Abstract
Background
Outcomes of veterans with ESRD may differ depending on where they receive dialysis and who finances this care, but little is known about variation in outcomes across different dialysis settings and financial arrangements.
Methods
We examined survival among 27,241 Veterans Affairs (VA)–enrolled veterans who initiated chronic dialysis in 2008–2011 at (1) VA-based units, (2) community-based clinics through the Veterans Affairs Purchased Care program (VA-PC), (3) community-based clinics under Medicare, or (4) more than one of these settings (“dual” care). Using a Cox proportional hazards model, we compared all-cause mortality across dialysis settings during the 2-year period after dialysis initiation, adjusting for demographic and clinical characteristics.
Results
Overall, 4% of patients received dialysis in VA, 11% under VA-PC, 67% under Medicare, and 18% in dual settings (nearly half receiving dual VA and VA-PC dialysis). Crude 2-year mortality was 25% for veterans receiving dialysis in the VA, 30% under VA-PC, 42% under Medicare, and 23% in dual settings. After adjustment, dialysis patients in VA or in dual settings had significantly lower 2-year mortality than those under Medicare; mortality did not differ in VA-PC and Medicare dialysis settings.
Conclusions
Mortality rates were highest for veterans receiving dialysis in Medicare or VA-PC settings and lowest for veterans receiving dialysis in the VA or dual settings. These findings inform institutional decisions about provision of dialysis for veterans. Further research identifying processes associated with improved survival for patients receiving VA-based dialysis may be useful in establishing best practices for outsourced veteran care.
Keywords: dialysis, mortality, end-stage renal disease, Medicare, Veterans Affairs, community care
The challenges of providing timely and high-quality care to veterans has garnered significant media and congressional attention, culminating most recently in the 2014 Veterans Choice and the 2018 Veterans Affairs (VA) Mission Acts, intended to increase access to community care for veterans. However, the VA has a long history of provision of community care, including dialysis services, that predates recent legislation.1 Dialysis for patients with ESRD has been a longstanding concern to the VA because veterans with ESRD are one of the fastest growing and most costly population with chronic conditions1–5 within the VA.
VA-enrolled veterans can obtain dialysis in a variety of different settings: (1) at one of the VA’s 74 in-house dialysis units; (2) VA-financed, community-based dialysis through the Purchased Care program (VA-PC); or (3) in Medicare-certified, community-based dialysis clinics, if they qualify for the ESRD entitlement (Medicare eligibility under the ESRD entitlement occurs 90 days after ESRD for those not already enrolled in Medicare because of age or disability). Most VA-enrolled veterans receive dialysis under Medicare.6 Many of the remaining patients receive treatment via VA-PC under their local authority, when VA facilities are unable to meet veteran demand for maintenance dialysis (e.g., insufficient capacity or geographic inaccessibility),7 and only approximately 4% receive dialysis within the VA. This system of VA-outsourced, non-VA dialysis under VA-PC was in place before the introduction of the Veterans Choice Act, the VA Mission Act, and the new VA Community Care Program, which expanded access to community care for a wide range of services but explicitly excludes chronic dialysis.8 Thus, VA-PC remains the only source of VA-financed dialysis in community settings and is one of the fastest growing source of dialysis for veterans. Over the past two decades, the share of VA dialysis expenditures on VA-PC community-based dialysis has increased markedly, from 17% in 1993 to 81% in 2017,9–11 and a growing proportion of VA patients on dialysis receive treatment in the private sector: 56% received treatment through VA-PC in 2008 compared with 77% in 2017.12
Outcomes of veterans’ care delivered in VA and non-VA settings have been compared across a wide range of conditions.13,14 Most notably, inpatient care for myocardial infarction, heart failure, or chronic obstructive pulmonary disorder is associated with lower mortality rates in VA compared with non-VA hospitals.15,16 To date, little is known about variation in veterans’ outcomes across different dialysis settings and financial arrangements. Recent analyses have shown that survival among veterans with CKD differs by VA and non-VA providers,4,17–19 which may be a function of differences in patient characteristics, quality of care, and care coordination across settings. Prior research using smaller, regional samples of veterans receiving dialysis (in 2001–2004 and 2007–2008) have yielded mixed results on differences in hospitalization and mortality outcomes across dialysis treatment settings.20–22 Among a 2008–2011 national cohort who received dialysis between 2008 and 2011, we found similar hospitalization rates for the 2 years after dialysis initiation across VA, VA-PC, Medicare, and multiple (i.e., dual) settings.6
This study compared 2-year all-cause mortality in a national cohort of veterans receiving outpatient dialysis in VA, VA-PC, Medicare, or more than one of these settings (dual settings). In contrast to a recent analysis that found differences in 1-year outcomes among veterans initiating treatment in VA and non-VA dialysis units,19 this study applied a more granular assessment by comparing outcomes across four dialysis settings (VA, VA-PC, Medicare, and dual use by more than one of these first three settings) up to 2 years after dialysis initiation. Distinguishing between veterans who receive dialysis under Medicare and VA-PC is important because although the VA pays for dialysis care in the community, they have little direct control over the quality of this care. Further, not all community-based dialysis facilities participate in the VA-PC program and this selection may associate with outcomes. We also examined dialysis utilization and mortality up to 2 years after dialysis initiation, instead of patients’ initial dialysis provider assignment and 1-year mortality as in the analysis by Streja et al.19 Finally, we adjust for a broad set of risk factors that have not been considered in prior work, to reduce unobserved confounding as much as possible.
As federal and VA policymakers address concerns about access, utilization, and outcomes of care among veterans, empirical evidence can be helpful in informing efforts to refine policies and approaches to care delivery. Mortality is an important quality indicator for patients on dialysis, but as a federal provider, the VA is not systematically included in public reports on dialysis provider quality, and community dialysis providers do not provide results for veterans dialyzing in those units. Understanding outcomes of veterans’ dialysis care is critical to identifying contributors to better survival among this vulnerable patient group and to inform patient decision-making and VA policy and strategic planning for care models to meet the future needs of the veteran population with ESRD.
Methods
Data, Study Design, and Cohort
We conducted a retrospective, cohort study of VA-enrolled veterans with ESRD who initiated maintenance dialysis between 2008 and 2011, using VA and Medicare data up to 2013 to observe 2 years of dialysis utilization and outcomes in VA and non-VA settings, as described elsewhere.6 VA data sources included enrollment files, inpatient and outpatient encounters, and non-VA community care financed by the VA. Medicare data included enrollment and claims files and the US Renal Data System (USRDS), the comprehensive national registry of all patients with ESRD and providers in the United States.23
Veterans included in our study were enrolled in, obtained health care services from, or received compensation or pension benefits from VA24 and initiated maintenance dialysis between 2008 and 2011. Veterans were excluded from the cohort if they received a renal transplant or died within the first 90 days or recovered renal function within the first 180 days after dialysis initiation (because their exposure to financing options and outpatient dialysis treatment were too limited to derive meaningful associations). We also excluded those who did not have a valid residential postal code or lived outside the United States (i.e., Puerto Rico) at the time of dialysis initiation; or had incomplete demographic or clinical information at the time of dialysis initiation in the USRDS. We also excluded veterans who were enrolled in Medicare Advantage or had unknown Medicare status at baseline; those without any VA, VA-PC, or Medicare claims or encounters for outpatient dialysis; and those hospitalized throughout the follow-up period. The final cohort included 27,241 veterans (Supplemental Figure 1).
