Abstract
Objectives:
Medical marijuana use may substitute prescription opioid use, whereas nonmedical marijuana use may be a risk factor of prescription opioid misuse. This study examined the associations between recreational marijuana legalization and prescription opioids received by Medicaid enrollees.
Methods:
State-level quarterly prescription drug utilization records for Medicaid enrollees during 2010–2017 were obtained from Medicaid State Drug Utilization Data. The primary outcome, opioid prescriptions received, was measured in three population-adjusted variables: number of opioid prescriptions, total doses of opioid prescriptions in morphine milligram equivalents, and related Medicaid spending, per quarter per 100 enrollees. Two difference-in- difference models were used to test the associations: eight states and DC that legalized recreational marijuana during the study period were first compared among themselves, then compared to six states with medical marijuana legalized before the study period. Schedule II and III opioids were analyzed separately.
Results:
In models comparing eight states and DC, legalization was not associated with Schedule II opioid outcomes; having recreational marijuana legalization effective in 2015 was associated with reductions in number of prescriptions, total doses, and spending of Schedule III opioids by 32% (95% CI: (−49%, −15%), p=0.003), 30% ((−55%, −4.4%), p=0.027), and 31% ((−59%, −3.6%), p=0.031), respectively. In models comparing eight states and DC to six states with medical marijuana legalization, recreational marijuana legalization was not associated with any opioid outcome.
Conclusions:
No evidence suggested that recreational marijuana legalization increased prescription opioids received by Medicaid enrollees. There was some evidence in some states for reduced Schedule III opioids following the legalization.
Keywords: marijuana, opioid, recreational marijuana legalization, opioid prescription, Medicaid
1. Introduction
The liberalization of marijuana laws has been a worldwide momentum in recent years. Following medical marijuana legalization in over half states in the US and a few countries in Europe and America, in 2012, Colorado and Washington in the US first passed laws to legalize marijuana use by adults aged 21 or older. Since then, recreational marijuana legalization has been adopted in eight states and DC where one fifth of US population live (Lawatlas, 2018). These state-wide laws emboldened other jurisdictions in the world to enable recreational marijuana market, with Uruguay and Canada passing country-level legalization in 2014 (Miroff, 2017) and 2017 (Austen, 2017), respectively. While intense debates are ongoing surrounding recreational marijuana legalization, little empirical evidence has been provided regarding its impacts on public health. Primarily constrained by data availability, existing research typically conducted pre- and post-legalization evaluations on one or two states in the US controlling for contemporaneous trends in a limited number of comparison states (Aydelotte et al., 2017; Cerda et al., 2017; Kerr et al., 2017; Livingston et al., 2017). Study findings were mixed. Some states with recreational marijuana legalization saw an increase in marijuana use (Cerda et al., 2017; Kerr et al., 2017) but no changes in motor vehicle crash fatality rates (Aydelotte et al., 2017).
The impacts of recreational marijuana legalization on other drugs remain unclear. Particularly, there have been considerable concerns about whether and how the opioid crisis may be influenced. Prescription opioid related harms are becoming a global problem, especially in the US (Dasgupta et al., 2018; Fischer et al., 2013). In the past 2 decades, the volume of opioid prescriptions quadrupled (Volkow, 2016) and opioid overdose deaths more than doubled (Warner et al., 2014). It is estimated that opioid misuse and overdose imposed an economic burden of $56 billion to the US each year (Birnbaum et al., 2011). In 2017, opioid crisis was declared a “National Public Health Emergency” (Drash and Merica, 2017; Merica, 2017).
There have been two hypotheses regarding the impacts of marijuana laws on opioid use. Marijuana is suggested to be effective in pain management (NationalAcademies, 2017) and could be used medically by patients as substitutes for opioids. There were emerging population studies suggesting that medical marijuana patients reported substituting marijuana for opioids (Lucas, 2012; Lucas et al., 2013; Lucas and Walsh, 2017; Reiman, 2009). The first hypothesis therefore suggested that liberalization of marijuana laws could reduce opioid use and related consequences if it increased marijuana use for medical purposes. In contrast, the competing hypothesis argued that marijuana, when used for nonmedical purposes, could act as a gateway drug to opioids and result in increased opioid misuse and related outcomes. A recent study reported that nonmedical marijuana use was associated with increased odds of prescription opioid misuse and opioid use disorder in a longitudinal, nationally representative sample in the US (Olfson et al., 2018). Liberalization of marijuana laws may thus lead to a deterioration of opioid crisis if it encouraged nonmedical use of marijuana.
Both hypotheses regarding the impacts of marijuana laws on opioid use may be valid. The net effects of medical or recreational marijuana legalization could be either positive or negative, depending on which of the two hypotheses dominated in reality. Recent studies on medical marijuana legalization reported that substantial reductions in opioid-related deaths, misuse, drug prescriptions, traffic fatalities, and inpatient stays were observed after medical marijuana was legalized (Bachhuber et al., 2014; Bradford and Bradford, 2016, 2017; Bradford et al., 2018; Kim et al., 2016; Liang et al., 2018; Powell et al., 2018; Shi, 2017). These findings appeared to support the first hypothesis, albeit indirectly, if marijuana use for medical purposes increased more than marijuana use for nonmedical purposes as a result of medical marijuana legalization. Regarding recreational marijuana legalization, there has been continuous concern that the legalization may exacerbate opioid crisis (Borchardt, 2017; Lopez, 2018) if the legalization primarily impacted nonmedical marijuana use. The empirical support is very limited. The only study focusing on recreational marijuana legalization indicated that the increasing trends in opioid-related deaths in Colorado were reversed following recreational marijuana legalization (Livingston et al., 2017). However, data on a single state without comparison states lack generalizability and causal inferences.
