Abstract
Astragaloside IV (AST) is the major active saponin in Astragalus membranaceus and, reportedly, has a variety of pharmacological activities. However, the potential of AST to ameliorate high glucose-mediated renal tubular epithelial-mesenchymal transition (EMT) remains undetermined. The aim of the present research was to explore the effect and mechanism of AST in EMT of renal tubular epithelial cells, as an underlying mechanism of renal fibrosis and a vital feature involved in diabetic nephropathy. The effect of AST on the EMT of renal tubular epithelial cells (HK-2) stimulated by high glucose was investigated and it was attempted to elucidate the potential underlying mechanism. The expression of E-cadherin and α-smooth muscle actin were determined by western blotting and immunofluorescence assays. The expression of the mammalian target of rapamycin complex 1 (mTORC1)/ ribosomal protein S6 kinase β-1 (p70S6K) signaling pathway and protein levels of four transcriptional factors (snail, slug, twist and zinc finger E-box-binding homeobox 1) were also determined by western blotting. Additionally, extracellular matrix components, including fibronectin (FN) and collagen type IV (Col IV) were detected by ELISA. The results suggested that the EMT of HK-2 cells and the mTORC1/p70S6K pathway were activated by high glucose. The expression of snail and twist in HK-2 cells was elevated by high glucose. Furthermore, extracellular matrix components, FN and Col IV, were increased in HK-2 cells cultured with high glucose. In turn, treatment with AST reduced EMT features in HK-2 cells, inhibited mTORC1/p70S6K pathway activation, downregulated expression of snail and twist, and reduced secretion of FN and Col IV. In summary, the findings suggested that AST ameliorates high glucose-mediated renal tubular EMT by blocking the mTORC1/p70S6K signaling pathway in HK-2 cells.
Key words: astragaloside IV, renal tubular, epithelial-mesenchymal transition, mammalian target of rapamycin complex 1/ribosomal protein S6 kinase β-1 signaling
Introduction
Diabetes mellitus (DM) is a serious illness associated with an increased risk of cardiovascular complications, including dyslipidemia, coronary artery disease, hypertension and myocardial infarction (1,2). In addition to cardiovascular injury, two other affected vital organs are the kidney [diabetic nephropathy (DN)] and eyes (3), with DN being one of the most common complications for patients with diabetic (4,5). The pathogenesis of DN involves mesangial expansion, basement membrane thickening, glomerular hypertrophy and renal fibrosis (6-8), among which progressive renal fibrosis is the important pathological characteristic of DN (9). The epithelial-mesenchymal transition (EMT) of renal tubular epithelial cells is one of the underlying mechanisms of renal fibrosis and encompasses a range of events whereby epithelial cells no longer exhibit certain epithelial traits, such as E-cadherin expression, and instead acquire typical characteristics of mesenchymal cells, such as α-smooth muscle actin (α-SMA) expression (10). A number of studies have reported that the process is connected to the production of interstitial myofibro-blasts during nephropathy (11-13). Constant downregulation of E-cadherin is reported to occur via transcriptional repression, mediated by transcription factors including snail, slug, twist and zinc finger E-box-binding homeobox 1 (ZEB-1) (14-16), which control E-cadherin transcription by cross interaction with the E-box binding sites in the E-cadherin promoter (17,18). However, the cellular molecular mechanisms underlying EMT are not completely understood (19). Therefore, it is vital to clarify the pathogenic mechanisms of EMT to formulate appropriate interventions.
Mammalian target of rapamycin (mTOR) is a serine/threonine protein kinase that regulates a series of growth-associated cellular processes. mTOR includes two complexes termed mTOR complex 1 (mTORC1) and complex 2 (mTORC2) (20). However, only mTORC1 is sensitive to rapamycin inhibition, and controls cell proliferation and growth via the phosphorylation of certain downstream targets, such as ribosomal protein S6 kinase β-1 (p70S6K) (20). Aberrant activation of the mTORC1/p70S6K pathway has been reported to be involved in the pathogenesis of DN (21). Furthermore, mTORC1/p70S6K signaling may mediate renal tubular EMT during DN (19).
Astragaloside IV (AST) is a small molecular saponin that is one of the main active ingredients extracted from Astragalus membranaceus (22,23). Growing evidence has confirmed that AST has a wide spectrum of pharmacological effects (24-28). However, to the best of our knowledge, the effect of AST on the EMT of renal tubular cells during DN has not yet been reported. Therefore, the present study was performed to investigate whether AST has an effect on EMT in renal tubular cells and to clarify the potential mechanisms involved.
Materials and methods
Cell culture and intervention
HK-2, the human proximal tubular epithelial cell line, was obtained from the American Type Culture Collection (Manassas, VA, USA) and cultured in Dulbecco’s modified Eagle’s medium (DMEM) supplemented with 5.56 mmol/l D-glucose [normal glucose (NG)]. For induction of EMT, the HK-2 cells (at ~60% confluence) were cultivated with high glucose (HG) medium including 60 mmol/l D-glucose for 72 h (19). Mannitol medium including 5.56 mmol/l glucose and 54.44 mmol/l mannitol, was used as an osmotic control (MA). AST, purchased from Shanghai YuanYe Biotechnology Co., Ltd. (Shanghai, China), was added when the cell culture medium was changed from NG to HG medium at a concentration of 50 µg/ml [AST low (ASTL)], 100 µg/ml [AST medium (ASTM)] or 200 µg/ml [AST high (ASTH)]. For the rapamycin administration group (Rap), rapamycin (Cell Signaling Technology, Inc., Danvers, MA, USA) was added at a concentration of 20 nmol/l (19).
