We examine tobacco product harm perceptions in youth at wave 1 of a national longitudinal study and evaluate new tobacco product use at wave 2.
Abstract
Video Abstract
BACKGROUND:
Researchers in several studies have examined correlations between tobacco harm perceptions and tobacco use in youth, but none have prospectively addressed the association between harm perceptions and subsequent new use across multiple noncigarette products.
METHODS:
Product-specific absolute and relative harm perceptions for cigarettes, electronic cigarettes (e-cigarettes), cigars, pipes, hookah, and smokeless tobacco were collected at wave 1 (W1) (2013–2014) among youth in the nationally representative US Population Assessment of Tobacco and Health Study (12–17 years of age; n = 10 081). At wave 2 (W2) (2014–2015), product-specific new use was calculated. Adjusted relative risks were used to estimate if harm perceptions at W1 predicted W2 new tobacco use.
RESULTS:
The proportion of youth who endorsed “a lot of harm” was highest for cigarettes (84.8%) and lowest for e-cigarettes (26.6%); the proportion of youth who thought products were “more harmful” than cigarettes was highest for cigars (30.6%) and lowest for e-cigarettes (5.1%). Among youth who had not used those products at W1, product-specific new use at W2 ranged from 9.1% (e-cigarettes) to 0.6% (pipes). Youth who believed that noncombustible tobacco products posed “no or little harm” at W1 were more likely to have tried those products at W2 (P < .05). Youth who viewed e-cigarettes, hookah, and smokeless tobacco as “less harmful” than cigarettes at W1 were more likely to try those tobacco products at W2 (P < .05).
CONCLUSIONS:
Low harm perceptions of noncigarette tobacco products predict new use of these products by youth within the next year. Targeting product-specific harm perceptions may prevent new tobacco use among youth.
What’s Known on This Subject:
Several studies have found an inverse relationship between tobacco harm perceptions and tobacco use in youth, but there is little known about whether youth harm perceptions of these products affect their subsequent use.
What This Study Adds:
Low levels of absolute and relative harm perceptions for electronic cigarettes, hookah, and smokeless tobacco are positively associated with the new use of these products within the next year by US youth. Targeting product-specific harm perceptions may prevent new tobacco use in youth.
Although the prevalence of US youth cigarette use has been declining in since 2011, the use of multiple tobacco products and electronic cigarette (e-cigarette) use increased through 2015, with some recent decreases seen in 2016 and 2017.1–4 Previous research in youth has revealed an inverse relationship between harm perceptions and cigarette experimentation, with lower harm perceptions of specific tobacco products being associated with a higher prevalence of use of those products.5,6 There is concern that youth may initiate noncigarette tobacco products (ie, e-cigarettes, cigars, pipes, hookah, and smokeless tobacco) because they perceive these products as less harmful than cigarettes.7 In addition, there was been a decline in the perceived risk of cigarette smoking in the general US population between 2006 and 2015, with youth reporting lower perceived risk of smoking than young adults aged 18 to 25 years or adults aged ≥26 years.8 In general, youth know that cigarette smoking is harmful but are unrealistically optimistic about or misunderstand their own risk.9 Findings suggest this is also likely true for noncigarette tobacco products.10,11
Harm perceptions are typically measured in 2 different ways: absolute and relative harm. In the extant literature, researchers have most often examined harm perceptions associated with the use of noncigarette tobacco products in comparison with cigarettes (relative harm) and have only occasionally examined them independently of cigarettes (absolute harm).12,13 Measures of relative perceived harm are used to provide an anchor for a comparison of the harms of novel or less prevalent tobacco products given the high awareness of the harms of smoking cigarettes.14 Absolute perceived harm is informative but has not often been explored for noncigarette tobacco products because relative perceived harm has become the standard for harm perception research.15 Because the lay public is often misinformed when it comes to the relative harm of tobacco products,16 especially the harms of novel products,5,17 measuring both absolute and relative tobacco product harm perceptions might provide a more effective way of assessing the acceptability of and susceptibility to using new tobacco products.12,18
Risk perceptions of tobacco products have been correlated with the use of those products in youth,6,12,19 young adults,5,20,21 and adults.15,22 Many of these existing studies are cross-sectional in nature, use convenience samples, or have low response rates. Two repeated cross-sectional studies in youth and adults, respectively, examined the relationship between smokeless tobacco22 and e-cigarette19 harm perceptions and subsequent use over time. To our knowledge, no previous studies have prospectively examined relationships between product harm perceptions and subsequent new use of multiple tobacco products in US youth. In the current study, we use nationally representative longitudinal data from wave 1 (W1) and wave 2 (W2) of the Population Assessment of Tobacco and Health (PATH) Study23 to (1) describe tobacco product harm perception patterns among youth who had not used the products at W1 and (2) assess whether tobacco product harm perceptions at W1 are associated with the new use of these products between W1 and W2. Our hypothesis was that absolute and relative tobacco product harm perceptions at W1 would be inversely related to the new use of that tobacco product by W2.
