In this study, we use a randomized controlled trial design to elucidate the ability of a 5-day course of mupirocin to reduce SA decolonization among infants who are critically ill.
Abstract
Video Abstract
BACKGROUND AND OBJECTIVES:
Staphylococcus aureus (SA) is the second leading cause of late-onset sepsis among infants in the NICU. Because colonization of nasal mucosa and/or skin frequently precedes invasive infection, decolonization strategies, such as mupirocin application, have been attempted to prevent clinical infection, but data supporting this approach in infants are limited. We conducted a phase 2 multicenter, open-label, randomized trial to assess the safety and efficacy of intranasal plus topical mupirocin in eradicating SA colonization in critically ill infants.
METHODS:
Between April 2014 and May 2016, infants <24 months old in the NICU at 8 study centers underwent serial screening for nasal SA. Colonized infants who met eligibility criteria were randomly assigned to receive 5 days of mupirocin versus no mupirocin to the intranasal, periumbilical, and perianal areas. Mupirocin effects on primary (day 8) and persistent (day 22) decolonization at all three body sites were assessed.
RESULTS:
A total of 155 infants were randomly assigned. Mupirocin was generally well tolerated, but rashes (usually mild and perianal) occurred significantly more often in treated versus untreated infants. Primary decolonization occurred in 62 of 66 (93.9%) treated infants and 3 of 64 (4.7%) control infants (P < .001). Twenty-one of 46 (45.7%) treated infants were persistently decolonized compared with 1 of 48 (2.1%) controls (P < .001).
CONCLUSIONS:
Application of mupirocin to multiple body sites was safe and efficacious in eradicating SA carriage among infants in the NICU; however, after 2 to 3 weeks, many infants who remained hospitalized became recolonized.
What’s Known on This Subject:
Staphylococcus aureus is a leading cause of late-onset sepsis among infants in the NICU. Decolonization regimens are used at many centers in an effort to prevent clinical infection, but controlled trials supporting this approach have not been conducted.
What This Study Adds:
A 5-day course of mupirocin applied to the intranasal, periumbilical, and perianal areas was safe and highly efficacious in eradicating S aureus colonization among infants in the NICU, but many who remained hospitalized became recolonized after 2 to 3 weeks.
Staphylococcus aureus (SA) is a leading cause of late-onset sepsis occurring after the third postnatal day among infants receiving intensive care. The risk of infection increases with decreasing birth weight and gestational age, although term infants are also affected, particularly those undergoing invasive procedures.1,2 Multicenter surveillance conducted in the United States between 2000 and 2011 revealed SA in 12% of episodes of late-onset sepsis among infants weighing ≤1000 g.3 Associated mortality has reached 25% among infants weighing ≤1500 g.4 Interventions to prevent these infections have the potential to improve survival for infants who are critically ill while reducing adverse outcomes, hospital stay, antibiotic use, and health care costs.5,6
The observation that SA colonization is a strong predictor of subsequent invasive infection serves as the basis for most available interventions.7,8 Approaches have included preventing transmission of SA by actively screening and isolating colonized infants9 and attempting to eradicate SA in infants who have become colonized using nasal and/or topical antimicrobial agents, such as mupirocin and chlorhexidine.10,11 In most interventions, researchers have targeted methicillin-resistant S aureus (MRSA) without concern for methicillin-susceptible S aureus (MSSA) because treatment options for MRSA are more limited, and some data suggest that MRSA infections are more severe.12 In the NICU, morbidity and mortality from MRSA and MSSA appear equivalent.4
After a randomized trial among adults revealed that mupirocin and chlorhexidine administration to all ICU admissions was efficacious in preventing nosocomial MRSA infection,9 guidelines were developed for universal MRSA decolonization of ICU patients.13 However, uncertainties about the applicability of these results to infants who are critically ill, particularly those who are premature, justify the need for evaluation before widespread implementation in the NICU.14–16 We conducted a phase 2 multicenter, open-label, randomized trial to assess the safety and efficacy of applying mupirocin to multiple sites (intranasal, periumbilical, and perianal) in eradicating the colonization of both MRSA and MSSA in infants who are critically ill.
Methods
Participants
The study was performed at NICUs in the United States associated with 6 Vaccine and Treatment Evaluation Units funded by the National Institute of Allergy and Infectious Diseases (see Study Sites Affiliated With the Vaccine Treatment and Evaluation Units in the Supplemental Information). At 1 NICU, nasal swabs were collected to identify SA colonization from all admissions, whereas the other centers performed selective nasal swab screenings of infants <24 months old who had an anticipated NICU stay of >14 days and lacked exclusionary congenital anomalies (Eligibility Criteria section of the Supplemental Information). Swabs were obtained as soon as possible after admission and then weekly thereafter. The median time from admission to the first swab at each site ranged from 0 (day of admission) to 4 days. Infants who tested positive for SA were assessed for eligibility (Eligibility Criteria section of the Supplemental Information) by the study team. At 1 site, infants with birth weights <1000 g who had nasal swabs positive for MRSA were routinely treated with mupirocin and were excluded from participation in this study. Isolation precautions were routine at all centers for infants who were MRSA-positive but not for infants who were MSSA-positive.
Randomization and Interventions
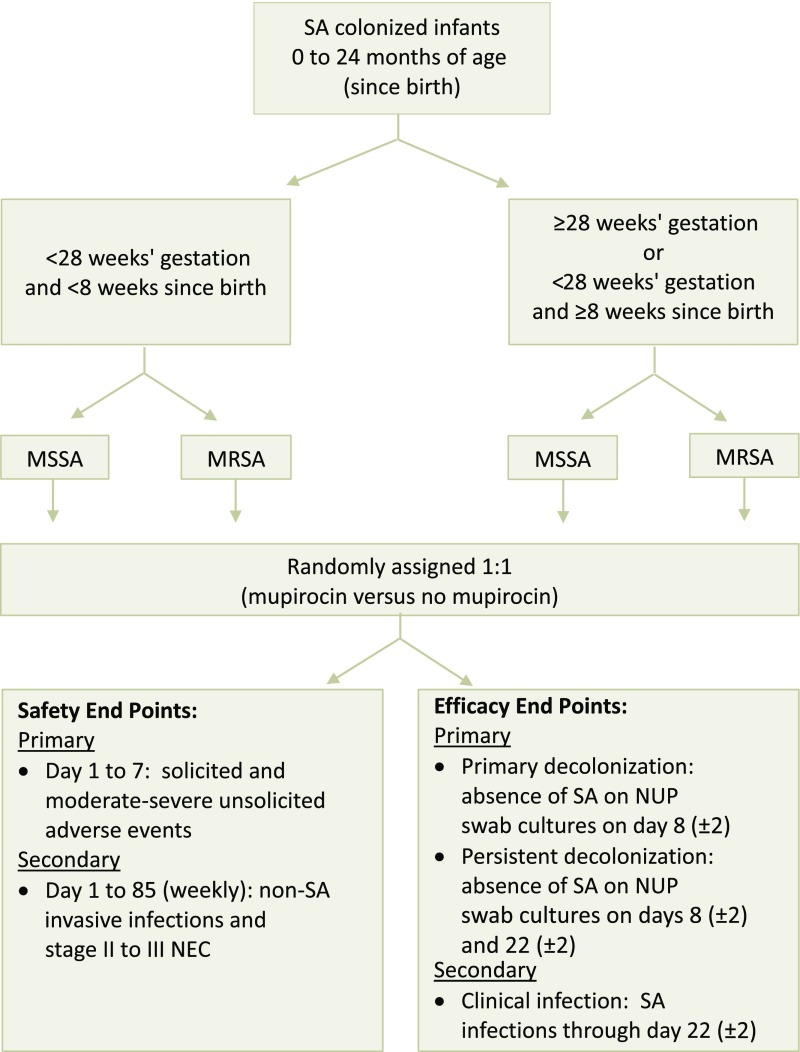
Infants enrolled at each site were stratified into 2 groups according to gestational age, postnatal age, and colonizing strain (MRSA versus MSSA; Fig 1). Age strata were defined as either <28 weeks’ gestation and <8 weeks of postnatal life (termed <28 weeks group) or >28 weeks’ gestation (termed >28 weeks group). Infants of <28 weeks’ gestation but >8 weeks postnatal age were included in the >28 weeks group. The single infant who tested positive for both MRSA and MSSA was categorized as MRSA-positive. Infants were randomly assigned by strata 1:1 to receive either mupirocin (treatment group) or no treatment (control group) by using an online module displaying only individual assignments (The Emmes Corporation, Rockville, MD).
