Abstract
Background
The role of electronic cigarettes (e-cigarettes) in product transitions has been debated.
Methods
We used nationally representative data from the Population Assessment of Tobacco and Health Study waves 1 (2013–2014) and 2 (2014–2015) to investigate the associations between e-cigarette initiation and cigarette cessation/reduction in the USA. We limited the sample to current cigarette smokers aged 25+ years who were not current e-cigarette users at wave 1. We modelled 30-day cigarette cessation and substantial reduction in cigarette consumption as a function of e-cigarette initiation between surveys using multivariable logistic regression.
Results
Between waves 1 and 2, 6.9% of cigarette smokers who were not current e-cigarette users transitioned to former smokers. After adjusting for covariates, cigarette smokers who initiated e-cigarette use between waves and reported they used e-cigarettes daily at wave 2 had 7.88 (95% CI 4.45 to 13.95) times the odds of 30-day cigarette cessation compared with non-users of e-cigarettes at wave 2. Cigarette smokers who began using e-cigarettes every day and did not achieve cessation had 5.70 (95% CI 3.47 to 9.35) times the odds of reducing their average daily cigarette use by at least 50% between waves 1 and 2 compared with e-cigarette non-users.
Conclusions
Daily e-cigarette initiators were more likely to have quit smoking cigarettes or reduced use compared with non-users. However, less frequent e-cigarette use was not associated with cigarette cessation/reduction. These results suggest incorporating frequency of e-cigarette use is important for developing a more thorough understanding of the association between e-cigarette use and cigarette cessation.
Keywords: electronic cigarette, e-cigarette, vaping, vape, ENDS, smoking cessation, e-cigarette initiation, cigarette reduction, product transitions, population assessment of tobacco and health, PATH
Introduction
Tobacco use is the leading preventable cause of death in the USA.1 The prevalence of cigarette smoking in the USA has declined considerably since the first Surgeon General’s report (from 42.4% in 1964 to 15.1% in 2015),1 2 but smoking remains responsible for more than 400 000 deaths each year.1
A large body of evidence demonstrates the benefits of cigarette smoking cessation.1 3 Adults who quit smoking gain 6–10 years of life compared with those who continue to smoke, and quitting before the age of 40 years decreases mortality risk by approximately 90%.4 In 2015, 57.2% of adult smokers in the USA were advised to quit smoking by a doctor or health professional.5 Although the majority of smokers appear to be aware of the health benefits associated with smoking cessation, fewer than one in ten smokers successfully quit over the prior year.5
The prevalence of electronic cigarette (e-cigarette) use has risen in recent years since e-cigarettes entered the market in 2007.6–8 Evidence on the efficacy of e-cigarettes as smoking cessation aids remains limited and inconclusive.9 10 Pooled analysis of two randomised controlled trials indicated that participants assigned to nicotine-containing e-cigarettes had 2.29 times the odds of 6-month cigarette cessation compared with the placebo group.11 Several cross-sectional studies,12–16 longitudinal analyses17 18 and meta-analyses19–21 have also shown an association between e-cigarette use and increased quit attempts and successes. However, other studies, including a systematic review and meta-analysis, have raised doubts about the efficacy of e-cigarettes as cessation/reduction aids for smokers22–24 and highlighted that e-cigarettes may not be a satisfying alternative to regular cigarettes.25 Furthermore, prior studies have shown dual product use is common, indicating e-cigarettes may be used as a complement rather than substitute to cigarette smoking.26
Prior studies investigating the role of e-cigarette use in cigarette cessation/reduction have largely relied on the analysis of non-representative samples, limiting the ability to generalise results to the population at large. Our study aims to estimate how the uptake of e-cigarettes is associated with cigarette cessation and changes in cigarette smoking intensity in adults in the USA.
Methods
Design
We used data from waves 1 and 2 of the Population Assessment of Tobacco and Health (PATH) Study to investigate the associations between e-cigarette initiation and cigarette cessation/reduction. The PATH Study is a large, nationally representative, cohort study designed to collect data on use patterns, risk perceptions, attitudes and health outcomes associated with tobacco products.27 28 Wave 1 data collection was carried out between September 2013 and December 2014 and included 32 320 adults aged ≥18. Data for wave 2 were collected approximately 1 year later, from October 2014 to October 2015. The weighted retention rate between waves was approximately 83%.27
Sample
The current analysis was restricted to adults 25 years and older who were current established tobacco cigarette smokers but not current e-cigarette users at wave 1. From a total sample of 5832 current smokers aged ≥25 years at wave 1 who were not current e-cigarette users, we excluded individuals with missing observations for poverty level (n=452), education (n=8), growing up in a house where someone smoked indoors (n=10), currently living with a cigarette smoker (n=13), average cigarette packs per day (n=181) and making a quit attempt in the year prior to wave 1 (n=11). Additionally, we excluded individuals if they were missing observations for cigarette smoking status (n=1) or e-cigarette use (n=32) at wave 2, leaving a final analytical sample of 5124.
Measures
Data on age, sex, race/ethnicity, household income, education and region were collected during the wave 1 interview. In the public access PATH data, age was grouped using 10-year categories from 25 to 74 years and an open-ended category for ≥75 years. Race/ethnicity was classified as non-Hispanic white, non-Hispanic black, Hispanic and other. Region was classified as living in the Northeast, Midwest, South or West. Income level was assessed based on reported annual household income and Health and Human Services guidelines for that year,29 30 resulting in the following categories: below poverty level, at or near poverty level and ≥twice poverty level.27 Education level was categorised as less than high school, high school or equivalent, some college, and bachelor’s/advanced degree. Data on living in a smoking household as a child, currently living with a cigarette smoker, frequency (some-day smoker, everyday smoker) and intensity (<1 pack per day, 1–2 packs per day, ≥2 packs per day) of cigarette use, time to first cigarette in the morning (≤5 min, 6–29 min, 30–59 min, ≥60 min), and prior quit attempt (within prior year) were assessed at wave 1.
