interviewer administered a feeding practices questionnaire about type of infant feeding (breast or bottle-feeding), type of milk used (breast, formula or other), age of discontinuing breastfeeding (exclusive and partial), age of introduction of juices and solid foods, use of the bottle to put the baby to sleep, methods of feeding the baby (i.e. using spoon, adding foods to bottle, etc.), caregiver’s response to bottle feeding (i.e. encouraging baby to drink it all or some more, or discontinuing the feeding) and distractions during feeding (i.e. using screens, with the rest of the family or none).
-Excessive weight gain.
Trained research personnel assessed the infant’s length and weight (34). Weight-for-length z score (WHLz) was calculated at each time point using the WHO AnthroPlus macro (34), which is based on the WHO growth charts standardized for age and sex (40). An adequate WHLz is defined by the WHO as a z-score within ± 2 standard deviations (SD); A z-score >2 SD indicates obesity, while <2 SD indicates malnutrition (40). Weight gain between the initial assessment (at 0-2 months) and the final assessment (at 4-6 months) was defined as (40):
-
-
Rapid, if the change in weight-for-length z-score was >0.67 SD;
-
-
Adequate, if the change in weight-for-length z-score was between −0.67 and 0.67 SD;
-
-
Slow, if the change in weight-for-length z-score was <−0.67 SD.
-Socio-demographics and general health questions.
This questionnaire was completed by participants and included questions about age, gender, education, occupation, type of insurance, pre-pregnancy weight, gestational weight gain, gestational age, use of pre-natal vitamins, use and availability of a breast pump, breastfeeding support, infant’s age and sex, type of pediatric center, WIC center, and immunization record.
Statistical plan
A sample size of 200 participants (100 per group) achieves 80% power at a 0.05 significance level to detect the effect size of 0.40 in the difference of 4-week changed continuous outcome variables (34).
Baseline characteristics were summarized and compared between the two study arms using two sample t-tests for continuous variables and chi-square tests for categorical variables. A series of logistic regression analyses were performed to determine group (intervention and control) difference in the dependent variables (feeding practices and excessive weight gain), separated by visits. The effect of the intervention on study outcomes was determined by the interaction term between the visit time (coded as baseline=0 and week 4=1) and study arms in order to test if there were any differences in the change of the outcomes between study groups. Subgroup analyses were performed among those that were breastfeeding initially. Also, subgroup analyses were conducted by site (Puerto Rico and Hawaii) and by age (<1 month and ≥1 month). All statistical models included site as a covariate to control for the potential difference effects across sites (i.e., heterogeneity due to unmeasured confounding or effect-modifying factors). SAS (version 9.3) was used for statistical analyses. Significance testing was set at a P value of <0.05.
Results
A total of 423 caregivers and infants were screened for eligibility; 221 (52%) did not meet inclusion criteria (mainly pre-term birth or small/large for gestational age) or declined to participate (Figure 1). Therefore, 202 eligible participants were randomized into the study groups (100 in control group and 102 in intervention group). There were no significant differences in baseline characteristics between groups (Table 1). This pattern persisted irrespective of site, implying that the randomized allocation to the groups was properly performed in both sites. Overall, mean age of caregivers was 27±5.13 years. Virtually all caregivers were mothers (99.5%), 53.5% had some college education or more, 60% were Hispanics, and race was diverse, with 7-10% Native Americans (Table 1). All had term pregnancies and 52.5% had healthy weight before pregnancy. Gestational weight gain was within the recommended range in 42.6%, above the recommended range in 37.1% and below the recommended range in 20.3%. Most used prenatal vitamins (96.5%) and only 6.4% had diabetes during pregnancy. About half of the infants were girls (49%), mean age was 1.0±0.45 months, 83.2% had adequate BMI at birth (14.3% were underweight and 2.5% were overweight at birth), the mean BMI z score was in accordance to the healthy weight category and 52.6% went to a community health center for their health care. Study retention at the end of the trial was 84% (n=86 in the control group and n=84 in the intervention group). No significant differences in dropout rate between the groups were noted; however, we found a significant lower drop-out among whites (5.6%) compared to non-whites (22.8%; p<0.05) and among those using prenatal vitamins (14.4%) compared to non-users (57.1%; p<0.05). The other demographic variables were not associated with dropout rate.
Figure 1.