FIGURE 1.
Study design. Day 1 began at the time the first dose of mupirocin was administered (treatment group) or at the time of randomization (control group) and ended at 11:59 pm of that same day. Subsequent days for patients and controls coincided with calendar days.
Within 24 hours of randomization, the treatment group began a 5-day course of mupirocin every 8 (±2) hours. Each dose was dispensed by the investigational pharmacy and consisted of mupirocin calcium 2% cream to the periumbilical and perianal areas and mupirocin calcium 2% intranasal ointment to the nares, applied in a standardized fashion by trained clinical nursing staff (Mupirocin Administration section of the Supplemental Information).
Surveillance for Clinical End Points
The study team reviewed the medical record and interviewed the parent or guardian at enrollment to document medical history, demographic characteristics, and clinical findings. Postrandomization clinical data were abstracted from medical records and clinical team interviews.
Nurses administering the study drug recorded pre- and postintervention pain assessment scores, vital signs, apneic events within 3 to 5 minutes after nasal application, and the maximal intervention level initiated for any discomfort or apnea detected. Trained study staff collected nasal, periumbilical, and perianal (NUP) swabs from infants in the treatment and control groups to culture for MSSA and MRSA within 24 hours of randomization (before treatment), every 2 weeks from day 8 to 64 (±2 days), and then on day 85 (±2 days). Conventions for assigning day numbers are described in Fig 1.
Objectives and End Points
The primary objective was to evaluate the safety and clinical acceptability of the mupirocin regimen, defined as the frequency of solicited adverse events (AEs) (fever, rash, nasal mucosal swelling, epistaxis, diarrhea, apnea, bradycardia, pain, and/or desaturations), moderate and severe unsolicited AEs, and serious AEs on days 1 to 7. Study personnel collected and graded events for severity and relationship to mupirocin (Grading of AEs section of the Supplemental Information).
The coprimary objective was to measure the efficacy of mupirocin in eradicating SA colonization. Decolonization was defined as the absence of SA in all NUP cultures. The absence of SA on day 8 ± 2 was considered primary decolonization, whereas the absence of SA on days 8 ± 2 and 22 ± 2 was considered persistent decolonization.
Secondary safety objectives were to assess for associations between mupirocin and non-SA clinical infections or severe necrotizing enterocolitis (NEC) (stages II and III by the Simplified Bell Staging System)17 during days 1 to 85 or until discharge. These events were considered theoretical undesired outcomes of drug-induced alterations in microbiota. Secondary efficacy objectives were to examine the efficacy of mupirocin in preventing clinical SA infections during days 1 to 22 or until discharge and time until SA decolonization. Clinical SA infection was defined as a culture of SA from a normally sterile body site or from the site of a clinical infection (Definitions of Clinical SA Infections and NEC section of the Supplemental Information).18 Prevention of clinical SA infection during days 23 to 85 was an exploratory objective.
Laboratory Methods
SA was detected in screening nasal swabs by culture or polymerase chain reaction in each site’s laboratory per local practices. By using protocol-defined methods, NUP swabs were cultured directly on BBL CHROMagar SA plates (Becton Dickinson, Sparks, MD) and incubated at 35 to 37°C overnight. Methicillin resistance was determined by either cefoxitin disk diffusion or oxacillin screening agar. SA isolates were cryopreserved at −70°C by using either Microbank or tryptic soy broth with 15% glycerol19 and shipped to Vanderbilt University Medical Center for mupirocin susceptibility testing using a commercially available E-test (Biomerieux, Durham, NC). All putative MRSA isolates were confirmed by detection of mecA.20
Statistical Analysis
The primary and secondary safety analyses and the secondary efficacy analysis were performed by using the intent-to-treat (ITT) cohort, which included all infants enrolled and randomly assigned (Fig 1). The primary efficacy analysis was performed on the modified intent-to-treat (mITT) cohort, which included infants whose NUP swabs obtained within 24 hours of randomization (controls) or within 24 hours before treatment (mupirocin group) were SA-positive at 1 or more body sites. Thus, infants who were spontaneously decolonized between screening and treatment were excluded from analysis. Infants in the mITT analysis of primary (day 8) and persistent (day 22) decolonization were designated to the modified intent-to-treat analysis of decolonization on day 8 (primary decolonization) (mITT-8) and modified intent-to-treat analysis of decolonization on day 22 (persistent decolonization) (mITT-22) cohorts, respectively.
Treatment effects on decolonization were assessed by using Fisher’s exact tests and exact 95% confidence intervals (CIs). Multiplicity, including CIs,21 was controlled by using the Holm method. Stratified analyses of treatment effects on decolonization were performed by using the Mantel-Haenszel test. Time effects (season and year) of colonization incidence during screening were assessed by Poisson regression, controlling for site and allowing for overdispersion. Time-to-event hazard ratios were estimated by using Cox proportional hazards models. For mupirocin efficacy, defined as 1 minus the relative risk (ratio of the proportions of subjects not decolonized, mupirocin-treated over controls), 95% CIs22,23 were provided. A sample size of 94 infants who were evaluable was chosen a priori to provide 90% power for the primary analysis, assuming a treatment increase of decolonization from a 35% basal rate to 70%.