This study aimed to provide empirical evidence about the relationship between recreational marijuana legalization and prescription opioids. We focused on Medicaid enrollees in the US. Medicaid is a US health insurance program jointly funded by the federal government and states, primarily covering beneficiaries with low income and disabilities. Medicaid enrollees are a priority population for opioid control with a disproportionate burden of pain as well as a higher risk of opioid overdose and misuse (Mack et al., 2015; Shmagel et al., 2016). Using 2010–2017 state Medicaid drug prescription data, we were able to examine all the eight states and DC that have legalized recreational marijuana in the US. We explored the heterogeneity in policy responses by analyzing different drug schedules separately.
2. Methods
This study is a secondary data analysis of state-quarter aggregate records of prescription opioids received by Medicaid enrollees in the US.
2.1. Data
State-quarter level records of prescription drugs received by Medicaid enrollees from the 1st quarter of 2010 through the 2nd quarter of 2017 were obtained from Medicaid State Drug Utilization Data (CMS, 2018). Because states’ reporting is mandatory in the Medicaid Drug Rebate Program, the prescription drug records were nearly complete in each state and quarter (DHHS, 2012). The data included quarterly records of filled prescription drugs dispensed in outpatient settings and reimbursed by Medicaid, but excluded drugs dispensed in emergency departments or inpatient settings or paid with cash (CMS, 2018).
2.2. Study population
All patients enrolled in Medicaid including those enrolled in fee-for-service programs and managed care programs were included. Records before 2010 were excluded because states’ reporting on managed care programs were irregular and inconsistent before then.
2.3. Measures
The primary outcome, prescription opioids received, were measured in three population- adjusted variables: 1) number of opioid prescriptions, 2) total doses of opioid prescriptions (in quantity of morphine milligram equivalents (MME)) (CDC, 2016), and 3) Medicaid spending on opioid prescriptions, per quarter per 100 Medicaid enrollees. Nominal spending was converted to 2017 constant US dollars using consumer price index. The number of Medicaid enrollees by state and year was obtained from annual Medicaid Managed Care Enrollment Reports (CMS, 2017). Prescription opioids were identified by linking the National Drug Code numbers in Medicaid State Drug Utilization Data to drug information (CDC, 2016) in the Approved Drug Products with Therapeutic Equivalence Evaluations published by the US Food and Drug Administration (FDA, 2017). Because we were primarily interested in prescription opioids potentially substitutable by marijuana, we followed previous studies (Liang et al., 2018; Wen et al., 2017) to exclude buprenorphine drugs typically used to treat opioid use disorder (e.g., Suboxone®, Subutex®) and included buprenorphine drugs commonly used in pain management (e.g., Butrans®, Belbuca®). All methadone drugs were included because they were generally prescribed for pain management in outpatient settings that our data source captured. Schedule II and Schedule III opioids were categorized separately to reflect their differences in drug misuse and overdose potential. According to the most recent classifications by the Drug Enforcement Agency (DEA, 2014), Hydrocodone-combination drugs such as Vicodin and Lortab were classified as Schedule II drugs. The types of prescription opioids included in our analysis were listed in Table 1 by drug schedule.
Table 1.
Schedule II and Schedule III Opioids in the US
| Schedule II | Schedule III |
|---|---|
| Alfentanil | Buprenorphine |
| Alphaprodine | Codeine & isoquinoline alkaloid |
| Anileridine | Codeine combination product |
| Bezitramide | Dihydrocodeine combination |
| Carfentanil | product |
| Codeine | Ethylmorphine combination product |
| Dextropropoxyphene, bulk (non-dosage | Morphine combination product |
| forms) | Nalorphine |
| Dihydrocodeine | Opium combination product |
| Dihydroetorphine | |
| Diphenoxylate | |
| Ethylmorphine | |
| Etorphine HCl | |
| Fentanyl | |
| Hydrocodone | |
| Hydromorphone | |
| Isomethadone | |
| Levo-alphacetylmethadol | |
| Levomethorphan | |
| Levorphanol | |
| Meperidine | |
| Meperidine intermediate-A/B/C | |
| Metazocine | |
| Methadone | |
| Methadone intermediate | |
| Metopon | |
| Moramide-intermediate | |
| Morphine | |
| Opium | |
| Oripavine | |
| Oxycodone† | |
| Oxymorphone | |
| Phenazocine | |
| Piminodine | |
| Poppy Straw/ Poppy Straw Concentrate | |
| Racemethorphan | |
| Racemorphan | |
| Remifentanil | |
| Sufentanil | |
| Tapentadol | |
| Thebaine | |
| Thiafentanil | |
Notes: In this study, Schedule II and Schedule III opioids were identified based on the current classifications by the US Drug Enforcement Agency (DEA) and analyzed separately. DEA defined Schedule II substances as those having “a high potential for abuse which may lead to severe psychological or physical dependence” and Schedule III substances as those having “a potential for abuse less than substances in Schedules I or II and abuse may lead to moderate or low physical dependence or high psychological dependence.” Opioids highlighted in bold were identified in the Medicaid State Drug Utilization Data. Opioids not highlighted in bold were excluded in the Medicaid State Drug Utilization Data because they were either excluded from the Approved Drug Products with Therapeutic Equivalence Evaluations published by the Food and Drug Administration (FDA) or not commonly used in outpatient settings.