Outcome and Covariates
The outcome of interest was death after the first 90 days up to 2 years after dialysis initiation, ascertained via VA administrative data supplemented with information from the USRDS. The explanatory variable of interest was dialysis treatment setting, defined as follows: exclusively VA dialysis (VA), exclusively VA-PC, exclusively Medicare-financed dialysis (Medicare), or dual dialysis across more than one of these settings. This exposure was on the basis of outpatient dialysis claims/encounters beginning at day 1 of initiation until either the end of the 2-year follow up or the date of death or renal transplant. In anticipation of variation in veterans’ dialysis settings over time, dialysis setting was initially identified in quarterly increments. Because the majority of patients (>80%) had no variation in dialysis setting throughout follow-up (Supplemental Figure 2), we collapsed dialysis setting into a time-invariant observation per patient for the primary analysis. This time-invariant measure represents dialysis setting over each participant’s observation period (2 years for participants who did not have renal transplant or did not die) and comprises veterans receiving care in dual settings within a quarter (e.g., VA and Medicare in a quarter) and across quarters (e.g., exclusively VA in one quarter and exclusively Medicare in another).6 We retained the time-varying quarterly dialysis setting variable, where dual setting comprises veterans receiving care in dual settings only within a quarter (e.g., VA and Medicare in a quarter), for sensitivity analysis.
Patient demographic characteristics at the time of dialysis initiation, constructed from VA, USRDS, and Medicare administrative data, included age, race/ethnicity, sex, employment status, regional and urban residential status, and calendar year of dialysis initiation. Clinical characteristics included baseline eGFR at dialysis initiation, receipt of pre-ESRD nephrology care within or outside the VA in the 2 years before ESRD onset, incident dialysis modality, type of vascular access at time of dialysis initiation, history of renal transplant, cause of ESRD (e.g., diabetes, hypertension), 29 indicators of diagnosed physical health conditions and mental health comorbidity,25,26 body mass index, hospitalization and institutionalization in the year before dialysis initiation, and hospice use in the 90 days before dialysis initiation. We also ascertained whether patients initiated dialysis in the inpatient setting, which may reflect illness severity/acuity and/or local practices.27
We also constructed baseline financial and geographic access characteristics that might be expected to influence veterans’ dialysis setting: insurance coverage derived from Medicare enrollment and self-report in the ESRD Medical Evidence Form23 (Medicare, Medicaid, private insurance, other), VA copayment exempt versus nonexempt status (determined on the basis of low income or service-related disability), straight-line distances from residence to nearest VA outpatient dialysis unit and to nearest VA medical center (VAMC), and degree of VA reliance for other outpatient care.28 Finally, we adjusted for several characteristics of the VAMC most frequented by (or else nearest to) each veteran, including whether the VAMC had nephrology services or a dialysis unit on site, and the 2011 fiscal year occupancy rate of each veteran’s nearest VA outpatient dialysis unit.
Statistical Analyses
Descriptive statistics, Kaplan–Meier survival curves, and crude mortality rates were assessed by dialysis treatment setting. For our primary analysis, a cause-specific multivariable Cox proportional hazard model29 was fit to examine the association between time-invariant dialysis treatment setting (i.e., over the entire 2-year observation after dialysis initiation) and survival (assessed quarterly). Patients were censored from analysis if they had a renal transplant during the observation period, or at the end of the 2-year follow-up period. This model controlled for demographic, clinical, and access characteristics detailed above. Proportional hazard assumptions were assessed by inspection of log(−log [survival]) curves and weighted Schoenfeld residuals, and were found to be adequate.
We conducted additional sensitivity analyses to address the issue of no observed dialysis in a quarter and the potential for immortal survival time bias for dual-setting users. First, 16% of cohort members had at least one quarter during follow-up in which no outpatient dialysis was observed, as may occur when patients are admitted to a hospital, receive dialysis under private insurance, or stop dialysis treatment. To determine if inclusion of these patients may have affected our results (i.e., the effect of having no dialysis in a quarter), we repeated the primary analysis model and included a variable indicating whether the veteran had no observed outpatient dialysis during at least one quarter in their follow up. Second, as cohort members who survived for longer periods of time had more opportunity to receive dialysis in dual settings, we examined the potential for immortal time bias for dual users. To evaluate the effect of immortal time bias, we fit a Cox model with a quarterly, time-varying dialysis setting variable, where for each observed quarter, veterans were coded as having VA, VA-PC, Medicare, dual, or no observed outpatient dialysis. We also examined the association of dialysis setting with mortality on the basis of treatment assignment in the first quarter only (VA, VA-PC, Medicare, dual, and no observed outpatient dialysis). All analyses were performed with SAS version 9.4 (SAS Institute Inc., Cary, NC). This study was approved by the Institutional Review Board of the Durham VA Health Care System (MIRB 01746/0014).
Results
Characteristics of Patient Cohort
Cohort members had a mean age of 71 years and were predominantly men (98%), white (67%), retired (83%), and already enrolled in Medicare at the time of dialysis initiation (94%; Table 1). Smaller proportions of patients were covered under Medicaid (15%) or an employer group health plan (15%) or had other insurance (34%) as determined by information from Centers for Medicare & Medicaid Services form 2728. Nearly two thirds of veterans lived at least 30 miles from the nearest VA outpatient dialysis unit. Over half of veterans initiated dialysis with an eGFR<10 ml/min per 1.73 m2. Most veterans were living in urban areas (85%) and 44% were living in Southern states. Overall, 60% of the cohort had diabetes, 74% had hypertension, 52% had congestive heart failure, and 38% had a mental health diagnosis. The majority of veterans had received prior nephrology care for up to 2 years (86%) before initiation of dialysis, and 61% had been hospitalized in the year before initiation.
Table 1.