Methods
Study Design and Participants
The PATH Study is a nationally representative longitudinal cohort survey of adult and youth residents of the United States ≥12 years old who are not institutionalized. Participants are recruited by using address-based, area-probability sampling with an in-person household screener that is used to select youth aged 12 to 17 years, their parents and/or guardians, and adults for Audio Computer-Assisted Self-Interviews. Bilingual interviewers and Spanish versions of the questionnaires and study materials were available. Weighted procedures were adjusted for sibling clustering and oversampling of adult tobacco users, young adults, and non-Hispanic African American adults.
The current study was focused on youth from the PATH study at W1 (September 2013–December 2014; n = 13 651) who completed a W2 interview (October 2014–October 2015; n = 11 996) and did not reach age 18 years by W2 (n = 10 081). The weighted completion rate for youth at W1 was 78.4%, and the weighted retention rate for youth at W2 was 88.4%.24 Further details about the PATH Study design and institutional review board–approved protocols are available elsewhere.25
Measures
Absolute and Relative Harm Perceptions
Tobacco products of interest were cigarettes, e-cigarettes, cigars (ie, traditional cigars, cigarillos, and filtered cigars), pipes, hookah, and smokeless tobacco. Questionnaires were used to assess harm perceptions for these products by asking about absolute and relative harm. Only youth who had seen or heard of the product were asked these questions. The absolute harm question asked, “How much do you think people harm themselves when they smoke or use [product]?” Youth could answer “no harm,” “a little harm,” “some harm,” or “a lot of harm.” Due to the low prevalence of youth who answered “no harm” across all tobacco products, “a little harm” was combined with “no harm” for 3 categories: “no or little harm,” “some harm,” and “a lot of harm.” For relative harm, the question was, “Is smoking or using [product] less harmful, about the same, or more harmful than smoking cigarettes?” Youth could answer “less harmful,” “about the same,” or “more harmful” than smoking cigarettes.
Tobacco Product New Use
The outcomes were new tobacco product use at W2 among W1 youth who had never used the tobacco product of interest. All tobacco products were considered separately (ie, cigarettes, e-cigarettes, cigars, pipes, hookah, and smokeless tobacco). For cigarettes, for example, the outcome of interest was new cigarette use at W2 among youth at W1 who had never used cigarettes. Namely, at W1, we focused on respondents who answered “no” to the question, “Have you ever smoked cigarettes, even 1 or 2 puffs?” Youth were asked similar questions for each tobacco product. At W2, youth were then asked the same question, and we examined differences between those who remained “never” users and those with new use (“ever” users). The subset of respondents identified as “never-to-ever” users for each product were classified as new users of that product between W1 and W2.
Background Characteristics
In youth interviews, standard sociodemographic information was collected, including age (12–14 years old and 15–17 years old), sex (male or female), race and/or ethnicity (non-Hispanic white, non-Hispanic African American, non-Hispanic other [Asian American, American Indian and/or Alaskan native, Pacific Islander, and those who reported >1 race], and Hispanic), education (sixth grade, seventh grade, eighth grade, ninth grade, 10th grade, 11th grade, and other [not enrolled, homeschooled, school not graded, 12th grade, and college or vocational school]), and region of the United States (Northeast, Midwest, South, and West). Parental education was used as a proxy for socioeconomic status. In parent and/or guardian interviews, participants denoted their highest level of education: less than high school, high school graduate, some college, and college graduate (4 years). In our study, we also considered youth ever substance use for alcohol and any other tobacco use at W1 (eg, e-cigarette use for W1 never-cigarette smokers). For both substances, ever use was defined and dichotomized as lifetime use or none.
Analysis
We first examined W1 harm perceptions by focusing on the absolute and relative response distribution. In subsequent analysis steps, we calculated W2 new use for each tobacco product. New use was calculated as the weighted number of youth who tried using each tobacco product between W1 and W2 among youth who never used that product but had heard of the product at W1 and completed a W2 interview. Our final analysis steps involved using binomial generalized linear models (with a log link) to estimate relative risks (RRs) of W2 tobacco product initiation, in which we linked absolute and relative harm perceptions to the new use of each of the tobacco products. Unadjusted models included either W1 absolute or relative harm perceptions as explanatory variables (2 separate models for each tobacco product). In adjusted models, we added W1 sex, age, race and/or ethnicity, region of the United States, parental education, and other alcohol and/or tobacco use. The sociodemographic covariates (ie, sex, age, race and/or ethnicity, region of the United States, and parental education) were included to account for variation in tobacco product use across subgroups and because they may confound the relationship between harm perceptions and new tobacco product use. Any W1 tobacco use other than the focal product as well as W1 alcohol use was included in adjusted models because they were presumed to impact whether youth might begin using other products.