Safety Oversight and Ethical Approvals
The protocol was approved by each site’s institutional review board. Each participant’s parent or legal guardian gave informed written consent before the initiation of study activities. A data safety monitoring board provided safety oversight.
Results
Participants
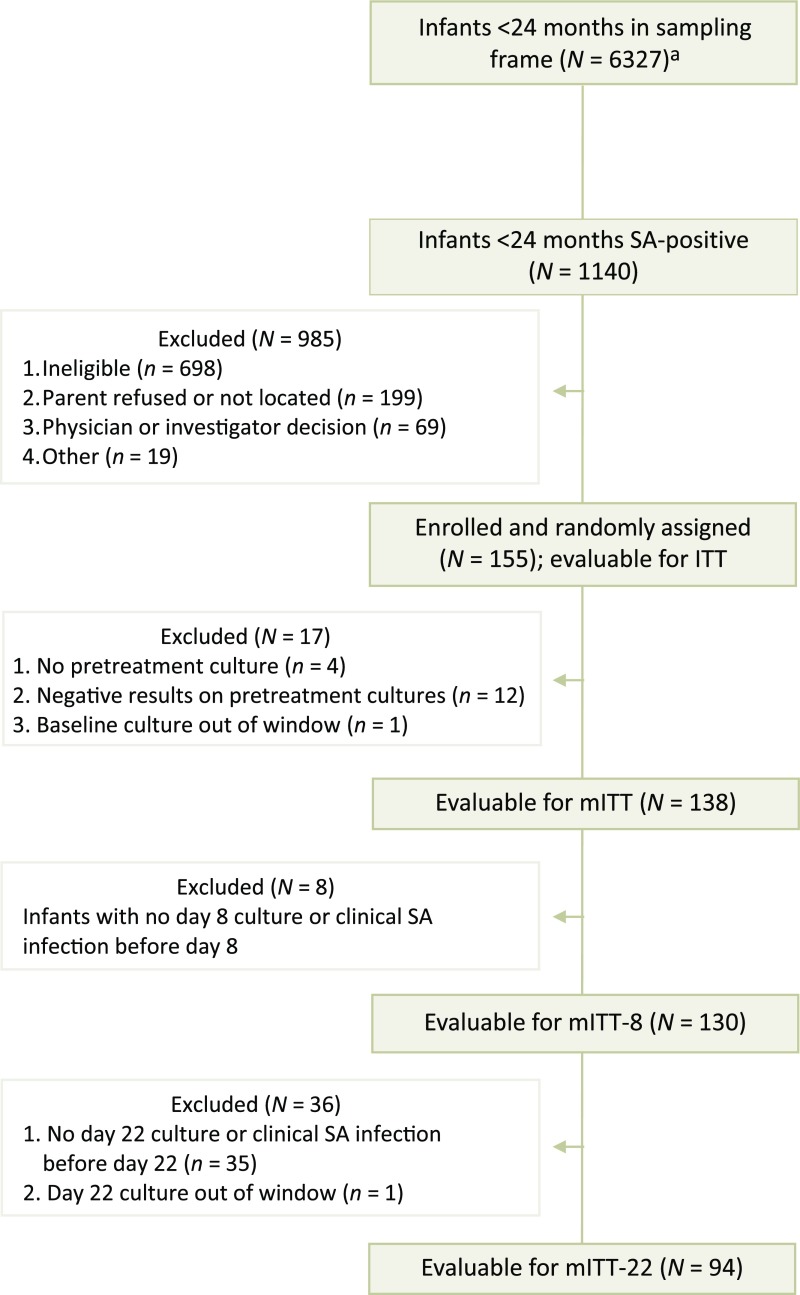
Between April 2014 and May 2016, SA was identified by nasal swabs from 1140 (18%) of 6327 infants, of whom 236 (20%) had MRSA, 902 (79%) had MSSA, 1 (<1%) had both, and 1 (<1%) was not specified; 155 of these infants with positive results (14% with MRSA and 86% with MSSA) were enrolled, randomly assigned, and included in the ITT analysis (Fig 2). The most common reason for the exclusion of 985 infants with SA colonization was ineligibility due to an anticipated NICU stay of <14 days (41.7%). A total of 130 infants were eligible for mITT-8 and 94 were eligible for mITT-22. Most infants who were treated received at least 13 of the 15 required mupirocin doses to both nares (94%) and to the periumbilical (91%) and perianal (90%) areas. Demographic and clinical features of treated and untreated groups at enrollment were comparable, as was the proportion with positive results at each NUP site (Table 1) and the proportion who completed the study.
FIGURE 2.
Subject enrollment. a Nasal swabs were collected from all admissions (universal screening) or from infants <24 months old who had an anticipated NICU stay of >14 days and lacked an exclusionary congenital anomaly (selective screening).
TABLE 1.
Demographic and Clinical Characteristics at Enrollment by Treatment Group for All Infants Randomly Assigned
| Mupirocin Group (n = 80) | Control Group (n = 75) | |
|---|---|---|
| Male sex, n (%) | 45 (56) | 42 (56) |
| Hispanic ethnicity, n (%) | 2 (3) | 4 (5) |
| Race, n (%) | ||
| Asian American | 1 (1) | 1 (1) |
| African American | 22 (28) | 25 (33) |
| White | 50 (63) | 41 (55) |
| Multiracial | 6 (8) | 7 (9) |
| Unknown | 1 (1) | 1 (1) |
| Birth wt, n (%), ga | ||
| <1000 | 29 (36) | 28 (37) |
| 1000–1500 | 23 (29) | 23 (31) |
| >1500 | 26 (33) | 22 (29) |
| Gestational age, n (%), wk | ||
| <28b | 21 (26) | 21 (28) |
| 28c | 59 (74) | 54 (72) |
| Postnatal age at enrollment, median (range), wk | 4 (0–22) | 3 (1–24) |
| Major comorbidities, n (%)d | ||
| NEC | 4 (5) | 1 (1) |
| Respiratory distress syndrome | 60 (75) | 56 (75) |
| Apnea of prematurity | 51 (64) | 48 (64) |
| Surgical procedures | 16 (20) | 14 (19) |
| With indwelling tubes or catheters, n (%) | ||
| Endotracheal tube or tracheostomy | 7 (9) | 6 (8) |
| Central vascular access | 14 (18) | 12 (16) |
| Orogastric tube | 23 (29) | 22 (29) |
| Screening nasal colonizing strain, n (%)e | ||
| MRSA or MRSA plus MSSA | 12 (15) | 8 (11) |
| MSSA | 66 (82) | 67 (89) |
| No positive results on baseline culture | 2 (3) | 0 |
| Pretreatment colonizing site, n (%)f | ||
| Nasal | 72 (90) | 66 (88) |
| Periumbilical | 31 (39) | 26 (35) |
| Perianal | 33 (41) | 18 (24) |
| No. sites colonized, n (%)g | ||
| 0 | 5 (6) | 7 (9) |
| 1 | 30 (37) | 34 (45) |
| 2 | 23 (29) | 20 (27) |
| 3 | 20 (25) | 12 (16) |
Includes all 155 infants evaluable for the ITT analysis.
