Abstract
Background
Injuries result in substantial number of deaths among children globally. The burden across many settings is largely unknown. We estimated global and regional child deaths due to injuries from publicly available evidence.
Methods
We searched for community-based studies and nationally representative data reporting on child injury deaths published after year 1990 from CINAHL, EMBASE, IndMed, LILACS, Global Health, MEDLINE, SCOPUS, and Web of Science. Specific and all-cause mortality due to injuries were extracted for three age groups (0-11 months, 1-4 years, and 0-4 years). We conducted random-effects meta-analysis on extracted crude estimates, and developed a meta-regression model to determine the number of deaths due to injuries among children aged 0-4 years globally and across the World Health Organization (WHO) regions.
Results
Twenty-nine studies from 16 countries met the selection criteria. A total of 230 data-points on 15 causes of injury deaths were retrieved from all studies. Eighteen studies were rated as high quality, although heterogeneity was high (I2 = 99.7%, P < 0.001) reflecting variable data sources and study designs. For children aged 0-11 months, the pooled crude injury mortality rate was 29.6 (95% confidence interval (CI) = 21.1-38.1) per 100 000 child population, with asphyxiation being the leading cause of death (neonatal) at 189.1 (95% CI = 142.7-235.4) per 100 000 followed by suffocation (post-neonatal) at 18.7 (95% CI = 11.8-25.7) per 100 000. Among children aged 1-4 years, the pooled crude injury mortality rate was 32.7 (95% CI = 27.3-38.1) per 100 000, with traffic injuries and drowning the leading causes of deaths at 10.8 (95% CI = 8.9-12.8) and 8.8 (95% CI = 7.5-10.2) per 100 000, respectively. Among children under five years, the pooled injury mortality rate was 37.7 (95% CI = 32.7-42.7) per 100 000, with traffic injuries and drowning also the leading causes of deaths at 10.3 (95% CI = 8.8-11.8) and 8.9 (95% CI = 7.8-9.9) per 100 000 respectively. When crude mortality changes over age, WHO regions, and study period were accounted for in our model, we estimated that in 2015 there were 522 167 (95% CI = 395 823-648 630) deaths among children aged 0-4 years, with South East Asia (SEARO) recording the highest number of deaths at 195 084 (95% CI = 159476-230502), closely followed by the Africa region (AFRO) with 176523 (95% CI = 115 040-237 831) deaths. Globally, traffic injuries and drowning were the leading causes of under-five injury fatalities in 2015 with 142 661 (22.0/100 000) and 123 270 (19.0/100 000) child deaths, respectively. The exception being burns in AFRO with 57 784 deaths (38.6/100 000).
Conclusions
Varying study designs, case definitions, and particularly limited country representation from Africa and South-East Asia (where we reported higher estimates), imply a need for more studies for better population representative estimates. This study may have however provided improved understanding on child injury death profiles needed to guide further research, policy reforms and relevant strategies globally.
Several children die each year from injuries, assault or violence, with many suffering from consequences of non-fatal injuries [1]. In 2015, there were 7.3 million deaths among children and adolescents [2], with low- and middle-income countries (LMICs) accounting for 80%-95% of all fatalities in this age group [1,3]. Although, the global burden of disease (GBD) collaborators reported that global child mortality decreased by about 50% between 1990 and 2015 [2], these were mainly due to a reduction in infectious causes. Injuries are known to contribute less to global childhood mortality in comparison to known leading causes like pneumonia, diarrhea, preterm births, neonatal infections, or malnutrition. However, a steady decline in infectious causes with limited knowledge on the burden of child injuries across world regions implies injuries may constitute a hidden burden [4,5]. According to the World Health Organization (WHO), between 2000 and 2010, percentage distribution of mortality from injuries among children under five years increased across all income groups, suggesting a need to address this more keenly globally [1].
One basic challenge in child injuries’ research and surveillance relates to the application of appropriate case definitions [6,7]. Largely, case definitions, coding, and overall design of child injury studies vary across world regions [3,6]. Injuries are mainly classified by intent, ie. those that were not predetermined (unintentional), or those that were planned (intentional) [8]. The International Classification of Disease 10 (ICD-10) [9], and the International Classification of External Causes of Injuries (ICECI) have provided standard codes and definitions to guide researchers in describing and identifying injury types [10]. In several surveys however, researchers appear to have been limited in appropriately classifying and reporting injuries, with this resulting misrepresentation of cases and/or inconclusive outcomes [11-13].
Moreover, despite various sources available for conducting national and subnational injuries surveillance, including death certificates, autopsy reports, hospital reports, insurance records, and police records [12,14], data on unintentional injuries are still collated from very limited sources – mainly manually from hospital records across many LMICs [15]. Due to unclear reporting procedures, limited technical capacity for electronic collation, and failure to account for deaths outside hospital settings, data are almost always incomplete and estimates are largely not representative [8,16]. With prevailing sparse data across many countries, it remains difficult to convince policy makers and relevant stakeholders on the magnitude of child injuries [1,3]. There are several doubts and persisting uncertainties around the global burden of child deaths from injuries, nonetheless newer studies are emerging in some settings [17]. Thus, retrieving the available data across world regions through a comprehensive and systematic search is imperative to guide better understanding of the burden, and possibly aid relevant policy decisions, actions and improved research in settings with limited data. We sought to provide estimates of the global and regional mortality and absolute number of deaths from injuries among children under five years from publicly available evidence.
METHODS
Search strategy
A systematic literature search of CINAHL, EMBASE, IndMed, LILACS, Global Health, MEDLINE, SCOPUS and Web of Science was conducted for studies reporting mortalities from injuries among children under the age of five years across world regions. Search dates were set from January 1990 to August 2018. A further search of OpenGrey, BIOSIS and relevant children international organizations was conducted for grey literature and conference abstracts. Reference lists of initially identified studies were hand-searched for more studies. Full search strategy and search terms are presented in Table S1 in Online Supplementary Document(Online Supplementary Document).
Selection criteria
Articles were selected if they were i) community-based studies or nationally representative data on mortality from child injuries, ii) conducted among children under the age of five years (or where this could possibly be extracted if this age group was included in a broader age range), and iii) published from the year 1990 onwards. For the definition of injury, we considered articles that described injuries as physical hurt or damage to the body resulting from intentional of unintentional causes including (but not limited to) traffic collisions, drowning, poisoning, suffocation, falls, burns, violence, assaults or homicide [9]. We excluded studies if they were i) conducted among children above five years only, ii) conducted on specific groups of children with underlying conditions that could make children more prone to injuries, iii) reporting on non-fatal outcomes from injuries, iv) published before the year 1990, and/or v) reviews, commentaries, editorials or viewpoints.
Data extraction
Two reviewers (DA and KB) independently screened studies against the selection criteria and extracted data from all selected studies. Any disagreements over article inclusion, exclusion or data extraction between the two reviewers were resolved through a final assessment by a third reviewer (IR). As we already employed a two-stage search and extraction process based on a combination of independent review and reassessment, we did not calculate Kappa statistics to determine agreement between the reviewers. We extracted data and relevant information systematically from each study. This included study location, period, design, location, WHO region, income category, coding of injury types, and corresponding deaths, population denominators, and injury mortality rates, respectively for ages 0-11 months, 1-4 years and 0-4 years. All extracted data were sorted in Excel Worksheet 2013 (Microsoft Inc, Redmond, WA, USA).