Outcome measures
Current smokers were defined as respondents who reported smoking more than 100 cigarettes in their lifetime and currently smoked every day or on some days.27 Former smokers at wave 2 were defined as individuals who were current smokers at wave 1, reported they did not smoke every day or some days at wave 2, and had not smoked any cigarettes in the 30 days prior to wave 2. Smokers who did not smoke every day or some days but smoked ≥1 cigarettes over the past 30 days (n=133) were reclassified as current smokers at wave 2 and were not considered to have quit smoking cigarettes. Consistent with prior analyses,18 31 substantial reduction in cigarette consumption was defined as a reduction in average cigarettes smoked per day of at least 50% between wave 1 and wave 2.
E-cigarette use was assessed at wave 1 and wave 2. Respondents were considered current e-cigarette users if they reported currently using e-cigarettes experimentally (no ‘regular’ e-cigarette use), on some days or every day.27 E-cigarette users were also asked to report if their e-cigarette used cartridges, was refillable and used a tank system.
Analysis
For all multivariable models, we adjusted for sex, age, race/ethnicity, region, household income, education, living in a smoking household as a child, currently living with a cigarette smoker, frequency and intensity of cigarette use, time to first cigarette in the morning, and prior quit attempt. We used multivariable logistic regression to model 30-day cigarette cessation and substantial reduction in cigarette consumption as a function of e-cigarette initiation between waves 1 and 2. Individuals who had quit smoking cigarettes for at least 30 days were not included in the analysis of reduction in cigarette use.
We conducted several sensitivity analyses to test the robustness of our findings. First, we investigated the association between e-cigarette use and cessation after collapsing use into a single category regardless of frequency. Second, to assess the durability of cessation among e-cigarette users and non-users, we repeated our logistic regression modelling cigarette cessation using 90-day cigarette cessation (instead of 30-day cessation) as the outcome variable. Third, we explored the possibility that e-cigarette initiation is a proxy for attempting to quit by limiting the primary 30-day cessation analysis to cigarette smokers who reported a quit attempt within the year prior to wave 1. Fourth, we investigated the effect of reclassifying smokers who started and stopped using e-cigarettes between wave 1 and wave 2 on the association between e-cigarette use and cigarette cessation. Fifth, we performed a series of sensitivity analyses to model cigarette cessation as a function of combined frequency of e-cigarette use and various product characteristics, including use of cartridges, refillable e-cigarettes and e-cigarettes with tank systems. Finally, we conducted a sensitivity analysis for cigarette reduction, using multivariable linear regression to model changes in cigarette smoking intensity as defined by the average number of cigarettes smoked daily at each wave.
Analyses were performed using STATA V.15. The wave 2 sample weights were incorporated to adjust for unequal probabilities of selection and non-response, and variances were estimated using Taylor series linearisation with the SVY routine.27 We considered a two-sided P value <0.05 statistically significant.
Results
Table 1 presents the descriptive statistics for the study sample. Participants were 55% male and predominantly (69.8%) non-Hispanic white. Approximately 75% of the sample was younger than 55 years, and a majority of respondents were either high school graduates (39.7%) or had completed some college (32.3%). Most cigarette smokers in our sample were everyday smokers (82.4%) but consumed less than one pack per day (63.7%). Almost half (45.0%) reported attempting to quit smoking in the year prior to wave 1.
Table 1.
Characteristics of current smokers who did not use e-cigarettes at wave 1, PATH (2013–2015) (n=5124)
| n | % | |
| Sex | ||
| Male | 2580 | 55.0 |
| Female | 2544 | 45.0 |
| Age | ||
| 25–34 years | 1454 | 28.1 |
| 35–44 years | 1186 | 22.7 |
| 45–54 years | 1195 | 23.2 |
| 55–64 years | 906 | 18.1 |
| 65–74 years | 314 | 6.5 |
| ≥75 years | 69 | 1.5 |
| Race/ethnicity | ||
| Non-Hispanic white | 3399 | 69.8 |
| Non-Hispanic black | 811 | 14.8 |
| Hispanic | 583 | 10.1 |
| Non-Hispanic other | 331 | 5.4 |
| Region | ||
| Northeast | 770 | 17.8 |
| Midwest | 1479 | 25.5 |
| South | 1987 | 39.4 |
| West | 888 | 17.3 |
| Household income | ||
| Below poverty level | 1945 | 35.6 |
| At or near poverty level | 1450 | 27.9 |
| ≥Twice poverty level | 1729 | 36.6 |
| Education | ||
| Less than high school | 889 | 16.3 |
| High school/GED | 1829 | 39.7 |
| Some college | 1796 | 32.3 |
| Bachelor’s/advanced degree | 610 | 11.7 |
| Lived in a smoking household as a child | ||
| No | 1438 | 27.8 |
| Yes | 3686 | 72.3 |
| Currently lives with a cigarette smoker | ||
| No | 2579 | 51.8 |
| Yes | 2545 | 48.2 |
| Frequency of cigarette use at wave 1 | ||
| Some-day cigarette smoker | 878 | 17.6 |
| Everyday cigarette smoker | 4246 | 82.4 |
| Intensity of cigarette smoking at wave 1 | ||
| <1 pack per day | 3303 | 63.7 |
| 1–2 packs per day | 1602 | 31.9 |
| ≥2 packs per day | 219 | 4.4 |
| Time to first cigarette in morning | ||
| ≤5 min | 1204 | 23.2 |
| 6–29 min | 2037 | 39.6 |
| 30–59 min | 98 | 2.0 |
| ≥60 min | 1785 | 35.2 |
| Tried to quit smoking cigarettes in year prior to wave 1 | ||
| No | 2787 | 55.1 |
| Yes | 2337 | 45.0 |
| New e-cigarette use at wave 2 | ||
| Non-user | 4461 | 87.0 |
| Experimental e-cigarette user | 358 | 6.9 |
| Some-day e-cigarette user | 178 | 3.5 |
| Everyday e-cigarette user | 127 | 2.6 |
Restricted to adults aged 25+ who were current cigarette smokers at wave 1 but not current e-cigarette users. Sample weights were incorporated to adjust the percentage estimates in the PATH sample for unequal probabilities of selection and non-response.
e-cigarettes, electronic cigarettes; GED, General Equivalency Development test; PATH, Population Assessment of Tobacco and Health.
