Abstract
Background:
Anxiety and depression (“internalizing”) disorders occur in approximately 50% of patients with alcohol use disorder (AUD) and mark a two-fold increase in the rate of relapse in the months following treatment. In a previous study using network modeling, we found that perceived stress and drinking to cope (DTC) with negative affect were central to maintaining network associations between internalizing psychopathology (anxiety and depression) and drinking in comorbid individuals. Here, we extend this approach to a causal framework.
Methods:
Measures of internalizing psychopathology, drinking urges/behavior, abstinence self-efficacy, and DTC were obtained from 362 adult AUD treatment patients who had a co-occurring anxiety disorder. Data were analyzed using a machine-learning algorithm (“Greedy Fast Causal Inference; GFCI) that infers paths of causal influence while identifying potential influences associated with unmeasured (“latent”) variables.
Results:
Drinking to cope with negative affect served as a central hub for two distinct causal paths leading to drinking behavior, 1) a direct syndromic pathway originating with social anxiety and 2) an indirect stress pathway originating with perceived stress.
Conclusions:
Findings expand the field’s knowledge of the paths of influence that lead from internalizing disorder to drinking in AUD as shown by the first application in psychopathology of a powerful network analysis algorithm (GFCI) to model these causal relationships.
Keywords: Comorbidity, alcohol use disorder, anxiety, machine learning, network analysis
Introduction
Network analysis is an analytic tool widely used in the physical and communication sciences to identify how factors interact to maintain complex systems (Strogatz, 2001). This analytic tool has only recently been applied by psychopathology researchers to identify associations important to maintaining networks representing psychopathology (Borsboom, 2017; Bryant et al., 2017; Galderisi et al., 2018; Haag et al., 2017; McNally, 2017). This approach has added new knowledge concerning the complex phenomena of psychiatric comorbidity, allowing for the identification of “bridge symptoms” (i.e., conduits of inter-symptom and inter-syndrome associations) that can illuminate the network structure of psychopathology and potentially identify high value targets for interventions (Borsboom and Cramer, 2013; Boschloo et al., 2015; Cramer et al., 2010; Jones et al., 2018).
In a recent study, we used network analysis of a theory-driven model (Kushner et al. 2000) to test whether drinking motivated by the goal of reducing negative affect (“drinking to cope”; DTC) served as a “bridge factor” in comorbid alcohol use and anxiety disorder. That work confirmed that DTC served as the sole link between alcohol craving/drinking and psychopathology associated with mood and anxiety (collectively termed “internalizing psychopathology”, INTPs) (Anker et al., 2017). However, while these findings provide new knowledge of the relationship structure of comorbidity maintaining elements consistent with expectations, the causal structure of these relationships could not be determined unambiguously by the network analytic approach used in that study.
Psychopathology researchers are increasingly using network modeling algorithms capable of identifying causal relationships within and between manifestations of psychiatric disorders. These approaches allow for the identification of symptoms that hold precedence as causal chain “activators”, “mediators”, and/or “products” in syndromes as diverse as PTSD, OCD, and depression (Jones et al., 2018; McNally et al., 2017a,b). A noted limitation of current causal network algorithms used in these studies, however, is that their output is restricted to directed acyclic graphs (DAGs) with the underlying assumption that all relevant variables are included in the model (i.e., without considering possible confounding/unmeasured “latent” variables) (McNally et al., 2017a,b). This limitation has recently been overcome by the introduction of another class of causal graphical models, Partial Ancestral Graphs (PAGs), which use an enriched set of edge types to convey both edge orientation and the possible influence of unmeasured (“latent”) variables not represented in the model.
The primary objective of the present study is to leverage recent developments in causal network analysis using the Greedy Fast Causal Inference (GFCI) algorithm (Ogarrio et al., 2016). The PAG produced by GFCI will be used to identify causal associations in the network of interacting internalizing psychopathology and alcohol use, and will determine the extent to which identified associations are influenced by variables not included in the model.