Quality criteria
We assessed quality of studies using a modified approach of the Centre for Reviews and Dissemination guidance for undertaking reviews in health care [18]. The assessment was based on four criteria: study design (causes of injuries reported with appropriate coding), sampling (representative of national population), statistical analysis (appropriate for child injury mortality estimation), and study limitation (description of potential sources of bias). See Table 1 for grading details.
Table 1.
Quality assessment criteria
| Criteria | Assessment | Score |
|---|---|---|
| Study design
(At least 10 injury types reported and based on standard
definitions or ICD coding?) |
Yes |
1 |
| No |
0 |
|
| Sampling (was
it representative of target sub-national population or national
population?) |
Nationally representative |
2 |
| Sub-nationally representative |
1 |
|
| No |
0 |
|
| Statistical
analysis (was it clear and appropriate for outcome
measure?) |
Yes |
1 |
| Ambiguous |
0 |
|
| Study
limitations (were potential sources of bias described) |
Yes |
1 |
| No |
0 |
|
| Final
assessment: High (4-5), Moderate (2-3), and low (0-1) | ||
Data analysis
For the three age groups, data were primarily sorted according to WHO regions: Africa (AFRO), Eastern Mediterranean (EMRO), Europe (EURO), Americas (PAHO), South East Asia (SEARO) and Western Pacific (WPRO). For the mechanism of injuries, data were sorted according to estimates for overall injuries, and individual injury types from each study. Mortality rates were estimated as number of child injury deaths per 100 000 child population. Standard errors were estimated from the crude mortality rates and child population assuming a Poisson distribution. Using a random effects meta-analysis (Der-Simonian and Laird method) [19], crude meta-estimates and confidence intervals were pooled from individual crude mortality rates and reported by injury-type and WHO regions. I-squared (I2) statistics and subgroup analysis were conducted to assess heterogeneity between studies. From reported crude mortality rates, we developed a meta-regression model to account for the absolute number of injury deaths among children under five years. In this model, we created six dummy variables accounting for each of the six WHO regions mainly from data that reported estimates for all injuries. We ran this regression model separately for each of the three age groups, while accounting for the study period and WHO regions. We tested the model using different WHO dummy region variables and chose the one that was most predictive (ie. AFRO, in which the proportion of variance (adjusted R2) of child injury mortality explained by WHO regions and study period was the greatest) as the control against which other variables (regions) were compared. Using a standardized ratio from the pooled crude mortality rates for seven causes of injuries that returned highest number of data-points (ie. traffic injuries, drowning, falls, poisoning, suffocation, burns, and assaults, with the remaining injury types grouped as “others”), we determined the number of deaths for each cause of injury by WHO regions. We summed these regional estimates to determine the absolute number of deaths for all injuries and specific causes of injuries among children aged 0-4 years worldwide. All statistical analyses were conducted on Stata 14 (Stata Corp LP, College Station, TX, USA).
RESULTS
Search results
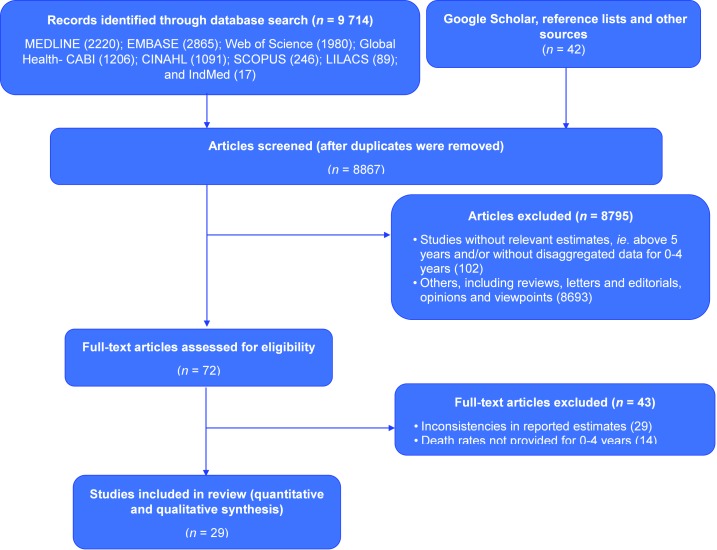
The literature search returned 9714 records from the electronic databases and 42 records from other sources. Following the removal of duplicates, screening of titles and abstracts, and the application of the selection criteria, 29 studies were selected. The process of selection of studies is described in Figure 1.
Figure 1.
Flowchart of search strategy and study selection.
Main study characteristics
The 29 studies were selected across 16 countries (Figure 2), with a total of 230 data points on different injury types among children aged 0-4 years (Table 2). Most data were from WPRO with 105 data points and China accounting for 73.3% of this (Figure 2). PAHO had 54 data-points, SEARO 24, AFRO 20, EURO 19 and EMRO 8. Traffic injuries and drowning had most data points (n = 31 each), followed by falls (n = 27), poisoning (n = 22), suffocation (n = 21), burns (n = 15) and assault (n = 15) (Table 2). Most studies were population-based injury surveillance, with study period ranging from 1990 to 2017. Heterogeneity was high across studies (I2 = 99.7%, P < 0.001), mainly due to varying case definitions, coding and overall study designs. Eighteen studies were rated as high quality with the remaining 11 rated as moderate quality (Table 3 and Table S2 in Online Supplementary Document(Online Supplementary Document)). All low-quality studies were not included in the review (see Table S3 in Online Supplementary Document(Online Supplementary Document) for details of low-quality studies excluded).
Figure 2.
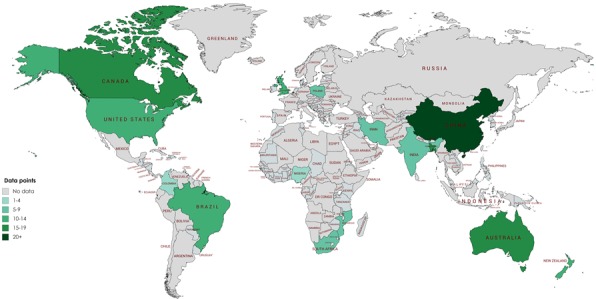
Sources of data on child injury deaths by country.
Table 2.
Data distribution by injury type and WHO region
| Injury type | AFRO | EMRO | EURO | PAHO | SEARO | WPRO | Total |
|---|---|---|---|---|---|---|---|
|
All Injuries
(V01-X59.9, Y85-Y86) |
4 |
1 |
2 |
5 |
1 |
14 |
27 |
|
Traffic
Injuries (V01-V99) |
3 |
1 |
2 |
7 |
3 |
15 |
31 |
|
Drowning
(W65-W74.9, V90-V90.0, and V92-V92.9) |
2 |
1 |
2 |
6 |
3 |
17 |
31 |
|
Burns
(X00-X19.9) |
3 |
1 |
1 |
6 |
2 |
2 |
15 |
|
Suffocation
(W75-W84) |
1 |
0 |
1 |
4 |
2 |
13 |
21 |
|
Falls
(W00-W19.9) |
3 |
1 |
2 |
4 |
3 |
14 |
27 |
|
Poisoning
(X40-X49.9) |
1 |
1 |
2 |
2 |
1 |
15 |
22 |
|
Firearm
(W32-W34.9) |
0 |
0 |
1 |
2 |
0 |
2 |
5 |
|
Cutting/Piercing (X71-X83) |
0 |
0 |
1 |
2 |
1 |
2 |
6 |
|
Venomous
Animals/Plants (X20-X29) |
0 |
1 |
0 |
0 |
3 |
0 |
4 |
|
Electrocution
(W85-W99) |
1 |
0 |
0 |
1 |
1 |
0 |
3 |
|
Asphyxiation
(T71.1) |
0 |
0 |
0 |
1 |
1 |
1 |
3 |
|
Medical
Procedures (Y84.8) |
1 |
1 |
1 |
0 |
0 |
1 |
4 |
|
Unspecified
unintentional injuries |
0 |
0 |
2 |
3 |
2 |
2 |
9 |
|
Assault/Homicide (X85-Y09) |
1 |
0 |
1 |
7 |
1 |
5 |
15 |
|
Intent
Unknown |
0 |
0 |
1 |
4 |
0 |
2 |
7 |
| Total | 20 | 8 | 19 | 54 | 24 | 105 | 230 |
AFRO – African region, EMRO – Eastern Mediterranean region, EURO – European region, PAHO – Pan-American Health Organization or American region, SEARO – South East Asia region, WPRO – Western Pacific region
Table 3.