Western blot analysis
Protein was isolated from HK-2 cells using lysis buffer including 1% NP-40, 1 mmol/l Na3VO4, 1 mmol/l phenylmethylsulfonyl fluoride, 1 mmol/l EDTA, 20 mmol/l NaF, 50 mmol/l Tris (pH 7.6), and 150 mmol/l NaCl. The concentration of proteins was measured with a bicinchoninic acid protein assay kit (Beyotime Institute of Biotechnology, Haimen, China) following the manufacturer’s protocol. For immunoblotting, equivalent quantities of protein (80 µg) from the different groups were separated by SDS-PAGE on 8% gels and transferred onto polyvinylidene difluoride membranes (EMD Millipore, Billerica, MA, USA), which were blocked in TBS-Tween containing 3% bovine serum albumin (BSA) at room temperature for 1 h, and then incubated with primary antibodies at 4°C overnight. The primary antibodies against mTOR (cat. no. 2983T; 1:1,000), phospho-mTOR (Ser2448; cat. no. 5536T; 1:1,000), p70S6K (cat. no. 2708T; 1:1,000), phospho-p70S6K (Thr389; cat. no. 9234T; 1:1,000), snail (cat. no. 3879T; 1:1,000), slug (cat. no. 9585T; 1:1,000), twist (cat. no. 46702S; 1:1,000), ZEB-1 (cat. no. A1500; 1:1,000) and E-cadherin (cat. no. 3195T; 1:1,000) were purchased from Cell Signaling Technology, Inc., and against α-SMA (cat. no. ab32575; 1:1,000) and GAPDH (cat. no. ab181602; 1:1,000) from Abcam (Cambridge, UK). Secondary antibody (cat. no. C40721-02; 1:1,000) was obtained from LI-COR Biosciences, (Lincoln, NE, USA) and incubation was at 4°C overnight. Quantification was performed by measuring the signal intensity of the protein bands with ImageJ software v1.46 (National Institutes of Health, Bethesda, MD, USA).
Immunofluorescence
HK-2 cells (3×104/ml) were seeded into 12-well plates containing glass coverslips. Following treatment, they were washed three times with cold PBS and then fixed with 100% cold methanol for 20 min at -20°C. Following three more washes with PBS, the HK-2 cells were blocked in 5% BSA at room temperature for 1 h, and then labeled with E-cadherin (1:200; cat. no. 3195T; Cell Signaling Technology, Inc.) and α-SMA (1:500; cat. no. ab32575; Abcam) antibodies at room temperature for 2 h. The slips were then incubated with DyLight 594 donkey anti-rabbit IgG (1:200; cat. no. E032421-01; EarthOx Life Sciences, Millbrae, CA, USA) for 1 h at room temperature. Subsequently, the nuclei were counter-stained with DAPI for 2 min, and then the cells were washed with PBS three times prior to mounting with fluorescence mounting medium. Images were captured with an Olympus BX43F fluorescence microscope (Olympus Corporation, Tokyo, Japan).
ELISA
The protein levels of fibronectin (FN) and collagen type IV (Col IV) were measured via enzyme-linked immunosorbent assays (cat. nos. 30357H and 30588H; Shanghai Boyun Biotech Co., Ltd., Shanghai, China;) according to the manufacturer’s instructions.
Statistical analysis
Data are expressed as means ± standard error. Statistical analyses were performed using one-way analysis of variance for multiple data comparisons, followed by the Neuman-Keuls test. P<0.05 was considered to indicate a statistically significant difference.
Results
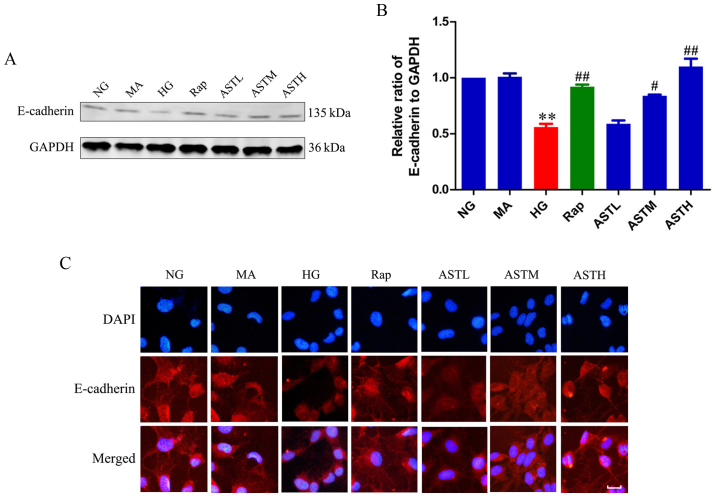
Effects of AST on E-cadherin expression
As demonstrated in Fig. 1A and B, the HG group exhibited significantly lower E-cadherin expression compared with the NG group (P<0.01). Additionally, the expression level of E-cadherin in the MA group did not differ significantly to that in the NG group, indicating that there were no obvious effects generated by the osmotic pressure. Rapamycin administration increased the expression of E-cadherin compared with HG treatment (P<0.01). Notably, the ASTM- and ASTH-treated groups also exhibited markedly higher E-cadherin expression compared with the HG group (P<0.05 and P<0.01, respectively). These results revealed E-cadherin expression was decreased in HK-2 cells induced by high glucose, detected by western blotting and immunofluorescence, while ASTM- and ASTH treatment could increase E-cadherin expression compared with HG (Fig. 1C).