Patient characteristics at dialysis initiation, by veterans’ dialysis setting utilization
| Characteristic | Overall | VA Dialysis | VA-PC | Medicare | Dual | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | (%) | N | (%) | N | (%) | N | (%) | N | (%) | |
| Sample size | 27,241 | (100.0) | 1100 | (100.0) | 3079 | (100.0) | 18,215 | (100.0) | 4847 | (100.0) |
| Time in study, mean | 586.1 | 630.7 | 617.3 | 561.3 | 649.2 | |||||
| Event/outcome: death | 9919 | (36.4) | 269 | (24.5) | 925 | (30.0) | 7621 | (41.8) | 1104 | (22.8) |
| Censor event: renal transplant | 628 | (2.3) | 25 | (2.3) | 56 | (1.8) | 422 | (2.3) | 125 | (2.6) |
| Censored because of end of follow-up | 16,694 | (61.3) | 806 | (73.3) | 2098 | (68.1) | 10,172 | (55.8) | 3618 | (74.6) |
| No outpatient dialysis in at least one quarter | 4234 | (15.5) | 311 | (28.3) | 391 | (12.7) | 2936 | (16.1) | 596 | (12.3) |
| ESRD incident yeara | ||||||||||
| 2008 | 6905 | (25.3) | 279 | (25.4) | 635 | (20.6) | 4775 | (26.2) | 1216 | (25.1) |
| 2009 | 6910 | (25.4) | 269 | (24.5) | 736 | (23.9) | 4673 | (25.7) | 1232 | (25.4) |
| 2010 | 6855 | (25.2) | 258 | (23.5) | 843 | (27.4) | 4503 | (24.7) | 1251 | (25.8) |
| 2011 | 6571 | (24.1) | 294 | (26.7) | 865 | (28.1) | 4264 | (23.4) | 1148 | (23.7) |
| Mena,b | 26,619 | (97.7) | 1070 | (97.3) | 3012 | (97.8) | 17,787 | (97.7) | 4750 | (98.0) |
| Age, yra,b | ||||||||||
| <55 | 2401 | (8.8) | 179 | (16.3) | 424 | (13.8) | 1066 | (5.9) | 732 | (15.1) |
| 55–64 | 6526 | (24.0) | 471 | (42.8) | 1373 | (44.6) | 2563 | (14.1) | 2119 | (43.7) |
| 65–74 | 6577 | (24.1) | 230 | (20.9) | 682 | (22.2) | 4545 | (25.0) | 1120 | (23.1) |
| 75–84 | 8610 | (31.6) | 174 | (15.8) | 503 | (16.3) | 7212 | (39.6) | 721 | (14.9) |
| ≥85 | 3127 | (11.5) | 46 | (4.2) | 97 | (3.2) | 2829 | (15.5) | 155 | (3.2) |
| Racea,c | ||||||||||
| White | 18,328 | (67.3) | 403 | (36.6) | 1748 | (56.8) | 13,628 | (74.8) | 2549 | (52.6) |
| Black | 6801 | (25.0) | 555 | (50.5) | 1010 | (32.8) | 3453 | (19.0) | 1783 | (36.8) |
| Hispanic | 1331 | (4.9) | 111 | (10.1) | 210 | (6.8) | 654 | (3.6) | 356 | (7.3) |
| Other | 781 | (2.9) | 31 | (2.8) | 111 | (3.6) | 480 | (2.6) | 159 | (3.3) |
| Employment statusa | ||||||||||
| Full/part time | 1394 | (5.1) | 107 | (9.7) | 179 | (5.8) | 755 | (4.1) | 353 | (7.3) |
| Retired | 22,527 | (82.7) | 776 | (70.5) | 2398 | (77.9) | 15,785 | (86.7) | 3568 | (73.6) |
| Not employed | 3320 | (12.2) | 217 | (19.7) | 502 | (16.3) | 1675 | (9.2) | 926 | (19.1) |
| Urban residencea,b | 23,132 | (84.9) | 1061 | (96.5) | 2483 | (80.6) | 15,429 | (84.7) | 4159 | (85.8) |
| United States regiona,b | ||||||||||
| Midwest | 6224 | (22.8) | 250 | (22.7) | 580 | (18.8) | 4356 | (23.9) | 1038 | (21.4) |
| Northeast | 4495 | (16.5) | 228 | (20.7) | 221 | (7.2) | 3615 | (19.8) | 431 | (8.9) |
| South | 11,912 | (43.7) | 372 | (33.8) | 1680 | (54.6) | 7589 | (41.7) | 2271 | (46.9) |
| West | 4610 | (16.9) | 250 | (22.7) | 598 | (19.4) | 2655 | (14.6) | 1107 | (22.8) |
| Home VAMCa,b | ||||||||||
| Distance <30 miles (versus ≥30) | 13,407 | (49.2) | 954 | (86.7) | 1298 | (42.2) | 8486 | (46.6) | 2669 | (55.1) |
| Has nephrology service | 22,863 | (83.9) | 1060 | (96.4) | 2445 | (79.4) | 15,025 | (82.5) | 4333 | (89.4) |
| Has dialysis unit | 17,079 | (62.7) | 1083 | (98.5) | 1302 | (42.3) | 11,108 | (61.0) | 3586 | (74.0) |
| Nearest VA dialysisa,b | ||||||||||
| Distance <30 miles (versus ≥30) | 9802 | (36.0) | 978 | (88.9) | 416 | (13.5) | 6207 | (34.1) | 2201 | (45.4) |
| HD occupancy: 40%–79% | 6933 | (25.5) | 274 | (24.9) | 742 | (24.1) | 4884 | (26.8) | 1033 | (21.3) |
| HD occupancy: 80%–99% | 11,196 | (41.1) | 459 | (41.7) | 1350 | (43.8) | 7231 | (39.7) | 2156 | (44.5) |
| HD occupancy: 100% | 9112 | (33.4) | 367 | (33.4) | 987 | (32.1) | 6100 | (33.5) | 1658 | (34.2) |
| Insurancea,c | ||||||||||
| Medicaid | 4134 | (15.2) | 135 | (12.3) | 373 | (12.1) | 2913 | (16.0) | 713 | (14.7) |
| Medicare | 25,504 | (93.6) | 930 | (84.5) | 2612 | (84.8) | 17,728 | (97.3) | 4234 | (87.4) |
| Employer-based | 3938 | (14.5) | 95 | (8.6) | 212 | (6.9) | 3353 | (18.4) | 278 | (5.7) |
| Other | 9298 | (34.1) | 129 | (11.7) | 605 | (19.6) | 7750 | (42.5) | 814 | (16.8) |
| VA copayment requiredb | 8247 | (30.3) | 104 | (9.5) | 234 | (7.6) | 7453 | (40.9) | 456 | (9.4) |
| VA relianceb,c | ||||||||||
| No VA or Medicare use | 1499 | (5.5) | 23 | (2.1) | 68 | (2.2) | 1305 | (7.2) | 103 | (2.1) |
| 0%–50% | 16,430 | (60.3) | 49 | (4.5) | 276 | (9.0) | 15,362 | (84.3) | 743 | (15.3) |
| >50%–100% | 9312 | (34.2) | 1028 | (93.5) | 2735 | (88.8) | 1548 | (8.5) | 4001 | (82.5) |
| eGFRa, ml/min per 1.73 m2 | ||||||||||
| <10 | 14,048 | (51.6) | 678 | (61.6) | 1712 | (55.6) | 8806 | (48.3) | 2852 | (58.8) |
| 10–15 | 9065 | (33.3) | 313 | (28.5) | 974 | (31.6) | 6299 | (34.6) | 1479 | (30.5) |
| >15 | 4128 | (15.2) | 109 | (9.9) | 393 | (12.8) | 3110 | (17.1) | 516 | (10.6) |
| Body mass indexa | ||||||||||
| <18.5 | 595 | (2.2) | 30 | (2.7) | 66 | (2.1) | 399 | (2.2) | 100 | (2.1) |
| ≤18.5–24 | 8642 | (31.7) | 351 | (31.9) | 817 | (26.5) | 6144 | (33.7) | 1330 | (27.4) |
| 25–29 | 8930 | (32.8) | 334 | (30.4) | 944 | (30.7) | 6128 | (33.6) | 1524 | (31.4) |