Four subjects were discharged from the hospital after randomization but before obtaining pretreatment NUP cultures and medical history.
Denotes <28 wk gestation and <8 wk postnatal life.
Denotes ≥28 wk gestation or <28 wk gestation and ≥8 wk of postnatal life.
These categories are not mutually exclusive.
Infants who had a surveillance nasal swab positive for SA were enrolled and randomly assigned.
Positive results on pretreatment NUP cultures were required for infants to be eligible for the mITT analysis.
Cultures were not collected from 2 infants treated with mupirocin and 2 control infants.
SA Incidence
The center-specific proportion of infants who were nasally screened and acquired SA after remaining in the NICU for at least 7 days ranged from 11% to 44%, with a corresponding incidence of 6.9 to 15.5 per 1000 hospital days. Statistically significant differences in the incidence of SA colonization were not seen by year of study or season.
Safety and Tolerability
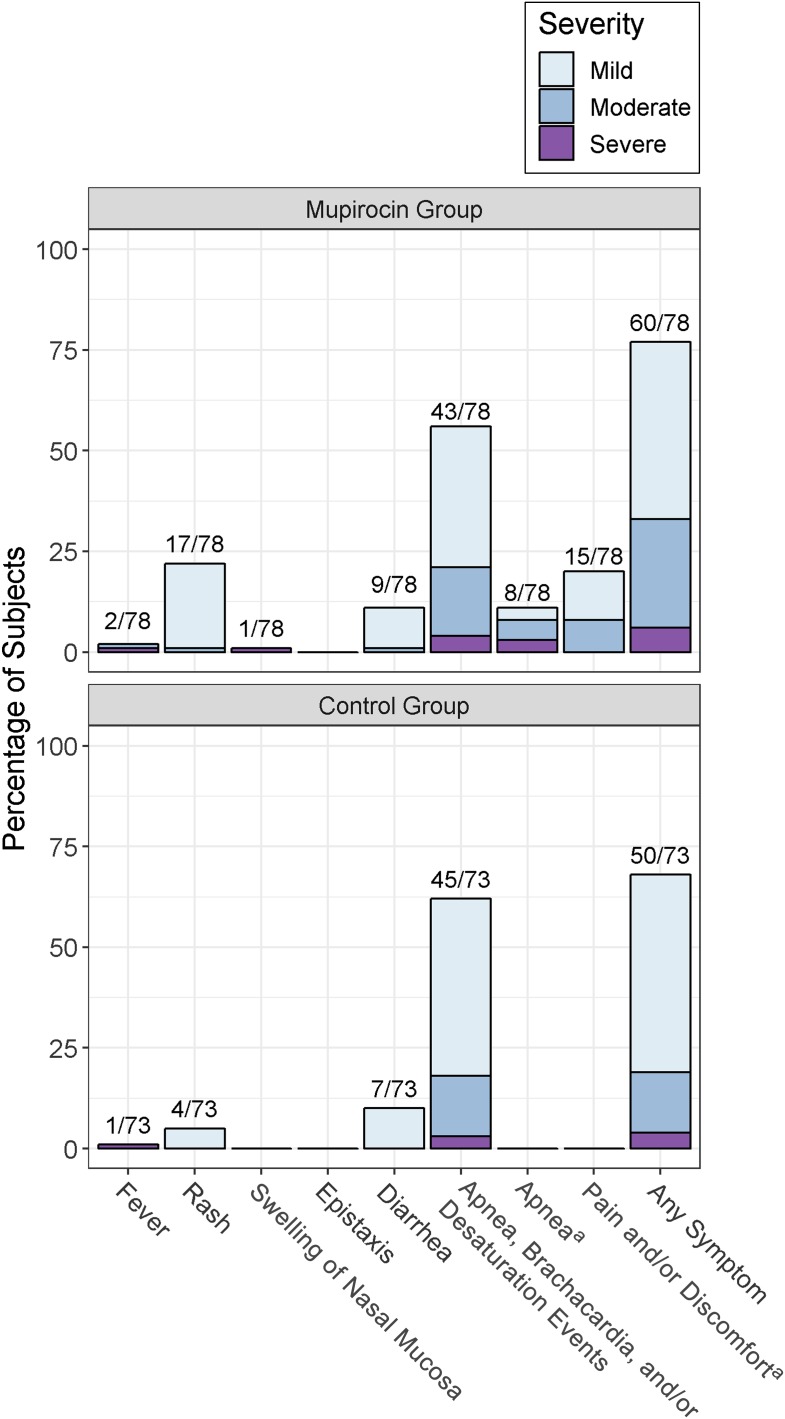
Overall, mupirocin was well tolerated (Fig 3). Rash was the only solicited reaction that was observed significantly more often in infants who were treated (22% vs 5%, odds ratio 5.1; 95% CI 1.5–21.7; P = .004). Most rashes were mild (1 had moderate severity), localized to the perianal area, and attributed to either contact dermatitis or yeast infection. One infant met criteria for severe nasal mucosal swelling (defined as bilateral involvement), with onset on day 7 and a duration of 3 weeks; the swelling was attributed to reflux-induced vomiting and irritation from a nasal cannula. Two infants (3%) experienced severe apnea within 3 to 5 minutes of mupirocin application, and no infant experienced severe pain or discomfort. Non-SA clinical infections occurred in 8% of infants who were treated and 7% of infants who were untreated. No infant in either group experienced severe NEC, or a product-related serious, moderate, or severe AE.
FIGURE 3.
Maximum severity of solicited AEs during 1 to 7 days in infants treated with mupirocin and controls, who were not treated. a Apnea and pain and/or discomfort were collected within 3 to 5 minutes of mupirocin application but were not collected for controls.
Efficacy
Primary decolonization occurred in significantly more recipients of mupirocin (94%) than controls who were untreated (5%), yielding an overall efficacy of 95% (Table 2). The treatment effect on primary decolonization was statistically significant at all study centers, with success rates reaching 100% at 5 of 7 centers and at least 85% at all centers (Supplemental Tables 8 and 9). Significantly more infants who were treated (46%) than control infants (2%) who had primary decolonization and remained in the NICU were persistently decolonized on day 22, yielding an efficacy of 44% (Table 2). The treatment effect on persistent decolonization was statistically significant at the 2 centers with the most participants in the mITT-22 cohort (Supplemental Tables 8 and 9). There were no apparent trends in the success of decolonization according to age strata or a methicillin susceptibility profile. Mupirocin use led to significantly higher frequencies of primary and persistent decolonization at each of the 3 application areas (Table 3).
TABLE 2.