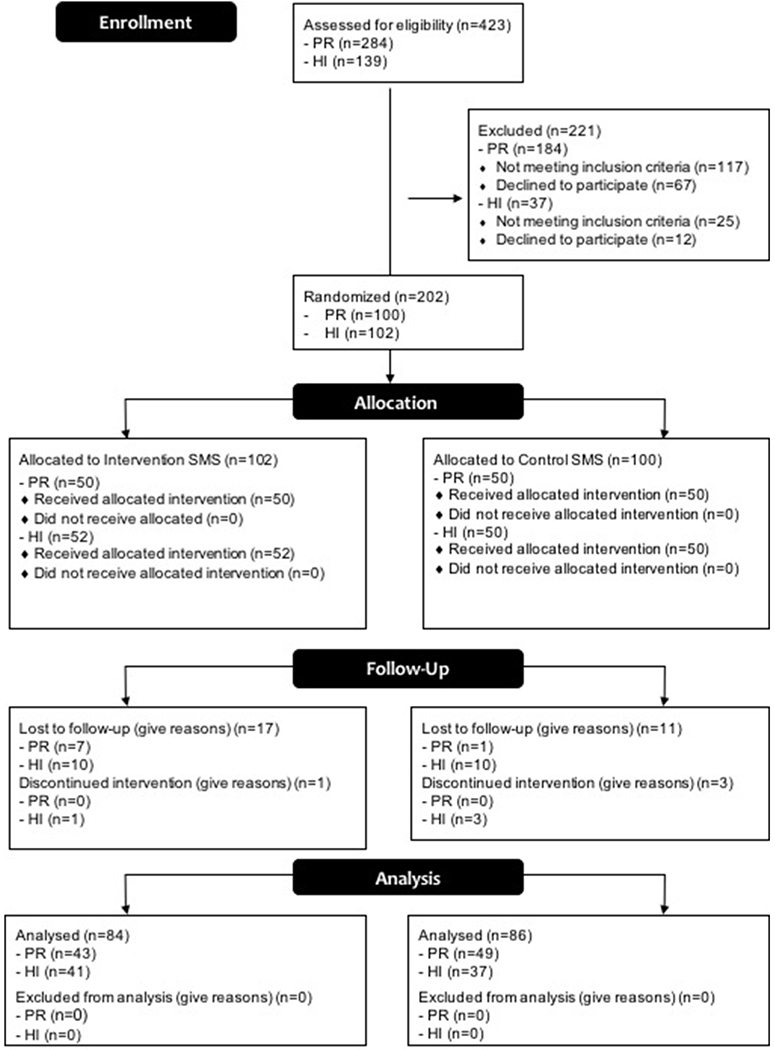
Consort diagram of the study. This figure presents a consort diagram of the study showing reasons for exclusion from the study.
Table 1.
Socio-demographic characteristics of the sample
| Control (n=100) |
Intervention (n=102) |
||||
|---|---|---|---|---|---|
| Characteristics | Mean | SD | Mean | SD | p-value* |
| Caregiver | |||||
| Age (years) | 27.0 | 5.02 | 26.9 | 5.27 | 0.861 |
| Number of children | 1.84 | 0.80 | 1.99 | 1.13 | 0.282 |
| Gestational age (weeks) | 38.9 | 1.00 | 39.0 | 1.12 | 0.327 |
| Pregnant weight gain (kg) | 12.7 | 5.53 | 12.6 | 5.08 | 0.911 |
| Ethnicity and race, n, % | |||||
| Asian | 20 | 20.0 | 22 | 21.6 | 0.813 |
| American Indian | 4 | 4.00 | 5 | 4.90 | 0.742 |
| Black | 12 | 12.0 | 15 | 14.7 | 0.561 |
| Hispanic | 60 | 61.2 | 62 | 62.0 | 0.707 |
| Native Hawaiian | 12 | 12.0 | 15 | 14.7 | 0.580 |
| Pacific Islander | 7 | 7.00 | 10 | 9.80 | 0.482 |
| White | 45 | 45.0 | 34 | 33.3 | 0.090 |
| Education | |||||
| Less than college, n, % | 42 | 42.0 | 49 | 49.5 | |
| Some college, n, % | 22 | 22.0 | 22 | 22.2 | 0.193 |
| College or higher, n, % | 36 | 36.0 | 28 | 28.3 | |
| Use of prenatal vitamins, n, % | 98 | 98.0 | 97 | 95.1 | 0.278 |
| Pre-pregnancy BMI (kg/m2) | 26.1 | 6.88 | 26.6 | 6.87 | 0.663 |
| Diabetes during pregnancy, n, % | 5 | 5.0 | 8 | 7.8 | 0.415 |
| Infant | |||||
| Gender (female), n, % | 48 | 48.0 | 51 | 50.0 | 0.781 |
| Age (months) | 0.98 | 0.47 | 0.93 | 0.44 | 0.455 |
| Weight for age z score | −0.05 | 0.85 | −0.05 | 0.85 | 0.976 |
| Length for age z score | 0.61 | 1.56 | 0.59 | 1.57 | 0.931 |
| BMI for age z score | −0.54 | 1.39 | −0.53 | 1.28 | 0.958 |
| Type of infant health center, n, % | |||||
| Health Center | 49 | 51.0 | 53 | 54.0 | 0.549 |
| Private office | 47 | 49.0 | 45 | 45.7 | |
site adjusted
All 18 messages were successfully sent over the course of the 4 months study. However, 6 participants consistently showed that messages bounced; these participants did not complete the study. In addition, 2 participants opted out of receiving messages by texting “STOP,” discontinuing their participation. An additional 4 participants had disconnected phone numbers and did not complete the trial. In terms of responding to questions sent via SMS, response from participants was greater on average for the first 4 questions (52-55%) than for the last 3 (32-34%).