Following previous research (Aydelotte et al., 2017; Cerda et al., 2017; Kerr et al., 2017; Livingston et al., 2017), the primary policy variable was the implementation of statewide recreational marijuana legalization identified by law implementation dates. During the study period, eight states and DC implemented recreational marijuana legalization (Supplemental Table S11). Because state-level heterogeneity in the duration of legalization may have differential impacts on prescription opioids, three dichotomous policy variables were created to indicate recreational marijuana legalization taking effect at different time points (Supplemental Table S11): 4th quarter of 2012 (Colorado and Washington), around 2nd quarter of 2015 (Alaska, DC, and Oregon), or around 4th quarter of 2016 (California, Massachusetts, Maine, and Nevada).
We also controlled for state-level time-varying covariates in the regressions, including a dichotomous variable indicating statewide medical marijuana legalization in effect, a dichotomous variable indicating statewide prescription drug monitoring program in effect, a dichotomous variable indicating statewide Medicaid expansion under the Affordable Care Act that provided insurance to all adults with income up to 138% of the US federal poverty level, a continuous variable for median household annual income adjusted to 2017 dollars with consumer price index, a continuous variable for annualized poverty rate, and a continuous variable for annualized unemployment rate (BLS, 2018; United States Census Bureau, 2018; Henry J. Kaiser Family Foundation, 2018).
2.4. Statistical analyses
The analysis was conducted at state-quarter level. A difference-in-difference approach was used to assess the associations of legalizing recreational marijuana with the three log- transformed continuous outcomes for Schedule II and Schedule III prescription opioids, separately. The coefficients in regression models can be interpreted as the average percentage change in prescription opioid outcomes in association with the implementation of recreational marijuana legalization.
The underlying assumption in the difference-in-difference approach is parallel trends in treatment and comparison states in the absence of policy change (Angrist and Pischke, 2008). In our study, treatment states were eight states (Alaska, California, Colorado, Maine, Massachusetts, Nevada, Oregon, and Washington) and DC that adopted recreational marijuana legalization in the study period. Before they adopted recreational marijuana legalization, they all had adopted medical marijuana legalization. Because medical marijuana legalization had significant impacts on trends in opioid-related outcomes including prescribing in Medicaid population (Bachhuber et al., 2014; Bradford and Bradford, 2016, 2017; Bradford et al., 2018; Kim et al., 2016; Liang et al., 2018; Powell et al., 2018; Shi, 2017), comparison states should have had medical marijuana legalization in effect to ensure their comparability with these treatment states prior to recreational marijuana legalization. We therefore made comparisons in two difference-in-difference models. Model A compared among eight states and DC themselves. Because they implemented recreational marijuana legalization at different time points, at a given time point, states that had not implemented legalization served as controls. Model B compared eight states and DC to six states (Hawaii, Michigan, Montana, New Mexico, Rhode Island, and Vermont) that had implemented medical marijuana legalization as of January 1st, 2010 but had not implemented recreational marijuana legalization during the study period. These two models were able to isolate the impacts of recreational marijuana legalization from the impacts of medical marijuana legalization on opioid prescriptions. Comparing eight states and DC to all the remaining 42 states violated the difference-in-difference assumption, because states without medical marijuana legalization had different trends in opioid prescriptions compared to states with medical marijuana legalization (Bachhuber et al., 2014; Bradford and Bradford, 2016, 2017; Bradford et al., 2018; Kim et al., 2016; Liang et al., 2018; Powell et al., 2018; Shi, 2017). To test the assumption of parallel trends in treatment and comparison states in the absence of policy change, we used repeated ANOVA to compare time trends in opioid outcomes between treatment and comparison states in years 2010, 2011, and 2012 when none of these states adopted recreational marijuana legalization.
Linear regressions were used, controlling for time-varying state covariates, state indicators, year and quarter indicators, and state-specific linear time trends. State indicators accounted for time-invariant state-level unobserved heterogeneities such as social norms about opioid use. Year and quarter indicators accounted for time-specific heterogeneities common to all the states at the same time, such as CDC Guideline for Prescribing Opioids for Chronic Pain published in 2016 (Dowell et al., 2016). State-specific linear time trends accounted for state- level time-variant trends in outcomes. Standard errors in the regression were clustered at the state level.
To test the robustness of results, we conducted a series of sensitivity tests. 1) Because California, Maine, Massachusetts, and Nevada had limited number of post-legalization observations, the policy impacts in these states may not be statistically discernable. In addition, the most recent quarters of Medicaid State Drug Utilization data may contain errors and are often subject to future revision. We excluded the observations after 3rd quarter of 2016 when these states implemented recreational marijuana legalization to focus the analyses on states legalizing recreational marijuana before 2016. 2) We moved Hydrocodone-combination drugs to Schedule III opioids to test results sensitivity to recent drug reclassifications. 3) It is suggested that adding state-specific time trends may attenuate estimates of policy impact if the policy impact acts upon the trend itself (Meer and West, 2015; Wolfers, 2006). We removed state-specific time trends in regressions and expected that the associations would be more discernable. 4) Following previous research (Bradford and Bradford, 2016, 2017), we also performed falsification tests on 4 drug classes, including blood-thinning agents, phosphorous-stimulating agents, antivirals, and antibiotics, as there is no scientific evidence suggesting the associations between marijuana and the underlying conditions that these drugs treat. These drugs were assumed to be not associated with recreational marijuana legalization but associated with common unmeasured confounding factors such as those affecting general prescribing, healthcare utilization, and healthcare resources at the state level.