Figure 1.
Effects of AST on E-cadherin expression in HK-2 cells. (A) Western blot analysis of E-cadherin. (B) Densitometry analysis of E-cadherin. (C) Expression of E-cadherin via immunofluorescence. Data are expressed as the mean ± standard error. n=3. Scale bar, 20 µm. **P<0.01 vs. NG; #P<0.05 vs. HG group; ##P<0.01 vs. HG group. AST, astragaloside IV; NG, normal glucose 5.56 mmol/l; MA, normal glucose 5.56 mmol/l + mannitol 54.44 mmol/l; HG, high glucose 60 mmol/l; Rap, high glucose + 20 nmol/l rapamycin; ASTL, high glucose + 50 µg/ml AST; ASTM, high glucose + 100 µg/ml AST; ASTH, high glucose + 200 µg/ml AST.
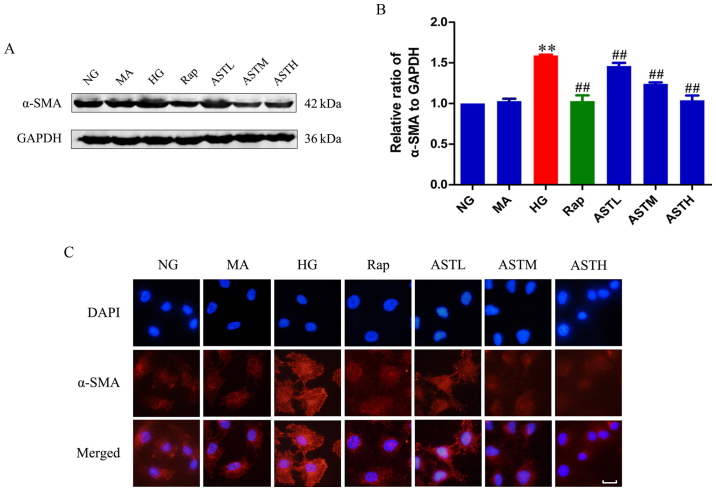
Effects of AST on α-SMA expression
Expression of α-SMA was upregulated in the HG group compared with the NG group (P<0.01; Fig. 2A and B). Additionally, there was no significant difference between the NG and MA groups, indicating no obvious effects generated by the osmotic pressure. In the rapamycin group, the mTOR inhibitor downregulated α-SMA expression compared with HG treatment alone (P<0.01), and administration of AST could also significantly decrease the expression of α-SMA compared with HG alone (P<0.01). The results were validated by immunofluorescence (Fig. 2C).
Figure 2.
Effects of AST on α-SMA expression in HK-2 cells. (A) Western blotting bands of α-SMA. (B) Densitometry analysis of α-SMA. (C) Expression of α-SMA via immunofluorescence. Data are expressed as the mean ± standard error. n=3. Scale bar, 20 µm.**P<0.01 vs. NG; ##P<0.01 vs. HG group. AST, astragaloside IV; NG, normal glucose 5.56 mmol/l; MA, normal glucose 5.56 mmol/l + mannitol 54.44 mmol/l; HG, high glucose 60 mmol/l; Rap, high glucose + 20 nmol/l rapamycin; ASTL, high glucose + 50 µg/ml AST; ASTM, high glucose + 100 µg/ml AST; ASTH, high glucose + 200 µg/ml AST; α-SMA, α-smooth muscle actin.
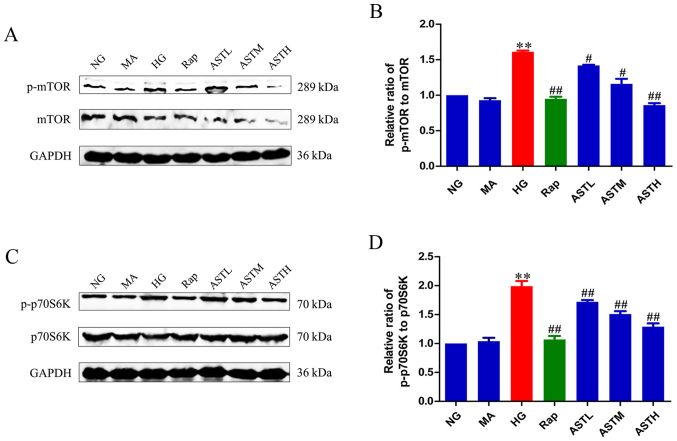
Effects of AST on mTORC1/p70S6K signaling
As demonstrated in Fig. 3A and B, the HG group exhibited markedly higher levels of phosphorylated mTOR compared with the NG group (P<0.01). Additionally, the phosphorylation of p70S6K, a main downstream target of mTOR, was also significantly increased in the HG group compared with in the NG group (P<0.01; Fig. 3C and D). These results revealed that HG activated mTORC1/p70S6K signaling. Furthermore, rapamycin reversed the abnormal activation induced by HG (P<0.01). There was no significant difference between the NG and MA groups, indicating no obvious effects generated by the osmotic pressure alone. Notably, the AST downregulated the phosphorylation of mTOR and its main downstream target, p70S6K, indicating that AST inhibits mTORC1/p70S6K signaling.