Table 2 shows feeding practices at baseline and end of the trial (four months) after adjusting by site and age. Feeding practices did not differ between groups at the end of the study. However, there was a trend for a greater proportion of caregivers in the intervention group stopping the feeding when infants showed signs of being full (44.1%) compared to controls (39.5%; p=0.07). Also, it is important to note that some were already being fed while using electronics at this early age (9.4% in the control group and 21.2% in the intervention group). Results were similar when stratified by site and by age (see supplementary online material).
Table 2.
Feeding practices in the sample at baseline and end of the trial adjusted for site and age
| Feeding practices | Control |
Intervention |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Visit 1 (n=100) | Visit 2 (n=86) | p-value¥ | Visit 1 (n=102) | Visit 2 (n=84) | p-value¥ | p-value€ | |||||
| n | % | n | % | n | % | n | % | ||||
| Type of milk feeding | |||||||||||
| Breastfeeding (partial/exclusive) | 73 | 73.0 | 46 | 53.5 | 0.901 | 73 | 71.6 | 44 | 52.4 | 0.908 | 0.958 |
| Formula feeding | 27 | 27.0 | 40 | 46.5 | 29 | 28.4 | 40 | 47.6 | |||
| Introduction of beverages and foods | |||||||||||
| Water | 15 | 15.5 | 29 | 34.1 | 0.480 | 18 | 18.0 | 38 | 44.7 | 0.092 | 0.216 |
| Juice | 0 | 0 | 13 | 15.1 | 1.000 | 1 | 1.0 | 10 | 11.8 | 0.704 | 0.291 |
| Formula | 61 | 62.2 | 52 | 60.5 | 0.441 | 65 | 64.4 | 54 | 64.3 | 0.610 | 0.815 |
| Solids | 0 | 0 | 25 | 29.1 | 1.000 | 0 | 0.0 | 35 | 41.7 | 0.093 | 0.720 |
| Cow’s milk | 0 | 0 | 0 | 0 | - | 0 | 0.0 | 0 | 0.0 | ||
| Other milks | 0 | 0 | 0 | 0 | - | 0 | 0.0 | 0 | 0.0 | ||
| Addition of foods to the bottle1 | |||||||||||
| Cereal | 0 | 0 | 8 | 9.3 | 1.000 | 2 | 2.0 | 13 | 15.3 | 0.168 | 0.888 |
| Babyfood/poi | 1 | 1.01 | 5 | 5.81 | 0.124 | 0 | 0.0 | 8 | 9.4 | 0.297 | 0.815 |
| No | 98 | 99.0 | 75 | 87.2 | 0.339 | 100 | 98.0 | 66 | 78.6 | 0.095 | 0.929 |
| Placing infant to sleep with milk bottle2 | |||||||||||
| Sometimes or frequently | 18 | 18.6 | 17 | 20.7 | 0.006 | 30 | 30.6 | 27 | 32.9 | 0.088 | 0.977 |
| Never/almost never | 79 | 81.4 | 65 | 79.3 | 68 | 69.4 | 55 | 67.1 | |||
| Caregiver’s response to feeding infant | |||||||||||
| Encourage infant to drink it all/some or more | 38 | 38.4 | 34 | 39.5 | 0.954 | 44 | 43.1 | 36 | 42.4 | 0.775 | 0.950 |
| Take the bottle and feed it later | 13 | 13.1 | 14 | 16.3 | 0.960 | 17 | 16.7 | 8 | 9.4 | 0.950 | 0.544 |
| Take the bottle and stop the feeding | 39 | 39.4 | 34 | 39.5 | 0.114 | 37 | 36.3 | 37 | 44.1 | 0.424 | 0.070 |
| Have not introduced the bottle | 4 | 4.04 | 2 | 2.33 | 0.306 | 3 | 2.9 | 2 | 2.4 | 0.110 | 0.906 |
| N/A | 5 | 5.05 | 2 | 2.33 | 0.887 | 1 | 1.0 | 1 | 1.2 | 0.253 | 1.000 |
| Caregiver’s method of feeding baby3 | |||||||||||
| Mainly using a spoon | 1 | 1 | 17 | 19.77 | 0.788 | 3 | 2.9 | 28 | 34.1 | 0.057 | 0.334 |
| Mainly adding it to the bottle | 0 | 0 | 6 | 6.98 | 1.000 | 0 | 0.0 | 9 | 10.6 | 0.306 | - |
| Spoon and adding in to the bottle | 0 | 0 | 4 | 4.65 | 1.000 | 1 | 1.0 | 2 | 2.4 | 0.495 | - |
| Has not started solids | 97 | 99.0 | 59 | 68.6 | 0.788 | 98 | 96.1 | 45 | 52.9 | 0.052 | 0.980 |
| Distractions while feeding infant4 | |||||||||||
| With distractions (playing or watching screens) | 25 | 25.8 | 16 | 9.36 | 0.219 | 18 | 17.8 | 18 | 21.2 | 0.573 | 0.866 |
| While family is eating | 12 | 12.4 | 23 | 26.7 | 0.883 | 12 | 11.9 | 13 | 15.5 | 0.083 | 0.168 |
| Without distractions | 60 | 61.9 | 47 | 54.7 | 0.310 | 71 | 70.3 | 53 | 62.4 | 0.310 | 0.154 |
Among partial breastfeeding
test for change within group
test for difference in change between groups