Materials and Methods
Participants
Data were obtained from 362 adult AUD treatment inpatients with co-occurring anxiety disorder at the baseline assessment of a randomized clinical trial (RCT)(Kushner et al., 2013). The baseline assessment occurred prior to the RCT’s clinical interventions within the first week of a 21-day residential chemical dependency treatment program. Inclusion criteria were current (past 30 days) DSM-IV-TR (American Psychiatric Association, 2000) diagnosis of alcohol dependence and at least one current diagnosis of the following anxiety disorders: panic (with or without agoraphobia), social anxiety, and/or generalized anxiety. Exclusion criteria were a history of bipolar disorder, psychosis or schizophrenia, current suicidality, or cognitive impairment. Participants who met criteria for major depression and PTSD were included as long as they endorsed the inclusionary anxiety disorder as “primary”; i.e., as the most problematic condition. That RCT was approved by the University of Minnesota Institutional Review Board and all participants provided written informed consent.
Measures
Measures assessed participants’ levels of internalizing psychopathology, stress and coping abilities, alcohol craving, and drinking behaviors (see Table 1). We constructed symptom-level aggregate measures of the following internalizing disorders: generalized anxiety, depression, social anxiety, panic, and agoraphobia. Two measures assessed behavioral aspects of drinking (i.e., alcohol craving and number of drinks consumed in the 4 months before treatment). Additionally, measures quantified the degree to which individuals’ experienced stressful situations and abstinence self-efficacy, as well as the extent to which participants drank in negative affect situations (DTC). With the exception of drinking amount, all other measures assessed the 30-day period preceding treatment entry. Table 1 contains the range and mean (SD) of each measure along with a description of corresponding assessments.
Table 1.
Measures assessed participants’ levels of internalizing psychopathology (blue), stress and coping abilities (yellow), alcohol craving, and drinking behaviors (magenta).
| Measure | Label | Score range | Mean (SD) | Description |
|---|---|---|---|---|
| Distress | ||||
| Generalized anxiety | GAD | 16 to 80 | 64.13 (11.59) | The total score on the Penn State Worry Questionnaire (Meyer et al., 1990) was taken to quantify the extent of generalized anxiety experienced by participants. |
| Depression | DEP | 0 to 63 | 20.40 (9.09) | The total score on the Beck Depression Inventory (Beck et al., 1996) was taken to quantify symptomatic manifestations of depression. |
| Fear | ||||
| Social phobia | SOC | 0 to 80 | 32.43 (17.30) | The total score on the Social Phobia Scale (Mattick and Clarke, 1998) was used to quantify fear of being evaluated/scrutinized during social situations. |
| Panic | PAN | 0 to 28 | 10.99 (6.34) | The total score on the Panic Disorder Severity Scale (Houck et al., 2002) was used to quantify the frequency and severity of panic symptoms. |
| Agoraphobia | AGR | 0 to 100 | 31.59 (19.78) | The summed score from the Mobility Inventory for Agoraphobia (Chambless et al., 1985) was used to quantify the frequency of situational (e.g., crowds, driving) avoidance as manifested in agoraphobia. |
| Stress & coping | ||||
| Perceived stress | STR | 10 to 40 | 28.15 (5.50) | The total score on the Perceived Stress Scale (Cohen et al., 1983) was used to quantify subjective stress and perceived ability to cope with stress. |
| Abstinence Self-efficacy | SEL | 8 to 48 | 32.91 (10.91) | The total score on the negative affect subscale of the Situational Confidence Questionnaire (Annis et al., 1988) was used to quantify participants confidence in their ability to refrain from drinking to cope. Values were coded so that high scores reflected low self-efficacy. |
| Drinking to cope in negative affect situations | DTC | 20 to 80 | 62.93 (12.15) | The Unpleasant Emotions subscale of the Inventory of Drinking Situations (Annis and Graham, 1995) was used to quantify drinking to cope during negative affect situations (e.g., “depressed”, “felt under a lot of pressure”). |
| Drinking | ||||
| Drinking behavior | DRI | 1608.76 (1271.51) | The total drinks consumed during the 4 months prior to residential treatment entry served as a measure of drinking behavior and was assessed with the Timeline Follow-Back Interview (Sobell and Sobell, 1992) | |
| Alcohol craving | CRA | 0 to 4 | 2.37 (1.05) | The frequency of alcohol craving during the 30 days prior to treatment was assessed using a single item from the Obsessive Compulsive Drinking Scale (Anton et al., 1996) regarding the amount of the participant’s time occupied with ideas, thoughts, impulses, or images related to drinking. |
Note. GAD = generalized anxiety; DEP = depression; SOC = social anxiety; PAN = panic; AGR = agoraphobia; STR = perceived stress; SEL = abstinence self-efficacy; DTC = drinking to cope; DRI = drinking behavior; CRA = alcohol craving
Statistical Analyses
Greedy Fast Causal Inference (GFCI).