Figure 3.
Effects of AST on mTORC1/p70S6K signaling in HK-2 cells. (A) Western blot analysis of p-mTOR. (B) Densitometry analysis of p-mTOR. (C) Western blot analysis of p-p70S6K. (D) Densitometry analysis of p-p70S6K. Data are expressed as mean ± standard error. n=3. **P<0.01 vs. NG group; #P<0.05 vs. HG group; ##P<0.01 vs. HG group. AST, astragaloside IV; NG, normal glucose 5.56 mmol/l; MA, normal glucose 5.56 mmol/l + mannitol 54.44 mmol/l; HG, high glucose 60 mmol/l; Rap, high glucose + 20 nmol/l rapamycin; ASTL, high glucose + 50 µg/ml AST; ASTM, high glucose + 100 µg/ml AST; ASTH, high glucose + 200 µg/ml AST; p- phospho-; mTOR, mammalian target of rapamycin; p70S6K, ribosomal protein S6 kinase β-1.
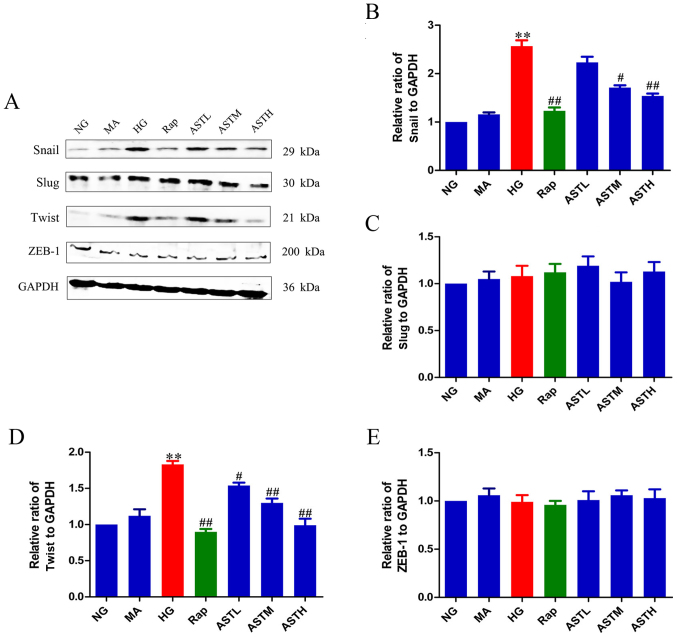
Effects of AST on transcription factors (snail, slug, twist and ZEB-1)
E-cadherin is a marker protein of epithelial layers and its expression is downregulated when EMT occurs (14-16,19). The zinc finger transcription factors (snail, slug, twist and ZEB-1) suppress E-cadherin expression (14-16,19). To verify whether these transcription factors have a role in EMT of HK-2 cells induced by high glucose, the protein expression of snail, slug, twist and ZEB-1 was determined. The expression of snail and twist was significantly enhanced in the HG group compared with in the NG group (P<0.01), while slug and ZEB-1 expression exhibited no significant changes (Fig. 4). Meanwhile, rapamycin treatment could decrease the expression of snail and twist when compared with HG treatment (P<0.01). Interestingly, the AST administrations could also down-regulate the protein levels of snail and twist (P<0.05, P<0.01). In addition, there was no significant difference between the NG and MA groups, indicating no obvious effects generated by the osmotic pressure alone.
Figure 4.
Effects of AST on transcriptional factors, snail, slug, twist and ZEB-1. (A) Western blot analysis of snail, slug, twist and ZEB-1. Relative abundance of (B) snail, (C) slug, (D) twist and (E) ZEB-1. Data are expressed as mean ± standard error. n=3. **P<0.01 vs. NG group; #P<0.05 vs. HG group; ##P<0.01 vs. HG group. AST, astragaloside IV; NG, normal glucose 5.56 mmol/l; MA, normal glucose 5.56 mmol/l + mannitol 54.44 mmol/l; HG, high glucose 60 mmol/l; Rap, high glucose + 20 nmol/l rapamycin; ASTL, high glucose + 50 µg/ml AST; ASTM, high glucose + 100 µg/ml AST; ASTH, high glucose + 200 µg/ml AST; ZEB-1, zinc finger E-box-binding homeobox 1.
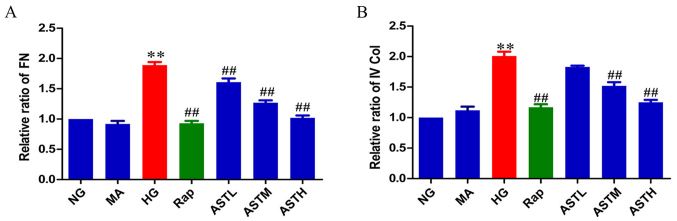
Effects of AST on FN and Col IV
The major extracellular matrix (ECM) proteins FN and Col IV are regarded as markers of fibrogenesis and can cause renal fibrosis when accumulated in DN. As evident in Fig. 5, the protein levels of FN and Col IV were significantly increased in the HG group compared with in the NG group (P<0.01); and no significant differences were observed between the MA and NG groups, indicating no marked effects generated by the osmotic pressure alone. In turn, treatment with rapamycin or AST downregulated the elevated FN and Col IV levels compared with HG treatment (P<0.01).