Missing value for 1 participant in control group visit 1
Missing value for 3 participants in control group visit 1, 4 participants in intervention group visit 1, 4 participants in control group visit 2, and 2 participants in intervention group visit 2
Missing value for 2 participants in control group visit 1
Missing value for 3 participants in control group visit 1, 1 participant in intervention group visit 1
Table 3 displays weight status and weight gain over time by study groups after adjusting by age and site. No significant group differences were found in weight status at the end of the trial and with weight changes from visit 1 to visit 2 (4 months later). It is noteworthy to mention that although most infants in both groups had adequate WHLz score (70-74%) in visit 2, 26-27% were already overweight/obese and 44-52% had excessive weight gain during the four-month follow-up. When stratified by site (see supplementary online material), there was a significant decrease in the proportion of infants classified as underweight in the initial visit compared to the follow-up visit in the intervention group in Puerto Rico. In Hawaii, we found a significant decrease in the proportion of infants with adequate weight and a significant increase in the proportion of infants with overweight or obesity in both the control and intervention groups. Among infants <1 month, there was a significant decrease in the proportion of infants with adequate weight and a significant increase in the proportion of infants with overweight or obesity in the initial visit compared to the follow-up visit in both the control and intervention groups. In infants ≥1 month, there was a significant increase in the proportion of infants with overweight or obesity in the initial visit compared to the follow-up visit in both the control and intervention groups.
Table 3.
Rapid weight gain and weight status at 4-6 months and weight changes during the study, adjusted by infant’s age and site
| Weight status/weight gain | Control |
Intervention |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Visit 1 (n=100)> | Visit 2 (n=86) | p-value¥ | Visit 1 (n=102) | Visit 2 (n=84) | p-value¥ | p-value€ | |||||
| n | % | n | % | n | % | n | % | ||||
| WHL z score1 | |||||||||||
| Underweight (<−2 z score) | 9 | 9.0 | 2 | 2.4 | 0.902 | 6 | 5.9 | 0 | 0.0 | - | - |
| Adequate (>−2 to <2 z score) | 84 | 84.0 | 59 | 70.2 | 0.462 | 89 | 88.1 | 61 | 74.4 | 0.338 | 0.424 |
| Obese (>2 z score) | 7 | 7.0 | 23 | 27.4 | 0.233 | 5 | 5.0 | 21 | 25.6 | 0.565 | 0.777 |
| Change in WHL z score*2 | |||||||||||
| Slow weight change (<−.67SD change) | 23 | 27.4 | 14 | 17.3 | 0.132 | ||||||
| Adequate weight gain (−0.67SD to 0.67SD) | 24 | 28.6 | 25 | 30.9 | 0.666 | ||||||
| Excessive weight change (>0.67SD change) | 37 | 44.1 | 42 | 51.9 | 0.363 | ||||||
test for change within group
test for difference in change between groups
test for difference between groups
Missing value for 2 participants in control group visit 1 and 2 and 1 participant in intervention group visit 1 and 2
Missing value for 2 participants in control group visit 2 and 3 participants in intervention group visit 2
We also analyzed changes in feeding practices and weight status/weight gain with the intervention among infants that were only breastfeeding at the first visit (see supplementary materials). We did not see any group differences in any of the feeding practices or in weight status or weight gain.
Discussion
In this trial among caregivers of healthy term infants 0-2 months participating in the WIC program in PR and HI, weekly SMS for improving feeding practices during four months had no significant effects on feeding practices or weight.