Among cigarette smokers who were not current e-cigarette users at wave 1, 337 (6.90%) individuals quit smoking cigarettes for at least 30 days (6.16% quit for at least 90 days). An additional 776 individuals (16.69%) achieved a substantial reduction (≥50%) in their average daily cigarette intake. The total number of new e-cigarette initiators at wave 2 was 663 (13.03%), with 127 (2.58% of the total sample) beginning to use e-cigarettes every day, 178 (3.51%) starting to use e-cigarettes some days and 358 (6.94%) initiating experimental use. At wave 2, 14.44% of those who quit cigarettes and 15.39% of those who reduced their cigarette consumption reported current e-cigarette use, with the remaining respondents reporting no current use of either product.
In the logistic regression of 30-day cigarette cessation, cigarette smokers who initiated daily e-cigarette use had 7.88 (95% CI 4.45 to 13.95) times the odds of quitting cigarette smoking compared with e-cigarette non-users (table 2). In contrast, e-cigarette experimenters showed reduced odds of quitting cigarette smoking (OR: 0.51; 95% CI 0.26 to 1.00). Additionally, individuals who were everyday smokers had decreased odds of achieving 30-day cigarette cessation compared with some-day smokers, while those who waited at least 60 min to smoke in the mornings had increased odds of quitting compared with those who reported smoking their first cigarette within 5 min of waking.
Table 2.
Logistic regression: 30-day cigarette cessation at wave 2, PATH (2013–2015) (n=5124)
| 30-Day cigarette cessation at wave 2 | |||
| Adjusted OR | (95% CI) | P value | |
| Sex | |||
| Male | Ref | – | – |
| Female | 1.14 | (0.91 to 1.41) | 0.250 |
| Age | |||
| 25–34 years | Ref | – | – |
| 35–44 years | 0.93 | (0.65 to 1.32) | 0.670 |
| 45–54 years | 0.95 | (0.63 to 1.44) | 0.803 |
| 55–64 years | 1.09 | (0.71 to 1.68) | 0.681 |
| 65–74 years | 1.32 | (0.73 to 2.38) | 0.354 |
| ≥75 years | 1.68 | (0.63 to 4.47) | 0.294 |
| Race/ethnicity | |||
| Non-Hispanic white | Ref | – | – |
| Non-Hispanic black | 0.61 | (0.40 to 0.92) | 0.018 |
| Hispanic | 0.83 | (0.57 to 1.21) | 0.323 |
| Non-Hispanic other | 1.07 | (0.60 to 1.92) | 0.810 |
| Region | |||
| Northeast | Ref | – | – |
| Midwest | 1.04 | (0.68 to 1.59) | 0.865 |
| South | 1.36 | (0.94 to 1.95) | 0.099 |
| West | 1.05 | (0.70 to 1.58) | 0.797 |
| Household income | |||
| Below poverty level | Ref | – | – |
| At or near poverty level | 1.12 | (0.79 to 1.59) | 0.514 |
| ≥Twice poverty level | 1.31 | (0.92 to 1.86) | 0.131 |
| Education | |||
| Less than high school | Ref | – | – |
| High school or equivalent | 0.90 | (0.59 to 1.39) | 0.638 |
| Some college | 0.99 | (0.66 to 1.49) | 0.975 |
| Bachelor’s/advanced degree | 0.91 | (0.53 to 1.57) | 0.732 |
| Lived in a smoking household as a child | |||
| No | Ref | – | – |
| Yes | 0.81 | (0.57 to 1.14) | 0.225 |
| Currently lives with a cigarette smoker | |||
| No | Ref | – | – |
| Yes | 0.98 | (0.73 to 1.32) | 0.886 |
| Frequency of cigarette use at wave 1 | |||
| Some-day cigarette smoker | Ref | – | – |
| Everyday cigarette smoker | 0.27 | (0.19 to 0.38) | <0.001 |
| Intensity of cigarette smoking at wave 1 | |||
| <1 pack per day | Ref | – | – |
| 1–2 packs per day | 0.88 | (0.61 to 1.26) | 0.480 |
| ≥2 packs per day | 0.85 | (0.30 to 2.36) | 0.748 |
| Time to first cigarette in morning | |||
| ≤5 min | Ref | – | – |
| 6–29 min | 1.28 | (0.86 to 1.91) | 0.221 |
| 30–59 min | 1.88 | (0.69 to 5.12) | 0.212 |
| ≥60 min | 1.88 | (1.21 to 2.93) | 0.005 |
| Tried to quit smoking cigarettes in year prior to wave 1 | |||
| No | Ref | – | – |
| Yes | 1.25 | (1.00 to 1.57) | 0.049 |
| New e-cigarette use at wave 2 | |||
| Non-user | Ref | – | – |
| Experimental e-cigarette user | 0.51 | (0.26 to 1.00) | 0.050 |
| Some-day e-cigarette user | 0.51 | (0.17 to 1.47) | 0.207 |
| Everyday e-cigarette user | 7.88 | (4.45 to 13.95) | <0.001 |
e-cigarette, electronic cigarette; PATH, Population Assessment of Tobacco and Health; Ref, reference.
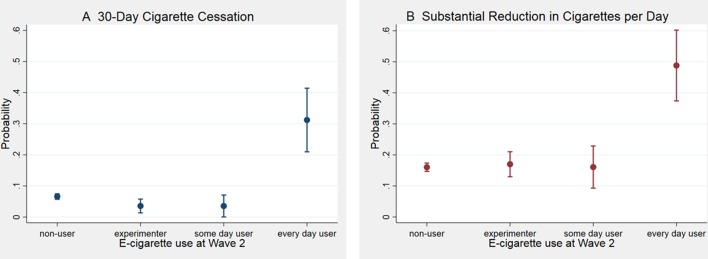
New e-cigarette initiators who reported everyday use at wave 2 had the highest predicted probability of achieving 30-day cigarette cessation between wave 1 and wave 2 (31.20%; 95% CI 20.97% to 41.42%). The probability of transitioning to former cigarette smoker was lower for non-users of e-cigarettes (6.60%; 95% CI 5.70% to 7.49%), new e-cigarette experimenters (3.56%; 95% CI 1.34% to 5.78%) and new some-day e-cigarette users (3.55%; 95% CI 0.03% to 7.07%) (figure 1A).
Figure 1.