Figure 5.
Effects of AST on FN and IV Col. (A) Relative abundance of FN. (B) Relative abundance of IV Col. Data are expressed as the mean ± standard error. n=3. **P<0.01 vs. NG group; ##P<0.01 vs. HG group. FN, fibronectin; AST, astragaloside IV; NG, normal glucose 5.56 mmol/l; MA, normal glucose 5.56 mmol/l + mannitol 54.44 mmol/l; HG, high glucose 60 mmol/l; Rap, high glucose + 20 nmol/l rapamycin; ASTL, high glucose + 50 µg/ml AST; ASTM, high glucose + 100 µg/ml AST; ASTH, high glucose + 200 µg/ml AST; IV Col, collagen type IV.
Discussion
The incidence of DM has been increasing worldwide and as a secondary complication, DN is one of the most significant causes of end-stage renal disease (29,30). In China (31) and the United States (32), ~16 and 26% of patients with DN develop end-stage renal disease, respectively; thus, effective and safe treatment strategies to delay the progression of DN are urgently required in the clinic (21). However, little progress has been made in the treatment of patients with DN (33). Although certain novel drugs, including dipeptidyl peptidase 4 inhibitors (34-36), sodium glucose cotransporter 2 inhibitors (37,38) and glucagon-like peptide 1 agonists (39), can help patients presenting with early-stage DN by tightly controlling blood glucose level, it remains largely unknown whether these drugs can ameliorate EMT of renal tubular cells, which also occurs in DN.
Astragalus membranaceus, a traditional Chinese herbal medicine, is widely used as a remedy in the treatment of a variety of clinical diseases, including seasonal allergic rhinitis (40), ischemic heart disease (41), leucopenia (42) and DN (43). AST is one of the main active ingredients of Astragalus membranaceus, the potential pharmaceutical properties of which may include anti-inflammatory (25), anti-oxidative injury (44), anti-cancer (28), anti-hepatitis (27), anti-chronic heart failure (26) and anti-diabetes effects (24,45). The current study aimed to determine whether AST altered EMT in renal tubular cells and to verify the potential mechanisms involved. To the best of our knowledge, the current study is the first to explore the effect and mechanism of AST on the EMT of renal tubular epithelial cells and whether the mTORC1/p70S6K signaling pathway in involved in this effect.
EMT is a physiological process required for wound healing, tissue remodeling and embryogenesis (19); however, EMT is also implicated in pathological processes of various diseases (13,46). For example, during DN, renal tubular epithelial cells undergo a trans-differentiation process and become myofibroblasts, which are the primary source of ECM in renal cells. Major ECM proteins, including FN and Col IV, are often regarded as markers of fibrogenesis (47-49), and their accumulation in patients with DN can lead to renal fibrosis (11,50).
In the present study, the detection of EMT marker proteins demonstrated that high glucose significantly downregulated E-cadherin expression and upregulated the generation of α-SMA. Furthermore, levels of FN and Col IV were increased by high glucose. In turn, treatment with AST could ameliorate the changes stimulated by high glucose. Previous studies have indicated that the mTORC1/p70S6K pathway has an important role in DN, with blockade of this pathway reported to slow DN development (19,21).
It was previously reported that quercetin effectively ameliorated the high glucose-induced EMT of HK-2 and NRK-52E cells and inhibited the activation of mTORC1/p70S6K (19). In vivo, diabetic rats exhibited a significant decline in renal function and severe renal fibrosis at 14 weeks after STZ injection, and mTORC1/p70S6K was activated in the renal cortex of the diabetic rats. Treatment with quercetin alleviated the decline in renal function, and the progression of renal fibrosis and inhibited mTORC1/p70S6K activation in the diabetic renal cortex (19). A HK-2 cell model was validated in the previous study, and based on this, HK-2 cells treated with high glucose was selected as the cell model to verify the effects of AST on EMT in the present study. The results of the current study confirmed previous findings, revealing that the phosphorylation of mTOR and its downstream target, p70S6K, was markedly increased in HK-2 cells induced by high glucose. Treatment with rapamycin inhibited the activation of the mTORC1/p70S6K pathway. Additionally, the association of mTORC1/p70S6K signaling with the EMT of renal tubular epithelial cells was confirmed. Notably, a study by Lu et al (19) indicated that the mTORC1/p70S6K pathway is also involved in the regulation of transcription factor expression, including snail and twist. In the present study, inhibiting mTORC1/p70S6K signaling via rapamycin downregulated the increased protein expression of snail and twist induced by high glucose. These results indicated that activation of mTORC1/p70S6K signaling promoted the progression of EMT by regulating snail and twist expression. Furthermore, AST administration inhibited the mTORC1/p70S6K pathway and reduced the expression of snail and twist; the potential mechanism is illustrated in Fig. 6. However, not studying more markers was a limitation of the present study. The findings of the present study require further validation in the future.
Figure 6.
Mechanism of AST ameliorates high glucose-mediated renal tubular epithelial-mesenchymal transition. AST, astragaloside IV; mTOR, mammalian target of rapamycin; p70S6K, ribosomal protein S6 kinase β-1; P, phospho-; α-SMA, α-smooth muscle actin; FN, fibronectin; IV Col, collagen type IV.