Characteristics of selected studies
| First author | Study period | Country | Income category | Study design | Quality grading |
|---|---|---|---|---|---|
|
AFRO | |||||
|
Nizamo [20] |
2000 |
Mozambique |
Low |
Population based. Registered
deaths |
Moderate |
|
Abdur-Rahman
[21] |
2015 |
Nigeria |
Lower middle |
Cross-sectional
Verbal
autopsy results |
Moderate |
|
Norman
Pacella [22] |
2000 |
South Africa |
Upper middle |
Population based. Death
certificates |
Moderate |
|
Sacarlal
[23] |
2006 |
Mozambique |
Low |
Cross-sectional survey. Verbal
autopsy results |
Moderate |
|
EMRO | |||||
|
Naghavi
[24] |
2005 |
Iran |
Upper middle |
Population based. Death registration
data |
Moderate |
|
EURO | |||||
|
DiGuiseppi
[25] |
1992 |
England & Wales |
High |
Population based. WHO European
detailed mortality database |
High |
|
Grajda [26] |
1999-2012 |
Poland |
High |
Population based. WHO European
detailed mortality database |
High |
|
PAHO | |||||
|
Celis [27] |
1997 |
Mexico |
Upper middle |
Population based. Death
certificates |
High |
|
D'Agostini [28] |
1996-2002 |
Brazil |
Upper middle |
Ecological model. Mortality data
from mortality information system |
High |
|
Espitia-Hardeman [29] |
2007 |
Colombia |
Upper middle |
Population based. Injury
surveillance system |
High |
|
Fingerhut
[30] |
1993 |
USA |
High |
Population based. Injury
surveillance system |
High |
|
Gawryszewski
[31] |
2003 |
Brazil |
Upper middle |
Population based. Mortality data
from mortality information system |
High |
|
Aldana [32] |
2009 |
Colombia |
Upper middle |
Population based. Death
certificates |
High |
|
Amram [33] |
2009 |
Canada |
High |
Population based. Injury
surveillance system |
High |
|
Clemens
[34] |
2012 |
Canada |
High |
Population based. Injury
surveillance system |
High |
|
SEARO | |||||
|
Rahman [35] |
2005 |
Bangladesh |
Lower middle |
Population based. Verbal autopsy
results |
High |
|
Jagnoor
[36] |
2003 |
India |
Lower middle |
Cross-sectional. Verbal autopsy
results |
High |
|
Alonge [37] |
2017 |
Bangladesh |
Lower middle |
Population based. Injury
surveillance system |
High |
|
WPRO | |||||
|
Huo [38] |
2004-2008 |
China |
Upper middle |
Population based. Annual reports of
mortality data for maternal and child health |
High |
|
Langley
[39] |
1993 |
New Zealand |
High |
Population based. Injury
surveillance system |
High |
|
Lili [40] |
2009-2014 |
China |
Upper middle |
Population based. Disease
surveillance information systems. |
High |
|
Scott [41] |
1994 |
Australia |
High |
Population based. Child deaths
registry |
High |
|
Wallis [42] |
2008 |
Australia |
High |
Population based. Child deaths
registry |
High |
|
Wang [43] |
2000-2008 |
China |
Upper middle |
Population based. Child deaths
obtained from Shenzhen Women and Child Health Surveillance
System for 2004-2008 |
Moderate |
|
Yang [44] |
2001 |
China |
Upper middle |
Population based. Disease
surveillance information systems. |
Moderate |
|
Zhang [45] |
1997-2012 |
China |
Upper middle |
Population based. Child deaths
registry |
Moderate |
|
Zhang [46] |
2004-2010 |
China |
Upper middle |
Population based. Child deaths
registry |
Moderate |
|
Wang [47] |
2004-2008 |
China |
Upper middle |
Population based. Child deaths
registry |
Moderate |
| Hayman [48] | 2002-2009 | New Zealand | High | Population based. Disease surveillance information systems. | Moderate |
AFRO – African region, EMRO – Eastern Mediterranean region, EURO – European region, PAHO – Pan-American Health Organization or American region, SEARO – South East Asia region, WPRO – Western Pacific region
Pooled crude child injury mortality meta-estimates
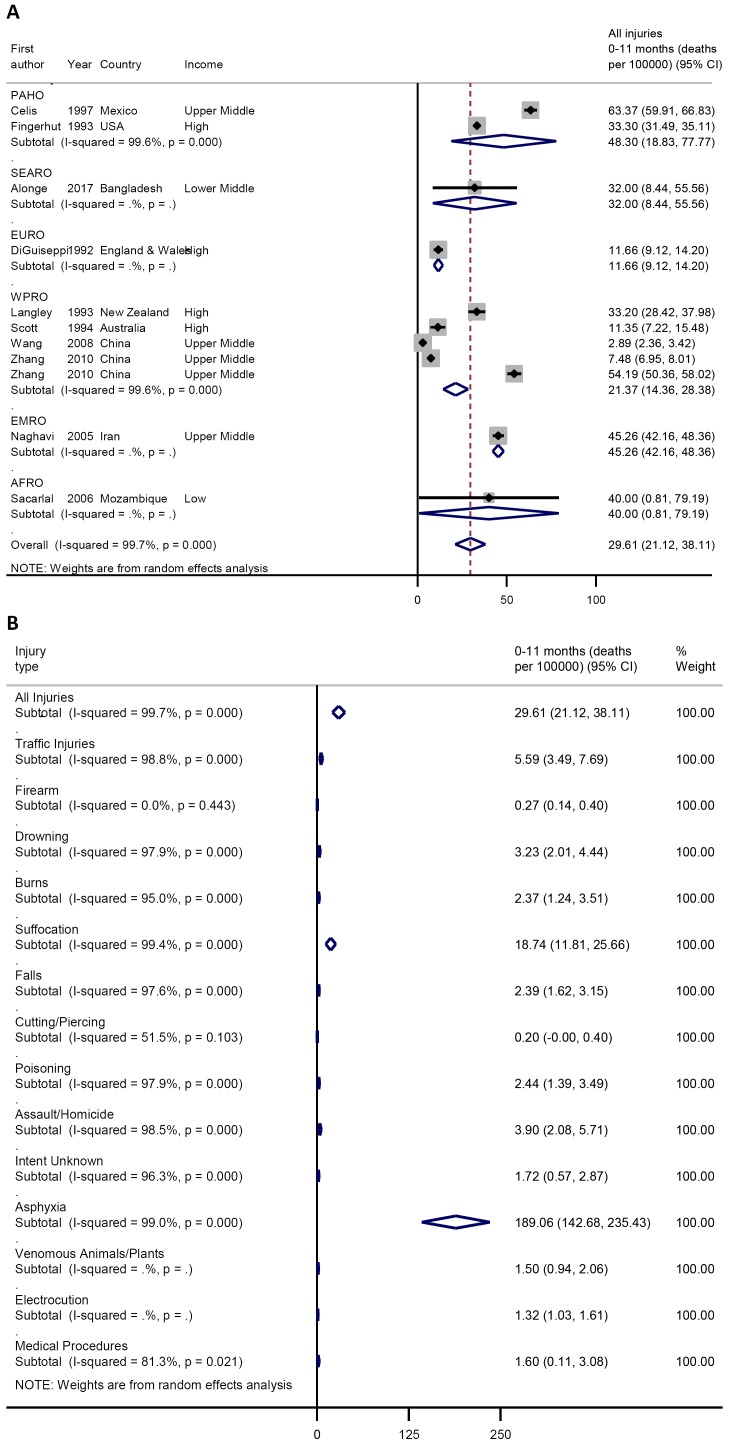
For children aged 0-11 months, the pooled crude injury mortality rate was 29.6 (21.1-38.1) per 100 000 child population (Figure 3, plate A), with asphyxiation being the leading cause of death (in the neonatal period) at 189.1 (95% confidence interval (CI) = 142.7-235.4) per 100 000 followed by suffocation (in the post-neonatal period) at 18.7 (95% CI = 11.8-25.7) per 100 000. Other notable causes of injury deaths in this age group include traffic injuries 5.6 (95% CI = 3.5-7.7) per 100 000, assault 3.6 (95% CI = 2.1-5.7) per 100 000, drowning 3.2 (95% CI = 2.0-4.4) per 100 000, and burns 2.4 (95% CI = 1.4-3.5) per 100 000 (Figure 3, plate B).