All estimates were weighted to represent the US youth population. Confidence intervals (CIs) were calculated by using the balanced repeated replication method with Fay’s adjustment and replicate weights.25 Analyses were performed by using svy commands in Stata 14 (Stata Corp, College Station, TX).26 In this work, we focus on 95% CIs; P values are provided to aid in interpretation.
Results
Background Characteristics and Harm Perceptions
Of the 10 081 youth who completed both a W1 and W2 interview, 61.4% were 12 to 14 years old, approximately half were male (51.5%), and 16.9% had ever used tobacco (Table 1). Approximately one-third of youth had ever drank alcohol at W1 (33.5%; Table 1).
TABLE 1.
Demographics and Other Characteristics of W1 Youth Who Completed a W2 Interview (n = 10 081)
| na | %b | 95% CIb | |
|---|---|---|---|
| Age, yc | |||
| 12–14 | 6217 | 61.4 | 61.0–61.8 |
| 15–17 | 3864 | 38.6 | 38.2–39.0 |
| Sex | |||
| Male | 5181 | 51.5 | 51.1–51.9 |
| Female | 4900 | 48.5 | 48.1–48.9 |
| Race and/or ethnicity | |||
| White, non-Hispanic | 4844 | 54.6 | 54.1–55.1 |
| African American, non-Hispanic | 1371 | 13.7 | 13.4–14.1 |
| Other, non-Hispanicd | 929 | 9.2 | 8.9–9.5 |
| Hispanic | 2937 | 22.5 | 22.2–22.9 |
| Education (grade in school) | |||
| Sixth | 694 | 6.8 | 6.3–7.4 |
| Seventh | 1914 | 19.0 | 18.4–19.6 |
| Eighth | 2009 | 20.0 | 19.3–20.7 |
| Ninth | 2049 | 20.3 | 19.6–20.9 |
| 10th | 1857 | 18.8 | 18.1–19.4 |
| 11th | 1153 | 11.5 | 10.9–12.2 |
| Othere | 377 | 3.6 | 3.2–4.0 |
| Census region | |||
| Northeast | 1439 | 16.1 | 15.7–16.5 |
| Midwest | 2233 | 22.4 | 22.1–22.6 |
| South | 3794 | 37.4 | 36.9–37.8 |
| West | 2615 | 24.2 | 23.8–24.5 |
| Ever substance use | |||
| Alcohol | 3297 | 33.5 | 32.0–35.0 |
| Tobacco | 1665 | 16.9 | 16.0–17.9 |
From the US PATH Study (2013–2014).
Unweighted sample size (numbers may not sum to the total because of missing data).
Percentages and 95% CIs are weighted to represent the US youth population at W1.
Specific ages were not available for PATH Study youth.
Includes Asian Americans, American Indians and/or Alaskan natives, Pacific Islanders, and those who reported >1 race.
Includes those who were not enrolled, who were homeschooled, whose schools were not graded, who were in 12th grade, and who were in college or vocational school.
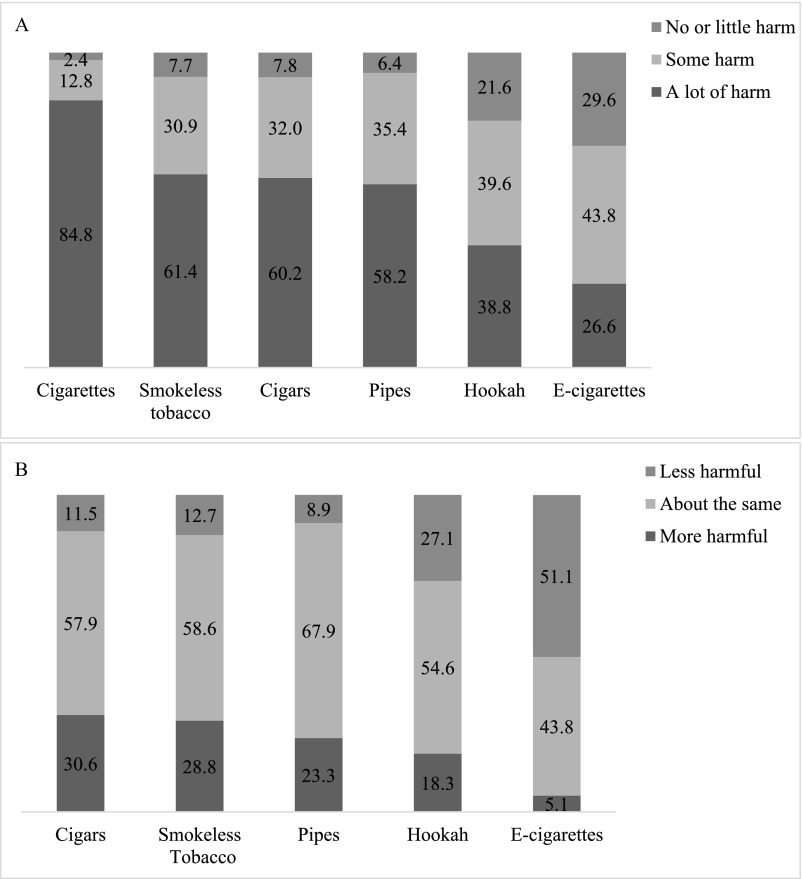
W1 absolute harm perceptions for youth who endorsed “a lot of harm” were highest for cigarettes (84.8%), lowest for e-cigarettes (26.6%), and similar for cigars (60.2%), pipes (58.2%), and smokeless tobacco (61.4%; Fig 1A). Relative harm perceptions for youth who endorsed a “more harmful” perception when other tobacco products were compared with cigarettes were highest for cigars (30.6%), followed by smokeless tobacco (28.8%), pipes (23.3%), and hookah (18.3%). They were lowest for e-cigarettes at 5.1% (Fig 1B).