3. Results
We focused on the results on number of opioid prescriptions per quarter per 100 Medicaid enrollees. The results for the other two outcomes (total doses of opioid prescriptions and Medicaid spending on opioid prescriptions) were similar and available in Supplemental Files2.
3.1. Descriptive statistics
Table 2 reports the descriptive statistics of pooled data by recreational marijuana legalization status. Compared to six states with medical marijuana legalization but without recreational marijuana legalization, eight states and DC that legalized recreational marijuana in the study period had slightly and insignificantly higher rates of Schedule II and III opioid prescriptions. Supplemental Table S22 reports ANOVA tests for time trend comparisons, suggesting that the time trends prior to legalization did not significantly differ between the states legalizing recreational marijuana in 2012 and the six comparison states, between the states legalizing recreational marijuana in 2015 and the six comparison states, or between the states legalizing recreational marijuana in 2016/7 and the six comparison states.
Table 2.
Descriptive Statistics of Pooled Data 2010–2017.
| States that Legalized Recreational Marijuana in 2010– 20171 |
States that Legalized Medical Marijuana before 20102 |
Between Group Difference Test |
|
|---|---|---|---|
| Mean, 95%CI | Mean, 95%CI | P-value | |
| Schedule II Opioid Prescriptions | |||
| Number of Opioid Prescription Dispensed per quarter per 100 Medicaid Enrollees | 12.52 (11.88,13.15) |
11.87 (11.13, 12.60) | 0.19 |
| Morphine Milligram Equivalents per quarter per 100 Medicaid Enrollees | 12741.80 (11938.63, 13544.97) |
12385.58 (11545.88, 13225.28) |
0.56 |
| Medicaid Spending on Opioid Prescriptions per quarter per 100 Medicaid Enrollees, 2017 dollars | 465.92 (434.62, 497.23) | 644.08 (527.17, 761.00) | <.001 |
| Schedule III Opioid Prescriptions | |||
| Number of Opioid Prescription Dispensed per quarter per 100 Medicaid Enrollees | 0.87 (0.79, 0.96) | 0.78 (0.69, 0.87) | 0.16 |
| Morphine Milligram Equivalents per quarter per 100 Medicaid Enrollees | 146.32 (133.49, 159.15) | 158.89 (136.04, 181.74) | 0.31 |
| Medicaid Spending on Opioid Prescriptions per quarter per 100 Medicaid Enrollees, 2017 dollars | 12.97 (11.90, 14.03) | 15.87 (13.19, 18.55) | 0.025 |
| Recreational Marijuana Legalization in Effect | 0.25 (0.20, 0.30) | 0 | <0.001 |
| Medical Marijuana Legalization in Effect | 0.94 (0.91, 0.97) | 1 | 0.0008 |
| Prescription Drug Monitoring Program in Effect | 0.79 (0.74, 0.83) | 0.82 (0.77, 0.88) | 0.34 |
| Medicaid Expansion as Part of Affordable Care Act | 0.36 (0.31, 0.42) | 0.38 (0.31, 0.46) | 0.66 |
| Median Household Income, 2017 dollars | 4527.91 (3514.36, 6541.46) | 4121.00 (1864.42, 6377.57) | 0.79 |
| Poverty Rate, % | 13.26 (12.92, 13.61) | 13.30 (12.73, 13.87) | 0.91 |
| Unemployment Rate, % | 7.34 (7.07, 7.61) | 6.38 (6.04, 6.72) | <0.001 |
Notes: state-quarter observations in 2010–2017 were pooed to provide the statistics.
The 8 states and DC that implemented recreational marijuana legalization during the study period included AK, CA, CO, DC, ME, MA, NV, OR, WA, and DC.
The 6 states that had implemented medical marijuana legalization as of January 1st, 2010 but had not implemented recreational marijuana legalization during the study period included HI, MI, MT, NM, RI, and VT.
Figure 1 shows the unadjusted time trends in number of Schedule III opioid prescriptions by legalization status. States that legalized recreational marijuana in 2015 and 2016/7 saw a reduction in number of Schedule III opioid prescriptions after the legalization took effect, whereas states that legalized recreational marijuana in 2012 saw a slight increase. Trends in number of Schedule II opioid prescriptions did not appear to differ by legalization status (not shown).
Figure 1.