Figure 3.
A. Pooled crude child injury mortality rate by WHO region, 0-11 months. B. Pooled crude child injury mortality rate by type of injury, 0-11 months.
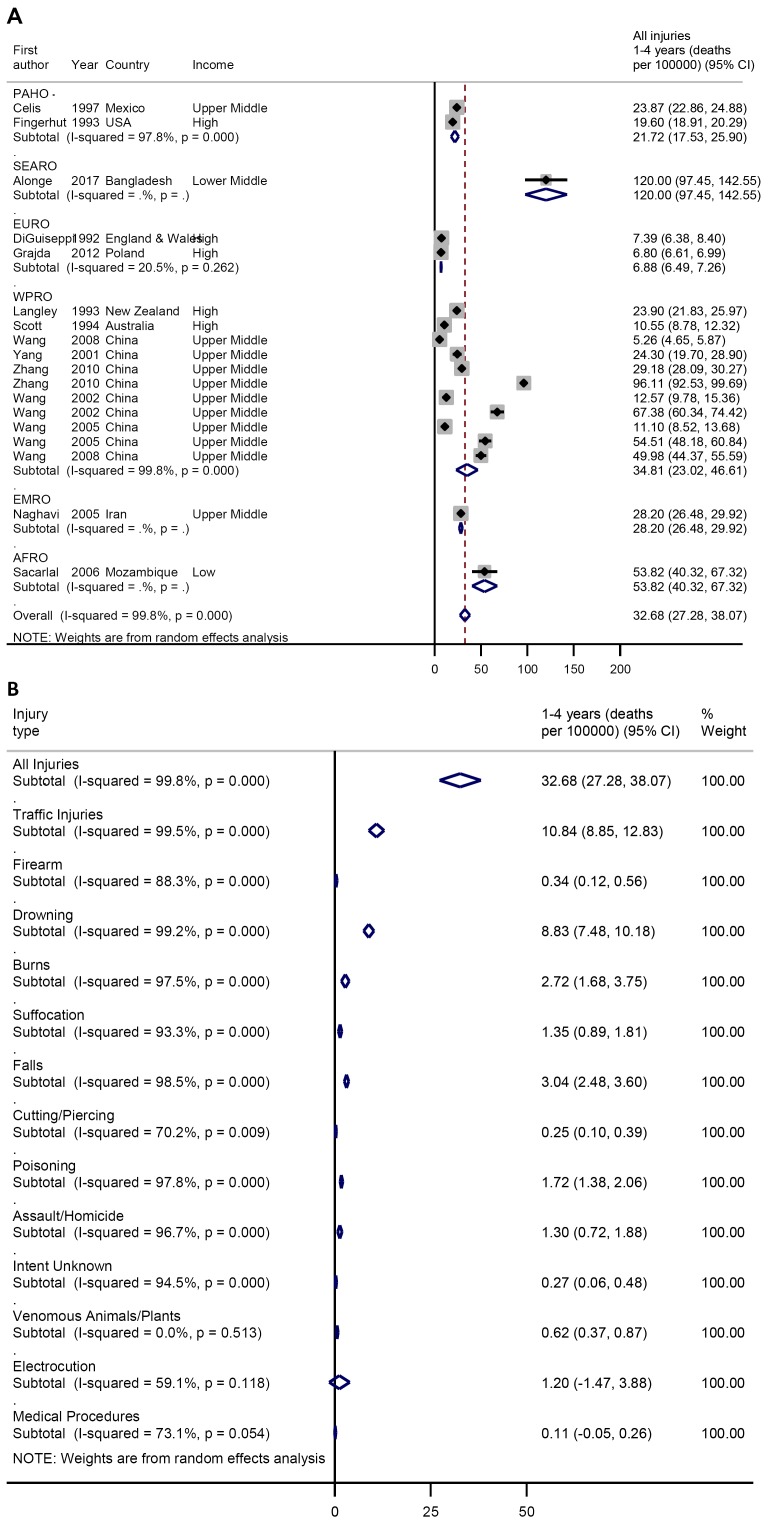
Among children aged 1-4 years, the pooled crude injury mortality rate was 32.7 (27.3-38.1) per 100 000 (Figure 4, plate A). Traffic injuries and drowning the leading causes of deaths at 10.8 (95% CI = 8.9-12.8) and 8.8 (95% CI = 7.5-10.2) per 100 000, respectively. Other causes injury deaths include falls 3.0 (95% CI = 2.5-3.6), burns 2.7 (95% CI = 1.7-3.8) per 100 000, poisoning 1.7 (95% CI = 1.4-2.1) per 100 000 (Figure 4, plate B).
Figure 4.
A. Pooled crude child injury mortality rate by WHO region, 1-4 years. B. Pooled crude child injury mortality rate by type of injury, 1-4 years.