FIGURE 1.
Weighted absolute and relative tobacco product harm perception percentages among youth at W1 who never used that product (US PATH Study, 2013–2014). The sample included youth who completed a W2 interview. All estimates are percentages and have been weighted to represent the US youth population at W1 who had seen or heard of the product. A, Absolute harm. B, Relative harm to cigarettes.
New Tobacco Product Use
Among youth who had never used but had heard of each product at W1, product-specific new use at W2 ranged from 9.1% for e-cigarettes to 0.6% for pipes (Table 2). W2 new use was similar for cigarettes, cigars, and hookah at 3.8%, 3.0%, and 3.1%, respectively, and 95% CIs for the use of those products did not overlap with those for new use of e-cigarettes, which was higher, nor new use of smokeless tobacco or pipes, which were lower (P < .05).
TABLE 2.
New Tobacco Product Use at W2 Among Youth Who Never Used That Product at W1
| na | %b | 95% CIb | |
|---|---|---|---|
| E-cigarettes | 819 | 9.1 | 8.3–10.0 |
| Cigarettes | 338 | 3.8 | 3.4–4.2 |
| Hookah | 290 | 3.1 | 2.7–3.5 |
| Cigars | 269 | 3.0 | 2.6–3.4 |
| Smokeless tobacco | 137 | 1.6 | 1.3–1.9 |
| Pipes | 67 | 0.6 | 0.5–0.8 |
From the US PATH Study (2014–2015).
Unweighted sample size.
Percentages and CIs are weighted to represent the US youth population at W2.
Absolute Harm Perceptions and New Use
In the multivariable analyses presented in Table 3, the unadjusted RR for the relationship between absolute harm perceptions and new use varied across tobacco products, with generally higher estimates seen in those reporting no or little harm or some harm compared with a lot of harm. Adjusted estimates reveal that youth who believed that e-cigarettes (adjusted relative risk [ARR]: 2.2; 95% CI: 1.7–2.8), cigars (ARR: 2.7; 95% CI: 1.8–4.0), pipes (ARR: 2.8; 95% CI: 1.2–6.6), hookah (ARR: 2.7; 95% CI: 2.0–3.8), and smokeless tobacco (ARR: 2.8; 95% CI: 1.7–4.5) posed no or little harm at W1 were 2 to 3 times more likely to have tried those products at W2 than youth who believed that these products posed a lot of harm (P < .05; Table 3). Conventional cigarettes were an exception. After adjustment, youth who thought there was some harm in cigarette smoking at W1 were approximately twice as likely to start smoking at W2 compared with youth who thought there was a lot of harm in smoking cigarettes (ARR: 1.9; 95% CI: 1.4–2.4). However, there was not a significant relationship between those who endorsed no or little harm versus a lot of harm in beginning to smoke cigarettes (Table 3).
TABLE 3.