| ≥30 | 9074 | (33.3) | 385 | (35.0) | 1252 | (40.7) | 5544 | (30.4) | 1893 | (39.1) |
| Primary cause of ESRDa | ||||||||||
| Diabetes | 12,224 | (44.9) | 582 | (52.9) | 1611 | (52.3) | 7507 | (41.2) | 2524 | (52.1) |
| Hypertension | 9060 | (33.3) | 260 | (23.6) | 882 | (28.6) | 6634 | (36.4) | 1284 | (26.5) |
| GN | 1520 | (5.6) | 74 | (6.7) | 161 | (5.2) | 960 | (5.3) | 325 | (6.7) |
| Other/uncertain | 4437 | (16.3) | 184 | (16.7) | 425 | (13.8) | 3114 | (17.1) | 714 | (14.7) |
| Prior health care utilizationa,b,c | ||||||||||
| Pre-ESRD nephrology | 23,301 | (85.5) | 1005 | (91.4) | 2531 | (82.2) | 15,412 | (84.6) | 4353 | (89.8) |
| Renal transplant | 337 | (1.2) | 14 | (1.3) | 22 | (0.7) | 244 | (1.3) | 57 | (1.2) |
| Hospitalization | 16,508 | (60.6) | 767 | (69.7) | 1960 | (63.7) | 10,707 | (58.8) | 3074 | (63.4) |
| Institutionalization | 4286 | (15.7) | 174 | (15.8) | 355 | (11.5) | 3210 | (17.6) | 547 | (11.3) |
| Hospice | 188 | (0.7) | 17 | (1.5) | 54 | (1.8) | 74 | (0.4) | 43 | (0.9) |
| Dialysis initiated during hospitalization | 15,476 | (56.8) | 510 | (46.4) | 1868 | (60.7) | 10,320 | (56.7) | 2778 | (57.3) |
| Incident dialysisa | ||||||||||
| In-center HD | 25,268 | (94.1) | 1026 | (93.3) | 2911 | (94.5) | 16,983 | (93.2) | 4708 | (97.1) |
| Home HD or PD | 1613 | (5.9) | 74 | (6.7) | 168 | (5.5) | 1232 | (6.8) | 139 | (2.9) |
| Dialysis access typea | ||||||||||
| Arterial venous fistula/graft | 6413 | (23.5) | 308 | (28.0) | 762 | (24.7) | 4016 | (22.0) | 1327 | (27.4) |
| Catheter | 19,211 | (70.5) | 713 | (64.8) | 2150 | (69.8) | 12,990 | (71.3) | 3358 | (69.3) |
| Other/unknown | 1617 | (5.9) | 79 | (7.2) | 167 | (5.4) | 1209 | (6.6) | 162 | (3.3) |
| Comorbid conditiona,b,c | ||||||||||
| Diabetes | 16,321 | (59.9) | 742 | (67.5) | 2156 | (70.0) | 10,057 | (55.2) | 3366 | (69.4) |
| Hypertension | 20,247 | (74.3) | 1013 | (92.1) | 2816 | (91.5) | 12,026 | (66.0) | 4392 | (90.6) |
| CHF | 14,183 | (52.1) | 499 | (45.4) | 1494 | (48.5) | 9840 | (54.0) | 2350 | (48.5) |
| COPD | 8007 | (29.4) | 292 | (26.5) | 921 | (29.9) | 5469 | (30.0) | 1325 | (27.3) |
| PVD | 6831 | (25.1) | 286 | (26.0) | 758 | (24.6) | 4664 | (25.6) | 1123 | (23.2) |
| Mental illness | 10,210 | (37.5) | 619 | (56.3) | 1658 | (53.8) | 5391 | (29.6) | 2542 | (52.4) |
| Hepatitis | 1694 | (6.2) | 167 | (15.2) | 326 | (10.6) | 535 | (2.9) | 666 | (13.7) |
| Anemia | 14,998 | (55.1) | 738 | (67.1) | 1887 | (61.3) | 9405 | (51.6) | 2968 | (61.2) |
| Arrhythmias | 9053 | (33.2) | 279 | (25.4) | 786 | (25.5) | 6849 | (37.6) | 1139 | (23.5) |
| Cerebrovascular disease | 4912 | (18.0) | 217 | (19.7) | 580 | (18.8) | 3246 | (17.8) | 869 | (17.9) |
| Coagulopathy | 2957 | (10.9) | 110 | (10.0) | 293 | (9.5) | 2087 | (11.5) | 467 | (9.6) |
| Dementia | 598 | (2.2) | 34 | (3.1) | 53 | (1.7) | 445 | (2.4) | 66 | (1.4) |
| Electrolytes | 15,449 | (56.7) | 661 | (60.1) | 1855 | (60.2) | 10,079 | (55.3) | 2854 | (58.9) |
| Hemiplegia | 520 | (1.91) | 30 | (2.7) | 61 | (2.0) | 325 | (1.8) | 104 | (2.1) |
| HIV | 201 | (0.7) | 18 | (1.6) | 34 | (1.1) | 71 | (0.4) | 78 | (1.6) |
| Ischemic heart disease | 13,628 | (50.0) | 438 | (39.8) | 1346 | (43.7) | 9709 | (53.3) | 2135 | (44.0) |
| Liver or mild liver disease | 1696 | (6.2) | 139 | (12.6) | 297 | (9.6) | 707 | (3.9) | 553 | (11.4) |
| Metastatic cancer | 480 | (1.8) | 19 | (1.7) | 54 | (1.8) | 351 | (1.9) | 56 | (1.2) |
| Other cancer/any tumor | 4736 | (17.4) | 193 | (17.5) | 478 | (15.5) | 3352 | (18.4) | 713 | (14.7) |
| Myocardial infarction | 5364 | (19.7) | 177 | (16.1) | 508 | (16.5) | 3896 | (21.4) | 783 | (16.2) |
| Other neurologic disorders | 2906 | (10.7) | 124 | (11.3) | 327 | (10.6) | 1956 | (10.7) | 499 | (10.3) |
| Paralysis | 1207 | (4.4) | 67 | (6.1) | 123 | (4.0) | 809 | (4.4) | 208 | (4.3) |
| Pulmonary circulatory disorder | 2520 | (9.3) | 88 | (8.0) | 305 | (9.9) | 1731 | (9.5) | 396 | (8.2) |
| Rheumatoid disease | 546 | 2.00 | 24 | (2.2) | 71 | (2.3) | 371 | (2.0) | 80 | (1.7) |
| Hypothyroidism | 3536 | (13.0) | 115 | (10.5) | 343 | (11.1) | 2561 | (14.1) | 517 | (10.7) |
| Ulcer disease | 1002 | (3.7) | 43 | (3.9) | 105 | (3.4) | 707 | (3.9) | 147 | (3.0) |
| Valvular disease | 4220 | (15.5) | 161 | (14.6) | 387 | (12.6) | 3091 | (17.0) | 581 | (12.0) |
| Weight loss | 2425 | (8.9) | 67 | (6.1) | 234 | (7.6) | 1835 | (10.1) | 289 | (6.0) |
| Inability to ambulate/transfer | 1714 | (6.3) | 78 | (7.1) | 164 | (5.3) | 1272 | (7.0) | 200 | (4.1) |
| Amputation | 902 | (3.3) | 54 | (4.9) | 146 | (4.7) | 511 | (2.8) | 191 | (3.9) |
Category indicators of variables shown are not all mutually exclusive (e.g., insurance coverage). VA reliance is defined as proportion of qualifying outpatient visits (Current Procedural Terminology codes 99201–99499) from all VA and Medicare visits during the 1 year before initiation of dialysis. Prior health care utilization look-back periods included 2 years for pre-ESRD nephrology care, 1 year for hospitalization and institutionalization, and one quarter for hospice care. HD, hemodialysis; PD, peritoneal dialysis; CHF, congestive heart failure; COPD, chronic obstructive pulmonary disorder, PVD, peripheral vascular disease.