Analyses were conducted with the GFCI algorithm which uses a 2-step process to make causal inferences, that can then be represented in graphical format. First, it performs a search of the space of penalized likelihood scores of all possible acyclic causal relationships among the measured variables to establish a preliminary assessment of which variable pairs are potentially causally related. To do this, it uses a fast score-based method called Fast Greedy Equivalence Search, which has been shown in simulation studies to converge on the correct causal model used to generate the data (Chickering 2002; Ramsey 2015). Second, it refines the preliminary assessment by performing a series of conditional independence tests to iteratively rule out causal models that imply conditional independence statements not found to be true of the data. For example, given hypothetical variables X, Y, and Z, it may find that X is independent of Y, X is not independent of Z, Y is not independent of Z, and X is not independent of Y given Z. In such a case, it would make several constraint-based determinations including that Z cannot be a cause of X or Y, and neither X or Y causes the other. We provide an additional example in Figure 1 to illustrate how constraint-based causal reasoning works. The result is a collection of empirically plausible causal associations which can be graphically represented as a PAG. The presence of a directed edge (→) in the PAG means that all possible causal models which did not contain this edge where removed in one of GFCI’s two steps mentioned above. Table 2 lists the possible edge types in a PAG and their corresponding meaning. For a more detailed account of GFCI’s assumptions and validation for finding correct causal relationships, see Ogarrio et al. (2016).
Figure 1.
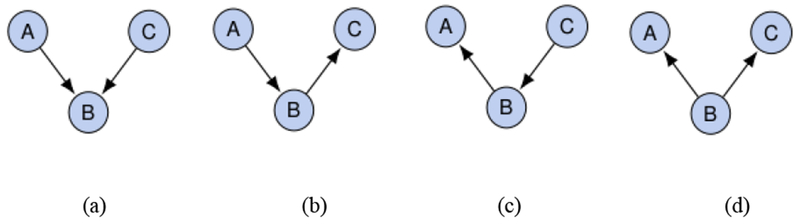
Figure 1 illustrates four different ways that variables A, B, and C could be causally related to each other according to constraint-based causal reasoning. Figure 1 (a) shows a collider graph, where A causes B, C causes B, and there is no edge between A and C. In this graph, the following statistical independence statements are true: A is unconditionally independent of C, and A is dependent on C conditional on B. However if the C to B edge is reversed (e.g. Figure 1 (b)), or the A to B edge is reversed (Figure 1 (c)), or both are reversed (Figure 1 (d)), we would instead find that A is unconditionally dependent on C, and that A is independent of C conditional on B. As such, conditional independence tests can sometimes identify causal direction, e.g. by identifying whether data were generated from Figure 1 (a), or from one of the other three graphs shown in Figure 1. FCI leverages observations like this to orient causal edges, and to rule out or allow for the possibility of latents confounding the causal relationships.
Table 2.
Edge types in a Partial Ancestral Graph (PAG).
| Edge Type | Meaning |
|---|---|
One of the following is true:
|
|
| Y is not a cause of X. In addition, at least one of the following is true:
|
|
All of the following are true:
|
|
All of the following are true:
|
We used the implementation of GFCI found in the Tetrad software package, version 6.3.4 (Ogarrio et al., 2016). This GFCI version employs a statistical model score module and a conditional independence test module using BIC and Fisher Z, respectively. Tetrad’s implementation of the BIC score includes a “penalty discount” parameter, which we set to the standard BIC value of 1. Fisher Z has a p-value threshold parameter (alpha) which we left at the default value of 0.01.
