Abstract
The Agency for Healthcare Research and Quality conducted internal work to formulate a model that could be used to analyze the Agency’s research portfolio, identify gaps, develop and prioritize its research agenda, and evaluate its performance. Existing models described the structure and components of the healthcare system. Instead, we produced a model of two functions: caring and learning. Central to this model is the commitment to and participation of people—patients, communities, and health professionals—and the organization of systems to respond to people’s problems using evidence. As a product of caring, the system produces evidence that is then used to adapt and continuously improve this response, closely integrating caring and learning. The Agency and the health services research and improvement communities can use this Care and Learn Model to frame an evidence-based understanding of vexing clinical, healthcare delivery, and population health problems and to identify targets for investment, innovation, and investigation.
KEY WORDS: health services research, healthcare delivery, health policy, evidence-based medicine, quality improvement
Healthcare in the USA often falls short of achieving the objectives of improving individual and population health1. Too often, quality is suboptimal and care is fragmented, difficult to navigate, and burdensome.2, 3 The mission of the Agency for Healthcare Research and Quality (AHRQ) is to produce evidence to make healthcare safer, of higher quality, more accessible, equitable, and affordable, and to work within the US Department of Health and Human Services and with other partners to make sure that this evidence is understood and used.4 AHRQ generates and synthesizes knowledge, translates science on what works in health and healthcare delivery, and catalyzes practice improvement to foster healthcare quality. AHRQ is unique among federal agencies. Its research focuses on “whole person care,” in other words, on person-centered care that addresses all of an individual’s health needs, aligned with their values, preferences, and goals in the context of their lives and the communities in which they live. AHRQ’s research is aimed at supporting learning health systems to apply and generate evidence to continually improve the quality and outcomes of care.
The purpose of this special article is to propose a model of the healthcare system, the result of internal work at AHRQ. It was designed to describe the functions of the healthcare system that the work of the Agency could inform and improve. When used, the model should help the Agency and the health services research and improvement communities identify research and improvement opportunities, evaluate existing programs, inform priority setting, and develop effective responses to the evolving needs of a rapidly changing healthcare landscape.
METHOD
Over several workshops, AHRQ program staff considered existing and potentially useful models. Existing models focused on one experience, one part of the system, or one type of patient. Some models described people in their social context (e.g., the Social Ecological model5 with its concentric circles); others described the interacting components of a healthcare system (the activated patient, the proactive team, information technology, and community as components of the Chronic Care Model,6 for example), but none were deemed sufficient for our purpose.
Working in small groups, staff identified and explored essential components of a model and organized them iteratively, testing the evolving models against AHRQ programs. The process continued until a consensus model emerged that effectively supported (a) the identification of diverse areas of need, and (b) the organization of existing and planned programs in healthcare improvement and research.
MODEL ELEMENTS
This work resulted in a model connecting two broad functions of the healthcare system as it interacts with people and their contexts to address problematic situations with evidence: a caring function and a learning function. This two-function model departs from prior models that describe the structure and components of the healthcare system. Those models focus on the flow of information or other resources through the system or the arrangement of organizations and offices. Instead, we found it useful to produce a model of healthcare functions. This is particularly useful at a time of rapid change in healthcare in which structures (e.g., primary care medical homes, medical neighborhoods, accountable care organizations) appear, change, and disappear while the need for the functions that they serve frequently remains. The model shows healthcare responding to problematic situations and learning from its experience to improve future responses and adapt to new circumstances.7
The purpose of this model is to ground AHRQ and health services research efforts in the core functions of healthcare. It can be adapted to encompass the wide range of problematic situations—affecting individuals or populations, practices or healthcare systems—to which healthcare must respond. These include (a) how to organize and deliver patient care, (b) how to attend to the needs of underserved populations, and (c) how to individualize care and support self-care. The system must deliver care that is safe and effective, efficient and equitable, timely, coordinated and integrated, and patient-centered. It must do this well for all, and for special populations, such as people who live with multiple chronic conditions, the socioeconomically disadvantaged, institutionalized, children and adolescents, and those at the end of their life.8 The system must also respond to the challenges of ensuring continuity of care (over time and within the healthcare system), and integrating primary care with public health and community-based programs that promote health and well-being.9
Healthcare should improve the chances that people—patients and populations—will live healthy lives and receive appropriate healthcare to support their health goals. It is people then, all people both healthy and ill, families, caregivers, communities and populations, who are at the center of the model.