Primary and Persistent SA Decolonization According to Group Assignment and Stratum
| Gestational Age | Enrollment Straina | Group | Decolonization, n (%) | No Decolonization, n (%) | Odds Ratio (95% CI) | P | Efficacy, % |
|---|---|---|---|---|---|---|---|
| Primary decolonization (mITT-8 group; n = 66 mupirocin recipients and 64 controls) | |||||||
| <28 wkb | MRSA | Mupirocin | 2 (100) | 0 (0) | — | .333 | 100 |
| Control | 0 (0) | 2 (100) | — | — | — | ||
| ≥28 wkc | MRSA | Mupirocin | 9 (100) | 0 (0) | — | <.001 | 100 |
| Control | 0 (0) | 5 (100) | — | — | — | ||
| <28 wkb | MSSA | Mupirocin | 16 (100) | 0 (0) | — | <.001 | 100 |
| Control | 1 (6) | 15 (94) | — | — | — | ||
| ≥28 wkc | MSSA | Mupirocin | 35 (90) | 4 (10) | 171 (25–1699) | <.001 | 89 |
| Control | 2 (5) | 39 (95) | — | ||||
| Total primary decolonizationd | All | Mupirocin | 62 (94) | 4 (6) | 288 (58–1433) | <.001 | 94 (85–98) |
| Control | 3 (5) | 61 (95) | — | — | |||
| Persistent decolonization (mITT-22 group, n = 46 mupirocin recipients and 48 controls) | |||||||
| <28 wk | MRSA | Mupirocin | 1 (100) | 0 (0) | — | .333 | 100 |
| Control | 0 (0) | 2 (100) | — | — | — | ||
| ≥28 wk | MRSA | Mupirocin | 2 (50) | 2 (50) | — | .167 | 50 |
| Control | 0 (0) | 5 (100) | — | — | — | ||
| <28 wk | MSSA | Mupirocin | 7 (47) | 8 (53) | — | .006 | 47 |
| Control | 0 (0) | 14 (100) | — | — | — | ||
| ≥28 wk | MSSA | Mupirocin | 11 (42) | 15 (58) | 19 (2–851) | <.001 | 40 |
| Control | 1 (4) | 26 (96) | — | — | — | ||
| Total persistent decolonizationd | All | Mupirocin | 21 (46) | 25 (54) | 37 (5–284) | <.001 | 44 (30–59) |
| Control | 1 (2) | 47 (98) | — | — | — |
—, not applicable.
Infants colonized with both MRSA and MSSA are listed as MRSA.
Less than 28 wk gestation and <8 wk postnatal age.
Greater than or equal to 28 wk gestation or <28 wk gestation and ≥8 wk of postnatal life.
Mantel-Haenszel χ2 test.
TABLE 3.
Decolonization by Body Area Among 130 Infants Eligible for the mITT-8 and 94 Infants Eligible for the mITT-22
| End Point | Anatomic Sitea | Treatment Group | Primary Decolonization, n (%) | No Primary Decolonization, n (%) | Odds Ratio (95% CI) | P | Efficacy, % |
|---|---|---|---|---|---|---|---|
| Primary decolonization (mITT-8 group) | Nasal | Mupirocin | 62 (95) | 3 (5) | 420 (70–2997) | <.001 | 95 |
| Control | 3 (5) | 61 (95) | — | — | — | ||
| Umbilical | Mupirocin | 27 (100) | 0 (0) | — | <.001 | 100 | |
| Control | 7 (27) | 19 (73) | — | — | — | ||
| Perianal | Mupirocin | 30 (97) | 1 (3) | 98 (9–4270) | <.001 | 96 | |
| Control | 4 (24) | 13 (77) | — | — | — | ||
| Persistent decolonization (mITT-22 group) | Nasal | Mupirocin | 23 (51) | 22 (49) | 49 (7–2066) | <.001 | 50 |
| Control | 1 (2) | 47 (98) | — | — | — | ||
| Umbilical | Mupirocin | 15 (94) | 1 (6) | 56 (5–2518) | <.001 | 92 | |
| Control | 4 (21) | 15 (79) | — | — | — | ||
| Perianal | Mupirocin | 15 (75) | 5 (25) | 12 (2–138) | .007 | 69 | |
| Control | 2 (20) | 8 (80) | — | — | — |
—, not applicable.
Each analysis includes only subjects with baseline colonization at the respective anatomic site.
The emergence of mupirocin resistance in subjects who were treated was not observed. However, the proportion of infants who were colonized with mupirocin-resistant strains at enrollment increased from 0% during the first 14 months of the study to 6% during the final 12 months (P = .05). The 4 resistant strains were observed at the center with the most enrollments (not the center administering mupirocin routinely to infants <1000 g at birth who were colonized).
The incidence of clinical infections per 1000 hospital days in infants who were mupirocin-treated versus controls before day 22 was 0.70 (95% CI 0.10–5.00) vs 3.11 episodes (95% CI 1.17–8.29). The mITT analysis of time to clinical infection before day 22 yielded a hazard ratio of 0.23 (95% CI 0.03–2.01; P = .18). All clinical infections (with the exception of the 1 treatment failure before day 22) were attributed to MSSA, matched the methicillin susceptibility of the colonizing strain, and manifested as either purulent soft-tissue infection or pneumonia (accompanied by bacteremia in 2 infants).
Discussion
To our knowledge, this is the first multicenter, randomized controlled trial used to assess the efficacy and durability of mupirocin in eradicating SA colonization among infants <24 months of age residing in a NICU. Numerous studies have revealed the value of mupirocin in controlling outbreaks in the NICU, but the impact on endemic SA colonization and its associated risks of SA transmission and progression to clinical infection are less certain.8,24–26 With this in mind, we managed infants for both primary (day 8) and persistent (day 22) decolonization. We addressed the likelihood that colonization would be present at multiple anatomic sites by applying mupirocin to multiple body sites rather than supplementing nasal mupirocin with chlorhexidine baths, which have undetermined safety in premature infants.27 We surveyed participants for unintended consequences that could result from perturbation of the microbiome, such as severe NEC and non-SA clinical infection, and other adverse reactions. Finally, we included infants colonized with both MRSA and MSSA.
Our findings reveal that mupirocin was highly efficacious (85%–100%) in inducing primary SA decolonization, impacting both MRSA and MSSA and extending across study centers, anatomic sites, and gestational age strata. A concomitant trend revealed a reduction in clinical SA infections before day 22, but the results did not achieve statistical significance. An exploratory survival analysis of clinical SA infections suggested that the reduction in SA infections would wane after day 22, which was supported by observations that recolonization occurred in approximately half of infants treated with mupirocin by day 22 and in 70% by day 85. A persistent reservoir of SA likely led to ongoing transmission, which was consistent with the steady incidence of SA acquisition during the 36-month study period.28 Supplementary strategies that might reduce recolonization include targeted retreatment of patients who have been recolonized and decolonization of caregivers and family members.29
Various targeted MRSA decolonization programs for infants in the NICU have been evaluated retrospectively by using historical controls as the comparator.28,30,31 In some instances, infants who had been recolonized were retreated. Each of these studies revealed a treatment effect; however, the duration of the effect, the impact of retreatment, and the effect of secular changes cannot be fully elucidated when historical controls are used.