Results
Participants
The mean age of the patient sample was 39.3 (SD = 10.24) and 138 (38%) participants were female. The proportion who endorsed the inclusionary anxiety disorders as “primary” (see Methods) were as follows: social anxiety disorder (n=151, 41.7%), generalized anxiety disorder (n=146, 40.3%), panic disorder without agoraphobia (n=54, 14.9%), and panic disorder with agoraphobia (n=11, 3.0%). 201 (56.0%) participants endorsed two or more anxiety disorders and 186 (51.4%) met diagnostic criteria for major depression. Table 1 shows the mean and SDs for all study measures.
GFCI Results
Figure 2 depicts the PAG generated by the GFCI algorithm. The resulting graph shows that the most proximal causal influence of drinking was drinking urges/craving, which was in turn causally influenced by DTC (i.e., DRI ← CRA ← DTC). The solid green arrows indicate that these relationships were unconfounded i.e., likely not influenced by unmeasured variables. Two additional variables converged on DTC, suggesting the presence of two distinct drinking paths that lead to drinking. The first (“syndromic”) pathway originated with social anxiety (SOC → DTC), and the second pathway originated with stress (STR o⇢ DTC). The dashed black arrows from stress to DTC indicate that this relationship may be influenced by an unmeasured variable. Together the arrows represent a causal model that involves possible direct influences of social anxiety and stress on DTC and more definite influences of DTC on alcohol craving that collectively results in drinking behavior (SOC/STR → DTC → CRA →DRI).
Figure 2.
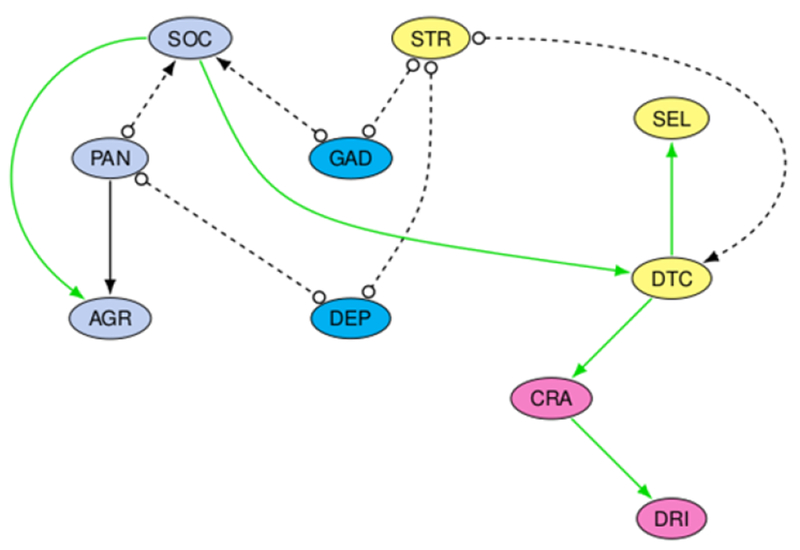
A partial ancestral graph (PAG) produced by the greedy fast casual inference algorithm depicting relationship magnitude (BIC values) between network elements in patients with INTP-AUD comorbidity. See Table 2 for an explanation of edge types.
Having established the drinking model, we next sought to identify variables integral to the causal drinking pattern by dropping individual network elements and re-analyzing the data. Results indicated that with exception of depression (and the variables noted above), the core directed drinking path (i.e., SOC/STR → DTC → CRA →DRI) remained following the removal of all other variables. This simplified model is shown in Figure 3 where depression’s (DEP) association with both stress (DEP o⋯o STR) and social anxiety (DEP o⋯o SOC) is necessary to retain overall directionality in the model. However, the PAG indicated ambiguity in the direction of depression’s associations with social anxiety and stress suggesting the possible influence of unmeasured variables.
Figure 3.