People in Context
People spend almost all of their time in their personal, social, and community contexts in which primary determinants of health operate.10 These contexts (a) influence health, (b) mediate the effects of healthcare, (c) promote or hinder access to and use of healthcare services, and (d) promote or hinder self-care. Entities such as churches and clubs, community-based governmental and nongovernmental services, neighbors, and extended families help attend to basic needs, recreation, education, housing, nutrition, or safety. Therefore, it is not sufficient for a healthcare model to depict only healthcare entities. The model instead recognizes and integrates the social contexts in which people live and face and solve health problems, and with which healthcare must interact to improve health.
People in Healthcare
The central interaction the model depicts is between the healthcare system and people. People interact with the healthcare system when they are healthy (for some forms of prevention, to give birth), when they are sick or injured (for diagnosis, treatment, and alleviation of pain and suffering), when they live with chronic conditions (for ongoing management, self-management support, technical problem-solving), and when they are at the end of life (for intensive, palliative, or hospice care). The model presents personnel, information, policies, and resources as organized to respond to the problems people have. Those problematic situations are not just conditions, but also social and life circumstances that influence a person’s ability to respond productively.
Health Professionals
In addition, healthcare’s response requires the work of health professionals, caring individually within interdisciplinary care teams functioning within a healthcare system and within the culture of its organizations. For healthcare to succeed, it is critically important that clinical, administrative, and support staff be engaged cognitively and emotionally in ensuring that healthcare responds properly. The system’s ability to respond to situations is limited, however, when health professionals are scarce, under-trained, burned-out, or impaired.11 Thus, people—those caring and those receiving care—must remain at the center of our model.
Evidence
A persistent frustration among observers of healthcare innovation is the implementation of “solutions” without evidence review to assess their value before implementation or proper evaluation afterwards. This is unscientific and wasteful.12 Instead, the model assumes that the practice routines and learning processes of healthcare should reflect the body of pertinent research evidence. This evidence must be drawn from biomedical, clinical, and health services research (including implementation science) that is produced routinely and in a collaborative and transparent fashion during the work of healthcare.13 Most needed is evidence about the effectiveness of interventions, of delivery approaches that best support their implementation, and of the strategies for health systems improvement. Health systems must collect and analyze data, observational and experimental, to generate evidence that fills knowledge gaps and fosters continuous learning.14 In this way, the model depicts the healthcare system as both a user and generator of evidence to effectively address the situation of persons. This response involves organizing people, information, resources, and policies. Also, the healthcare system must evaluate the way it responds and it must disseminate evidence about its performance and outcomes, thus contributing to the adaptation and improvement of care.
A TWO-FUNCTION MODEL
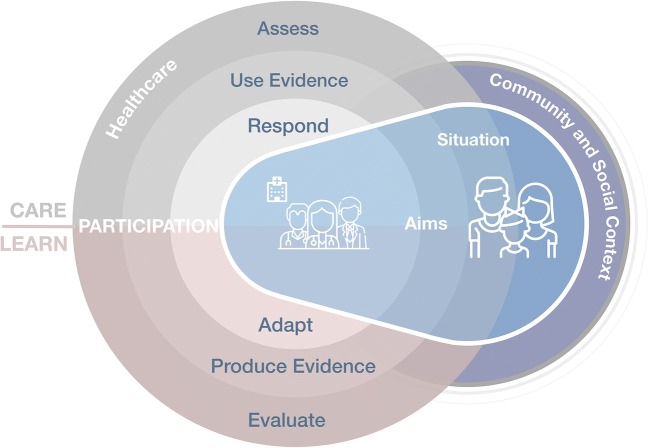
Taken together, the model depicts a caring-and-learning healthcare system, centered on the aims of people and addressing their particular situations. The system serves as an evidence-based resource from which people can draw to achieve health and wellness. The system responds to improve health and the experiences of care for patients and clinicians, or to achieve other more specific outcomes. Performance on these goals, at different points in time and over time, provides feedback to the system, which must care, adapt, and learn. Figure 1 depicts the resulting Care and Learn Model. Table 1 describes each of the model’s components.