Predicted probabilities of (A) cigarette cessation and (B) reduction at wave 2 by electronic cigarette (e-cigarette) initiation, Population Assessment of Tobacco and Health (2013–2015). Predicted probabilities of achieving 30-day cigarette cessation and reduction as a function of e-cigarette initiation between waves were calculated using coefficients estimated from the models shown in tables 2 and 3.
At wave 1, the mean reported average daily cigarette use was 13.97 cigarettes. Cigarette smokers who began using e-cigarettes every day and did not quit smoking cigarettes had 5.70 times the odds of reducing their daily cigarette use by at least 50% compared with e-cigarette non-users (95% CI 3.47 to 9.35) (table 3). Some-day e-cigarette users and e-cigarette experimenters did not significantly change their cigarette consumption compared with non-users. Cigarette smokers who smoked every day or grew up in a household with indoor smoking were less likely to reduce their cigarette use between waves. However, smokers who smoked at least one pack per day, waited at least 60 min for their first cigarette on waking or reported a recent quit attempt were more likely to reduce their cigarette use.
Table 3.
Logistic regression: at least 50% reduction in average cigarette consumption between wave 1 and wave 2, PATH (2013–2015) (n=4672)
| Substantial reduction at wave 2 | |||
| Adjusted OR | (95% CI) | P value | |
| Sex | |||
| Male | Ref | – | – |
| Female | 0.80 | (0.68 to 0.95) | 0.011 |
| Age | |||
| 25–34 years | Ref | – | – |
| 35–44 years | 0.80 | (0.62 to 1.03) | 0.089 |
| 45–54 years | 0.77 | (0.58 to 1.01) | 0.057 |
| 55–64 years | 1.13 | (0.85 to 1.50) | 0.414 |
| 65–74 years | 0.69 | (0.43 to 1.11) | 0.129 |
| ≥75 years | 0.72 | (0.27 to 1.89) | 0.503 |
| Race/ethnicity | |||
| Non-Hispanic white | Ref | – | – |
| Non-Hispanic black | 1.68 | (1.31 to 2.17) | <0.001 |
| Hispanic | 1.43 | (1.08 to 1.88) | 0.012 |
| Non-Hispanic other | 1.29 | (0.80 to 2.08) | 0.297 |
| Region | |||
| Northeast | Ref | – | – |
| Midwest | 1.16 | (0.80 to 1.70) | 0.424 |
| South | 1.29 | (0.89 to 1.87) | 0.175 |
| West | 1.42 | (0.96 to 2.10) | 0.081 |
| Household Income | |||
| Below poverty level | Ref | – | – |
| At or near poverty level | 0.91 | (0.72 to 1.15) | 0.430 |
| ≥Twice poverty level | 0.78 | (0.62 to 0.98) | 0.037 |
| Education | |||
| Less than high school | Ref | – | – |
| High school or equivalent | 0.94 | (0.75 to 1.18) | 0.591 |
| Some college | 0.99 | (0.76 to 1.30) | 0.957 |
| Bachelor’s/advanced degree | 1.01 | (0.70 to 1.47) | 0.952 |
| Lived in a smoking household as a child | |||
| No | Ref | – | – |
| Yes | 0.79 | (0.65 to 0.96) | 0.017 |
| Currently lives with a cigarette smoker | |||
| No | Ref | – | – |
| Yes | 1.11 | (0.92 to 1.34) | 0.275 |
| Frequency of cigarette use at wave 1 | |||
| Some-day cigarette smoker | Ref | – | – |
| Everyday cigarette smoker | 0.44 | (0.34 to 0.57) | <0.001 |
| Intensity of cigarette smoking at wave 1 | |||
| <1 pack per day | Ref | – | – |
| 1–2 packs per day | 1.76 | (1.35 to 2.31) | <0.001 |
| ≥2 packs per day | 5.33 | (3.68 to 7.71) | <0.001 |
| Time to first cigarette in the morning | |||
| ≤5 min | Ref | – | – |
| 6–29 min | 1.20 | (0.95 to 1.52) | 0.123 |
| 30–59 min | 0.83 | (0.37 to 1.84) | 0.640 |
| ≥60 min | 1.67 | (1.27 to 2.20) | <0.001 |
| Tried to quit smoking cigarettes in year prior to wave 1 | |||
| No | Ref | – | – |
| Yes | 1.41 | (1.18 to 1.68) | <0.001 |
| New e-cigarette use at wave 2 | |||
| Non-user | Ref | – | – |
| Experimental e-cigarette user | 1.08 | (0.78 to 1.48) | 0.641 |
| Some-day e-cigarette user | 1.00 | (0.58 to 1.74) | 0.988 |
| Everyday e-cigarette user | 5.70 | (3.47 to 9.35) | <0.001 |
e-cigarette, electronic cigarette; PATH, Population Assessment of Tobacco and Health; Ref, reference.
New e-cigarette initiators who reported everyday use at wave 2 had the highest predicted probability of reducing their average daily cigarette use by at least 50% (48.80%; 95% CI 37.39% to 60.21%). The probability of substantial reduction was lower for non-users of e-cigarettes (16.03%; 95% CI 14.69% to 17.37%), new e-cigarette experimenters (17.00%; 95% CI 12.97% to 21.03%) and new some-day e-cigarette users (16.08%; 95% CI 9.29% to 22.88%) (figure 1B).
The results of our sensitivity analyses can be found in online supplementary tables S1–S8. We found that collapsing all e-cigarette use into a single category substantially attenuated the association between e-cigarette use and 30-day cigarette cessation (online supplementary table S1). Similar results to the primary 30-day cessation model were produced in the model of 90-day cigarette cessation (online supplementary table S2) and the analysis restricted to individuals who reported a quit attempt in the last 12 months (online supplementary table S3). Additionally, reclassifying respondents who started and stopped using e-cigarettes between waves as a new level of e-cigarette use did not affect our results (online supplementary table S4).
tobaccocontrol-2017-054108supp001.pdf (369.6KB, pdf)
We found e-cigarette initiators who used non-cartridge-based e-cigarettes daily were significantly more likely to report 30-day cigarette cessation compared with e-cigarette non-users, while cartridge-based daily e-cigarette users showed no significant difference compared with non-users (online supplementary table S5). Similarly, e-cigarette initiators who primarily used refillable e-cigarettes daily were significantly more likely to quit compared with e-cigarette non-users, while non-refillable daily e-cigarette users showed no significant difference (online supplementary table S6). Similar results were seen among new daily tank-based e-cigarette users who were significantly more likely to quit compared with e-cigarette non-users (online supplementary table S7).