In conclusion, to the best of our knowledge, the present study is the first research to determine the effects of AST on EMT in HK-2 cells via the mTORC1/p70S6K signaling pathway. The present findings provided confirmation that AST reduces EMT in renal tubular cells stimulated by high glucose via mTORC1/p70S6K signaling, and subsequent downregulation of the expression of the transcription factors snail and twist in HK-2 cells. The conclusions will be validated using in vivo models in future studies.
Acknowledgments
Not applicable.
Funding
The present study was supported by the Young Medical Talents of Wuxi (grant no. QNRC020), Young Project of Wuxi Health and Family Planning Research (grant no. Q201706), and Wuxi Science and Technology Development Guidance Plan (Medical and Health Care; grant no. CSZON1744).
Availability of data and materials
The datasets used and/or analyzed during the present study are available from the corresponding author on reasonable request.
Authors’ contributions
DW and ZC conceived and designed the study. DW, XC, YY and CL performed the experiments. DW and XC wrote the paper. YY and CL critically reviewed and edited the manuscript. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Dixit P, Ghaskadbi S, Mohan H, Devasagayam TP. Antioxidant properties of germinated fenugreek seeds. Phytother Res. 2005;19:977–983. doi: 10.1002/ptr.1769. [DOI] [PubMed] [Google Scholar]
- 2.Roberts KT. The potential of fenugreek (Trigonella foenum-graecum) as a functional food and nutraceutical and its effects on glycemia and lipidemia. J Med Food. 2011;14:1485–1489. doi: 10.1089/jmf.2011.0002. [DOI] [PubMed] [Google Scholar]
- 3.Kashihara N, Haruna Y, Kondeti VK, Kanwar YS. Oxidative stress in diabetic nephropathy. Curr Med Chem. 2010;17:4256–4269. doi: 10.2174/092986710793348581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Collins AJ, Foley RN, Herzog C, Chavers B, Gilbertson D, Ishani A, Kasiske B, Liu J, Mau LW, McBean M, et al. US Renal Data System 2010 Annual Data Report. Am J Kidney Dis. 2011;57(Suppl 1):A8, e1–e526. doi: 10.1053/j.ajkd.2010.10.007. [DOI] [PubMed] [Google Scholar]
- 5.Reutens AT, Atkins RC. Epidemiology of diabetic nephropathy. Contrib Nephrol. 2011;170:1–7. doi: 10.1159/000324934. [DOI] [PubMed] [Google Scholar]
- 6.Brosius FC, Khoury CC, Buller CL, Chen S. Abnormalities in signaling pathways in diabetic nephropathy. Expert Rev Endocrinol Metab. 2010;5:51–64. doi: 10.1586/eem.09.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Steffes MW, Osterby R, Chavers B, Mauer SM. Mesangial expansion as a central mechanism for loss of kidney function in diabetic patients. Diabetes. 1989;38:1077–1081. doi: 10.2337/diab.38.9.1077. [DOI] [PubMed] [Google Scholar]
- 8.Ziyadeh FN. The extracellular matrix in diabetic nephropathy. Am J Kidney Dis. 1993;22:736–744. doi: 10.1016/S0272-6386(12)80440-9. [DOI] [PubMed] [Google Scholar]
- 9.Valcourt U, Kowanetz M, Niimi H, Heldin CH, Moustakas A. TGF-beta and the Smad signaling pathway support tran-scriptomic reprogramming during epithelial-mesenchymal cell transition. Mol Biol Cell. 2005;16:1987–2002. doi: 10.1091/mbc.e04-08-0658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Badid C, Desmouliere A, Babici D, Hadj-Aissa A, McGregor B, Lefrancois N, Touraine JL, Laville M. Interstitial expression of alpha-SMA: An early marker of chronic renal allograft dysfunction. Nephrol Dial Transplant. 2002;17:1993–1998. doi: 10.1093/ndt/17.11.1993. [DOI] [PubMed] [Google Scholar]
- 11.Hills CE, Squires PE. The role of TGF-β and epithelial-to mesenchymal transition in diabetic nephropathy. Cytokine Growth Factor Rev. 2011;22:131–139. doi: 10.1016/j.cytogfr.2011.06.002. [DOI] [PubMed] [Google Scholar]
- 12.Liu Y. New insights into epithelial-mesenchymal transition in kidney fibrosis. J Am Soc Nephrol. 2010;21:212–222. doi: 10.1681/ASN.2008121226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thiery JP, Acloque H, Huang RY, Nieto MA. Epithelial-mesenchymal transitions in development and disease. Cell. 2009;139:871–890. doi: 10.1016/j.cell.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 14.Nieto MA. The snail superfamily of zinc-finger transcription factors. Nat Rev Mol Cell Biol. 2002;3:155–166. doi: 10.1038/nrm757. [DOI] [PubMed] [Google Scholar]
- 15.Peinado H, Olmeda D, Cano A. Snail, Zeb and bHLH factors in tumour progression: An alliance against the epithelial phenotype. Nat Rev Cancer. 2007;7:415–428. doi: 10.1038/nrc2131. [DOI] [PubMed] [Google Scholar]