Few dietary interventions for preventing excessive weight in infants have been effective (41,42). Effective interventions have been conducted through home visits, individual and group counseling sessions or a combination of these (43), but these are high burden, resource intensive, and not easily translatable and/or embedded into current nutrition programs. The use of SMS could address some of these limitations but alone may not be enough to promote changes in caregivers’ behaviors related to infant dietary practices, as shown in the present study. However, it could be used to complement individual contacts or sessions. For example, a trial using SMS to improve breastfeeding found that weekly SMS for 8 weeks significantly lowered the reduction in the exclusive breastfeeding rate in the intervention group (6%) compared to the comparison group (14%) after controlling for important confounders (p<0.05)(31). This intervention also included individual phone calls when mothers responded to texts about their level of distress with breastfeeding; if they were distressed, a breastfeeding counselor called them. Therefore, more intense interventions may be needed in this age group to promote behavioral changes.
The timing of the messages in relation to the targeted behavior may have affected the effectiveness of the current intervention. Interventions may need to start during pregnancy to impact the mother’s decision about breastfeeding and about other early infant feeding practices. In fact, one of the few other SMS interventions among infants focusing on breastfeeding or infant feeding advice found significant positive results when the weekly SMS started in the third trimester of pregnancy and continued 12 months post-partum (30). Mothers in the intervention group had engaged in exclusive breastfeeding longer when evaluated at 6 months (11.4 weeks) compared to the control group (8.9 weeks). Also, the intervention group had a significantly lower rate of introduction of solid foods before 4 months (adjusted OR=0.27; 95% CI, 0.08-0.94).
Other caregivers may also need to be included in the intervention, as mothers may be returning to work and leaving the infant in the care of another person. The messages could be shared with child care providers and child care centers so that infants receive consistent feeding practices. Indeed, 37% of our participants reported returning to work within 3 months. Also, more information with increased frequency may be needed to help mothers and other caregivers change some of the behaviors related to infant feeding practices. As we reported previously, 41% of participants mentioned at the end of the study that they would like to receive more messages (34).
Weight status or weight gain was also similar between groups. A longer and more intense intervention may be needed for this. However, it is worth noting that although most infants were categorized as having an adequate weight at both visits, a large proportion had excessive weight gain during this short period of time (42.9% in the control group and 52.4% in the intervention group; p>0.05). If this excessive weight gain continues, it may be enough to shift infants to the overweight/obese category. In fact, in this short period of time, we did see that 25% of infants in the control group and 21% of infants in the intervention group shifted from underweight or adequate weight to overweight/obese. Health care professionals may often ignore this early rapid weight gain if infants are still within the adequate weight range in the growth charts, but it may be the start of a new growth trajectory leading to overweight/obesity later in life. In fact, several studies have consistently shown that early excessive weight gain significantly increases the risk of obesity later in life (6,8,44–47). This is particularly important if the rapid weight gain occurs in the first 6 months of life, as it may be affecting the metabolic programming that occurs at this stage of life (8).
There are some strengths and limitations of the current trial that should be acknowledged. One of the strengths includes the design, a multi-site trial conducted in WIC clinics among a high-risk population, which improves external validity, offers greater statistical power and quicker recruitment (48). Response and retention rates were high, which is vital to ensure the power and internal validity of longitudinal research. The intervention was based on the TTM of health behavior change and focused on reinforcing the WIC feeding messages that caregivers were already receiving. Trained personnel assessed weight and length using standardized methods. A limitation is the short duration (four months), which may not be enough to detect changes in weight, the timeline, the low intensity of the intervention, and lack of inclusion of other infant caregivers, such as grandmothers. As mentioned previously, 37% of participants reported returning to work within 3 months, leaving the infant in the care of another person.
In conclusion, the present intervention had no significant effect on improving feeding practices or weight among caregivers of healthy term infants participating in the WIC program in PR and HI. In the future, we plan to improve the outcomes through earlier dissemination of messages (starting at pregnancy), with higher frequency of SMS and higher level of intensity (additional contacts by phone or other means), longer intervention, and inclusion of other caregivers to achieve the desired effects. If future studies show that this type of intervention is successful in preventing obesity, it could be adopted by the WIC program. This is important as WIC visits during the first year occur every 6 months for certification and re-certification, with educational contacts every 3 months. Therefore, SMS could be used to re-enforce messages between visits.