Generalized Linear Models Used to Link Absolute Harm Perceptions of Tobacco Products Among Youth at W1 to New Use at W2
| RRa | 95% CIa | ARRa,b | 95% CIa | |
|---|---|---|---|---|
| Cigarettes | ||||
| No or little harm | 1.5 | 0.7–3.0 | 1.5 | 0.8–3.0 |
| Some harm | 2.4c | 1.9–3.1 | 1.9c | 1.4–2.4 |
| A lot of harm | 1.0 | — | 1.0 | — |
| E-cigarettes | ||||
| No or little harm | 3.0c | 2.4–3.8 | 2.2c | 1.7–2.8 |
| Some harm | 1.6c | 1.3–2.1 | 1.3c | 1.0–1.7 |
| A lot of harm | 1.0 | — | 1.0 | — |
| Cigars overall | ||||
| No or little harm | 3.7c | 2.5–5.5 | 2.6c | 1.8–4.0 |
| Some harm | 1.6c | 1.2–2.2 | 1.3 | 0.9–1.8 |
| A lot of harm | 1.0 | — | 1.0 | — |
| Pipes | ||||
| No or little harm | 4.2c | 1.8–9.5 | 2.8c | 1.2–6.6 |
| Some harm | 1.4 | 0.7–2.9 | 1.1 | 0.6–2.2 |
| A lot of harm | 1.0 | — | 1.0 | — |
| Hookah | ||||
| No or little harm | 3.6c | 2.6–5.0 | 2.7c | 2.0–3.8 |
| Some harm | 1.5c | 1.0–2.1 | 1.2 | 0.8–1.7 |
| A lot of harm | 1.0 | — | 1.0 | — |
| Smokeless tobacco | ||||
| No or little harm | 3.2c | 1.9–5.4 | 2.8c | 1.7–4.5 |
| Some harm | 1.5 | 0.9–2.4 | 1.3 | 0.8–2.2 |
| A lot of harm | 1.0 | — | 1.0 | — |
From the US PATH Study (2013–2015). The sample included youth who completed a W2 interview and had never used each product at W1 but had heard of the product, respectively. —, not applicable.
Estimates and 95% CIs are weighted to represent the US youth population at W2.
ARRs are from generalized linear models (binomial family with log link) that are controlled for age, sex, race, region, parental education, ever alcohol use, and ever tobacco use at W1. In adjusted models for e-cigarettes, cigars, and smokeless tobacco, a generalized linear model (Poisson family with log link) was used.
Statistically significant at the α = .05 level.
Relative Harm Perceptions and New Use
The results in Table 4 show that youth who perceived e-cigarettes (ARR: 1.6; 95% CI: 1.2–2.2), hookah (ARR: 1.9; 95% CI: 1.2–3.1), and smokeless tobacco (ARR: 2.4; 95% CI: 1.4–4.2) to be less harmful than cigarettes at W1 were approximately twice as likely to try those tobacco products at W2 compared with youth who thought that they were more harmful than or equally as harmful as cigarettes (P < .05; Table 4). This pattern was not found for cigars or pipes (P > .05; Table 4). Unadjusted estimates were similar to adjusted estimates; RR estimates for relative harm perceptions were slightly smaller than those for absolute harm perceptions (Table 3).
TABLE 4.
Generalized Linear Models Used to Link Relative Harm Perceptions of Tobacco Products Among Youth at W1 to New Use at W2
| RRa | 95% CIa | ARRa,b | 95% CIa | |
|---|---|---|---|---|
| E-cigarettes | ||||
| Less harmful | 2.0c | 1.4–2.8 | 1.6c | 1.2–2.2 |
| About the same | 1.2 | 0.9–1.8 | 1.1 | 0.8–1.6 |
| More harmful | 1.0 | — | 1.0 | — |
| Cigars overall | ||||
| Less harmful | 1.7c | 1.1–2.8 | 1.5 | 1.0–2.4 |
| About the same | 0.8 | 0.6–1.1 | 0.9 | 0.6–1.2 |
| More harmful | 1.0 | — | 1.0 | — |
| Pipes | ||||
| Less harmful | 1.9 | 0.8–4.4 | 2.1 | 0.9–5.0 |
| About the same | 0.8 | 0.4–1.7 | 0.8 | 0.4–1.7 |
| More harmful | 1.0 | — | 1.0 | — |
| Hookah | ||||
| Less harmful | 2.1c | 1.3–3.4 | 1.9c | 1.2–3.1 |
| About the same | 1.0 | 0.7–1.6 | 1.0 | 0.6–1.6 |
| More harmful | 1.0 | — | 1.0 | — |
| Smokeless tobacco | ||||
| Less harmful | 2.2c | 1.2–4.1 | 2.3c | 1.3–4.0 |
| About the same | 1.1 | 0.6–1.8 | 1.3 | 0.8–2.1 |
| More harmful | 1.0 | — | 1.0 | — |
From the US PATH Study (2013–2015). The sample included youth who completed a W2 interview and had never used each product at W1 but had heard of the product, respectively. —, not applicable.
Estimates and 95% CIs are weighted to represent the US youth population at W2.
ARRs are from generalized linear models (binomial family with log link) that are controlled for age, sex, race, region, parent education, ever alcohol use, and ever use of tobacco products other than the focal product at W1. In adjusted models for e-cigarettes, cigars, and smokeless tobacco, a generalized linear model (Poisson family with log link) was used.