A prospective cluster randomized trial of adults in the ICU revealed that a 5-day course of twice-daily intranasal mupirocin plus daily chlorhexidine baths administered to all patients at admission without regard to SA colonization status was superior to targeted decolonization of patients with MRSA colonization or a previous infection.9 During the 18-month intervention, universal decolonization at admission reduced MRSA-positive clinical culture results by 37% compared with 25% for targeted decolonization, although a significant decrease in MRSA bloodstream infections was not seen. The prompt reduction in the reservoir of SA that resulted from treating all patients without awaiting results of screening tests likely contributed to the superiority of universal decolonization in this trial.26 Another contributing factor may be the relatively brief duration of hospitalization (median 7 days), thus limiting the risk of recolonization. Universal decolonization was also more effective than targeted decolonization in reducing bloodstream infections from any pathogen, an effect likely mediated by chlorhexidine baths.32 Whether a universal decolonization regimen would be similarly effective among infants who are critically ill is unknown. A retrospective study evaluated a 7-year program in which mupirocin was applied to the nares, umbilicus, eroded skin, and wounds of all patients in the NICU twice daily throughout hospitalization.30 The SA colonization rate decreased from 60% at baseline to <5%; however, there were periodic peaks to 20% that were associated with clinical infections.
In our study, we provided careful observations of AEs related to mupirocin use in a controlled, open-label fashion and identified no serious safety concerns. The perianal rashes that appeared to be treatment-related did not lead to systemic complications. The absence of NEC and non-SA clinical infections in our study and elsewhere is also reassuring.31 Finally, emergence of mupirocin-resistant strains was uncommon in our population, as it has been in other NICU decolonization programs.8,33 Resistant strains appeared in enrollment swabs at 1 site, but we cannot determine whether the cause was our intervention or the introduction of a resistant strain from an exogenous source. Nonetheless, widespread use of mupirocin could induce resistance and should be considered in decisions regarding programmatic use.34
Several limitations of our study are noteworthy. The open-label design could produce reporting bias, particularly for safety parameters (such as rash), because the nurses were instructed to examine infants who were treated for rash before each mupirocin application. Concerns about a possible increased risk of nosocomial infection related to inert topical ointments in premature infants led to the decision not to use a placebo.35–37 Our study was not statistically powered to assess the secondary and exploratory aims of preventing clinical SA infection, which therefore can only be inferred by considering the strong association between colonization and infection. Most importantly, our stringent inclusion and exclusion criteria, screening requirements, and targeted decolonization strategy resulted in only ∼14% of all infants who were colonized undergoing randomization, half of whom received mupirocin. The low treatment coverage was largely attributable to the decision to enroll only infants whose length of stay would be ≥14 days from screening to allow sufficient time for treatment and evaluation of primary decolonization.
Our study reveals several drawbacks related to the strategy of screening infants in the NICU for SA and targeting those with positive results for isolation and decolonization with mupirocin. For one, our observation that the vast majority of infants who are colonized and who develop clinical infection harbor MSSA rather than MRSA suggests that the common focus on infants with MRSA alone is inadequate. Second, although we were not statistically powered to assess the secondary aim of preventing clinical SA infection, our results suggest that a large number of infants (25) would need to receive mupirocin to prevent 1 clinical SA infection. Third, in NICUs where length of stay is prolonged, reacquisition of SA is likely and may be associated with an increased risk of clinical infection. Finally, although mupirocin resistance has been uncommon to date in NICUs with decolonization programs, it has occurred in other inpatient settings.38,39 Susceptibility patterns should be monitored when consistent use is expected.34
Conclusions
We found that mupirocin was safe and highly efficacious in inducing primary SA decolonization in the NICU, an effect that is expected to translate to the prevention of clinical infection during the 2- to 3-week period after colonization, at which time most SA infections seem to occur.4,29 With these findings, it is suggested that in NICUs where clinical SA infections are prevalent, mupirocin decolonization might reduce the burden of MRSA and MSSA and prevent clinical infections. However, with the observed recolonization thereafter it is suggested that more effective means for interrupting transmission should be sought.
Acknowledgments
We thank all of the families who participated in the study. We acknowledge Alexander Agthe, MD, and Harry Keyserling, MD, for assistance with this study, and J. Kristy Johnson, PhD, for contributions to microbiologic methods and the performance of laboratory assays. We thank the following individuals who provided support and oversight: Richard Gorman, MD, Suzanne Murray, RN, BSN, Mirjana Nesin, MD, Janie Russell, Venus Shahamatdar, MD, Marina Lee, PhD, Effie Nomicos, MSN, and Dennis Dixon, PhD (National Institute of Allergy and Infectious Disease, Division of Microbiology and Infectious Disease). We thank Stephanie Pettibone for assistance with data management and the members of the Data Safety Monitoring Board (Leonard Weisman, MD, Vance Fowler Jr, MD, H. Cody Meissner, MD, Alfred Bartolucci, PhD, Penelope Dennehy, MD). We thank the NICU nurses and physicians at each center for their support and enthusiasm for this project and the study teams for their invaluable contributions to recruitment, data collection, and data quality: Ginkohny Cummings, PNP, Kimberly Wilhelmi, RN, Aly Kwon, and Brenda Dorsey, RN, BSN, MS (University of Maryland School of Medicine); Shanda Phillips, RN, BSN, Deborah Myers, Natalia Jimenez, PhD, Roberta Winfrey, Mary Jones, RN, Debbie Hunter, MSN, Julie Anderson, RN, Jennifer Nixon, MBA, Nicole Soper, MLS, and Lauren Jones (Vanderbilt University Medical Center); Melissa Bowles Hawkins, MSN, RN, Linda Breuer, LPN, and Sabrina Dipiazza, RN, BSN, MA (Cardinal Glennon Children’s Hospital and Saint Louis University); Megan Bledsoe, MSc, Shannon Clark, MPH, Georgann Meredith, RN, BSN, Nancy A. Neilan, MS, MT, Jami Penny, LPN, Karen Snyder, CAN, Joanne Thurber, RN, J. Christopher Day, MD, Douglas Swanson, MD, Jennifer Schuster, MD, MSCI, and Denise Smith, RN, NNP-BC (Children’s Mercy Hospital); and Nancy Back, Cara Kohlrieser, Kristin Buschle, Michelle Kroeger, and Susan Parker (Cincinnati Children’s Hospital Medical Center). For assistance in specimen processing and cultures at the clinical and research laboratories at each center, we thank LiChang Zhao, PhD (University of Maryland School of Medicine), Drs Robert Jerris and Lars Westblade (Children’s Healthcare of Atlanta), Raymond Scott Duncan, PhD, and Rangaraj Selvarangan, BVSc, PhD (Children’s Mercy Hospital), Joel Mortenson, PhD (Cincinnati Children’s Hospital Medical Center), and Kathy Lottenbach, MS (Saint Louis University).