- 16.Thiery JP, Sleeman JP. Complex networks orchestrate epithelial-mesenchymal transitions. Nat Rev Mol Cell Biol. 2006;7:131–142. doi: 10.1038/nrm1835. [DOI] [PubMed] [Google Scholar]
- 17.Cano A, Pérez-Moreno MA, Rodrigo I, Locascio A, Blanco MJ, del Barrio MG, Portillo F, Nieto MA. The transcription factor snail controls epithelial-mesenchymal transitions by repressing E-cadherin expression. Nat Cell Biol. 2000;2:76–83. doi: 10.1038/35000025. [DOI] [PubMed] [Google Scholar]
- 18.Hajra KM, Chen DY, Fearon ER. The SLUG zinc-finger protein represses E-cadherin in breast cancer. Cancer Res. 2002;62:1613–1618. [PubMed] [Google Scholar]
- 19.Lu Q, Ji XJ, Zhou YX, Yao XQ, Liu YQ, Zhang F, Yin XX. Quercetin inhibits the mTORC1/p70S6K signaling-mediated renal tubular epithelial-mesenchymal transition and renal fibrosis in diabetic nephropathy. Pharmacol Res. 2015;99:237–247. doi: 10.1016/j.phrs.2015.06.006. [DOI] [PubMed] [Google Scholar]
- 20.Ma XM, Blenis J. Molecular mechanisms of mTOR-mediated translational control. Nat Rev Mol Cell Biol. 2009;10:307–318. doi: 10.1038/nrm2672. [DOI] [PubMed] [Google Scholar]
- 21.Wu W, Hu W, Han WB, Liu YL, Tu Y, Yang HM, Fang QJ, Zhou MY, Wan ZY, Tang RM, et al. Inhibition of Akt/mTOR/p70S6K Signaling Activity With Huangkui Capsule Alleviates the Early Glomerular Pathological Changes in Diabetic Nephropathy. Front Pharmacol. 2018;9:443. doi: 10.3389/fphar.2018.00443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li M, Qu YZ, Zhao ZW, Wu SX, Liu YY, Wei XY, Gao L, Gao GD. Astragaloside IV protects against focal cerebral ischemia/reperfusion injury correlating to suppression of neutrophils adhesion-related molecules. Neurochem Int. 2012;60:458–465. doi: 10.1016/j.neuint.2012.01.026. [DOI] [PubMed] [Google Scholar]
- 23.Luo Y, Qin Z, Hong Z, Zhang X, Ding D, Fu JH, Zhang WD, Chen J. Astragaloside IV protects against ischemic brain injury in a murine model of transient focal ischemia. Neurosci Lett. 2004;363:218–223. doi: 10.1016/j.neulet.2004.03.036. [DOI] [PubMed] [Google Scholar]
- 24.Du Q, Zhang S, Li A, Mohammad IS, Liu B, Li Y. Astragaloside IV: Astragaloside IV Inhibits Adipose Lipolysis and Reduces Hepatic Glucose Production via Akt Dependent PDE3B Expression in HFD-Fed Mice. Front Physiol. 2018;9:15. doi: 10.3389/fphys.2018.00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li C, Yang F, Liu F, Li D, Yang T. NRF2/HO-1 activation via ERK pathway involved in the anti-neuroinflammatory effect of Astragaloside IV in LPS induced microglial cells. Neurosci Lett. 2018;666:104–110. doi: 10.1016/j.neulet.2017.12.039. [DOI] [PubMed] [Google Scholar]
- 26.Tang B, Zhang JG, Tan HY, Wei XQ. Astragaloside IV inhibits ventricular remodeling and improves fatty acid utili-zation in rats with chronic heart failure. Biosci Rep. 2018;38:38. doi: 10.1042/BSR20171036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang S, Li J, Huang H, Gao W, Zhuang C, Li B, Zhou P, Kong D. Anti-hepatitis B virus activities of astragaloside IV isolated from radix Astragali. Biol Pharm Bull. 2009;32:132–135. doi: 10.1248/bpb.32.132. [DOI] [PubMed] [Google Scholar]
- 28.Zhu J, Wen K. Astragaloside IV inhibits TGF-β1-induced epithelial-mesenchymal transition through inhibition of the PI3K/Akt/NF-κB pathway in gastric cancer cells. Phytother Res. 2018;32:1289–1296. doi: 10.1002/ptr.6057. [DOI] [PubMed] [Google Scholar]
- 29.Brownlee M. The pathobiology of diabetic complications: A unifying mechanism. Diabetes. 2005;54:1615–1625. doi: 10.2337/diabetes.54.6.1615. [DOI] [PubMed] [Google Scholar]
- 30.Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010–2030. Diabetes Res Clin Pract. 2010;87:4–14. doi: 10.1016/j.diabres.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 31.Liu ZH. Nephrology in china. Nat Rev Nephrol. 2013;9:523–528. doi: 10.1038/nrneph.2013.146. [DOI] [PubMed] [Google Scholar]
- 32.Afkarian M, Zelnick LR, Hall YN, Heagerty PJ, Tuttle K, Weiss NS, de Boer IH. Clinical Manifestations of Kidney Disease Among US Adults With Diabetes, 1988–2014. JAMA. 2016;316:602–610. doi: 10.1001/jama.2016.10924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.de Boer IH. A new chapter for diabetic kidney disease. N Engl J Med. 2017;377:885–887. doi: 10.1056/NEJMe1708949. [DOI] [PubMed] [Google Scholar]
- 34.Penno G, Garofolo M, Del Prato S. Dipeptidyl peptidase-4 inhibition in chronic kidney disease and potential for protection against diabetes-related renal injury. Nutr Metab Cardiovasc Dis. 2016;26:361–373. doi: 10.1016/j.numecd.2016.01.001. [DOI] [PubMed] [Google Scholar]