Finally, the linear regression investigating the association of e-cigarette uptake and cigarette smoking intensity showed cigarette smokers who began using e-cigarettes every day and did not quit smoking cigarettes reduced their average daily cigarette use by 5.60 (95% CI 3.52 to 7.68) more cigarettes than the reference group of e-cigarette non-users (online supplementary table S8).
Discussion
The current study investigated the association of e-cigarette initiation and cigarette smoking cessation among adults in a nationally representative cohort. Among cigarette smokers, those who began using e-cigarettes every day had 5.7 times the odds of reducing their average daily cigarette use by at least 50% compared with e-cigarette non-users. We also observed cigarette smokers who initiated daily e-cigarette use had 7.9-fold higher odds of having quit smoking cigarettes for at least 30 days than e-cigarette non-users.
Prior analysis of PATH data from wave 1 found daily use of e-cigarettes was associated with being a former smoker.32 Similarly, recent data from the 2014 National Health Inteview Survey (NHIS) indicate recently quit smokers were more than four times as likely to be daily users of e-cigarettes compared with daily cigarette smokers.33 Our results agree with data from the Current Population Survey-Tobacco Use Supplement (2014–2015) suggesting that compared with non-users, e-cigarette users were more likely to attempt to quit smoking cigarettes and to succeed in quitting.13 Furthermore, population-level trends show a significant increase in the overall rate of cigarette smoking cessation in the USA from 2010–2011 to 2014–2015 alongside a similar rise in e-cigarette use, suggesting e-cigarettes may contribute to the increase in population tobacco cessation rates.13
Consistent with our analysis, prior studies have shown frequent e-cigarette use is associated with higher likelihood of reducing the quantity of cigarettes smoked.18 34 Some smokers may be using e-cigarettes to reduce their cigarette consumption as a stepping stone to cessation; evidence suggests smokers who reduce the number of daily cigarettes smoked are more likely to attempt to quit and successfully quit.35
In contrast to our findings, a recent meta-analysis of e-cigarettes and cigarette smoking cessation, which included four longitudinal studies, showed the odds of quitting cigarettes were 28% lower in those who used e-cigarettes compared with those who did not use e-cigarettes.23 However, few studies included in the meta-analysis reported on the intensity of e-cigarette use. Similarly, a study using the 2010 Tobacco Use Supplement of the Current Population Survey found ever-use of e-cigarettes was not significantly associated with change in cigarettes smoked per day36 but did not report intensity of e-cigarette use.
Our analysis demonstrates the frequency of e-cigarette use makes a difference in the odds of cigarette cessation/reduction. These results are consistent with existing findings that daily e-cigarette users are more likely to attempt to quit smoking18 37 and achieve cigarette cessation compared with non-users.37–39 Recent evidence shows more than 70% of recent quitters who used e-cigarettes were still using e-cigarettes daily, suggesting frequent use may be critical to preventing relapse.13 Prior evidence has also shown daily e-cigarette use is associated with higher likelihood of reducing the quantity of cigarettes smoked.18
Although daily e-cigarette users seem to gain the most benefits in terms of increased likelihood of cigarette cessation/reduction, they represent a small proportion of e-cigarette users among smokers. In our sample, only 19.82% of smokers who initiated e-cigarette use between waves reported daily e-cigarette use compared with 26.93% who reported some-day use and 53.25% who reported experimental use. The e-cigarette experimenters and some-day users, who comprise a greater proportion of users, may represent dual product users who are using e-cigarettes in conjunction with tobacco cigarettes instead of as a substitute, raising doubts about the net benefits of e-cigarette use to adult smokers. Additional research is needed to understand the impact of dual product use on trends in cigarette use.
In addition to frequency of use, our supplementary analyses suggest e-cigarette product characteristics play a role in cigarette cessation. We found new daily e-cigarette users who used e-cigarettes without cartridges, refillable e-cigarettes and tank-based e-cigarettes increased their likelihood of 30-day cigarette cessation compared with non-users. E-cigarettes that use cartridges are typically first-generation e-cigarette products sometimes referred to as ‘cigalikes’ due to their similar appearance to traditional cigarettes.40 Refillable and tank-based e-cigarettes, on the other hand, represent second-generation and third-generation products.41 Our findings suggest users of second-generation and third-generation e-cigarettes are more likely to quit smoking cigarettes, possibly because later generation models have been shown to be more effective at delivering nicotine.41 42 These findings are consistent with prior evidence showing tank users were more likely and cigalike users were less likely to have quit compared with e-cigarette non-users.39
The potential benefits of e-cigarettes as cigarette smoking cessation/reduction aids must be carefully weighed against the potential harms. Many researchers and public health experts believe using e-cigarettes carries less health risks than smoking cigarettes.43 44 Small, short-term studies of e-cigarette use suggest e-cigarettes have a smaller impact on cardiovascular health45 46 and expose users to substantially fewer carcinogens compared with cigarettes.47 However, other studies indicate e-cigarette use may have detrimental short-term health effects.48–50 Lack of evidence on the long-term impact of e-cigarette use means the true public health impact is not yet known.
Furthermore, many public health experts worry e-cigarettes renormalise cigarettes, the use of which has become stigmatised in recent decades, and serve as a precursor to smoking cigarettes.44 A growing body of evidence, including a systematic review and meta-analysis,51 has demonstrated e-cigarette use may be associated with the uptake of cigarettes among youth and young adults in the USA,52–54 the UK55 and Mexico.56 However, some research has disputed this claim.57 58 Future research should continue to investigate the association of e-cigarette initiation and tobacco cigarette use using longitudinal data and begin assessing the long-term health consequences of e-cigarette and dual product use.
The primary strength of our analysis is we provide evidence on the association between e-cigarette initiation specifically and cigarette smoking cessation/reduction. The temporal element provided using PATH cohort data provides a vital aspect missing from many prior studies. Additionally, the data used in this analysis come from a large, nationally representative survey of the US adult population. Furthermore, our analysis examines outcomes of interest, assesses e-cigarette use for cessation/reduction as the exposure of interest, includes appropriate comparison groups, measures dose of e-cigarette use and assesses e-cigarette product type, as proposed by Villanti et al 59, to determine if a study provides sufficient information to answer whether e-cigarettes can facilitate smoking cessation and/or reduction. Finally, the results of our analysis were robust to all sensitivity checks conducted, including varying the definition of former smoker to 90-day cessation and limiting the analysis to smokers with prior quit attempts.