Statistically significant at the α = .05 level.
For both absolute and relative harm models, associations decreased in magnitude with adjustment for sex, age, race and/or ethnicity, US region, parental education, and W1 ever alcohol and/or tobacco use (Tables 3 and 4). In all adjusted models that included absolute or relative harm perceptions and other covariates, ever tobacco use was inversely associated with new tobacco product use (P < .001; data not shown). The relationship between ever alcohol use and new tobacco product use was not consistent across products.
Discussion
Findings from this study highlight that low harm perceptions of noncigarette products predict the subsequent use of those products in youth. Specifically, in this nationally representative, longitudinal study, low absolute and relative harm perceptions of e-cigarettes, hookah, and smokeless tobacco predicted the new use of those products in youth within the next year when controlling for potential covariates, including ever use of other tobacco products. Similarly, never-cigarette smokers who identified cigarettes as having some compared with a lot of harm were nearly twice as likely to report new cigarette use at W2. There was no significant relationship between youth who endorsed no or little versus a lot of harm in cigarettes, which is likely because youth are generally aware of cigarette harms, and only a small number of individuals reported no or little harm in cigarettes.
Although our findings are consistent with those in previous cross-sectional studies that reveal associations between low relative harm perceptions and experimentation with e-cigarettes, cigars, pipes, hookah, and smokeless tobacco at follow-up,20,21,27,28 they provide novel prospective evidence of this important relationship between harm perceptions and new use across multiple tobacco products in a nationally representative sample. They demonstrate a consistent longitudinal relationship between harm perceptions and new use across multiple noncigarette products despite variation in perceptions of the addictiveness and harms of various tobacco products in young people.5,17
Cigarette advertising has been documented as a reason for smoking initiation in youth.29 Findings from this study suggest that advertising or other messages that effectively lower harm perceptions of noncigarette products may induce new use of those products in youth. This is of particular importance to tobacco regulatory policy in the United States, where the Food and Drug Administration (FDA) is required to evaluate its efforts using a public health standard that balances the potential harms and benefits of a policy at the population level. In implementing comprehensive nicotine regulation, the FDA will need to ensure that public education efforts and reduced risk or reduced exposure messages on products do not inadvertently promote new product use in young people.
In this study, we extend the findings from other work on tobacco product relative perceived harm17,21 using longitudinal data from a nationally representative sample to assess absolute harm perceptions in addition to relative harm perceptions. By measuring both absolute and relative tobacco product harm perceptions among youth, our estimates show new evidence of the similarity between the measures, and we suggest that only 1 harm perception type may be sufficient in future population surveys. We document absolute harm perceptions of cigarette and noncigarette products in youth, which were lower than reported by adult participants in the National Cancer Institute’s Health Information National Trends Survey.15 Differences in harm perceptions among youth compared with adults are expected because judgments of risk increase with age,30 and this study provides baseline estimates that can be compared over time, both within the PATH Study and in other national samples of youth.
Factors influencing new use of tobacco products are important targets for future intervention, both at the individual and population levels. This study highlights that lower product-specific harm perceptions are positively associated with the new use of e-cigarettes, hookah, and smokeless tobacco products. Findings for pipes and cigars were less consistent. It is also notable that the new use of e-cigarettes was >2 times that of conventional cigarettes and other tobacco products. These observations underscore the need for education and communication efforts to convey accurate information on and address inaccurate beliefs about the absolute and relative harms of tobacco products in an effort to reduce youth tobacco use. Such efforts should be coordinated across local, state, and national levels (eg, The Real Cost Campaign by the FDA).31
Clinical encounters provide another important venue for this type of education. Clinicians should assess the use of all tobacco products, not only cigarettes, and educate youth on the basis of empirical evidence of product-specific harm. Both the Surgeon General and the American Academy of Pediatrics have online resources available.32,33 Additionally, regulation is needed to ensure that misleading claims on tobacco products are not present to facilitate or reinforce misperceptions of the harm (or lack of harm) of specific products. Continued epidemiologic surveillance of multiple tobacco products across time will also be necessary and allow for the investigation of temporal trends of the harm perceptions' role in developing and sustaining tobacco use among youth.
Several important study limitations merit mention, including the self-reported nature of the data. The study involved small sample sizes for some of the tobacco products (eg, pipes), leading to wide CIs, and the inability to explore dual and/or multiple tobacco product use. W1 lifetime tobacco use (rather than the specific product) was included in adjusted models because models would not converge when the use of other individual tobacco products were included as covariates. Additionally, we did not examine how use of specific products influences changes in perceptions of the harm of other tobacco products, which warrants further study. Lastly, we focused on the relationship between absolute and relative harm perceptions by controlling for other variables and not the association between covariates and new use. Perceived addictiveness and social influences, such as peer and/or parent tobacco use and marketing and/or media, are important topics for future research. Those limitations notwithstanding, in the current study, we provide new knowledge about the relationships between harm perceptions across a relatively wide range of tobacco products and the risk of subsequent use of those products in a large, prospective, nationally representative sample of US youth.