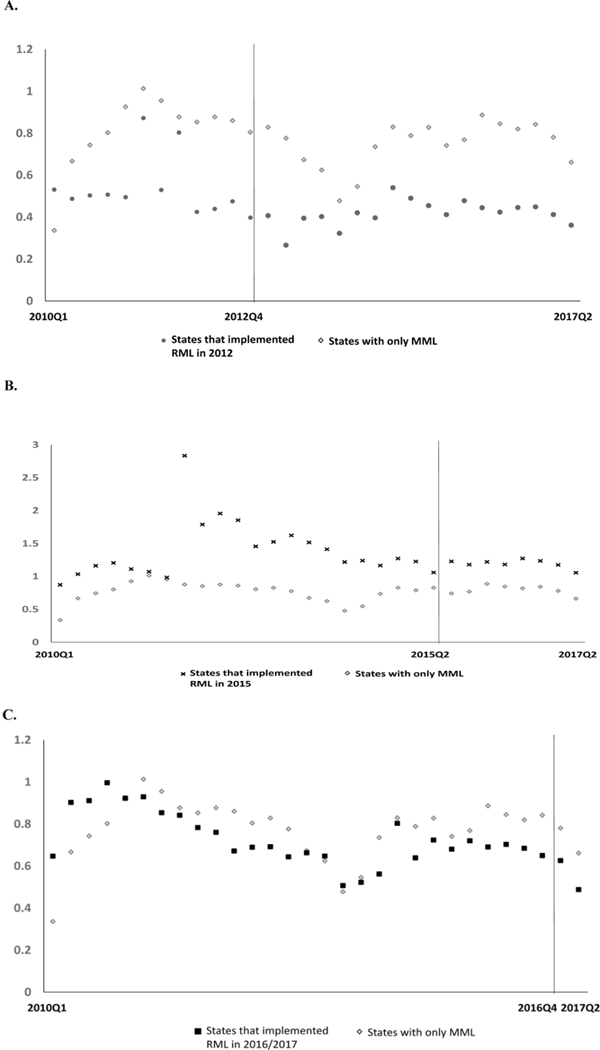
Time Trends in Number of Schedule III Opioid Prescriptions per Quarter per 100 Medicaid Enrollees by Marijuana Legalization Status, 2010–2017,Figure 1a. States that implemented Recreational Marijuana Legalization in 2012 compared to States with Medical Marijuana Legalization Only,Figure 1b. States that implemented Recreational Marijuana Legalization in 2015 compared to States with Medical Marijuana Legalization Only,Figure 1c. States that implemented Recreational Marijuana Legalization in 2016/7 compared to States with Medical Marijuana Legalization Only, Notes: (RML: recreational marijuana legalization; MML: medical marijuana legalization) CO and WA implemented recreational marijuana legalization in 2012; AK, DC, and OR implemented recreational marijuana legalization in 2015; CA, MA, ME, and NV implemented recreational marijuana legalization in late 2016 or early 2017. HI, MI, MT, NM, RI, and VT had implemented medical marijuana legalization as of January 1st, 2010 but had not implemented recreational marijuana legalization during the study period.
3.2. Regression results
Based on difference-in-difference regressions, Figure 2 reports predicted percentage changes in number of opioid prescriptions associated with recreational marijuana legalization (detailed regression results available in Supplemental File Tables S3 and S42). In Model A that compared among eight states and DC with recreational marijuana legalization, recreational marijuana legalization was not associated with number of prescriptions, total doses, or spending of Schedule II opioids. However, having recreational marijuana legalization effective in 2015 was associated with reductions in number of prescriptions, total doses, and spending of Schedule III opioids by 32% (95% CI: (−49%, −15%), p=0.003), 30% ((−55%, −4.4%), p=0.027), and 31% ((−59%, −3.6%), p=0.031) respectively. In Model B that compared eight states and DC to six states with medical marijuana legalization, recreational marijuana legalization was not associated with any Schedule II or Schedule III opioid outcome.
Figure 2.
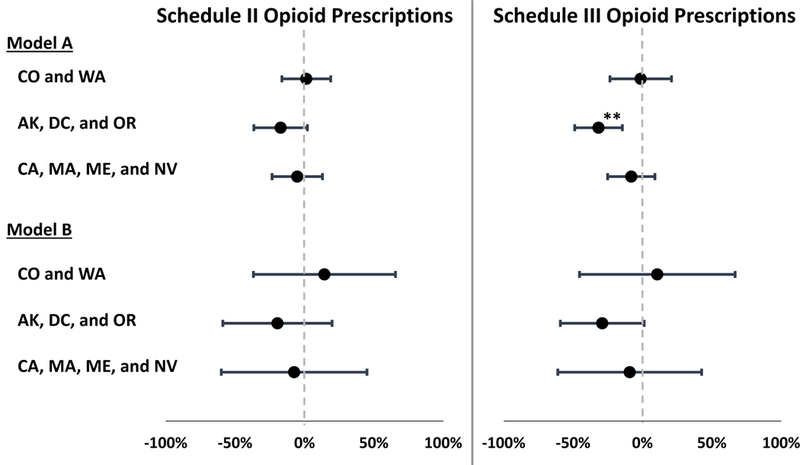
Percentage Changes in Number of Opioid Prescriptions Associated with the Implementation of Recreational Marijuana Legalization. **p<01, Error bars represent 95% confidence intervals estimated from the linear regressions., Notes: In addition to DC, 8 states that implemented recreational marijuana legalization during the study period included AK, CA, CO, ME, MA, NV, OR, and WA. Model A compared among 8 states and DC. Model B compared 8 states and DC to 6 states that had implemented medical marijuana legalization as of January 1st, 2010 but had not implemented recreational marijuana legalization during the study period (HI, MI, MT, NM, RI, VT). All regressions also controlled for medical marijuana legalization in effect, prescription drug monitoring program in effect, Medicaid expansion as part of affordable care act, median household income, poverty rate, unemployment rate, state indicators, year indicators, quarter indicators, and state-specific linear time trends. Standard Errors were clustered at state level. See detailed regression results in Supplemental Tables S3 and S44.
3.3. Sensitivity analyses results
Removing observations after 3rd quarter of 2016 did not alter the results (Supplemental Table S53). Our results were also robust to the rescheduling of Hydrocodone-combination drugs (Supplemental Table S63). After removing state-specific time trends, coefficients of recreational marijuana legalization became significantly negative in some model specifications, but the overall results did not differ from the main results (Supplemental Table S73). The associations between recreational marijuana legalization and number of prescriptions in the four drug classes were all nonsignificant in falsification tests (results not shown).
4. Discussion
Using eight-year quarterly data on prescription opioids received by Medicaid enrollees in the US, the study added to the still limited literature about the impacts of recreational marijuana legalization on opioid use. It enhanced internal validity by adding comparison states and controlling for multiple confounders that were absent in previous research (Livingston et al., 2017), such as presence of prescription drug monitoring program, Medicaid expansion. It also enhanced generalizability by investigating all states legalizing recreational marijuana in the US.