- 35.Wang D, Zhang G, Chen X, Wei T, Liu C, Chen C, Gong Y, Wei Q. Sitagliptin ameliorates diabetic nephropathy by blocking TGF-β1/Smad signaling pathway. Int J Mol Med. 2018;41:2784–2792. doi: 10.3892/ijmm.2018.3504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhang GY, Wang DD, Cao Z, Wei T, Liu CX, Wei QL. Sitagliptin ameliorates high glucose-induced cell proliferation and expression of the extracellular matrix in glomerular mesangial cells. Exp Ther Med. 2017;14:3862–3867. doi: 10.3892/etm.2017.5002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wanner C, Inzucchi SE, Lachin JM, Fitchett D, von Eynatten M, Mattheus M, Johansen OE, Woerle HJ, Broedl UC, Zinman B. Empagliflozin and progression of kidney disease in type 2 diabetes. N Engl J Med. 2016;375:323–334. doi: 10.1056/NEJMoa1515920. [DOI] [PubMed] [Google Scholar]
- 38.Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, Mattheus M, Devins T, Johansen OE, Woerle HJ, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373:2117–2128. doi: 10.1056/NEJMoa1504720. [DOI] [PubMed] [Google Scholar]
- 39.Muskiet MHA, Tonneijck L, Smits MM, van Baar MJB, Kramer MHH, Hoorn EJ, Joles JA, van Raalte DH. GLP-1 and the kidney: From physiology to pharmacology and outcomes in diabetes. Nat Rev Nephrol. 2017;13:605–628. doi: 10.1038/nrneph.2017.123. [DOI] [PubMed] [Google Scholar]
- 40.Matkovic Z, Zivkovic V, Korica M, Plavec D, Pecanic S, Tudoric N. Efficacy and safety of Astragalus membranaceus in the treatment of patients with seasonal allergic rhinitis. Phytother Res. 2010;24:175–181. doi: 10.1002/ptr.2877. [DOI] [PubMed] [Google Scholar]
- 41.Li SQ, Yuan RX, Gao H. Clinical observation on the treatment of ischemic heart disease with Astragalus membranaceus. Zhongguo Zhong Xi Yi Jie He Za Zhi. 1995;15:77–80. In Chinese. [PubMed] [Google Scholar]
- 42.Zhang C, Zhu C, Ling Y, Zhou X, Dong C, Luo J, Liu Y. The clinical value of Huangqi injection in the treatment of leucopenia: A meta-analysis of clinical controlled trials. PLoS One. 2013;8:e83123. doi: 10.1371/journal.pone.0083123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Li M, Wang W, Xue J, Gu Y, Lin S. Meta-analysis of the clinical value of Astragalus membranaceus in diabetic nephropathy. J Ethnopharmacol. 2011;133:412–419. doi: 10.1016/j.jep.2010.10.012. [DOI] [PubMed] [Google Scholar]
- 44.Qiao Y, Fan CL, Tang MK. Astragaloside IV protects rat retinal capillary endothelial cells against high glucose-induced oxidative injury. Drug Des Devel Ther. 2017;11:3567–3577. doi: 10.2147/DDDT.S152489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chen X, Wang DD, Wei T, He SM, Zhang GY, Wei QL. Effects of astragalosides from Radix Astragali on high glucose-induced proliferation and extracellular matrix accumulation in glomerular mesangial cells. Exp Ther Med. 2016;11:2561–2566. doi: 10.3892/etm.2016.3194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nieto MA. Epithelial-Mesenchymal Transitions in development and disease: Old views and new perspectives. Int J Dev Biol. 2009;53:1541–1547. doi: 10.1387/ijdb.072410mn. [DOI] [PubMed] [Google Scholar]
- 47.Gonzalez J, Klein J, Chauhan SD, Neau E, Calise D, Nevoit C, Chaaya R, Miravete M, Delage C, Bascands JL, et al. Delayed treatment with plasminogen activator inhibitor-1 decoys reduces tubulointerstitial fibrosis. Exp Biol Med (Maywood) 2009;234:1511–1518. doi: 10.3181/0903-RM-105. [DOI] [PubMed] [Google Scholar]
- 48.Wang JY, Yin XX, Wu YM, Tang DQ, Gao YY, Wan MR, Hou XY, Zhang B. Ginkgo biloba extract suppresses hypertrophy and extracellular matrix accumulation in rat mesangial cells. Acta Pharmacol Sin. 2006;27:1222–1230. doi: 10.1111/j.1745-7254.2006.00360.x. [DOI] [PubMed] [Google Scholar]
- 49.Xu W, Shao X, Tian L, Gu L, Zhang M, Wang Q, Wu B, Wang L, Yao J, Xu X, et al. Astragaloside IV ameliorates renal fibrosis via the inhibition of mitogen-activated protein kinases and antiapoptosis in vivo and in vitro. J Pharmacol Exp Ther. 2014;350:552–562. doi: 10.1124/jpet.114.214205. [DOI] [PubMed] [Google Scholar]
- 50.Li Y, Kang YS, Dai C, Kiss LP, Wen X, Liu Y. Epithelial-to-mesenchymal transition is a potential pathway leading to podocyte dysfunction and proteinuria. Am J Pathol. 2008;172:299–308. doi: 10.2353/ajpath.2008.070057. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the present study are available from the corresponding author on reasonable request.