Conclusions
The current examination of the association between absolute and relative harm perceptions and noncigarette tobacco use in a longitudinal sample suggests that US youth with low absolute and relative perceived harms of a product are more likely to try that product when compared with youth with higher perceived harms. Educating youth about the harms of specific tobacco products may prevent product-specific initiation and thus reduce tobacco use.
Glossary
- ARR
adjusted relative risk
- CI
confidence interval
- e-cigarette
electronic cigarette
- FDA
Food and Drug Administration
- PATH
Population Assessment of Tobacco and Health
- RR
relative risk
- W1
wave 1
- W2
wave 2
Footnotes
Dr Parker conceptualized and designed the study, conducted the analyses, drafted the initial manuscript, and reviewed and revised the manuscript; Dr Villanti conceptualized and designed the study and reviewed and revised the manuscript; Drs Quisenberry, Stanton, Doogan, Redner, Gaalema, Kurti, Nighbor, Roberts, Cepeda-Benito, and Higgins critically discussed the conceptualization of the study and reviewed the manuscript for important intellectual content; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Conducted as part of the collaborative effort of the National Institutes of Health, Food and Drug Administration, and Tobacco Centers of Regulatory Science Vulnerable Populations Working Group and supported in part by Tobacco Centers of Regulatory Science award P50DA036114 from the National Institute on Drug Abuse and the Food and Drug Administration, Tobacco Centers of Regulatory Science award P50CA180908 from the National Cancer Institute and the Food and Drug Administration, Center for Evaluation and Coordination of Training and Research in Tobacco Regulatory Science award U54CA189222 from the National Cancer Institute and the Food and Drug Administration, Institutional Training Grant award T32DA07242 from the National Institute on Drug Abuse, and Centers of Biomedical Research Excellence award P20GM103644 from the National Institute of General Medical Sciences. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Food and Drug Administration. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Lee YO, Hebert CJ, Nonnemaker JM, Kim AE. Youth tobacco product use in the United States. Pediatrics. 2015;135(3):409–415 [DOI] [PubMed] [Google Scholar]
- 2.Kasza KA, Ambrose BK, Conway KP, et al. Tobacco-product use by adults and youths in the United States in 2013 and 2014. N Engl J Med. 2017;376(4):342–353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jamal A, Gentzke A, Hu SS, et al. Tobacco use among middle and high school students - United States, 2011-2016. MMWR Morb Mortal Wkly Rep. 2017;66(23):597–603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang TW, Gentzke A, Sharapova S, Cullen KA, Ambrose BK, Jamal A. Tobacco product use among middle and high school students - United States, 2011-2017. MMWR Morb Mortal Wkly Rep. 2018;67(22):629–633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Berg CJ, Stratton E, Schauer GL, et al. Perceived harm, addictiveness, and social acceptability of tobacco products and marijuana among young adults: marijuana, hookah, and electronic cigarettes win. Subst Use Misuse. 2015;50(1):79–89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Song AV, Morrell HE, Cornell JL, et al. Perceptions of smoking-related risks and benefits as predictors of adolescent smoking initiation. Am J Public Health. 2009;99(3):487–492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Persoskie A, O’Brien EK, Nguyen AB, Tworek C. Measuring youth beliefs about the harms of e-cigarettes and smokeless tobacco compared to cigarettes. Addict Behav. 2017;70:7–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pacek LR, McClernon FJ. Decline in the perceived risk of cigarette smoking between 2006 and 2015: findings from a U.S. nationally representative sample. Drug Alcohol Depend. 2018;185:406–410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Romer D, Jamieson P. Do adolescents appreciate the risks of smoking? Evidence from a national survey. J Adolesc Health. 2001;29(1):12–21 [DOI] [PubMed] [Google Scholar]
- 10.Wang TW, Trivers KF, Marynak KL, et al. Harm perceptions of intermittent tobacco product use among U.S. youth, 2016. J Adolesc Health. 2018;62(6):750–753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Agaku I, Odani S, Vardavas C, Neff L. Self-identified tobacco use and harm perceptions among US youth. Pediatrics. 2018;141(4):e20173523. [DOI] [PubMed] [Google Scholar]