We found no evidence to support the concern that recreational marijuana legalization increased opioid prescriptions received by Medicaid enrollees. Instead, there was some evidence in some model specifications that the legalization might be associated with reduction in Schedule III opioids in states that implemented legalization in 2015 (Alaska, DC, and Oregon). It appeared that, if the hypotheses about marijuana’s substitution effect and gateway effect on opioid use are both valid, the gateway effect of marijuana did not outweigh its substitution effect. Another possibility is that the hypothesis about marijuana’s gateway effect lacks support. Unfortunately, we were not able to directly assess these mechanisms in this study.
It is not clear why two comparisons yielded slightly different results. Both models have advantages and limitations. The treatment and comparison states in the first model comparing among eight states and DC were more comparable, as they all had adopted recreational marijuana legalization at some time points. On the other hand, the second model comparing eight states and DC to six states with medical marijuana legalization had a larger sample size to detect statistical significance. We therefore chose to report findings in both comparisons. Irrespective of their slight differences, the core findings from the two comparisons were consistent that recreational marijuana legalization did not increase prescription opioids received and most coefficients for the outcome variables were nonsignificant.
In accordance with our previous study on medical marijuana legalization and prescription opioids received by Medicaid enrollees (Liang et al., 2018), the association between recreational marijuana legalization and reduction in prescription opioids seemed to be only evident in some models for Schedule III opioids but not for Schedule II opioids. Because this line of research only emerged recently, the explanation for the differential associations remains unknown. As discussed in our previous study (Liang et al., 2018), we hypothesized that such differences may be partly attributable to the differences in clinical practice and drug efficacy between the two drug classes. According to Controlled Schedule Schedules classified by US Drug Enforcement Administration, Schedule II opioids have greater potential for opioid misuse and overdose than Schedule III opioids (DEA, 2018). In clinical practice, Schedule II opioids must be refilled with monthly prescriptions whereas Schedule III opioids are fillable within six months without new prescriptions (DEA, 2018). Receiving regular monitoring and evaluations from physicians, patients prescribed with Schedule II may be less likely to switch to other drugs. Regarding drug efficacy, Schedule III opioids are often used to treat mild to moderate pain symptoms, for which marijuana is suggested to be also effective (NationalAcademies, 2017). But the evidence for marijuana’s efficacy to treat severe pain symptoms is still limited. Patients prescribed with Schedule II opioids might be less likely to receive recommendation from physicians to switch to marijuana. These hypotheses need future research on individual observations to provide empirical support. It is also worth noting that despite large effect size detected for Schedule III opioids in terms of percentage point reduction (~30% in some states), the absolute level of opioid prescribing rates was low for this drug class (less than one opioid prescription dispensed per quarter per 100 enrollees). The impact of the legalization converted to absolute levels was modest.
This study has limitations primarily related to data availability. First, we evaluated the implementation of legalization instead of commercialization (permitting retail sale of marijuana). Because several states did not open retail markets during our study period, our results may be biased toward the null. Second, despite the size of state-level observations is larger in this study than previous research, our study sample is still small and some statistically nonsignificant associations may simply reflect the lack of statistical power. Particularly, observations in postlegalization period were limited for states implementing legalization in 2016/7. Third, we were not able to explore why states implementing legalization at different time points may demonstrate differential changes in opioid prescriptions. Fourth, we grouped states based on their law implementation dates. However, the states implementing the legalization on the same dates may have opened their retail markets on different dates (e.g., Colorado and Washington). We were not able to identify the degree of marijuana commercialization in each state or evaluate the independent impacts of commercialization because of limited sample size. Further, similar to other state-level investigations of aggregate data, we were not able to explore causal mechanisms of the findings at individual level. Particularly, the hypotheses about substitution and gateway effects of marijuana cannot be directly tested. Additionally, the outcomes analyzed in this study represented opioid prescribing but not patients’ legitimate use or misuse of prescription opioids. Finally, the findings may not be generalizable to opioids dispensed in non-outpatient settings or to the general population. The findings represented a limited number of states in the US but may not be generalizable to other states in the US or to population in other countries.
5. Conclusions
Our findings suggested that legalizing recreational marijuana did not lead to discernable increase in prescription opioids received by Medicaid enrollees. There was some evidence in some states that recreational marijuana legalization may be associated with reduction in Schedule III prescription opioids. Future investigation is needed to validate the findings after full commercialization is realized.
Supplementary Material
Highlights.
Recreational marijuana has been legalized in eight states and DC.
Recreational marijuana legalization did not increase opioid prescriptions.
Recreational marijuana legalization may have reduced Schedule III opioids.
Acknowledgements
The authors thank Kun Zhang at Centers for Disease Control and Prevention for providing conversion table for oral morphine milligram equivalents.
Role of the Funding Source
This research was supported by grant R01DA042290 (PI: Shi) from the National Institute on Drug Abuse. Yuhua Bao was supported by a pilot grant from the Center for Health Economics of Treatment Interventions for Substance Use Disorder, HCV, and HIV, a National Institute on Drug Abuse Center of Excellence (P30DA050500). This article is the sole responsibility of the authors and does not reflect the views of the National Institute on Drug Abuse.