Our study is subject to several limitations. One potential limitation is we did not use clinical measures to confirm smoking status; the present analysis relies exclusively on self-reported data. However, prior validation studies have shown self-reported cigarette smoking behaviours among adults are consistent and reliable.60 Although we used two waves of data, we cannot establish how recently behaviours changed between waves, nor can we establish the order of those changes; therefore, we cannot conclude e-cigarette initiation preceded cigarette cessation or reduction. However, it is not required that e-cigarette use precede a quit attempt in order to impact cessation as preventing relapse is a key component of durable cessation. Our conclusions are also limited by the relatively short follow-up time between wave 1 (2013–2014) and wave 2 (2014–2015) of the survey. Whereas more than half of adult smokers report past-year quit attempts, less than 10% stopped smoking cigarettes for at least 1 year.61 Further estimates suggest only 3%–5% of quitters who attempt to quit without treatment successfully abstain from smoking cigarettes for 6–12 months.62 Due to the short follow-up time between waves, our analysis cannot establish the sustainability of cigarette cessation among individuals who transitioned from current smokers at wave 1 to former smokers at wave 2.
Conclusion
We found daily e-cigarette initiators were more likely to have quit smoking cigarettes or reduced use compared with non-users. However, less frequent e-cigarette use was not associated with cigarette cessation/reduction. Our findings add to the growing evidence suggesting adult smokers in the USA are using e-cigarettes to help themselves quit smoking cigarettes or reduce their cigarette use. Understanding the implications of e-cigarette use for product transitions away from tobacco use may help inform the Federal Drug Administration Center for Tobacco Products on the expected contribution of e-cigarettes to future trends in tobacco cigarette use and the burden of tobacco-related disease. Additionally, findings from this study can inform future health education and communication efforts around cigarette smoking cessation and harm reduction strategies.
What this paper adds.
Prior literature suggests the possible effectiveness of electronic cigarettes (e-cigarettes) for cigarette smoking cessation, but most existing evidence relied on non-representative samples, limiting the ability to draw generalisable conclusions.
Using data from wave 1 and wave 2 of the Population Assessment of Tobacco and Health Study, we show daily e-cigarette initiators were more likely to have reduced their cigarette use and quit smoking cigarettes compared with non-users.
The same trends were not observed with e-cigarette initiators reporting experimental or some-day use, suggesting the frequency of e-cigarette use may play an important role in cigarette smoking cessation/reduction.
Acknowledgments
The authors would like to thank Rose Marie Robertson and Glenn Hirsch for helpful comments and suggestions on an earlier version of the manuscript.
Footnotes
Contributors: AS designed the study. KMB analysed the data and wrote the first draft of the manuscript. All authors contributed to interpreting the findings and revising the manuscript.
Funding: Research reported in this publication was supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health and the Center for Tobacco Products under Award Number P50HL120163. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Food and Drug Administration.
Competing interests: None declared.
Patient consent: Detail has been removed from this case description/these case descriptions to ensure anonymity. The editors and reviewers have seen the detailed information available and are satisfied that the information backs up the case the authors are making.
Ethics approval: Institutional review board approval was not required as we based the study on secondary analyses of publicly available, de-identified data.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Public-use data files for the Population Assessment of Tobacco and Health (PATH) study can be accessed from the National Addiction & HIV Data Archive Program.
Correction notice: This article has been corrected since it was published Online First. The supplementary file had minor errors within it and has now been replaced with a corrected file.
References
- 1. United States Department of Health and Human Services. The health consequences of smoking—50 years of progress: a report of the surgeon general, 2014. [Google Scholar]
- 2. Jamal A, King BA, Neff LJ, et al. Current cigarette smoking among adults - United States, 2005-2015. MMWR Morb Mortal Wkly Rep 2016;65:1205–11. 10.15585/mmwr.mm6544a2 [DOI] [PubMed] [Google Scholar]
- 3. White WB. Smoking-related morbidity and mortality in the cardiovascular setting. Prev Cardiol 2007;10:1–4. 10.1111/j.1520-037X.2007.06050.x [DOI] [PubMed] [Google Scholar]
- 4. Jha P, Ramasundarahettige C, Landsman V, et al. 21st-century hazards of smoking and benefits of cessation in the United States. N Engl J Med 2013;368:341–50. 10.1056/NEJMsa1211128 [DOI] [PubMed] [Google Scholar]
- 5. Babb S, Malarcher A, Schauer G, et al. Quitting smoking among adults- United States, 2000-2015. MMWR Morb Mortal Wkly Rep 2017;65:1457–64. 10.15585/mmwr.mm6552a1 [DOI] [PubMed] [Google Scholar]
- 6. Glasser AM, Collins L, Pearson JL, et al. Overview of electronic nicotine delivery systems: a systematic review. Am J Prev Med 2017;52:e33–e66. 10.1016/j.amepre.2016.10.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Regan AK, Promoff G, Dube SR, et al. Electronic nicotine delivery systems: adult use and awareness of the ’e-cigarette' in the USA. Tob Control 2013;22:19–23. 10.1136/tobaccocontrol-2011-050044 [DOI] [PubMed] [Google Scholar]
- 8. McMillen RC, Gottlieb MA, Shaefer RM, et al. Trends in electronic cigarette use among U.S. adults: use is increasing in both smokers and nonsmokers. Nicotine Tob Res 2015;17:1195–202. 10.1093/ntr/ntu213 [DOI] [PubMed] [Google Scholar]
- 9. Orellana-Barrios MA, Payne D, Mulkey Z, et al. Electronic cigarettes - A narrative review for clinicians. Am J Med 2015;128:674–81. 10.1016/j.amjmed.2015.01.033 [DOI] [PubMed] [Google Scholar]