Supplementary Material
Acknowledgments
The authors acknowledge Linda Chock (Branch Chief), Iris Takahashi (Clinic Operations Section Chief), Laura Morihara (Wahiawa WIC Coordinator), Wendy Baker (Wahiawa WIC Office Assistant), Jean Kanda (Leeward WIC Coordinator), Dawn Fujimoto-Redoble (Leeward WIC Nutritionist), and Christina Mariano (Pearl City WIC Coordinator) from the Hawai’i Department of Health WIC Services Branch. They also acknowledge the Puerto Rico WIC Program, including Dana Miró (Executive Director), Blanca Sastre (Interim supervisor of Nutrition and Lactation Division), Alexandra Reyes (Nutrition Education Coordinator), Iris Roldan (Breastfeeding Coordinator), Ivelisse Bruno (Breastfeeding Peer Support Coordinator), Sherley M. Panell (Nutrition Supervisor in Plaza Las Americas WIC Clinic) and her team, and Marta Meaux (Nutrition Supervisor in Trujillo Alto WIC Clinic) and her team. They also thank the WIC participants and undergraduate and graduate research assistants.
Sources of support: This study was supported by the National Institute of Minority Health and Health Disparities (NIMHD), of the National Institutes of Health under award number U54MD008149. Infrastructure support was also provided in part by the National Institute on Minority Health and Health Disparities RCMI Grant: 8G12MD007600. This research was also supported in part by grant U54MD007584 (RMATRIX) from the National Institute on Minority Health and Health Disparities (NIMHD) of the National Institutes of Health (NIH).
Footnotes
Publisher's Disclaimer: Disclaimers: There are no conflicts of interests to disclose.
ClinicalTrials.gov Identifier: NCT02903186
There are no conflicts of interests to disclose.
The authors’ responsibilities were as follows—CP, JB and MC: designed research; CP, JB, CG, and MC: conducted research; JEL: analyzed data; CP, JEL, JB: wrote the paper. CP: had primary responsibility for final content. All authors read and approved the final version of the paper.
References
- 1.Johnson B, thorn B, Mcgill B, Suchman A, Mendelson M, Patlan KL, Freeman B, Gotlieb R, Connor P. WIC Participant and Program Characteristics 2012. Alexandria, VA: U.S. Department of Agriculture, Food and Nutrition Service; 2013. [Google Scholar]
- 2.Snethen JA, Hewitt JB, Goretzke M. Childhood obesity: the infancy connection. J. Obstet. Gynecol. Neonatal Nurs 2007;36(5):501–510. [DOI] [PubMed] [Google Scholar]
- 3.Taveras EM, Gillman MW, Kleinman K, Rich-Edwards JW, Rifas-Shiman SL. Racial/ethnic differences in early-life risk factors for childhood obesity. Pediatrics 2010;125(4):686–695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Adair L Long-term consequences of nutrition and growth in early childhood and possible preventive interventions. Nestle Nutr Inst Work. Ser 2014;78:111–120. [DOI] [PubMed] [Google Scholar]
- 5.Nader PR, O’Brien M, Houts R, Bradley R, Belsky J, Crosnoe R, Friedman S, Mei Z, Susman EJ, Network NI of CH and HDECCR. Identifying risk for obesity in early childhood. Pediatrics 2006;118(3):e594–601. [DOI] [PubMed] [Google Scholar]
- 6.Stettler N, Zemel BS, Kumanyika S, Stallings VA. Infant weight gain and childhood overweight status in a multicenter, cohort study. Pediatrics 2002;109(2):194–199. [DOI] [PubMed] [Google Scholar]
- 7.Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N. Engl. J. Med 1997;337(13):869–873. [DOI] [PubMed] [Google Scholar]
- 8.Young BE, Johnson SL, Krebs NF. Biological determinants linking infant weight gain and child obesity: current knowledge and future directions. Adv. Nutr 2012;3(5):675–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Center for Disease Control and Prevention. Behavioral Risk Factor Surveillance System Survey (BRFSS) data. 2009(April/01). Available at: http://www.cdc.gov/BRFSS/.