USRDS.
Veterans Health Administration.
Medicare.
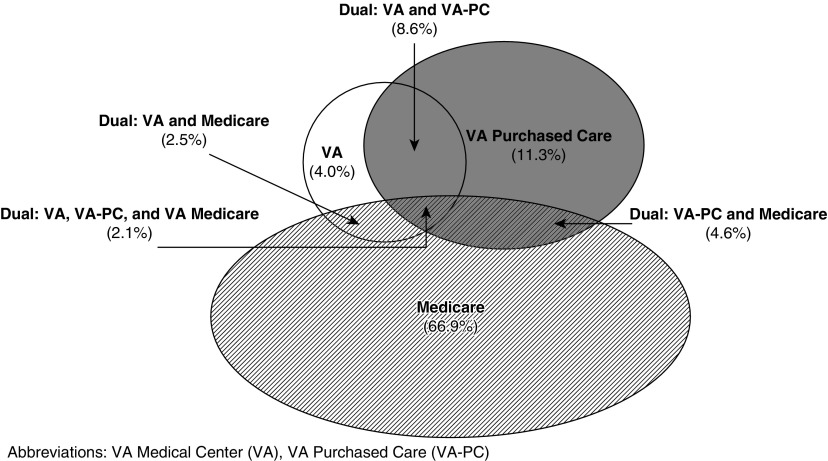
Two thirds of veterans received dialysis under Medicare exclusively throughout the 2-year observation period, 4% received dialysis only in the VA, 11% received dialysis outside the VA under VA-PC only, and 18% received dialysis under dual settings (within or across quarters) (Figure 1). Among the latter group, most received dialysis in multiple settings for a relatively short period of time over the 2-year observation period. However, a large proportion of dual users (>70%) had dual use in the first quarter and transitioned to exclusive single-setting use after the first quarter, with the largest proportion transitioning to VA-PC (Supplemental Figure 3). Moreover, 74% of dual use involved VA dialysis in the first 2 years after dialysis initiation, of which 48% comprised dual VA and VA-PC settings, exclusive of Medicare (Figure 1).
Figure 1.
The majority of veterans receive dialysis in non-VA settings and dual VA and non-VA settings in the 2 years after dialysis initiation.
As shown in Table 1, Medicare patients were predominantly older (55% aged ≥75 years) and white (75%), whereas patients on VA-only dialysis were younger (59% aged <65 years) and 61% were black or Hispanic. Veterans exclusively receiving dialysis in VA were mostly exempted from VA copayment (91%), lived fewer than 30 miles from a VA outpatient dialysis unit (89%), and roughly half had a mental health diagnosis (56%). VA-PC and Medicare patients were more likely to start dialysis during hospitalization and to have catheter versus permanent access placement as compared with patients on VA-only dialysis, and were less likely to have pre-ESRD nephrology care.
Two-Year Survival by Dialysis Treatment Setting
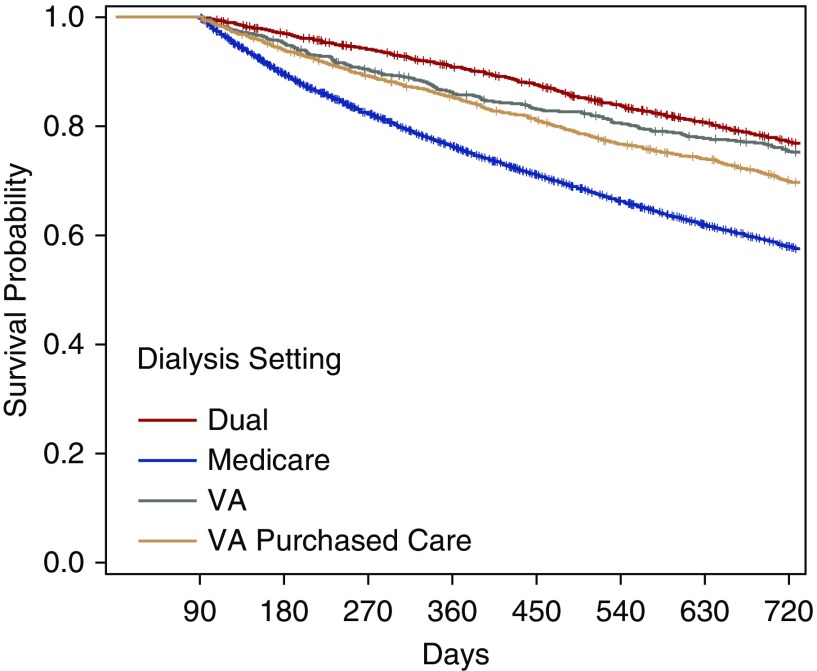
Crude 2-year mortality was 25% for veterans receiving VA dialysis only, 30% for VA-PC only, 42% for Medicare only, and 23% for veterans obtaining dialysis in more than one setting (Figure 2, Table 1).
Figure 2.
Unadjusted survival is lower in non-VA, compared to VA and dual dialysis settings. Time (in days) from dialysis initiation to renal transplantation, death, or end of follow-up period of observation. + denotes censored event (renal transplant or end of follow-up). Because of sample exclusion criteria, there are no observed deaths in the first 90 days after dialysis initiation.