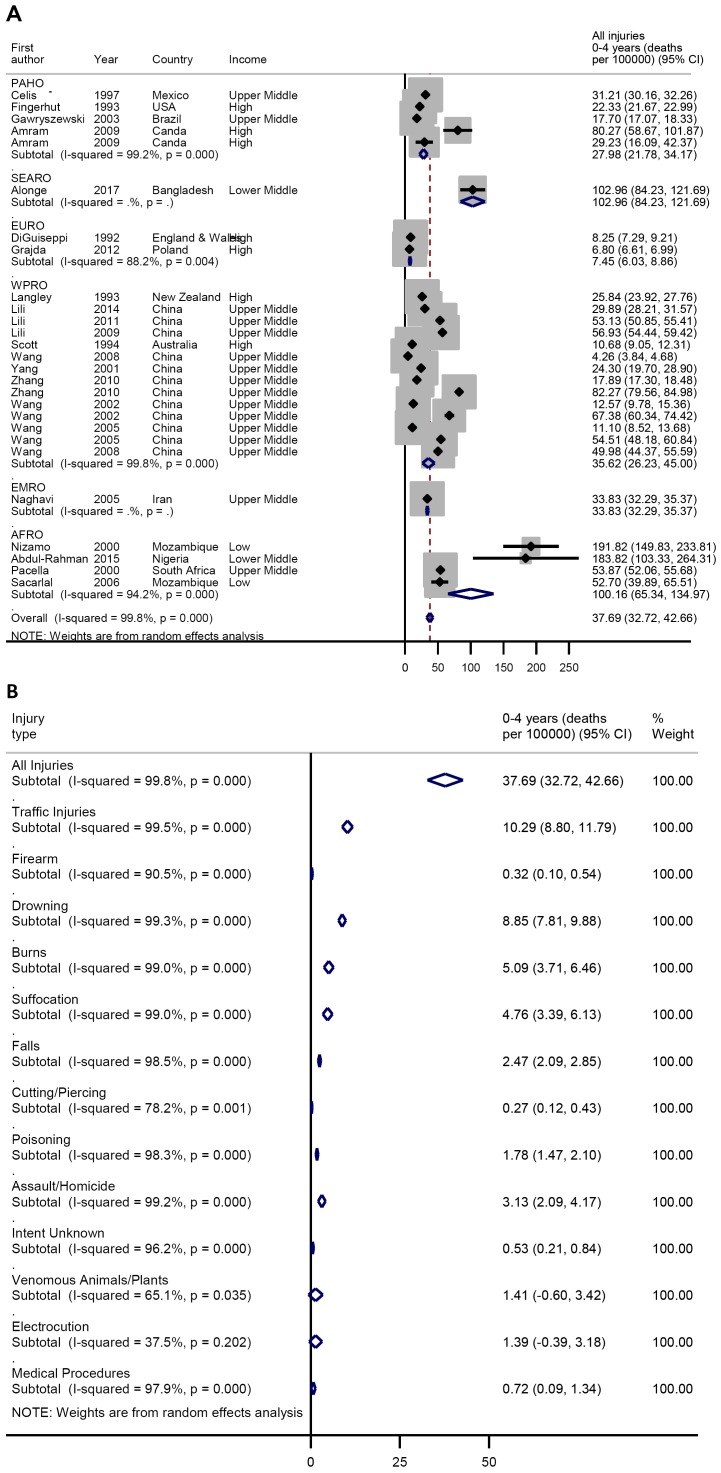
Among children under five years, the pooled injury mortality rate was 37.7 (95% CI = 32.7-42.7) per 100 000 (Figure 5, plate A). Traffic injuries and drowning were also the leading causes of deaths in this age-group at 10.3 (95% CI = 8.8-11.8) and 8.9 (95% CI = 7.8-9.9) per 100 000 respectively. Others include burns 5.1 (3.7-6.5) per 100 000, suffocation 4.8 (95% CI = 3.4-6.1) per 100 000, assault 3.1 (95% CI = 2.1-2.9) per 100 000, falls 2.5 (95% CI = 2.1-2.9) per 100 000, poisoning 1.8 (95% CI = 1.5-2.1) per 100 000, venomous animals and plants 1.4 (95% CI = 0.6-3.4) per 100 000 and electrocution 1.4 (95% CI = 0.4-3.2) per 100 000 (Figure 5, plate B). Further details on the distribution of crude child injury mortality rates across each WHO region are available from Figures S1-S6 in Online Supplementary Document(Online Supplementary Document).
Figure 5.
A. Pooled crude child injury mortality rate by WHO region, 0-4 years. B. Pooled crude child injury mortality rate by type of injury, 0-4 years.
Estimated global and regional deaths from child injuries
The between study variance (adjusted R2) from our model was 30.3%, P = 0.037 (Table 4). Having accounted for crude child injury mortality changes over age, WHO regions, and study period in our model, we estimated that in 2015 there were 522 167 (95% CI = 395 823-648 630) deaths among children aged 0-4 years, accounting for an adjusted injury mortality rate of 80.5 (95% CI = 61.0-100.0) per 100 000. SEARO recorded the highest number of child injury deaths at 195 084 (95% CI = 159 476-230 502) with an adjusted mortality rate at 105.1 (95% CI = 85.9-124.2) per 100 000. This was closely followed by AFRO with 176 523 (95% CI = 115 040-237 831) deaths, with the adjusted mortality rate being the highest from all regions at 118.0 (95% CI = 76.9-159.0) per 100 000. EURO had the lowest number of under-five injury deaths in 2015 at 13 173 (95% CI = 10 539-15 632), with an adjusted injury mortality rate of 37.6 (95% CI = 22.1-32.8) per 100 000 (Table 5).
Table 4.
Meta-regression model statistics
| Under 5 injury mortality (per 100 000) | Coefficient | Standard error | t | P > |t| | Lower CI | Upper CI |
|---|---|---|---|---|---|---|
|
reg1
(PAHO) |
-62.72354 |
23.99989 |
-2.61 |
0.017 |
-112.7864 |
-12.66065 |
|
reg2
(SEARO) |
-12.92205 |
41.31005 |
-0.31 |
0.758 |
-99.09331 |
73.24921 |
|
reg3
(EURO) |
-90.3925 |
29.76 |
-3.04 |
0.007 |
-152.4708 |
-28.31423 |
|
reg4
(WPRO) |
-65.96893 |
20.79313 |
-3.17 |
0.005 |
-109.3426 |
-22.59521 |
|
reg5
(EMRO) |
-67.67915 |
37.58827 |
-1.80 |
0.087 |
-146.0869 |
10.72861 |
|
Year |
1.197741 |
1.043791 |
1.15 |
0.265 |
-.9795689 |
3.375052 |
|
_cons
(AFRO) |
-2299.962 |
2091.543 |
-1.10 |
0.005 |
-6662.844 |
-2062.92 |
|
REML
estimate of between-study variance
(tau2) = 928.7 | ||||||
|
%
residual variation due to heterogeneity
(I2) = 99.77% | ||||||
|
Proportion of between-study variance explained
(adjusted
R2) = 30.33% | ||||||
|
Joint
test for all covariates, Model
F(6,20) = 2.84 | ||||||
|
With
Knapp-Hartung
modification = 0.0365 | ||||||
AFRO – African region, EMRO – Eastern Mediterranean region, EURO – European region, PAHO – Pan-American Health Organization or American region, SEARO – South East Asia region, WPRO – Western Pacific region, Reg – dummy variables representing each WHO region, t – model probability, cons – model constant (equivalent to AFRO region from model), REML – residual maximum likelihood
Table 5.