- 10. Hajek P. Electronic cigarettes for smoking cessation. Lancet 2013;382:1614–6. 10.1016/S0140-6736(13)61534-2 [DOI] [PubMed] [Google Scholar]
- 11. Hartmann-Boyce J, McRobbie H, Bullen C, et al. Electronic cigarettes for smoking cessation. Cochrane Database Syst Rev 2016;9 10.1002/14651858.CD010216.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Siegel MB, Tanwar KL, Wood KS. Electronic cigarettes as a smoking-cessation tool: results from an online survey. Am J Prev Med 2011;40:472–5. 10.1016/j.amepre.2010.12.006 [DOI] [PubMed] [Google Scholar]
- 13. Zhu SH, Zhuang YL, Wong S, et al. E-cigarette use and associated changes in population smoking cessation: evidence from US current population surveys. BMJ 2017;358:j3262–8. 10.1136/bmj.j3262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Friend K, Levy DT. Reductions in smoking prevalence and cigarette consumption associated with mass-media campaigns. Health Educ Res 2002;17:85–98. 10.1093/her/17.1.85 [DOI] [PubMed] [Google Scholar]
- 15. Giovenco DP, Delnevo CD. Prevalence of population smoking cessation by electronic cigarette use status in a national sample of recent smokers. Addict Behav 2018;76:129–34. 10.1016/j.addbeh.2017.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Rahman MA, Hann N, Wilson A, et al. E-cigarettes and smoking cessation: evidence from a systematic review and meta-analysis. PLoS One 2015;10:1–16. 10.1371/journal.pone.0122544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Etter JF, Bullen C. A longitudinal study of electronic cigarette users. Addict Behav 2014;39:491–4. 10.1016/j.addbeh.2013.10.028 [DOI] [PubMed] [Google Scholar]
- 18. Brose LS, Hitchman SC, Brown J, et al. Is the use of electronic cigarettes while smoking associated with smoking cessation attempts, cessation and reduced cigarette consumption? A survey with a 1-year follow-up. Addiction 2015;110:1160–8. 10.1111/add.12917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Khoudigian S, Devji T, Lytvyn L, et al. The efficacy and short-term effects of electronic cigarettes as a method for smoking cessation: a systematic review and a meta-analysis. Int J Public Health 2016;61:257–67. 10.1007/s00038-016-0786-z [DOI] [PubMed] [Google Scholar]
- 20. Malas M, van der Tempel J, Schwartz R, et al. Electronic cigarettes for smoking cessation: a systematic review. Nicotine Tob Res 2016;18:1926–36. 10.1093/ntr/ntw119 [DOI] [PubMed] [Google Scholar]
- 21. El Dib R, Suzumura EA, Akl EA, et al. Electronic nicotine delivery systems and/or electronic non-nicotine delivery systems for tobacco smoking cessation or reduction: a systematic review and meta-analysis. BMJ Open 2017;7:e012680–7. 10.1136/bmjopen-2016-012680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Grana RA, Popova L, Ling PM. A longitudinal analysis of electronic cigarette use and smoking cessation. JAMA Intern Med 2014;174:812–4. 10.1001/jamainternmed.2014.187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kalkhoran S, Glantz SA. E-cigarettes and smoking cessation in real-world and clinical settings: a systematic review and meta-analysis. Lancet Respir Med 2016;4:116–28. 10.1016/S2213-2600(15)00521-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Doran N, Brikmanis K, Petersen A, et al. Does e-cigarette use predict cigarette escalation? A longitudinal study of young adult non-daily smokers. Prev Med 2017;100:279–84. 10.1016/j.ypmed.2017.03.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Pechacek TF, Nayak P, Gregory KR, et al. The potential that electronic nicotine delivery systems can be a disruptive technology: results from a national survey. Nicotine Tob Res 2016;18:1989–97. 10.1093/ntr/ntw102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kasza KA, Ambrose BK, Conway KP, et al. Tobacco product use by youth and adults in the United States in 2013 and 2014. N Engl J Med 2017;376:342–53. 10.1056/NEJMsa1607538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. USDHHS. Population Assessment of Tobacco and Health (PATH) Study [United States] public-use files: user guide. ICPSR36498-v1. 2016. 10.3886/ICPSR36498.v1 [DOI]
- 28. Hyland A, Ambrose BK, Conway KP, et al. Design and methods of the Population Assessment of Tobacco and Health (PATH) Study. Tob Control 2017;26 10.1136/tobaccocontrol-2016-052934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. U.S. Department of Health and Human Services. Annual update of the HHS poverty guidelines, 2014. [Google Scholar]
- 30. U.S. Department of Health and Human Services. Annual update of the HHS poverty guidelines, 2013. [Google Scholar]
- 31. Moore D, Aveyard P, Connock M, et al. Effectiveness and safety of nicotine replacement therapy assisted reduction to stop smoking: systematic review and meta-analysis. BMJ 2009;338:b1024 10.1136/bmj.b1024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Coleman BN, Rostron B, Johnson SE, et al. Electronic cigarette use among US adults in the Population Assessment of Tobacco and Health (PATH) Study, 2013-2014. Tob Control 2017;26:e117–e126. 10.1136/tobaccocontrol-2016-053462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Delnevo CD, Giovenco DP, Steinberg MB, et al. Patterns of electronic cigarette use among adults in the United States. Nicotine Tob Res 2016;18:715–9. 10.1093/ntr/ntv237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Caponnetto P, Auditore R, Russo C, et al. Impact of an electronic cigarette on smoking reduction and cessation in schizophrenic smokers: a prospective 12-month pilot study. Int J Environ Res Public Health 2013;10:446–61. 10.3390/ijerph10020446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Begh R, Lindson-Hawley N, Aveyard P. Does reduced smoking if you can’t stop make any difference? BMC Med 2015;13:257 10.1186/s12916-015-0505-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Shi Y, Pierce JP, White M, et al. E-cigarette use and smoking reduction or cessation in the 2010/2011 TUS-CPS longitudinal cohort. BMC Public Health 2016. 16 10.1186/s12889-016-3770-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Levy DT, Yuan Z, Luo Y, et al. The relationship of e-cigarette use to cigarette quit attempts and cessation: Insights from a large, nationally representative U.S. survey. Nicotine Tob Res 2017. 10.1093/ntr/ntx166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Biener L, Hargraves JL. A longitudinal study of electronic cigarette use among a population-based sample of adult smokers: association with smoking cessation and motivation to quit. Nicotine Tob Res 2015;17:127–33. 10.1093/ntr/ntu200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hitchman SC, Brose LS, Brown J, et al. Associations between E-Cigarette type, frequency of use, and quitting smoking: Findings from a longitudinal online panel survey in Great Britain. Nicotine Tob Res 2015;17:1187–94. 10.1093/ntr/ntv078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Seidenberg AB, Jo CL, Ribisl KM. Differences in the design and sale of e-cigarettes by cigarette manufacturers and non-cigarette manufacturers in the USA. Tob Control 2016;25:e3–e5. 10.1136/tobaccocontrol-2015-052375 [DOI] [PubMed] [Google Scholar]