Footnotes
Conflict of Interest
The authors declared no conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Angrist JD, Pischke J-S, 2008. Mostly harmless econometrics: An empiricist’s companion. Princeton University Press, Princeton. [Google Scholar]
- Austen I, 2017. Ready or Not, Recreational Marijuana Use Is Coming to Canada. Accessed on April 1, 2018. https://www.nytimes.com/2017/11/04/world/canada/canada-marijuana-legal-justin-trudeau.html.
- Aydelotte JD, Brown LH, Luftman KM, Mardock AL, Teixeira PGR, Coopwood B, Brown CVR, 2017. Crash fatality rates after recreational marijuana legalization in Washington and Colorado. Am. J. Public Health 107, 1329–1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bachhuber MA, Saloner B, Cunningham CO, Barry CL, 2014. Medical cannabis laws and opioid analgesic overdose mortality in the United States, 1999–2010. JAMA Intern. Med. 174, 1668–1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birnbaum HG, White AG, Schiller M, Waldman T, Cleveland JM, Roland CL, 2011. Societal costs of prescription opioid abuse, dependence, and misuse in the United States. Pain Med. 12, 657–667. [DOI] [PubMed] [Google Scholar]
- Borchardt D, 2017. Sean Spicer Wrongly Links Recreational Marijuana With Opioid Crisis. Available at https://www.forbes.com/sites/debraborchardt/2017/02/23/sean-spicer-wrongly-links-recreational-marijuana-with-opioid-crisis/#39523c943ea9. Accessed on July 3, 2018. Archived at WebCite http://www.webcitation.org/70e3hjv5o.
- Bradford AC, Bradford WD, 2016. Medical marijuana laws reduce prescription medication use in Medicare Part D. Health Affairs 35, 1230–1236. [DOI] [PubMed] [Google Scholar]
- Bradford AC, Bradford WD, 2017. Medical marijuana laws may be associated with a decline in the number of prescriptions for Medicaid enrollees. Health Affairs 36, 945–951. [DOI] [PubMed] [Google Scholar]
- Bradford AC, Bradford WD, Abraham A, Adams GB, 2018. Association between US state medical cannabis laws and opioid prescribing in the Medicare Part D population. JAMA Intern. Med. 178, 667–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bureau of Labor Statistics (BLS), 2018. Local Area Unemployment Statistics. Available from https://www.bls.gov/web/laus/laumstrk.htm. Accessed on 2018–04-30. Archived by WebCite at http://www.webcitation.org/6z51qzpRV.
- Center for Disease Control and Prevention (CDC), 2016. National Center for Injury Prevention and Control CDC compilation of benzodiazepines, muscle relaxants, stimulants, zolpidem, and opioid analgesics with oral morphine milligram equivalent conversion factors, 2016 version. Atlanta, GA: Centers for Disease Control and Prevention, Atlanta Georgia; http://www.pdmpassist.org/pdf/BJA_performance_measure_aid_MME_conversion.pdf. [Google Scholar]
- Cerda M, Wall M, Feng T, Keyes KM, Sarvet A, Schulenberg J, O’Malley PM, Pacula RL, Galea S, Hasin DS, 2017. Association of state recreational marijuana laws with adolescent marijuana use. JAMA Pediatrics 171, 142–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Medicare and Medicaid Services (CMS), 2018. Medicaid State Drug Utilization Data. Accessed on 2018–04-30. https://www.medicaid.gov/medicaid/prescription-drugs/state-drug-utilization-data/index.html.
- Centers for Medicare and Medicaid Services (CMS), 2017. Medicaid Managed Care Enrollment Report. Accessed on 2018–04-30. https://www.medicaid.gov/medicaid/managed-care/enrollment/index.html.
- Dasgupta N, Beletsky L, Ciccarone D, 2018. Opioid crisis: No easy fix to its social and economic determinants. Am. J. Public Health 108, 182–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Human Health Services (DHHS), 2012. States’ collection of rebates for drugs paid through Medicaid managed care organizations. https://oig.hhs.gov/oei/reports/oei-03-11-00480.pdf. Department of Health and Human Services, Washington, D.C. [Google Scholar]
- Drug Enforcement Agency (DEA), 2018. Controlled Substance Schedules. Available from Accessed on 2018–04-30. https://www.deadiversion.usdoj.gov/schedules.
- Drug Enforcement Agency (DEA), 2018. Prescriptions: Questions and Anwers. Accessed on 2018–04-30. Available from https://www.deadiversion.usdoj.gov/faq/prescriptions.htm.
- Drug Enforcement Agency (DEA), 2014. Schedules of Controlled Substances: Rescheduling of Hydrocodone Combination Products From Schedule III to Schedule II Accessed 2018–04-30. Available from https://www.deadiversion.usdoj.gov/fed_regs/rules/2014/fr0822.htm. [PubMed]
- Dowell D, Haegerich TM, Chou R, 2016. CDC guideline for prescribing opioids for chronic pain—United States, 2016. JAMA 315, 1624–1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drash W, Merica D, 2017. Trump: ‘The opioid crisis is an emergency’. Accessed on 2018–04-30. Available from http://www.cnn.com/2017/08/10/health/trump-opioid-emergency-declaration-bn/index.html.
- Fischer B, Keates A, Buhringer G, Reimer J, Rehm J, 2013. Non-medical use of prescription opioids and prescription opioid-related harms: why so markedly higher in North America compared to the rest of the world? Addiction (Abingdon, England) 109(2), 177–181. [DOI] [PubMed] [Google Scholar]
- Food and Drug Administration (FDA), 2017. Approved Drug Products with Therapeutic Equivalence Evaluations (Orange Book). Food and Drug Administratio, Silver Spring, MD. [Google Scholar]
- Kerr DCR, Bae H, Phibbs S, Kern AC, 2017. Changes in undergraduates’ marijuana, heavy alcohol and cigarette use following legalization of recreational marijuana use in Oregon. Addiction 112, 1992–2001. [DOI] [PubMed] [Google Scholar]
- Henry J Kaiser Family Foundation (KFF), 2018. Status of State Action on the Medicaid Expansion Decision. Accessed on 2018–04-30. https://www.kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act.