- 10.Torres R, Santos E, Orraca L, Elias A, Palacios C. Diet quality, social determinants, and weight status in Puerto Rican children aged 12 years. J. Acad. Nutr. Diet. 2014;114(8):1230–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Soltero SM, Palacios C. Association between dietary patterns and body composition in a group or puerto rican obese adults: A pilot study. P. R. Health Sci. J 2011;30(1):22–27. [PMC free article] [PubMed] [Google Scholar]
- 12.Torres R, Serrano M, Perez CM, Palacios C. Physical environment, diet quality, and body weight in a group of 12-year-old children from four public schools in Puerto Rico. P. R. Health Sci. J 2014;33(1):14–21. [PMC free article] [PubMed] [Google Scholar]
- 13.Lee SK, Novotny R, Daida YG, Vijayadeva V, Gittelsohn J. Dietary patterns of adolescent girls in Hawaii over a 2-year period. J. Am. Diet. Assoc 2007;107(6):956–961. [DOI] [PubMed] [Google Scholar]
- 14.Rios E, Sinigaglia O, Diaz B, Campos M, Palacios C. Development of a Diet Quality Score for Infants and Toddlers and its Association with Weight. J. Nutr. Heal. Food Sci 2016;4(3):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dodgson JE, Codier E, Kaiwi P, Oneha MFM, Pagano I. Breastfeeding patterns in a community of Native Hawaiian mothers participating in WIC. Fam. Community Health 2007;30(2 Suppl):S46–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Anstey EH, Chen J, Elam-Evans LD, Perrine CG. Racial and Geographic Differences in Breastfeeding — United States, 2011–2015. MMWR. Morb. Mortal. Wkly. Rep 2017;66(27):723–727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.DiSantis KI, Hodges EA, Johnson SL, Fisher JO. The role of responsive feeding in overweight during infancy and toddlerhood: a systematic review. Int. J. Obes. (Lond). 2011;35(4):480–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gortmaker SL, Peterson K, Wiecha J, Sobol AM, Dixit S, Fox MK, Laird N. Reducing obesity via a school-based interdisciplinary intervention among youth: Planet Health. Arch. Pediatr. Adolesc. Med 1999;153(4):409–418. [DOI] [PubMed] [Google Scholar]
- 19.Rennie KL, Livingstone MB, Wells JC, McGloin A, Coward WA, Prentice AM, Jebb SA. Association of physical activity with body-composition indexes in children aged 6–8 y at varied risk of obesity. Am. J. Clin. Nutr 2005;82(1):13–20. [DOI] [PubMed] [Google Scholar]
- 20.Yin Z, Hanes J Jr, Moore JB, Humbles P, Barbeau P, Gutin B. An after-school physical activity program for obesity prevention in children: the Medical College of Georgia FitKid Project. Eval. Health Prof 2005;28(1):67–89. [DOI] [PubMed] [Google Scholar]
- 21.Grote V, Theurich M, Koletzko B. Do complementary feeding practices predict the later risk of obesity? Curr. Opin. Clin. Nutr. Metab. Care 2012;15(3):293–297. [DOI] [PubMed] [Google Scholar]
- 22.Mihrshahi S, Battistutta D, Magarey A, Daniels LA. Determinants of rapid weight gain during infancy: baseline results from the NOURISH randomised controlled trial. BMC Pediatr. 2011;11(1):99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wen LM, Baur LA, Simpson JM, Rissel C, Flood VM. Effectiveness of an early intervention on infant feeding practices and “tummy time”: a randomized controlled trial. Arch. Pediatr. Adolesc. Med 2011;165(8):701–707. [DOI] [PubMed] [Google Scholar]
- 24.Campbell KJ, Lioret S, McNaughton SA, Crawford DA, Salmon J, Ball K, McCallum Z, Gerner BE, Spence AC, Cameron AJ, Hnatiuk JA, Ukoumunne OC, Gold L, Abbott G, Hesketh KD. A parent-focused intervention to reduce infant obesity risk behaviors: a randomized trial. Pediatrics 2013;131(4):652–660. [DOI] [PubMed] [Google Scholar]
- 25.Daniels LA, Mallan KM, Battistutta D, Nicholson JM, Perry R, Magarey A. Evaluation of an intervention to promote protective infant feeding practices to prevent childhood obesity: outcomes of the NOURISH RCT at 14 months of age and 6 months post the first of two intervention modules. Int. J. Obes. (Lond). 2012;36(10):1292–1298. [DOI] [PubMed] [Google Scholar]
- 26.Kavanagh KF, Cohen RJ, Heinig MJ, Dewey KG. Educational intervention to modify bottle-feeding behaviors among formula-feeding mothers in the WIC program: impact on infant formula intake and weight gain. J. Nutr. Educ. Behav 2008;40(4):244–50. [DOI] [PubMed] [Google Scholar]
- 27.Taylor RW, Williams SM, Fangupo LJ, Wheeler BJ, Taylor BJ, Daniels L, Fleming EA, McArthur J, Morison B, Erickson LW, Davies RS, Bacchus S, Cameron SL, Heath A- LM. Effect of a Baby-Led Approach to Complementary Feeding on Infant Growth and Overweight. JAMA Pediatr. 2017;171(9):838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Taylor BJ, Gray AR, Galland BC, Heath A- LM, Lawrence J, Sayers RM, Cameron S, Hanna M, Dale K, Coppell KJ, Taylor RW. Targeting Sleep, Food, and Activity in Infants for Obesity Prevention: An RCT. Pediatrics 2017;139(3):e20162037. [DOI] [PubMed] [Google Scholar]