Glossary
- AE
adverse event
- CI
confidence interval
- ITT
intent-to-treat
- mITT
modified intent-to-treat
- mITT-8
modified intent-to-treat analysis of decolonization on day 8 (primary decolonization)
- mITT-22
modified intent-to-treat analysis of decolonization on day 22 (persistent decolonization)
- MRSA
methicillin-resistant Staphylococcus aureus
- MSSA
methicillin-susceptible Staphylococcus aureus
- NEC
necrotizing enterocolitis
- NUP
nasal, periumbilical, and perianal
- SA
Staphylococcus aureus
Footnotes
Dr Kotloff conceptualized the study design, oversaw the project, designed the data collection instruments, assisted in the development of the data analysis plan, drafted the initial manuscript, and revised the manuscript; Dr Shirley assisted with the design of the study and the data collection instruments and reviewed and revised the manuscript; Drs Creech and Thomsen directed the laboratory where bacterial isolates were confirmed for identity and tested for susceptibility, assisted with the study design, coordinated and supervised the data collection, and reviewed and edited the manuscript; Mr Oler and Dr Conrad assisted with the design of the data collection instruments and the development of the data analysis plan, conducted statistical analyses, and reviewed and edited the manuscript; Dr Stephens assisted with the design of the study and reviewed and revised the manuscript; Drs Frey, Harrison, Staat, Anderson, Dulkerian, Al-Hosni, Pahud, Bernstein, Yi, Petrikin, and Haberman and Ms Stephens assisted with the study design, coordinated and supervised the data collection, and reviewed and edited the manuscript; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
This trial has been registered at www.clinicaltrials.gov (identifier NCT01827358).
FINANCIAL DISCLOSURE: Dr Conrad’s company is a subcontractor for the sponsor of the study (Division of Microbiology and Infectious Diseases), providing data management and statistical support; the other authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by funds from the National Institute of Allergy and Infectious Diseases, the National Institutes of Health, and the US Department of Health and Human Services under contracts HHSN272200800057C (University of Maryland, Baltimore); HHSN27220080000C (Vanderbilt University); HHSN272200800003C (Saint Louis University); HHSN27220800008C (University of Iowa); HHSN272200800008C, Option 8A-09-0065-CMH, COA 3, and HHSN272200800006C (Cincinnati Children’s Hospital); HHSN272200800005C (Emory University); and HHSN272200800013C (Emmes Corporation). Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: Dr Kotloff reports funds to conduct research on rotavirus vaccine in Africa from Merck, Sharpe, and Dohme; Dr Creech reports grant funding and personal consultation fees from GlaxoSmithKline and Pfizer for staphylococcal vaccine development; Dr Harrison reports grants from Merck and GlaxoSmithKline and consultation fees from Pfizer; Dr Pahud reports grant funding from Pfizer and consultation fees from Pfizer, Sanofi, and Sequiris; Dr Bernstein reports consultation fees from Merck and Takeda; Dr Anderson reports funds to conduct clinical research from MedImmune, Regeneron, Pfizer, and Novavax and personal fees from AbbVie; the other authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Vergnano S, Menson E, Smith Z, et al. Characteristics of invasive Staphylococcus aureus in United Kingdom neonatal units [published correction appears in Pediatr Infect Dis J. 2013;32(5):e226]. Pediatr Infect Dis J. 2011;30(10):850–854 [DOI] [PubMed] [Google Scholar]
- 2.Carey AJ, Duchon J, Della-Latta P, Saiman L. The epidemiology of methicillin-susceptible and methicillin-resistant Staphylococcus aureus in a neonatal intensive care unit, 2000-2007. J Perinatol. 2010;30(2):135–139 [DOI] [PubMed] [Google Scholar]
- 3.Greenberg RG, Kandefer S, Do BT, et al. ; Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network . Late-onset sepsis in extremely premature infants: 2000-2011. Pediatr Infect Dis J. 2017;36(8):774–779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shane AL, Hansen NI, Stoll BJ, et al. ; Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network . Methicillin-resistant and susceptible Staphylococcus aureus bacteremia and meningitis in preterm infants. Pediatrics. 2012;129(4). Available at: www.pediatrics.org/cgi/content/full/129/4/e914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stoll BJ, Hansen NI, Adams-Chapman I, et al. ; National Institute of Child Health and Human Development Neonatal Research Network . Neurodevelopmental and growth impairment among extremely low-birth-weight infants with neonatal infection. JAMA. 2004;292(19):2357–2365 [DOI] [PubMed] [Google Scholar]
- 6.Stoll BJ, Hansen N, Fanaroff AA, et al. Late-onset sepsis in very low birth weight neonates: the experience of the NICHD Neonatal Research Network. Pediatrics. 2002;110(2, pt 1):285–291 [DOI] [PubMed] [Google Scholar]
- 7.Huang YC, Chou YH, Su LH, Lien RI, Lin TY. Methicillin-resistant Staphylococcus aureus colonization and its association with infection among infants hospitalized in neonatal intensive care units. Pediatrics. 2006;118(2):469–474 [DOI] [PubMed] [Google Scholar]
- 8.Delaney HM, Wang E, Melish M. Comprehensive strategy including prophylactic mupirocin to reduce Staphylococcus aureus colonization and infection in high-risk neonates. J Perinatol. 2013;33(4):313–318 [DOI] [PubMed] [Google Scholar]
- 9.Huang SS, Septimus E, Kleinman K, et al. ; CDC Prevention Epicenters Program; AHRQ DECIDE Network and Healthcare-Associated Infections Program . Targeted versus universal decolonization to prevent ICU infection [published correction appears in N Engl J Med. 2013;369(6):587 and 2014;370(9):886]. N Engl J Med. 2013;368(24):2255–2265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ammerlaan HS, Kluytmans JA, Berkhout H, et al. ; MRSA Eradication Study Group . Eradication of carriage with methicillin-resistant Staphylococcus aureus: effectiveness of a national guideline. J Antimicrob Chemother. 2011;66(10):2409–2417 [DOI] [PubMed] [Google Scholar]
- 11.Tzermpos F, Kanni T, Tzanetakou V, et al. An algorithm for the management of Staphylococcus aureus carriage within patients with recurrent staphylococcal skin infections. J Infect Chemother. 2013;19(5):806–811 [DOI] [PubMed] [Google Scholar]
- 12.Kaplan SL. Community-acquired methicillin-resistant Staphylococcus aureus infections in children. Semin Pediatr Infect Dis. 2006;17(3):113–119 [DOI] [PubMed] [Google Scholar]
- 13.Agency for HealthCare Research and Quality; The REDUCE MRSA Trial Working Group Universal ICU decolonization: an enhanced protocol. 2013. Available at: https://www.ahrq.gov/professionals/systems/hospital/universal_icu_decolonization/index.html. Accessed September 1, 2017