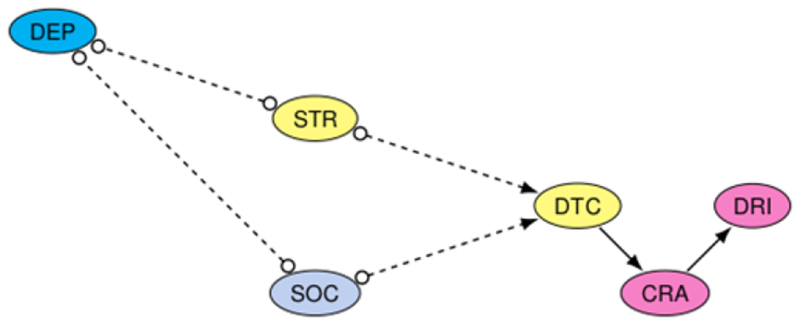
Removal of any other element (e.g., GAD, PAN, AGR, and SEL) did not result in changes to the core drinking pathway identified in Figure 3.
Discussion
In an earlier study, we used a regularized partial correlations network approach (graphical LASSO) to demonstrate that DTC served as a bridge between INTP- and AUD-related variables (Anker et al., 2017). In the present study, we extended this work by modeling these variables using a network analysis algorithm capable of inferring paths of causal influence and detecting the influence of unmeasured variables on these paths. First, the study demonstrated the key role DTC plays in transmitting changes from INTP phenomena to alcohol craving and drinking; i.e., DTC provides a necessary causal link between these comorbid conditions. Second, this study is the first to empirically isolate unique and primary roles for social anxiety symptoms and stress from among several common INTPs, in driving alcohol craving and use directly via their influence on DTC. As a corollary of the second finding, the third novel contribution made by this study is the discovery that depression may not transmit changes to drinking behavior directly, but may do so via it’s relationship with social anxiety and stress.
The finding that DTC serves as a causal antecedent to drinking aligns with and supplements a growing body of epidemiological and clinical findings as well as theory. Data from the National Epidemiological Survey on Alcohol and Related Conditions (NESARC; N ~ 44,000) showed that those with an anxiety disorder who endorsed DTC drank significantly more alcohol and were significantly more likely to develop a new AUD within the next 3 years than was the case for those with an anxiety disorder who did not endorse DTC (Crum et al., 2013a, 2013b; Menary et al., 2011). In fact, those with an anxiety disorder who did not endorse DTC drank significantly less and had the same prospective AUD risk compared to those with no anxiety disorder (Menary et al., 2011). Additionally, recent clinical research shows that targeting the reduction of DTC directly in comorbid patients improves outcomes relative to treatments targeting anxiety symptoms without reference to DTC (Anker et al., 2016; Kushner et al., 2013). Those past findings were consistent with but unable to demonstrate the causal connections illuminated in the present work.
The present findings also help to clarify long-standing uncertainty related to the distinctions between types of INTP and risk for AUD via DTC (Kushner, 2014; Kushner et al., 1990). Kushner et al. (2012) used a latent variable modeling approach in the NESARC dataset to demonstrate that shared rather than unique variance of INTP contributed to AUD, leading the authors to conclude that it is the INTP “load” (the collective INTP burden) rather than the presence of a specific INTP disorder(s), that elevated AUD risk (Kushner et al., 2012). The present findings, while not inconsistent with these earlier findings, suggest a more refined conclusion. That is, while the strength of the association between drinking problems and INTPs increases with INTP load, the causal paths by which unique INTP disorders contribute to this association can differ. Specifically, social anxiety (and perceived stress) contribute directly to the complex of DTC, craving, and drinking while depression may do so only indirectly through its relationship with both social anxiety and perceived stress.
The finding that perceived stress directly influences the complex of DTC, craving, and drinking has important implications. For example, these results suggest that sources of strong stress other than INTP phenomena could engage the causal cascade through which DTC operates to increase alcohol craving and drinking. This is consistent with a large number of field and laboratory studies demonstrating that stressors such as poverty, family discord, racism and social isolation contribute to increased alcohol use and AUD risk even in the absence of diagnosed INTP disorders (Kushner and Anker, n.d.). This conclusion also aligns with emerging neuroscientific models in which negative affect and stress play a key role in the process of addiction without reference to formal anxiety or mood disorder criteria (Koob and Volkow, 2009).