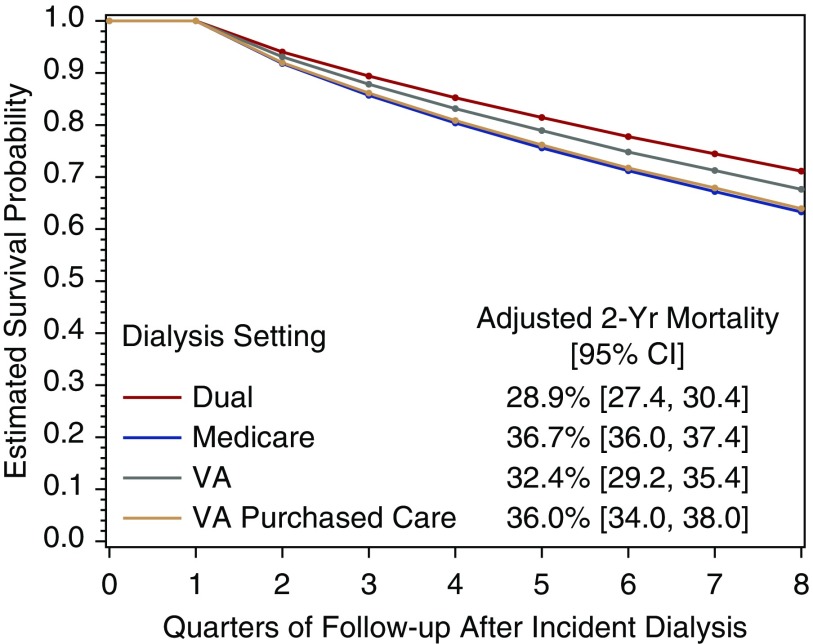
In the adjusted Cox model, dialysis setting was associated with 2-year mortality (P<0.001; Figure 3). Compared with veterans receiving dialysis exclusively from Medicare, 2-year mortality was lower for those dialyzing exclusively in the VA (hazard ratio (HR), 0.84; 95% confidence interval [95% CI], 0.73 to 0.96; P=0.01) and those receiving dialysis in dual settings (HR, 0.72; 95% CI, 0.66 to 0.78; P<0.001). There was no significant difference in mortality for veterans receiving dialysis through VA-PC compared with Medicare (HR, 0.97; 95% CI, 0.89 to 1.07; P=0.57). As shown in Figure 3, direct-adjusted estimates of 2-year mortality after dialysis initiation were 29% for veterans dialyzing in dual settings (95% CI, 27.4% to 30.4%), 32% for veterans receiving VA-only dialysis (95% CI, 29.2% to 35.4%), 36% for those receiving dialysis under VA-PC (95% CI, 34.0% to 38.0%), and 37% for those receiving dialysis exclusively through Medicare (95% CI, 36.0% to 37.4%). See Supplemental Table 1 for full model results.
Figure 3.
After adjustment in a Cox proportional hazards model, veterans' 2-year survival is lowest and nearly equivalent across both non-VA dialysis settings and higher in VA and dual settings. Direct adjusted survival functions, by dialysis setting (with time assessed quarterly), from dialysis initiation to censoring at renal transplantation or end of follow-up period of observation. Because of sample exclusion criteria, there are no observed deaths in the first 90 days after dialysis initiation. Estimated 2-year mortality rates were generated from the Cox regression model, adjusting for patient baseline demographic, clinical, financial, and geographic access characteristics (full set of model estimates are available in Supplemental Table 1).
Sensitivity Analyses
In the primary analysis model with time-invariant dialysis setting and the additional covariate identifying those who had at least one quarter in which there were no observed outpatient dialysis treatments (in at least one quarter during the 2-year follow up), we found a slightly greater reduction in 2-year mortality for VA settings compared with Medicare than in the primary model (Supplemental Table 1). We found similar associations for VA-PC and dual settings compared with Medicare, and a nearly two-fold greater risk of death for veterans with at least one quarter of no outpatient dialysis, compared with those with observed outpatient dialysis in all noncensored quarters of follow-up. In time-varying analyses of dialysis setting, mortality remained lower for those receiving dialysis in VA and dual settings compared with Medicare, and there was four-fold greater mortality among those with no quarterly outpatient dialysis (versus Medicare). For the model with dialysis setting that comprises only the initial quarter dialysis setting, we found no significant difference in mortality between dual versus Medicare setting within the first quarter (HR, 0.91; 95% CI, 0.83 to 1.01; P=0.06; full model results not shown).
Discussion
Among members of this national cohort of veterans who initiated dialysis between 2008 and 2011, we found that 2-year mortality rates were lower for those receiving dialysis exclusively in VA dialysis facilities and for those dialyzing in more than one setting than for those who received dialysis exclusively through Medicare. Further, mortality rates for veterans receiving dialysis in VA-PC settings were no different than for those receiving dialysis under Medicare. These findings are consistent with the results of a recent study that reported lower mortality among veterans beginning dialysis within the VA (versus non-VA providers) and provide the added insight that mortality rates are lower among veterans receiving dialysis exclusively in the VA or across multiple settings (including instances involving some dialysis within VA) up to 2 years after initiating dialysis, compared with those receiving dialysis under VA-PC or Medicare. Earlier studies had shown either no difference between VA and private sector dialysis,21 lower mortality among patients receiving dual VA and VA-PC compared with VA dialysis,22 or lower mortality among patients initiating dialysis in VA.19 These mixed findings were likely because of differences in study years, sampling strategy (regional versus national samples), data used (VA data versus merged VA and Medicare administrative data), and timeframe of observation (1- versus 2-year follow-up). This study improves upon earlier work by linking Medicare administrative and USRDS national registry data with VA administrative data and expanding the analysis on a national sample with a wider range of comparisons to reflect the array of dialysis treatment and financial arrangements available to veterans with ESRD. Consequently, our results reflect the most comprehensive cohort of veterans and data sources to date.
What might explain more favorable survival rates in cohort members who used VA dialysis or received dialysis in a dual setting compared with those who received dialysis under Medicare? Although the VA pays for dialysis in Medicare-certified dialysis facilities in the community, VA providers have little control over the quality of dialysis care for veterans in these facilities, and cross-system use may expose these patients to more fragmented care. Compared with veterans receiving dialysis exclusively under Medicare, those who dialyze exclusively within the VA likely have more ready access to comprehensive care benefits, care coordination due to colocation of dialysis and nondialysis services, and informational continuity stemming from VA’s seamless electronic medical record. Prior work demonstrating more favorable survival in VA than outside the VA did not compare outcomes among those receiving care under Medicare versus VA-PC. Our results reporting longer survival among veterans receiving VA dialysis than those receiving dialysis in the community under the VA-PC raise concerns about the outsourcing of dialysis care to the community for the veteran population.
Dialysis represents a significant care transition and receiving dialysis across multiple settings involves additional transitions that may place patients at higher risk for mortality. Although we hypothesized that those receiving care in more than one setting would be at risk for worse outcomes, the highest survival was found among veterans who received treatment in some combination of care under the auspices of VA and non-VA health systems (Figure 1, Table 1). Immortal time bias may have influenced our estimates because dual users had to survival multiple quarters to achieve the “dual” designation (notably half of dual users who received treatment in a single setting in the first quarter). However, the persistence of our findings in our sensitivity analyses (in which we modeled treatment exposures to minimize the potential for immortal time bias, albeit with HRs closer to 1.0), suggests that this bias is a partial but not complete explanation for the high survival among dual users. It is noteworthy that almost one in three of these patients received some of their dialysis care within the VA. This suggests the possibility that VA involvement in the first 2 years of maintenance dialysis is important for veteran outcomes, whether it plays a role in the initiation of dialysis, ongoing care, or care coordination of dialysis and nondialysis needs of veterans with ESRD, and is associated with longer survival. More work is needed to understand care patterns (i.e., sequencing of care settings), the merits of a dual-system approach, and the role that VA serves during care transitions that are attributable to favorable outcomes for those receiving care in the VA and community-based settings.