- 29.Hesketh KD, Campbell KJ. Interventions to prevent obesity in 0–5 year olds: an updated systematic review of the literature. Obesity (Silver Spring). 2010;18 Suppl 1:S27–35. [DOI] [PubMed] [Google Scholar]
- 30.Jiang H, Li M, Wen LM, Hu Q, Yang D, He G, Baur LA, Dibley MJ, Qian X. Effect of short message service on infant feeding practice: findings from a community-based study in Shanghai, China. JAMA Pediatr. 2014;168(5):471–478. [DOI] [PubMed] [Google Scholar]
- 31.Gallegos D, Russell-Bennett R, Previte J, Parkinson J. Can a text message a week improve breastfeeding? BMC Pregnancy Childbirth 2014;14(1):372–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Poorman E, Gazmararian J, Parker RM, Yang B, Elon L. Use of Text Messaging for Maternal and Infant Health: A Systematic Review of the Literature. Matern. Child Health J 2014. doi: 10.1007/s10995-014-1595-8 [doi]. [DOI] [PubMed] [Google Scholar]
- 33.Tate EB, Spruijt-Metz D, O’Reilly G, Jordan-Marsh M, Gotsis M, Pentz MA, Dunton GF. mHealth approaches to child obesity prevention: successes, unique challenges, and next directions. Transl. Behav. Med 2013;3(4):406–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Banna J, Campos M, Gibby C, Graulau RE, Meléndez M, Reyes A, Lee JE, Palacios C. Multi-site trial using short mobile messages (SMS) to improve infant weight in low-income minorities: Development, implementation, lessons learned and future applications. Contemp. Clin. Trials 2017;62:56–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am. J. Health Promot 1997;12(1):38–48. [DOI] [PubMed] [Google Scholar]
- 36.Food and Nutrition Service (FNS);, US Department of Agriculture (USDA). Women, Infants, and Children (WIC). 2017. Available at: https://www.fns.usda.gov/wic/women-infants-and-children-wic Accessed February 23, 2017.
- 37.Food and Nutrition Services (FNS); US Department of Agriculture (USDA). Value Enhanced Nutrition Assessment (VENA) -- WIC Nutrition Assessment Policy. WIC Policy Memo #2006-5; 2006. Available at: https://www.fns.usda.gov/value-enhanced-nutrition-assessment-vena-wic-nutrition-assessment-policy Accessed February 23, 2017.
- 38.Food and Nutrition Service U. WIC Regulations-7CFR246.
- 39.World Health Organization (WHO). WHO AnthroPlus software. WHO; 2013. Available at: http://www.who.int/growthref/tools/en/ Accessed February 18, 2017. [Google Scholar]
- 40.World Health Organization (WHO). WHO Global Database on Child Growth and Malnutrition. WHO Libr; 2015. Available at: http://www.who.int/nutgrowthdb/en/ Accessed February 18, 2017. [Google Scholar]
- 41.Dattilo AM, Birch L, Krebs NF, Lake A, Taveras EM, Saavedra JM. Need for Early Interventions in the Prevention of Pediatric Overweight : A Review and Upcoming Directions. J. Obes 2012;2012:1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ciampa PJ, Kumar D, Barkin SL, Sanders LM, Yin HS, Perrin EM, Rothman RL. Interventions aimed at decreasing obesity in children younger than 2 years: a systematic review. Arch. Pediatr. Adolesc. Med 2010;164(12):1098–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Blake-Lamb TL, Locks LM, Perkins ME, Woo Baidal JA, Cheng ER, Taveras EM. Interventions for Childhood Obesity in the First 1,000 Days A Systematic Review. Am. J. Prev. Med 2016;50(6):780–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ong KK, Loos RJF. Rapid infancy weight gain and subsequent obesity: systematic reviews and hopeful suggestions. Acta Paediatr. 2006;95(8):904–8. [DOI] [PubMed] [Google Scholar]
- 45.Baird J, Fisher D, Lucas P, Kleijnen J, Roberts H, Law C. Being big or growing fast: systematic review of size and growth in infancy and later obesity. BMJ 2005;331(7522):929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Druet C, Stettler N, Sharp S, Simmons RK, Cooper C, Smith GD, Ekelund U, Lévy-Marchal C, Jarvelin M- R, Kuh D, Ong KK. Prediction of childhood obesity by infancy weight gain: an individual-level meta-analysis. Paediatr. Perinat. Epidemiol 2012;26(1):19–26. [DOI] [PubMed] [Google Scholar]
- 47.Monteiro POA, Victora CG. Rapid growth in infancy and childhood and obesity in later life - a systematic review. Obes. Rev 2005;6(2):143–154. [DOI] [PubMed] [Google Scholar]
- 48.Weinberger M, Oddone EZ, Henderson WG, Smith DM, Huey J, Giobbie-Hurder A, Feussner JR. Multisite randomized controlled trials in health services research: scientific challenges and operational issues. Med. Care 2001;39(6):627–34. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