Limitations
These findings should be understood within the context of several limitations of the study’s method. First, a limitation (of sorts) is that the fields of psychopathology and social sciences research have traditionally taught that it is not possible to infer causal influences from cross-sectional data. While it is true that traditional data analytic techniques would not be able to infer causal paths in cross-sectional data, the GFCI network algorithm used in this study was specifically designed to do just that. This method employs the two-step algorithm described in detail in the Methods to empirically identify potential causal paths by evaluating the fit of models with all possible causal paths followed by a deductive algorithm to rule out causal paths that are logically impossible given the data. This analytic method is innovative in the field of psychopathology and, as such, may not feel intuitive or trustworthy to some traditionally trained researchers. With that said, this method has been shown to identify correct causal paths in simulated data sets and has also proven capable to identifying causal mechanisms in real biological data (Chickering 2002; Goudet et al. 2017; Ramsey 2015). The ultimate contribution that this approach makes to our field remains to be seen but this work shows its potential to meaningfully increase the knowledge yield from existing data as well as yet to be collected data. The true test of the value of the present findings will be found in using them to refine hypotheses for testing using more traditional analytic methods such as experimental and prospective approaches.
A second limitation is that the GFCI models tested assumes that the real world processes governing relationships between the variables are acyclic (acyclicity assumption, perSpirtes et al. (2000)). While this same feature (the assumption of acyclicity) applies to all of the previously published network modeling work in psychopathology and to a very large proportion of all psychopathology modeling research, it remains important to note. For example, influential theoretical models and clinical experience suggest that INTP-AUD comorbidity develops and is maintained with both feedforward and feedback cyclical influences(e.g., Kushner et al., 2000). According to this view, stress and DTC increase drinking, however, increased drinking also increases the intensity of stress while decreasing one’s ability to cope with stressful life experiences. While the models tested identify direct paths to drinking that are most probable, information regarding the extent to which downstream factors influence upstream factors would further understanding of the dynamic nature of associations involved in comorbid INTP-AUD. In summary, while it seems likely that cyclical effects exist in the INTP-AUD relationship that could not be detected in this study, this does not diminish the validity of the acyclical paths we were able to demonstrate.
Third, the relatively small sample size and large number of variables could introduce heterogeneity that could weaken the internal validity of the drinking path identified in Figure 2. To address this, we subsampled 90% of the sample 10,000 times, created a GFCI graph for each of the 10,000 datasets, and aggregated them into a single graph based on the percentage of edges that were most commonly present. The resulting graph verified the directionality of the drinking path (see Supplement, Figure S2), suggesting heterogeneity did not appreciably affect our core finding of a directed social anxiety/stress → DTC → craving → drinking path.
A final limitation is that the sample was restricted to patients receiving residential care for AUD who had a co-occurring anxiety disorder and, therefore, our findings may have limited generalizability. Despite the high frequency of patients that fit this profile, it is unclear whether the results would extend to other populations, such as non-treatment seeking individuals with substance dependence, those with non-alcohol related substance dependency (opioids, marijuana, or stimulants), and/or individuals with different non-substance related co-occurring disorders (e.g., PTSD). Demonstrating the same model applies to different patient populations with varying combinations of substance use disorders and co-occurring internalizing disorders would test the generalizability (external validity) of the model.
Conclusion
These findings further our understanding of the intricate interplay between multiple constructs and pathways involved in the maintenance of drinking among those with INTP-AUD comorbidity and they provide novel treatment implications for the importance of targeting upstream (social anxiety, perceived stress, and depression) and more terminal (DTC) influences associated with drinking in this relapse-prone population. These findings also highlight a new (to psychopathology) algorithm with unique and desirable capabilities that could help guide the direction of more controlled/experimental research efforts that test identified causal patterns involved in psychopathology.
Supplementary Material
Acknowledgments
This work was supported by NIAAA grant K01AA024805 awarded to the first author, NIDA training grant T320A037183 to support the work of the fourth author, and NIAAA grant R01AA015069 awarded to the last author.