- 14.Milstone AM, Song X, Coffin S, Elward A; Society for Healthcare Epidemiology of America’s Pediatric Special Interest Group . Identification and eradication of methicillin-resistant Staphylococcus aureus colonization in the neonatal intensive care unit: results of a national survey. Infect Control Hosp Epidemiol. 2010;31(7):766–768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nelson MU, Bizzarro MJ, Dembry LM, Baltimore RS, Gallagher PG. One size does not fit all: why universal decolonization strategies to prevent methicillin-resistant Staphylococcus aureus colonization and infection in adult intensive care units may be inappropriate for neonatal intensive care units. J Perinatol. 2014;34(9):653–655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Popoola VO, Milstone AM. Decolonization to prevent Staphylococcus aureus transmission and infections in the neonatal intensive care unit. J Perinatol. 2014;34(11):805–810 [DOI] [PubMed] [Google Scholar]
- 17.Neu J, Walker WA. Necrotizing enterocolitis. N Engl J Med. 2011;364(3):255–264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting [published correction appears in Am J Infect Control. 2008;36(9):655]. Am J Infect Control. 2008;36(5):309–332 [DOI] [PubMed] [Google Scholar]
- 19.Clinical and Laboratory Standards Institute Performance Standards for Antimicrobial Susceptibility Testing. 26th ed. Wayne, PA: Clinical and Laboratory Standards Institute; 2016 [Google Scholar]
- 20.Kondo Y, Ito T, Ma XX, et al. Combination of multiplex PCRs for staphylococcal cassette chromosome mec type assignment: rapid identification system for mec, ccr, and major differences in junkyard regions. Antimicrob Agents Chemother. 2007;51(1):264–274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ludbrook J. Multiple inferences using confidence intervals. Clin Exp Pharmacol Physiol. 2000;27(3):212–215 [DOI] [PubMed] [Google Scholar]
- 22.Miettinen O, Nurminen M. Comparative analysis of two rates. Stat Med. 1985;4(2):213–226 [DOI] [PubMed] [Google Scholar]
- 23.Farrington CP, Manning G. Test statistics and sample size formulae for comparative binomial trials with null hypothesis of non-zero risk difference or non-unity relative risk. Stat Med. 1990;9(12):1447–1454 [DOI] [PubMed] [Google Scholar]
- 24.Hitomi S, Kubota M, Mori N, et al. Control of a methicillin-resistant Staphylococcus aureus outbreak in a neonatal intensive care unit by unselective use of nasal mupirocin ointment. J Hosp Infect. 2000;46(2):123–129 [DOI] [PubMed] [Google Scholar]
- 25.Lally RT, Lanz E, Schrock CG. Rapid control of an outbreak of Staphylococcus aureus on a neonatal intensive care department using standard infection control practices and nasal mupirocin. Am J Infect Control. 2004;32(1):44–47 [DOI] [PubMed] [Google Scholar]
- 26.Popoola VO, Carroll KC, Ross T, Reich NG, Perl TM, Milstone AM. Impact of colonization pressure and strain type on methicillin-resistant Staphylococcus aureus transmission in children. Clin Infect Dis. 2013;57(10):1458–1460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Neri I, Ravaioli GM, Faldella G, Capretti MG, Arcuri S, Patrizi A. Chlorhexidine-induced chemical burns in very low birth weight infants. J Pediatr. 2017;191:262–265.e2 [DOI] [PubMed] [Google Scholar]
- 28.Pierce R, Lessler J, Popoola VO, Milstone AM. Meticillin-resistant Staphylococcus aureus (MRSA) acquisition risk in an endemic neonatal intensive care unit with an active surveillance culture and decolonization programme. J Hosp Infect. 2017;95(1):91–97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Popoola VO, Budd A, Wittig SM, et al. Methicillin-resistant Staphylococcus aureus transmission and infections in a neonatal intensive care unit despite active surveillance cultures and decolonization: challenges for infection prevention. Infect Control Hosp Epidemiol. 2014;35(4):412–418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Huang YC, Lien RI, Su LH, Chou YH, Lin TY. Successful control of methicillin-resistant Staphylococcus aureus in endemic neonatal intensive care units–a 7-year campaign. PLoS One. 2011;6(8):e23001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pierce R, Bryant K, Elward A, Lessler J, Milstone AM. Bacterial infections in neonates following mupirocin-based MRSA decolonization: a multicenter cohort study. Infect Control Hosp Epidemiol. 2017;38(8):930–936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Climo MW, Yokoe DS, Warren DK, et al. Effect of daily chlorhexidine bathing on hospital-acquired infection. N Engl J Med. 2013;368(6):533–542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Suwantarat N, Carroll KC, Tekle T, Ross T, Popoola VO, Milstone AM. Low prevalence of mupirocin resistance among hospital-acquired methicillin-resistant Staphylococcus aureus isolates in a neonatal intensive care unit with an active surveillance cultures and decolonization program. Infect Control Hosp Epidemiol. 2015;36(2):232–234 [DOI] [PubMed] [Google Scholar]
- 34.Peterson LR, Samia NI, Skinner AM, Chopra A, Smith B. Antimicrobial stewardship lessons from mupirocin use and resistance in methicillin-resitant Staphylococcus aureus. Open Forum Infect Dis. 2017;4(2):ofx093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Conner JM, Soll RF, Edwards WH. Topical ointment for preventing infection in preterm infants. Cochrane Database Syst Rev. 2004;(1):CD001150. [DOI] [PubMed] [Google Scholar]
- 36.Edwards WH, Conner JM, Soll RF; Vermont Oxford Network Neonatal Skin Care Study Group . The effect of prophylactic ointment therapy on nosocomial sepsis rates and skin integrity in infants with birth weights of 501 to 1000 g. Pediatrics. 2004;113(5):1195–1203 [DOI] [PubMed] [Google Scholar]
- 37.AlKharfy T, Ba-Abbad R, Hadi A, AlFaleh K. Use of topical petroleum jelly for prevention of sepsis in very low-birthweight infants: a prospective, randomised controlled trial. Paediatr Int Child Health. 2014;34(3):194–197 [DOI] [PubMed] [Google Scholar]
- 38.Poovelikunnel TT, Budri PE, Shore AC, Coleman DC, Humphreys H, Fitzgerald-Hughes D. Molecular characterization of nasal methicillin-resistant Staphylococcus aureus isolates showing increasing prevalence of mupirocin resistance and associated multidrug resistance following attempted decolonization. Antimicrob Agents Chemother. 2018;62(9):e00819-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cho OH, Baek EH, Bak MH, et al. The effect of targeted decolonization on methicillin-resistant Staphylococcus aureus colonization or infection in a surgical intensive care unit. Am J Infect Control. 2016;44(5):533–538 [DOI] [PubMed] [Google Scholar]