Global and regional child deaths (0-4 y) by injury type in 2015*
| Injury
type |
World |
AFRO |
EMRO |
EURO |
PAHO |
SEARO |
WPRO |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Rate |
Deaths |
Rate |
Deaths |
Rate |
Deaths |
Rate |
Deaths |
Rate |
Deaths |
Rate |
Deaths |
Rate |
Deaths |
|
|
Traffic
injuries |
21.99 |
142661 |
26.14 |
39110 |
20.24 |
13389 |
7.73 |
3689 |
12.44 |
9279 |
17.04 |
31630 |
10.17 |
12715 |
|
Drowning |
19.00 |
123270 |
6.59 |
9866 |
6.25 |
4135 |
4.42 |
2108 |
7.31 |
5449 |
35.31 |
65533 |
18.09 |
22605 |
|
Burns |
10.89 |
70638 |
38.63 |
57784 |
6.85 |
4529 |
5.15 |
2459 |
10.67 |
7953 |
3.47 |
6440 |
1.98 |
2472 |
|
Suffocation |
10.25 |
66483 |
4.48 |
6695 |
5.95 |
3938 |
3.68 |
1756 |
12.44 |
9279 |
2.76 |
5114 |
7.06 |
8830 |
|
Falls |
5.34 |
34626 |
4.59 |
6871 |
4.17 |
2757 |
1.84 |
878 |
1.38 |
1031 |
14.69 |
27274 |
5.51 |
6888 |
|
Poisoning |
3.84 |
24931 |
1.18 |
1762 |
3.13 |
2067 |
1.47 |
703 |
1.78 |
1326 |
1.84 |
3409 |
3.81 |
4768 |
|
Assault/Homicide |
6.62 |
42937 |
15.19 |
22726 |
2.23 |
1477 |
2.21 |
1054 |
6.52 |
4860 |
4.49 |
8334 |
2.26 |
2826 |
|
Other
injuries† |
2.56 |
16621 |
21.20 |
31711 |
1.49 |
985 |
1.10 |
527 |
2.76 |
2062 |
25.51 |
47350 |
1.41 |
1766 |
|
All
injuries |
80.50 |
522167 |
118.00 |
176523 |
50.30 |
33276 |
27.60 |
13173 |
55.30 |
41239 |
105.10 |
195084 |
50.30 |
62871 |
|
Lower
CI |
61.02 |
395823 |
76.90 |
115040 |
48.96 |
32390 |
22.08 |
10539 |
43.06 |
32107 |
85.92 |
159476 |
37.02 |
46270 |
| Upper CI | 99.99 | 648630 | 158.98 | 237831 | 52.64 | 34822 | 32.75 | 15632 | 67.55 | 50370 | 124.18 | 230502 | 63.58 | 79472 |
AFRO – African region, EMRO – Eastern Mediterranean region, EURO – European region, PAHO - Pan-American Health Organization or American region, SEARO – South East Asia region, WPRO – Western Pacific region
*Estimates based on meta-regression model.
†Includes asphyxiation, firearms, cutting/piercing, venomous animal/plants, electrocution and medical procedures.
Globally, traffic injuries and drowning were the leading causes of under-five injury fatalities in 2015 with 142 661 (22.0 per 100 000) and 123 270 (19.0 per 100 000) child deaths, respectively. Burns were the leading causes of child injury fatalities in AFRO (57784 deaths), drowning in WPRO and SEARO (22 605 and 65 533 deaths, respectively), and suffocation jointly leading with traffic injuries in PAHO (9279 deaths).
DISCUSSION
This study provided the first estimates of the mortality due to injuries, and by specific cause, among children under five years across WHO regions. Several authors have noted that child survival has increased globally, but with uneven progress persisting across many developing countries [2,5]. There are still doubts on the trend in fatalities from child injuries over the years, and how they compare to the decrease observed from other important causes of child mortality [4,8]. This is due to predominantly limited data and research on child injuries across many world settings [13,49]. Our findings thus, among others, highlight the need for renewed efforts from all stakeholders towards addressing a rather hidden burden of child injuries globally.
Our global estimate of over 522 000 (80.5/100 000) children under five years who died due to injuries in 2015 is higher than previously reported. Liu and colleagues [5] estimated over 327000 deaths in 2015, with an upper limit of about 410 000. Our model was primarily based on WHO regions, and with the individual regional estimates contributing to the global estimates. We believe the relatively higher global estimate provided in this study are particularly driven by the higher number of deaths in Africa and South-East Asia. The estimates in these two regions are plausible as previous studies have reported that the two regions contribute highest to overall global child mortality [2]. Besides, the estimate given by Liu and colleagues did not include deaths due to injuries in the neonatal period. We therefore could expect that as a quarter of world’s livebirths was recorded in sub-Saharan Africa in 2015, accidental deaths (eg from asphyxia, at 189/100 000 in this study) in the neonatal period would be relatively higher in this region, ultimately contributing to the high number of deaths we reported. One other factor for the relatively higher estimate is the fact that we reported a greater number of child injury deaths by specific cause (seven) than reported previously, with a small fraction of child deaths (at 2.56/100 000), labelled as “others”, that could not be accounted for (Table 5). For example, the WHO reported an injury mortality of 38.8/100 000 among children under 20 years in 2008 [1], and the category labelled “others” was as high as 34.3% of all deaths at 13.3/100 000 [1]. This implies that with more leading specific causes of child injury deaths reported separately in this study, our overall global estimate for all injuries could expectedly be higher.
Our estimates of higher child deaths from traffic injuries and drowning, representing 27.3% and 23.6% of all injury deaths, have been well documented in previous studies [1,2]. In 2008, the WHO reported that traffic injuries and drowning were the leading causes of deaths among children globally, with an estimated mortality rate of 10.7 and 7.2 per 100 000, respectively among children aged 0-18 years. Drowning was particularly a leading cause of death in the WPRO and SEARO with 22 650 and 65 533 deaths, respectively. Chan et al [17] noted that drowning was the leading cause of injury deaths in China, with about 11 000 deaths in children under five years in 2010, which if expressed in terms of the entire WPRO and demographic changes since then, may be relatively similar to our estimate. According to Chandran et al. [3] drowning is an important cause of unintentional injury deaths accounting for 19% of all injury deaths in children under five years, which is relatively in the range of our proportion of 23.6%.While prevailing unsafe roads with high rates of pedestrian accidents in many LMICs may be attributable to the high deaths from traffic injuries among children [16], the increased access to unfenced water sources in rural areas, and lack of close supervision and unavailability of life jackets at swimming pools and related recreational sites are leading risks for high number of child deaths from drowning in many settings [2]. Addressing safety on world roads and at recreational sites are important steps towards reducing child deaths from injuries.
Meanwhile, in the African region, burns were the leading causes of child injury deaths accounting for 33% of all deaths, compared to traffic injuries at 22%. This is an important finding in this study which underscores a need to address exposures to fire and flames more keenly. Across many LMICs, children aged 1-4 years have been disproportionately affected by burns [50], as children are at increased risk due to prevalent outdoor cooking and use of firewood in rural settings, asides other challenges from limited parental supervision and literacy [51]. The WHO reported that rate of deaths from fire and flames among children in LMICs is close to 11 times higher than recorded in HICs [1].
Although we have attempted to provide improved estimates of child deaths by different causes of injuries and across WHO regions, it is worthwhile to note that our estimates are limited by widespread disparities in child deaths, a challenge that is well situated in many reports. For example, in 2008, Black et al [52] estimated that injuries accounted for 279 000 deaths among children aged 1-4 years, with an upper limit of 738000. In the same year, the WHO estimated 950 000 deaths from injuries among children aged 0–18 years, with mortality among 1-4 years at 45.8/100 000 [1]. In 2015, the GBD collaborators reported even lower estimates of child deaths from injuries with about 180 000 deaths estimated in children aged 0-4 years [2]. These disparities are occasioned by varying study designs, case definitions and limited data from many LMICs, which clearly reflected in the distribution of the pooled crude rates for the different age groups, and the high heterogeneity when our data were aggregated. Besides, with several countries in the South-East Asia and African region not represented, the generalization of these estimates may be somewhat limited.