- 41. Wagener TL, Floyd EL, Stepanov I, et al. Have combustible cigarettes met their match? The nicotine delivery profiles and harmful constituent exposures of second-generation and third-generation electronic cigarette users. Tob Control 2017;26:e23–e28. 10.1136/tobaccocontrol-2016-053041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Farsalinos KE, Spyrou A, Tsimopoulou K, et al. Nicotine absorption from electronic cigarette use: comparison between first and new-generation devices. Sci Rep 2014;4:4133 10.1038/srep04133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Cahn Z, Siegel M. Electronic cigarettes as a harm reduction strategy for tobacco control: a step forward or a repeat of past mistakes? J Public Health Policy 2011;32:16–31. 10.1057/jphp.2010.41 [DOI] [PubMed] [Google Scholar]
- 44. Gornall J. Why e-cigarettes are dividing the public health community. BMJ 2015;350:h3317 10.1136/bmj.h3317 [DOI] [PubMed] [Google Scholar]
- 45. Farsalinos KE, Tsiapras D, Kyrzopoulos S, et al. Acute effects of using an electronic nicotine-delivery device (electronic cigarette) on myocardial function: comparison with the effects of regular cigarettes. BMC Cardiovasc Disord 2014;14:78 10.1186/1471-2261-14-78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Yan XS, D’Ruiz C, D’Ruiz C. Effects of using electronic cigarettes on nicotine delivery and cardiovascular function in comparison with regular cigarettes. Regul Toxicol Pharmacol 2015;71:24–34. 10.1016/j.yrtph.2014.11.004 [DOI] [PubMed] [Google Scholar]
- 47. Goniewicz ML, Knysak J, Gawron M, et al. Levels of selected carcinogens and toxicants in vapour from electronic cigarettes. Tob Control 2014;23:133–9. 10.1136/tobaccocontrol-2012-050859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Pisinger C, Døssing M. A systematic review of health effects of electronic cigarettes. Prev Med 2014;69:248–60. 10.1016/j.ypmed.2014.10.009 [DOI] [PubMed] [Google Scholar]
- 49. Antoniewicz L, Bosson JA, Kuhl J, et al. Electronic cigarettes increase endothelial progenitor cells in the blood of healthy volunteers. Atherosclerosis 2016;255:179–85. 10.1016/j.atherosclerosis.2016.09.064 [DOI] [PubMed] [Google Scholar]
- 50. Carnevale R, Sciarretta S, Violi F, et al. Acute impact of tobacco vs electronic cigarette smoking on oxidative stress and vascular function. Chest 2016;150:606–12. 10.1016/j.chest.2016.04.012 [DOI] [PubMed] [Google Scholar]
- 51. Soneji S, Barrington-Trimis JL, Wills TA, et al. Association between initial use of e-cigarettes and subsequent cigarette smoking among adolescents and young adults: a systematic review and meta-analysis. JAMA Pediatr 2017;171:788–22. 10.1001/jamapediatrics.2017.1488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Loukas A, Marti CN, Cooper M, et al. Exclusive e-cigarette use predicts cigarette initiation among college students. Addict Behav 2018;76:343–7. 10.1016/j.addbeh.2017.08.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Barrington-Trimis JL, Urman R, Berhane K, et al. E-cigarettes and future cigarette use. Pediatrics 2016;138:e20160379 10.1542/peds.2016-0379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Leventhal AM, Strong DR, Kirkpatrick MG, et al. Association of electronic cigarette use with initiation of combustible tobacco product smoking in early adolescence. JAMA 2015;314:700–7. 10.1001/jama.2015.8950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Conner M, Grogan S, Simms-Ellis R, et al. Do electronic cigarettes increase cigarette smoking in UK adolescents? Evidence from a 12-month prospective study. Tob Control 2017:. 10.1136/tobaccocontrol-2016-053539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Lozano P, Barrientos-Gutierrez I, Arillo-Santillan E, et al. A longitudinal study of electronic cigarette use and onset of conventional cigarette smoking and marijuana use among Mexican adolescents. Drug Alcohol Depend 2017;180:427–30. 10.1016/j.drugalcdep.2017.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Kozlowski LT, Warner KE. Adolescents and e-cigarettes: objects of concern may appear larger than they are. Drug Alcohol Depend 2017;174:209–14. 10.1016/j.drugalcdep.2017.01.001 [DOI] [PubMed] [Google Scholar]
- 58. Etter JF. E-cigarettes: methodological and ideological issues and research priorities. BMC Med 2015;13:32 10.1186/s12916-014-0264-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Villanti AC, Feirman SP, Niaura RS, et al. How do we determine the impact of e-cigarettes on cigarette smoking cessation or reduction? Review and recommendations for answering the research question with scientific rigor. Addiction 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Soulakova JN, Hartman AM, Liu B, et al. Reliability of adult self-reported smoking history: data from the tobacco use supplement to the current population survey 2002-2003 cohort. Nicotine Tob Res 2012;14:952–60. 10.1093/ntr/ntr313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Malarcher A, Dube S, Shaw L, et al. Centers for Disease Control and Prevention (CDC). Quitting smoking among adults--United States, 2001-2010. MMWR Morb Mortal Wkly Rep 2011;60:1513–9. [PubMed] [Google Scholar]
- 62. Hughes JR, Keely J, Naud S. Shape of the relapse curve and long-term abstinence among untreated smokers. Addiction 2004;99:29–38. 10.1111/j.1360-0443.2004.00540.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
tobaccocontrol-2017-054108supp001.pdf (369.6KB, pdf)