- 12.Ambrose BK, Rostron BL, Johnson SE, et al. Perceptions of the relative harm of cigarettes and e-cigarettes among U.S. youth. Am J Prev Med. 2014;47(2, suppl 1):S53–S60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Amrock SM, Zakhar J, Zhou S, Weitzman M. Perception of e-cigarette harm and its correlation with use among U.S. adolescents. Nicotine Tob Res. 2015;17(3):330–336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kaufman AR, Suls JM, Klein WMP. Communicating tobacco product harm: compared to what? Addict Behav. 2016;52:123–125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bernat JK, Ferrer RA, Margolis KA, Blake KD. US adult tobacco users’ absolute harm perceptions of traditional and alternative tobacco products, information-seeking behaviors, and (mis)beliefs about chemicals in tobacco products. Addict Behav. 2017;71:38–45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Majeed BA, Weaver SR, Gregory KR, et al. Changing perceptions of harm of e-cigarettes among U.S. adults, 2012-2015. Am J Prev Med. 2017;52(3):331–338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wackowski OA, Delnevo CD. Young adults’ risk perceptions of various tobacco products relative to cigarettes: results from the National Young Adult Health Survey. Health Educ Behav. 2016;43(3):328–336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mermelstein RJ. Adapting to a changing tobacco landscape: research implications for understanding and reducing youth tobacco use. Am J Prev Med. 2014;47(2 suppl 1):S87–S89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Amrock SM, Lee L, Weitzman M. Perceptions of e-cigarettes and noncigarette tobacco products among US youth. Pediatrics. 2016;138(5):e20154306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Choi K, Forster JL. Beliefs and experimentation with electronic cigarettes: a prospective analysis among young adults. Am J Prev Med. 2014;46(2):175–178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Villanti AC, Cobb CO, Cohn AM, Williams VF, Rath JM. Correlates of hookah use and predictors of hookah trial in U.S. young adults. Am J Prev Med. 2015;48(6):742–746 [DOI] [PubMed] [Google Scholar]
- 22.Feirman SP, Donaldson EA, Parascandola M, Snyder K, Tworek C. Monitoring harm perceptions of smokeless tobacco products among U.S. adults: Health Information National Trends Survey 2012, 2014, 2015. Addict Behav. 2018;77:7–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.United States Department of Health and Human Services; National Institutes of Health; National Institute on Drug Abuse; United States Department of Health and Human Services; Food and Drug Administration; Center for Tobacco Products Population assessment of tobacco and health (PATH) study [United States] public-use files. Ann Arbor, MI: Inter-university Consortium for Political and Social Research. Available at: 10.3886/ICPSR36498.v7. Accessed October 1, 2018 [DOI]
- 24.US Department of Health and Human Services; National Institutes of Health; National Institute on Drug Abuse; Food and Drug Administration; Center for Tobacco Products . Population Assessment of Tobacco and Health (PATH) Study Public-Use Files: User Guide. Rockville, MD: Inter-University Consortium for Political and Social Research; 2017 [Google Scholar]
- 25.Hyland A, Ambrose BK, Conway KP, et al. Design and methods of the Population Assessment of Tobacco and Health (PATH) study. Tob Control. 2017;26(4):371–378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stata Corp Stata Statistical Software: Release 14. College Station, TX: Stata Corp LP; 2015 [Google Scholar]
- 27.Brose LS, Brown J, Hitchman SC, McNeill A. Perceived relative harm of electronic cigarettes over time and impact on subsequent use. A survey with 1-year and 2-year follow-ups. Drug Alcohol Depend. 2015;157:106–111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.O’Connor RJ, McNeill A, Borland R, et al. Smokers’ beliefs about the relative safety of other tobacco products: findings from the ITC collaboration. Nicotine Tob Res. 2007;9(10):1033–1042 [DOI] [PubMed] [Google Scholar]
- 29.National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health Preventing Tobacco Use Among Youth and Young Adults: A Report of the Surgeon General. Atlanta, GA: Centers for Disease Control and Prevention; 2012. Available at: www.ncbi.nlm.nih.gov/books/NBK99237/. Accessed May 9, 2018 [PubMed] [Google Scholar]
- 30.Millstein SG, Halpern-Felsher BL. Perceptions of risk and vulnerability In: Fischhoff B, Nightingale EO, Iannotta JG, eds. Adolescent Risk and Vulnerability: Concepts and Measurement. Washington, DC: National Academies Press (US); 2001. Available at: https://www.ncbi.nlm.nih.gov/books/NBK223741/. Accessed February 19, 2018 [PubMed] [Google Scholar]
- 31.Food and Drug Administration The Real Cost Campaign. Available at: https://www.fda.gov/TobaccoProducts/PublicHealthEducation/PublicEducationCampaigns/TheRealCostCampaign/default.htm. Accessed July 19, 2018
- 32.US Surgeon General Resources. Available at: https://e-cigarettes.surgeongeneral.gov/resources.html. Accessed July 18, 2018
- 33.American Academy of Pediatrics Resources on e-cigarettes. Available at: https://www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/Pages/Resources-on-E-cigarettes.aspx. Accessed July 19, 2018