CONCLUSION
Our findings suggest deaths from child injuries are higher than previously reported. Knowledge and awareness are crucial steps in the response to child deaths from injuries, as several interventions are currently skewed towards infectious, neonatal and nutritional causes. Countries need to leverage on existing low-cost information systems and the established national demographic surveillance to collate and process data on child injuries to inform the needed policy reforms. Moreover, educational campaigns, good road designs and legislation, swimming lessons with necessary safety precautions, and availability of safer homes, schools and communities are proven strategies. We believe the findings of this study are revealing and may have provided better understanding on child injury death profiles needed to guide further research, policy reforms and relevant strategies to reduce this burden across world regions.
Footnotes
Funding: This study was supported by the Maternal and Child Epidemiology Estimates (MCEE) grant from the Bill and Melinda Gates Foundation and by The World Bank Group.
Authorship contributions: IR and DA conceptualized and designed the study. KB and DA conducted the literature searches and prepared the data with oversight from IR. DA, KYC and IR conducted the analysis. DA, KB, KYC, SP, HC and IR wrote the manuscript. All authors have critically reviewed and approved the final manuscript as submitted.
Competing interests: Harry Campbell and Igor Rudan are Co-Editor-in-Chief of the Journal of Global Health. To ensure that any possible conflict of interest relevant to the journal has been addressed, this article was reviewed according to best practice guidelines of international editorial organizations. The authors completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author). The authors declare no competing interests.
Additional Material
REFERENCES
- 1.Peden M, Oyegbite K, Ozanne-Smith J, Hyder AA, Branche C, Rahman AF, et al. World report on child injury prevention. Geneva, Switzerland: World Health Organization; 2008. [PubMed] [Google Scholar]
- 2.Kassebaum N, Kyu HH, Zoeckler L, Olsen HE, Thomas K, Pinho C, et al. Child and adolescent health from 1990 to 2015: Findings from the global burden of diseases, injuries, and risk factors 2015 study. JAMA Pediatr. 2017;171:573–92. doi: 10.1001/jamapediatrics.2017.0250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chandran A, Hyder AA, Peek-Asa C. The global burden of unintentional injuries and an agenda for progress. Epidemiol Rev. 2010;32:110–20. doi: 10.1093/epirev/mxq009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bartlett SN. The problem of children’s injuries in low-income countries: a review. Health Policy Plan. 2002;17:1–13. doi: 10.1093/heapol/17.1.1. [DOI] [PubMed] [Google Scholar]
- 5.Liu L, Johnson HL, Cousens S, Perin J, Scott S, Lawn JE, et al. Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet. 2012;379:2151–61. doi: 10.1016/S0140-6736(12)60560-1. [DOI] [PubMed] [Google Scholar]
- 6.Schuurman N, Cinnamon J, Matzopoulos R, Fawcett V, Nicol A, Hameed SM. Collecting injury surveillance data in low- and middle-income countries: The Cape Town Trauma Registry pilot. Glob Public Health. 2011;6:874–89. doi: 10.1080/17441692.2010.516268. [DOI] [PubMed] [Google Scholar]
- 7.Cinnamon J, Schuurman N. Injury surveillance in low-resource settings using Geospatial and Social Web technologies. Int J Heal Geogr Electronic Resour. 2010;9:25. doi: 10.1186/1476-072X-9-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.de Ramirez SS, Hyder AA, Herbert HK, Stevens K. Unintentional Injuries: Magnitude, Prevention, and Control. Annu Rev Public Health. 2012;33:175–91. doi: 10.1146/annurev-publhealth-031811-124558. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization. International Classification of Diseases, 10th Revision (ICD-10). Geneva, Switzerland: World Health Organization; 2004. [Google Scholar]
- 10.World Health Organization. International Classification of External Causes of Injury (ICECI). Geneva, Switzerland: World Health Organization; 2010. [Google Scholar]
- 11.Overpeck MD, McLoughlin E. Did that injury happen on purpose? Does intent really matter? Inj Prev. 1999;5:11–2. doi: 10.1136/ip.5.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Holder Y, Peden M, Krug E, Lund J, Gururaj G, Kobusingye O. Injury surveillance guidelines. Geneva, Switzerland: World Health Organization; 2001. [Google Scholar]
- 13.Hyder AA, Sugerman DE, Puvanachandra P, Razzak J, El-Sayed H, Isaza A, et al. Global childhood unintentional injury surveillance in four cities in developing countries: A pilot study. Bull World Health Organ. 2009;87:345–52. doi: 10.2471/BLT.08.055798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kirkwood G, Parekh N, Pollock AM. Preventing injury in children and adolescents. Trauma. 2010;12:221–38. doi: 10.1177/1460408610380817. [DOI] [Google Scholar]
- 15.Hyder AA. Injuries in low- and middle-income countries: a neglected disease in global public health. Injury. 2013;44:579–80. doi: 10.1016/j.injury.2013.01.028. [DOI] [PubMed] [Google Scholar]
- 16.Adeloye D, Thompson JY, Akanbi MA, Azuh D, Samuel V, Omoregbe N, et al. The burden of road traffic crashes, injuries and deaths in Africa: A systematic review and meta-analysis. Bull World Health Organ. 2016;94:510–521A. doi: 10.2471/BLT.15.163121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chan KY, Yu X, Lu J, Demaio AR, Bowman K, Theodoratou E. Causes of accidental childhood deaths in China in 2010: A systematic review and analysis. J Glob Health. 2015;5:1–9. doi: 10.7189/jogh.05.010412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Centre for Reviews and Dissemination. Systematic Reviews CRD’s guidance for undertaking reviews in health care. York, UK: Centre for Reviews and Dissemination; 2008. [Google Scholar]
- 19.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 20.Nizamo H, Meyrowitsch DW, Zacarias E, Konradsen F. Mortality due to injuries in Maputo City, Mozambique. Int J Inj Contr Saf Promot. 2006;13:1–6. doi: 10.1080/17457300500151705. [DOI] [PubMed] [Google Scholar]
- 21.Abdur-Rahman L, Taiwo J, Ofoegbu C, Adekanye A, Ajide O, Ijagbemi C, et al. Community survey of childhood injuries in North-Central Nigeria. Ann Pediatr Surg. 2015;11:136–9. doi: 10.1097/01.XPS.0000462928.45595.53. [DOI] [Google Scholar]