Survival was lowest for veterans exclusively dialyzing in VA-PC or Medicare, which suggests that the VA may want to ensure that high-quality community providers are available to all veterans needing dialysis care in the community. In addition, the VA should scrutinize its processes of care to identify best practices associated with improved outcomes and use this information to inform future community care purchasing agreements. Risk-adjusted or quality-based VA-PC outpatient dialysis payments may be a model for obtaining high-value community care for veterans. Collectively, our results argue for more study to understand how decisions about site of care are made, and the extent to which these decisions reflect the preferences of veterans versus system needs.
With increasing prevalence of ESRD among veterans and VA priorities to improve veterans’ access to care, assessing the consequences of the VA Health Care System’s “make versus buy” decision-making process for dialysis care is critically important.30 The tradeoffs of “making” more VA dialysis care must be balanced against the tradeoffs of “buying” outpatient dialysis care from providers in the private sector as well as potential savings in VA dollars related to other medical care. Our findings suggest considerations of both the clinical consequences and operational realties of effective and efficient provision of dialysis services to veterans. Although most veterans used Medicare benefits for dialysis care during the study period, the VA met increasing demand for VA dialysis through its in-house service and primarily through VA-PC in communities. However, our results raise the possibility that efforts to make additional VA capacity may improve both patient access to VA care and survival outcomes of patients otherwise receiving VA-PC, and also align services with veteran preferences and reduce VA-PC expenditures.31 However, VA and Medicare resources for patients with ESRD are quite different. The VA operates under a fixed global budget and is limited in its ability to expand in-house services. Nearly three times as many veterans obtained community dialysis via VA-PC than did from VA facilities, and demand for VA-PC dialysis continues to outpace current VA supply. The lower rates of survival among veterans receiving dialysis exclusively through VA-PC (compared with VA-only dialysis) also highlight potential opportunities to improve coordination and information-sharing of patient conditions through, for instance, augmented oversight or a platform to facilitate communication between providers to ensure that access to care and outcomes improve together. Our finding of lower mortality among veterans dialyzing in dual settings further underscores the importance and promise of improving VA partnerships with community providers to support treatment, coordination, and transitions of chronic dialysis care between VA and non-VA systems.7
There are study limitations that should be noted. First, results may not generalize to veterans receiving dialysis through Medicare Advantage or private insurance (approximately 9000 veterans) because we were not able observe dialysis claims from these sources, or to veterans initiating dialysis after 2011. Analyses were conducted among veterans initiating dialysis between 2008 and 2011 and may not reflect current trends in Centers for Medicare & Medicaid Services and VA payment and contracting policy, which have changed since 2012. Second, our results may be subject to unmeasured confounding and the associations described may not be causal. Systematic differences between veterans who dialyze in VA versus under VA-PC or Medicare suggest that our results may reflect the impact of unmeasured confounders, especially those pertaining to care during the pre-dialysis period, that are not captured in our analyses. Measures of social support including marital status, VA beneficiary travel reimbursement, and clinical measures were not uniformly available across VA-PC and Medicare data. Third, we were also unable to examine intermediate outcomes of dialysis treatment (e.g., urea reduction ratio, anemia treatment) that reflect the quality of dialysis care and influence risk for mortality because of the limited availability of laboratory data from non-VA settings. Finally, we were not able to identify or characterize VA-PC providers from the VA-PC claims. This is important because the majority of private-sector dialysis facilities are freestanding units and studies that found relationships between ESRD outcomes and dialysis facility characteristics have excluded the VA’s hospital-based facilities.32,33 Further research is needed to better understand whether observed differences in veterans’ dialysis outcomes are attributable to the type of provider to which VA is outsourcing its services.
Among members of a national cohort of veterans who started dialysis between 2008 and 2011, mortality rates were highest for those receiving dialysis in the community under Medicare or VA-PC, and lowest for veterans receiving dialysis in VA or in more than one setting. These findings argue for more work to understand the ways in which decisions about dialysis setting unfold, the role that VA plays in supporting veterans’ dialysis care, and processes and best practices associated with improved survival for veterans.
Disclosures
M.L.M. reports ownership of Amgen stock from his spouse’s employment. A.M.O. has received funding from the Department of Veterans Affairs, Centers for Disease Control and Prevention, and National Institutes of Health, as well as honoraria/speaker fees from UpToDate, Fresenius Medical Care, Dialysis Clinics Inc., the University of Alabama at Birmingham, and the Coalition for the Supportive Care of Kidney Patients. All other authors (V.W., C.J.C., K.M.S., T.S.Z.B., P.L.H., D.E., S.T.C., and H.J.W.) report no potential conflicts of interest.
Supplementary Material
Acknowledgments
The authors thank Dr. Michael Fischer, Dr. Wissam Kourany, and Dr. Rudy Rodriguez for scientific counsel and helpful comments to this manuscript.
V.W., C.J.C., P.L.H., D.E., A.M.O., S.T.C., and M.L.M. designed the study; V.W., K.M.S., T.S.Z.B., and H.J.W. obtained data and constructed variables for analysis; C.J.C. and K.M.S. analyzed the data; V.W., C.J.C., and K.M.S. made the figures; all authors interpreted the results, drafted and revised the paper, and approved the final version of the manuscript.
This study was funded by the Department of Veterans Affairs (VA) Health Services Research and Development Service (grant IIR 12-342) and a VA Research Career Scientist award (grant RCS 10-391), and was supported by the Center of Innovation for Health Services Research in Primary Care (grant CIN 13-410) at the Durham VA Medical Center.
The interpretation and reporting of these data are the responsibility of the authors and do not reflect the official policy or interpretation of the US Government or the Department of Veterans Affairs.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
This article contains the following supplemental material online at http://jasn.asnjournals.org/lookup/suppl/doi:10.1681/ASN.2018050521/-/DCSupplemental.
Supplemental Material
Supplemental Figure 1. Sampling frame.
Supplemental Figure 2. Visualization of veteran dialysis settings, by quarter.
Supplemental Figure 3. Visualization of veteran dual dialysis settings subcohort, by quarter.
Supplemental Table 1. Full regression results, including sensitivity analyses.