- Kim JH, Santaella-Tenorio J, Mauro C, Wrobel J, Cerda M, Keyes KM, Hasin D,Martins SS, Li G, 2016. State medical marijuana laws and the prevalence of opioids detected among fatally injured drivers. Am J. Public Health 106, 2032–2037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawatlas, 2018. Recreational Marijuana Laws. Available at Accessed on 2018–04-30. http://lawatlas.org/datasets/recreational-marijuana-laws.
- Liang D, Bao Y, Wallace M, Grant I, Shi Y, 2018. Medical cannabis legalization and opioid prescriptions: Evidence on US Medicaid enrollees during 1993–2014. doi: 10.1111/add.14382. Addiction 113, 2060–2070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livingston MD, Barnett TE, Delcher C, Wagenaar AC, 2017. recreational cannabis legalization and opioid-related deaths in Colorado, 2000–2015. Am. J. Public Health 107, 1827–1829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez G, 2018. Jeff Sessions: Marijuana helped cause the opioid epidemic. The research: No. Accessed on July 3, 2018. https://www.vox.com/policy-and-politics/2018/2/8/16987126/jeff-sessions-opioid-epidemic-marijuana.
- Lucas P, 2012. Cannabis as an adjunct to or substitute for opiates in the treatment of chronic pain. J. Psychoactive Drugs 44, 125–133. [DOI] [PubMed] [Google Scholar]
- Lucas P, Reiman A, Earleywine M, McGowan SK, Oleson M, Coward MP, Thomas B, 2013. Cannabis as a substitute for alcohol and other drugs: A dispensary-based survey of substitution effect in Canadian medical cannabis patients. Addict. Res. Theory 21, 435–442. [Google Scholar]
- Lucas P, Walsh Z, 2017. Medical cannabis access, use, and substitution for prescription opioids and other substances: A survey of authorized medical cannabis patients. Int. J. Drug Policy 42, 30–35. [DOI] [PubMed] [Google Scholar]
- Mack KA, Zhang K, Paulozzi L, Jones C, 2015. Prescription practices involving opioid analgesics among Americans with Medicaid, 2010. J. Health Care Poor Underserved 26, 182–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meer J, West J, 2015. Effects of the minimum wage on employment dynamics. J. Hum. Resour. 51, 500–522. [Google Scholar]
- Merica D, 2017. Trump declares opioid epidemic a national public health emergency. Accessed on 2018–04-30. http://www.cnn.com/2017/10/26/politics/donald-trump-opioid-epidemic/index.html.
- Miroff N, 2017. In Uruguay’s marijuana experiment, the government is your pot dealer. Accessed on April 1, 2018. https://www.washingtonpost.com/world/the_americas/in-uruguays-marijuana-experiment-the-government-is-your-pot-dealer/2017/07/07/6212360c-5a88-11e7-aa69-3964a7d55207_story.html?noredirect=on&utm_term=.e68ce4e3d21e.
- National Academies, 2017. The health effects of cannabis and cannabinoids: The current state of evidence and recommendations for research. National Academies Press, National Academies of Sciences, Engineering, Medicine. [PubMed] [Google Scholar]
- Olfson M, Wall MM, Liu SM, Blanco C, 2018. Cannabis use and risk of prescription opioid use disorder in the United States. Am. J. Psychiatry 175, 47–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell D, Pacula RL, Jacobson M, 2018. Do medical marijuana laws reduce addictions and deaths related to pain killers? J. Health Econ. 58, 29–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiman A, 2009. Cannabis as a substitute for alcohol and other drugs. Harm Reduct. J. 6, 35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi Y, 2017. Medical marijuana policies and hospitalizations related to marijuana and opioid pain reliever. Drug Alcohol Depend. 173, 144–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shmagel A, Foley R, Ibrahim H, 2016. Epidemiology of chronic low back pain in US adults: Data From the 2009–2010 National Health and Nutrition Examination Survey. Arthritis Care Res. 68, 1688–1694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Census Bureau, 2017. Historical Poverty Tables: People and Families - 1959 to 2016. Available from https://www.census.gov/data/tables/time-series/demo/income-poverty/historical-poverty-people.html. Accessed on 2018–04-30. Archived by WebCite at http://www.webcitation.org/6z51yO3Nm.
- Volkow ND, 2016. America’s addiction to opioids: Heroin and prescription drug abuse. Accessed on 2018–04-30. https://www.drugabuse.gov/about-nida/legislative-activities/testimony-to-congress/2016/americas-addiction-to-opioids-heroin-prescription-drug-abuse.
- Warner M, Hedegaard H, Chen LH, 2014. Trends in drug-poisoning deaths involving opioid analgesics and heroin: United States, 1999–2012. Centers for Disease Control and Prevention. [PubMed] [Google Scholar]
- Wen H, Schackman BR, Aden B, Bao Y, 2017. States with prescription drug monitoring mandates saw a reduction in opioids prescribed to medicaid enrollees. Health Affairs 36, 733–741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfers J, 2006. Did unilateral divorce laws raise divorce rates? A reconciliation and new results. Am. Econ. Rev. 96, 1802–1820. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