- 22.Norman R, Matzopoulos R, Groenewald P, Bradshaw D. The high burden of injuries in South Africa. Bull World Health Organ. 2007;85:695–702. doi: 10.2471/BLT.06.037184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sacarlal J, Nhacolo AQ, Sigaque B, Nhalungo DA, Abacassamo F, Sacoor CN, et al. A 10 year study of the cause of death in children under 15 years in Manhiça, Mozambique. BMC Public Health. 2009;9:1–10. doi: 10.1186/1471-2458-9-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Naghavi M, Pourmalek F, Shahraz S, Jafari N, Delavar B, Motlagh ME. The burden of injuries in Iranian children in 2005. Popul Health Metr. 2010;8:1–9. doi: 10.1186/1478-7954-8-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.DiGuiseppi C, Roberts I. Injury mortality among children and teenagers in England and Wales, 1992. Inj Prev. 1997;3:47–9. doi: 10.1136/ip.3.1.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grajda A, Kułaga Z, Gurzkowska B, Góźdź M, Wojtyło M, Litwin M. Trends in external causes of child and adolescent mortality in Poland, 1999–2012. Int J Public Health. 2017;62:117–26. doi: 10.1007/s00038-016-0908-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Celis A, Villaseńor M. Injury mortality among children and teenagers in Mexico, 1997. Inj Prev. 2001;7:74–5. doi: 10.1136/ip.7.1.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.D’Agostini RA, Guimarăes Blank VL, Marino Calvo MC. Injury deaths in the metropolitan region of Florianópolis, Southern Brazil, 1996–2002. Int J Inj Contr Saf Promot. 2009;16:49–55. doi: 10.1080/17457300802573739. [DOI] [PubMed] [Google Scholar]
- 29.Espitia-Hardeman V, Borse NN, Dellinger AM, Betancourt CE, Villareal AN, Caicedo LD, et al. The burden of childhood injuries and evidence based strategies developed using the injury surveillance system in Pasto, Colombia. Inj Prev. 2011;17:i38–44. doi: 10.1136/ip.2009.026112. [DOI] [PubMed] [Google Scholar]
- 30.Fingerhut LA, Annest JL, Baker SP, Kochanek KD, McLoughlin E. Injury mortality among children and teenagers in the United States, 1993. Inj Prev. 1996;2:93–4. doi: 10.1136/ip.2.2.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gawryszewski VP, Rodrigues EMS. The burden of injury in Brazil, 2003. Sao Paulo Med J. 2006;124:208–13. doi: 10.1590/S1516-31802006000400007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Aldana MCDR, Navarrete N. Epidemiology of a decade of Pediatric fatal burns in Colombia, South America. Burns. 2015;41:1587–92. doi: 10.1016/j.burns.2015.05.005. [DOI] [PubMed] [Google Scholar]
- 33.Amram O, Walker BB, Schuurman N, Pike I, Yanchar N. Disparities in paediatric injury mortality between aboriginal and non-aboriginal populations in British Columbia, 2001–2009. Int J Environ Res Public Health. 2016;13:11–5. doi: 10.3390/ijerph13070651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Clemens T, Tamim H, Rotondi M, Macpherson AK. A population based study of drowning in Canada. BMC Public Health. 2016;16:559. doi: 10.1186/s12889-016-3221-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rahman A, Rahman F, Shafinaz S, Linnan M. Bangladesh Health and Injury Survey Report on Children. Dhaka: Directorate General of Health Services, Ministry of Health and Family Welfare; 2005. [Google Scholar]
- 36.Jagnoor J, Bassani DG, Keay L, Ivers RQ, Thakur JS, Gururaj G, et al. Unintentional injury deaths among children younger than 5 years of age in India: A nationally representative study. Inj Prev. 2011;17:151–5. doi: 10.1136/ip.2010.029934. [DOI] [PubMed] [Google Scholar]
- 37.Alonge O, Agrawal P, Talab A, Rahman QS, Rahman AF, El Arifeen S, et al. Fatal and non-fatal injury outcomes: results from a purposively sampled census of seven rural subdistricts in Bangladesh. Lancet Glob Health. 2017;5:e818–27. doi: 10.1016/S2214-109X(17)30244-9. [DOI] [PubMed] [Google Scholar]
- 38.Huo K, Zhao Y, Feng H, Yao M, Sävman K, Wang X, et al. Mortality rates of children aged under five in Henan province, China, 2004-2008. Paediatr Perinat Epidemiol. 2010;24:343–8. doi: 10.1111/j.1365-3016.2010.01126.x. [DOI] [PubMed] [Google Scholar]
- 39.Langley JD, Smeijers J. Injury mortality among children and teenagers in New Zealand compared with the United States of America. Inj Prev. 1997;3:195–9. doi: 10.1136/ip.3.3.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lili X, Jian H, Liping L, Zhiyu L, Hua W. Epidemiology of injury-related death in children under 5 years of age in hunan province, China, 2009-2014. PLoS One. 2017;12:e0168524. doi: 10.1371/journal.pone.0168524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Scott I, Moller J, Bordeaux S. Injury mortality among children and teenagers in Australia, 1994. Inj Prev. 1997;3:46–7. doi: 10.1136/ip.3.1.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wallis BA, Watt K, Franklin RC, Kimble RM. Drowning in Aboriginal and Torres Strait Islander children and adolescents in Queensland (Australia). BMC Public Health. 2015;15:795. doi: 10.1186/s12889-015-2137-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang Y, He C, Li X, Miao L, Zhu J, Liang J. Nationwide study of injury-related deaths among children aged 1-4 years in China, 2000-2008. J Paediatr Child Health. 2014;50:E94–101. doi: 10.1111/j.1440-1754.2012.02525.x. [DOI] [PubMed] [Google Scholar]
- 44.Yang L, Lam LT, Liu Y, Geng WK, Liu DC. Epidemiological profile of mortality due to injuries in three cities in the Guangxi Province, China. Accid Anal Prev. 2005;37:137–41. doi: 10.1016/j.aap.2004.02.005. [DOI] [PubMed] [Google Scholar]
- 45.Zhang W, Chen D, Xu Y, Yang R, Zhao Z. Mortality Rate for Children under 5 Years of Age in Zhejiang Province, China from 1997 to. PLoS One. 2015;10:e0127770. doi: 10.1371/journal.pone.0127770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zhang L, Li Z, Li X, Zhang J, Zheng L, Jiang C, et al. Study on the trend and disease burden of injury deaths in Chinese population, 2004-2010. PLoS One. 2014;9:e85319. doi: 10.1371/journal.pone.0085319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wang H, Smith GA, Stallones L, Xiang H. Injury-related childhood mortality in migrant households in a Southern City of China. Inj Prev. 2010;16:161–5. doi: 10.1136/ip.2009.023069. [DOI] [PubMed] [Google Scholar]
- 48.Hayman RM, McDonald G, De C, Baker NJ, Mitchell EA, Dalziel SR. Infant suffocation in place of sleep: New Zealand national data 2002-2009. Arch Dis Child. 2015;100:610–4. doi: 10.1136/archdischild-2014-306961. [DOI] [PubMed] [Google Scholar]
- 49.Alonge O, Hyder AA. Reducing the global burden of childhood unintentional injuries. Arch Dis Child. 2014;99:62–9. doi: 10.1136/archdischild-2013-304177. [DOI] [PubMed] [Google Scholar]
- 50.Sharma RK, Parashar A. Special considerations in paediatric burn patients. Indian J Plast Surg. 2010;43:S43–50. doi: 10.4103/0970-0358.70719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Imamura JH, Troster EJ, de Oliveira CAC. What types of unintentional injuries kill our children? Do infants die of the same types of injuries? A systematic review. Clinics (Sao Paulo) 2012;67:1107–16. doi: 10.6061/clinics/2012(09)20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Black RE, Cousens S, Johnson HL, Lawn JE, Rudan I, Bassani DG, et al. Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet. 2010;375:1969–87. doi: 10.1016/S0140-6736(10)60549-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.