References
- 1.Watnick S, Crowley ST: ESRD care within the US Department of Veterans Affairs: A forward-looking program with an illuminating past. Am J Kidney Dis 63: 521–529, 2014 [DOI] [PubMed] [Google Scholar]
- 2.US Renal Data System (USRDS) : USRDS 2012 Annual Data Report: Atlas of End-Stage Renal Disease in the United States. Bethesda, MD, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases (NIH-NIDDK), 2012 [Google Scholar]
- 3.Veterans Health Administration : Allocation Resource Center: Fiscal Year 2011 Workload and Cost Report. Department of Veterans Affairs, Braintree, MA, 2012 [Google Scholar]
- 4.US Renal Data System (USRDS) : USRDS 2016 Annual Data Report, Volume 1: Chronic Kidney Disease in the United States. Bethesda, MD, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases (NIH-NIDDK), 2016 [Google Scholar]
- 5.Yoon J, Scott JY, Phibbs CS, Wagner TH: Recent trends in Veterans Affairs chronic condition spending. Popul Health Manag 14: 293–298, 2011 [DOI] [PubMed] [Google Scholar]
- 6.Wang V, Coffman CJ, Stechuchak KM, Berkowitz TSZ, Hebert PL, Edelman D, et al.: Comparative assessment of utilization and hospital outcomes of veterans receiving VA and non-VA outpatient dialysis [published online ahead of print August 9, 2018]. Health Serv Res 10.1111/1475-6773.13022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Crowley ST, Murphy K: Delivering a “New Deal” of kidney health opportunities to improve outcomes within the veterans health administration. Am J Kidney Dis 72: 444–450, 2018 [DOI] [PubMed] [Google Scholar]
- 8.Veterans Health Administration (VHA) Office of Community Care : Veterans Choice Program (VCP) Overview. Washington, DC, Department of Veteran Affairs, 2017 [Google Scholar]
- 9.Veterans Health Administration Health Economics Resource Center : VHA Costs in Cost Distribution Report, FY1993-FY2003. Department of Veterans Affairs, Menlo Park, CA, 2009 [Google Scholar]
- 10.Veterans Health Administration Allocation Resource Center : Workload and Cost Report. Department of Veterans Affairs, Braintree, MA, 2018 [Google Scholar]
- 11.Veterans Health Administration (VHA) : Purchase of Non-VA Hemodialysis Treatments, 2009. Washington, DC, Department of Veterans Affairs Chief Business Office, 2009 [Google Scholar]
- 12.Veterans Health Administration Office of the Under Secretary for Health Policy and Services : VHA Enrollment and Forecasting: Dialysis Patients and Utilization by Care Location, 2006–2017. Department of Veterans Affairs, Washington, DC, 2018
- 13.O’Hanlon C, Huang C, Sloss E, Anhang Price R, Hussey P, Farmer C, et al.: Comparing VA and non-VA quality of care: A systematic review. J Gen Intern Med 32: 105–121, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Trivedi AN, Matula S, Miake-Lye I, Glassman PA, Shekelle P, Asch S: Systematic review: Comparison of the quality of medical care in veterans affairs and non-veterans affairs settings. Med Care 49: 76–88, 2011 [DOI] [PubMed] [Google Scholar]
- 15.Blay E Jr, DeLancey JO, Hewitt DB, Chung JW, Bilimoria KY: Initial public reporting of quality at veterans affairs vs non-veterans affairs hospitals. JAMA Intern Med 177: 882–885, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nuti SV, Qin L, Rumsfeld JS, Ross JS, Masoudi FA, Normand SL, et al.: Association of admission to veterans affairs hospitals vs non-veterans affairs hospitals with mortality and readmission rates among older men hospitalized with acute myocardial infarction, heart failure, or pneumonia. JAMA 315: 582–592, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kalantar-Zadeh K, Crowley ST, Beddhu S, Chen JLT, Daugirdas JT, Goldfarb DS, et al.: Renal replacement therapy and incremental hemodialysis for veterans with advanced chronic kidney disease. Semin Dial 30: 251–261, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kurella Tamura M, Thomas IC, Montez-Rath ME, Kapphahn K, Desai M, Gale RC, et al.: Dialysis initiation and mortality among older veterans with kidney failure treated in medicare vs the department of veterans affairs. JAMA Intern Med 178: 657–664, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Streja E, Kovesdy CP, Soohoo M, Obi Y, Rhee CM, Park C, et al.: Dialysis provider and outcomes among United States veterans who transition to dialysis. Clin J Am Soc Nephrol 13: 1055–1062, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hynes DM, Koelling K, Stroupe K, Arnold N, Mallin K, Sohn MW, et al.: Veterans’ access to and use of Medicare and Veterans Affairs health care. Med Care 45: 214–223, 2007 [DOI] [PubMed] [Google Scholar]
- 21.Hynes DM, Stroupe KT, Fischer MJ, Reda DJ, Manning W, Browning MM, et al.: for ESRD Cost Study Group : Comparing VA and private sector healthcare costs for end-stage renal disease. Med Care 50: 161–170, 2012 [DOI] [PubMed] [Google Scholar]
- 22.Wang V, Maciejewski ML, Patel UD, Stechuchak KM, Hynes DM, Weinberger M: Comparison of outcomes for veterans receiving dialysis care from VA and non-VA providers. BMC Health Serv Res 13: 26, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.US Renal Data System : 2015 Researcher’s Guide to the USRDS Database. Bethesda, MD, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2016 [Google Scholar]
- 24.US Department of Veterans Affairs , VA Information Resource Center, 2014. Available at: https://vaww.virec.research.va.gov/VAMCS/Cohorts/Details.htm#. Accessed September 20, 2018 [Google Scholar]
- 25.Gagne JJ, Glynn RJ, Avorn J, Levin R, Schneeweiss S: A combined comorbidity score predicted mortality in elderly patients better than existing scores. J Clin Epidemiol 64: 749–759, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kilbourne AM, Morden NE, Austin K, Ilgen M, McCarthy JF, Dalack G, et al.: Excess heart-disease-related mortality in a national study of patients with mental disorders: Identifying modifiable risk factors. Gen Hosp Psychiatry 31: 555–563, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Arif FM, Sumida K, Molnar MZ, Potukuchi PK, Lu JL, Hassan F, et al.: Early mortality associated with inpatient versus outpatient hemodialysis initiation in a large cohort of US veterans with incident end-stage renal disease. Nephron 137: 15–22, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liu CF, Manning WG, Burgess JF Jr, Hebert PL, Bryson CL, Fortney J, et al.: Reliance on Veterans Affairs outpatient care by Medicare-eligible veterans. Med Care 49: 911–917, 2011 [DOI] [PubMed] [Google Scholar]
- 29.Van Der Pas S, Nelissen R, Fiocco M: Different competing risks models for different questions may give similar results in arthroplasty registers in the presence of few events. Acta Orthop 89: 145–151, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vanneman ME, Harris AHS, Asch SM, Scott WJ, Murrell SS, Wagner TH: Iraq and Afghanistan veterans' use of veterans health administration and purchased care before and after veterans choice program implementation. Med Care 55: S37–S44, 2017 [DOI] [PubMed] [Google Scholar]
- 31.Government Accountability Office (GAO) : VA Dialysis Pilot: Documentation of Plans for Concluding the Pilot Needed to Improve Transparency and Accountability (GAO-14-646). Washington, DC, Government Accountability Office, 2014
- 32.Garg PP, Frick KD, Diener-West M, Powe NR: Effect of the ownership of dialysis facilities on patients’ survival and referral for transplantation. N Engl J Med 341: 1653–1660, 1999 [DOI] [PubMed] [Google Scholar]
- 33.Hirth RA, Held PJ, Orzol SM, Dor A: Practice patterns, case mix, Medicare payment policy, and dialysis facility costs. Health Serv Res 33: 1567–1592, 1999 [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.