References
- American Psychiatric Association, 2000. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR), 4th ed. American Psychiatric Association, Arlington, VA. [Google Scholar]
- Anker JJ, Forbes MK, Almquist ZW, Menk JS, Thuras P, Unruh AS, Kushner MG, 2017. A network approach to modeling comorbid internalizing and alcohol use disorders. J. Abnorm. Psychol. 126, 325–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anker JJ, Kushner MG, Thuras P, Menk J, Unruh AS, 2016. Drinking to cope with negative emotions moderates alcohol use disorder treatment response in patients with co-occurring anxiety disorder. Drug Alcohol Depend. 159, 93–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Annis H, Martin Graham J, Addiction Research Foundation, Foundation, O.A.R., 1988. Situational Confidence Questionnaire (SCQ): User’s Guide. Addiction Research Foundation. [Google Scholar]
- Annis HM, Graham JM, 1995. Profile types on the Inventory of Drinking Situations: Implications for relapse prevention counseling. Psychol. Addict. Behav. 9, 176. [Google Scholar]
- Anton RF, Moak DH, Latham PK, 1996. The obsessive compulsive drinking scale: A new method of assessing outcome in alcoholism treatment studies. Arch. Gen. Psychiatry 53, 225–231. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK, 1996. BDI-II: Beck depression inventory. Pearson. [Google Scholar]
- Borsboom D, 2017. A network theory of mental disorders. World Psychiatry 16, 5–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsboom D, Cramer AOJ, 2013. Network analysis: an integrative approach to the structure of psychopathology. Annu. Rev. Clin. Psychol. 9, 91–121. [DOI] [PubMed] [Google Scholar]
- Boschloo L, van Borkulo CD, Rhemtulla M, Keyes KM, Borsboom D, Schoevers RA, 2015. The Network Structure of Symptoms of the Diagnostic and Statistical Manual of Mental Disorders. PLoS One 10, e0137621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant RA, Creamer M, O’Donnell M, Forbes D, McFarlane AC, Silove D, Hadzi-Pavlovic D, 2017. Acute and Chronic Posttraumatic Stress Symptoms in the Emergence of Posttraumatic Stress Disorder: A Network Analysis. JAMA Psychiatry 74, 135–142. [DOI] [PubMed] [Google Scholar]
- Chambless DL, Caputo GC, Jasin SE, Gracely EJ, Williams C, 1985. The Mobility Inventory for Agoraphobia. Behav. Res. Ther. 23, 35–44. [DOI] [PubMed] [Google Scholar]
- Chickering DM. Optimal Structure Identification With Greedy Search. J Mach Learn Res. 2002;3(Nov):507–554. [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R, 1983. A global measure of perceived stress. J. Health Soc. Behav. 24, 385–396. [PubMed] [Google Scholar]
- Cramer AOJ, Waldorp LJ, van der Maas HLJ, Borsboom D, 2010. Comorbidity: a network perspective. Behav. Brain Sci. 33, 137–50; discussion 150–93. [DOI] [PubMed] [Google Scholar]
- Crum RM, La Flair L, Storr CL, Green KM, Stuart EA, Alvanzo AAH, Lazareck S, Bolton JM, Robinson J, Sareen J, Mojtabai R, 2013a. Reports of drinking to self-medicate anxiety symptoms: longitudinal assessment for subgroups of individuals with alcohol dependence. Depress. Anxiety 30, 174–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crum RM, Mojtabai R, Lazareck S, Bolton JM, Robinson J, Sareen J, Green KM, Stuart EA, La Flair L, Alvanzo AAH, Storr CL, 2013b. A prospective assessment of reports of drinking to self-medicate mood symptoms with the incidence and persistence of alcohol dependence. JAMA Psychiatry 70, 718–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galderisi S, Rucci P, Kirkpatrick B, Mucci A, Gibertoni D, Rocca P, Rossi A, Bertolino A, Strauss GP, Aguglia E, Others, 2018. Interplay Among Psychopathologic Variables, Personal Resources, Context-Related Factors, and Real-life Functioning in Individuals With Schizophrenia: A Network Analysis. JAMA Psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goudet O, Kalainathan D, Caillou P, Lopez-Paz D, Guyon I, Sebag M, Tritas A, Tubaro P 2017. Learning functional causal models with generative neural networks. arXiv preprint arXiv:1709.05321.
- Haag C, Robinaugh DJ, Ehlers A, Kleim B, 2017. Understanding the Emergence of Chronic Posttraumatic Stress Disorder Through Acute Stress Symptom Networks. JAMA Psychiatry 74, 649–650. [DOI] [PubMed] [Google Scholar]
- Houck PR, Spiegel DA, Shear MK, Rucci P, 2002. Reliability of the self-report version of the panic disorder severity scale. Depress. Anxiety 15, 183–185. [DOI] [PubMed] [Google Scholar]
- Jones PJ, Mair P, Riemann BC, Mugno BL, McNally RJ, 2018. A network perspective on comorbid depression in adolescents with obsessive-compulsive disorder. J. Anxiety Disord. 53, 1–8. [DOI] [PubMed] [Google Scholar]
- Koob GF, Volkow ND, 2009. Neurocircuitry of Addiction. Neuropsychopharmacology 35, 217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kushner MG, 2014. Seventy-five years of comorbidity research. J. Stud. Alcohol Drugs Suppl. 75 Suppl 17, 50–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kushner MG, Abrams K, Thuras P, Thuras P, Hanson KL, 2000. Individual differences predictive of drinking to manage anxiety among non-problem drinkers with panic disorder. Alcohol. Clin. Exp. Res. 24, 448–458. [PubMed] [Google Scholar]
- Kushner MG, Anker JJ, n.d. Negative Emotions and Alcohol Use Disorder Treatment In: Preedy VR (Ed.), Neuroscience of Alcohol. Elsevier. [Google Scholar]
- Kushner MG, Maurer EW, Thuras P, Donahue C, Frye B, Menary KR, Hobbs J, Haeny AM, Van Demark J, 2013. Hybrid cognitive behavioral therapy versus relaxation training for co-occurring anxiety and alcohol disorder: a randomized clinical trial. J. Consult. Clin. Psychol. 81, 429–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kushner MG, Sher KJ, Beitman BD, 1990. The relation between alcohol problems and the anxiety disorders. Am. J. Psychiatry 147, 685–695. [DOI] [PubMed] [Google Scholar]
- Kushner MG, Wall MM, Krueger RF, Sher KJ, Maurer E, Thuras P, Lee S, 2012. Alcohol dependence is related to overall internalizing psychopathology load rather than to particular internalizing disorders: evidence from a national sample. Alcohol. Clin. Exp. Res. 36, 325–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattick RP, Clarke JC, 1998. Development and validation of measures of social phobia scrutiny fear and social interaction anxiety1. Behav. Res. Ther 36, 455–470. [DOI] [PubMed] [Google Scholar]
- McNally RJ, 2017. Networks and Nosology in Posttraumatic Stress Disorder. JAMA Psychiatry 74, 124–125. [DOI] [PubMed] [Google Scholar]
- McNally RJ, Heeren A, Robinaugh DJ, 2017a. A Bayesian network analysis of posttraumatic stress disorder symptoms in adults reporting childhood sexual abuse. Eur. J. Psychotraumatol. 8, 1341276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNally RJ, Mair P, Mugno BL, Riemann BC, 2017b. Co-morbid obsessive–compulsive disorder and depression: a Bayesian network approach. Psychol. Med 1–11. [DOI] [PubMed] [Google Scholar]
- Menary KR, Kushner MG, Maurer E, Thuras P, 2011. The prevalence and clinical implications of self-medication among individuals with anxiety disorders. J. Anxiety Disord. 25, 335–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer TJ, Miller ML, Metzger RL, Borkovec TD, 1990. Development and validation of the Penn State Worry Questionnaire. Behav. Res. Ther. 28, 487–495. [DOI] [PubMed] [Google Scholar]
- Ogarrio JM, Spirtes P, Ramsey J, 2016. A Hybrid Causal Search Algorithm for Latent Variable Models. JMLR Workshop Conf. Proc. 52, 368–379. [PMC free article] [PubMed] [Google Scholar]
- Ramsey JD. Scaling up greedy equivalence search for continuous variables. CoRR, abs/150707749. 2015. [Google Scholar]
- Sobell LC, Sobell MB, 1992. Timeline Follow-Back In: Measuring Alcohol Consumption. Humana Press, Totowa, NJ, pp. 41–72. [Google Scholar]
- Spirtes P, Glymour C, Scheines R, 2000. Causation, Prediction, and Search. Adaptive Computation and Machine Learning.
- Strogatz SH, 2001. Exploring complex networks. Nature 410, 268–276. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