Figure 1.
The Care and Learn Model. The two key functions of the system are to care and to learn. Caring starts in response to a problematic situation affecting people (a healthy or sick person or population). The healthcare system must gather information to assess the situation, identify appropriate evidence, and organize a response. The response, using evidence-based practice, entails organizing and mobilizing people, information, and processes, taking into account the community and social contexts. Learning is a continuous function of the system by which all responses are evaluated according to aims relevant to the situation and deemed important by key stakeholders. This evaluation produces practice-based evidence from which stakeholders must draw to adapt healthcare’s response to people’s problematic situations. The model hinges on the participation of people needing care and those responding with care, on the ongoing engagement in the functions of caring and learning, and on their commitment to achieving the aims of these functions.
Table 1.
Descriptions of the Terms Used in the Care and Learn Model
| Term | Description |
|---|---|
| Situation | A problem significant enough that it warrants action |
| Participation | Relationships by which people contribute to advancing the situation toward its resolution |
| Aims | The resolution sought through clinical care or population health interventions |
| Care | The production of action (e.g., treatment) that responds appropriately to the situation |
| Assess | The process of developing sufficient understanding of the situation to discover which aspects demand action |
| Use evidence | The judicious application of the best available research to assess and respond to the situation in a manner that optimizes the aims |
| Respond | The organization of people, information, policies, and resources to address the situation and achieve aims |
| Learn | The production of new insight into the nature and significance of problems and the adequacy of care |
| Evaluate | The process of contrasting achievements of responding to the situation with the aims of that response |
| Produce evidence | The rigorous capture and use of data and experiences produced in the course of responding to the situation to evaluate and improve the response to achieve its aims |
| Adapt | The process of changing the existing response to optimize its ability to achieve aims |
USING THE CARE AND LEARN MODEL TO GUIDE HEALTH SERVICES RESEARCH AND IMPROVEMENT
As described above, we developed this model to inform the evolution of AHRQ’s research agenda, priorities, and programs, to develop a balanced portfolio of research, and to guide the advancement of learning healthcare organizations. Yet, the health services research and improvement communities can use this model to frame an evidence-based understanding of vexing clinical, healthcare delivery, and population health problems and to identify target points for investment, investigation, implementation, and improvement.
Consider, for example, how the model might be applied to the challenges healthcare faces in responding to patients with multimorbidity. The research enterprise and the healthcare system are often successful at addressing the diagnosis and treatment of patients with individual conditions. As the prevalence of multimorbidity increases, not just among the elderly, evidence demonstrates that usual care falls short of responding well to persons with multiple chronic conditions.15 Aiming at improving disease-specific targets and shuttling patients across uncoordinated specialty care appointments often fails to advance patient goals (which frequently remain undisclosed) and may lead to unintended harm from disease-treatment and treatment-treatment adverse interactions (evaluate). Since multimorbidity disproportionately affects disadvantaged people,16 these patients have fewer resources to overcome the difficulties created by inadequate healthcare responses to their problematic situations. The result is an overwhelming burden of treatment that results in poor fidelity to treatments and poor health outcomes (assess).17 There are massive research needs related to this situation. How might we best assess the goals and needs of complex patients with multimorbidity? How might we judiciously use evidence—much of which has excluded patients with multiple chronic conditions—to inform their care? How might we break silos, bring coherence to disparate clinical guidelines, and coordinate care to prevent unintentional harm and reduce the healthcare workload delegated to patients and caregivers (respond)? How might we evaluate the impact of new models of care designed to meet the needs of patients with multimorbidity and measure their effect on people’s ability to cope and thrive? How might we characterize, in clinical and “big data” repositories, outcomes in people with different multimorbidity profiles, recognize people at risk of becoming overwhelmed by care, and identify strategies to improve outcomes (produce evidence)? How might we ensure the participation in care of overwhelmed patients and caregivers? How might we organize and support the work that health professionals and community health workers do together to advance the situation of these patients (adapt)?
The Care and Learn Model grounds the design, conduct, and evaluation of research, implementation, and improvement programs on the problems of caring for people and learning from that experience. This stance calls for a closer integration of the research enterprise with the healthcare delivery systems. In this way, it resonates with other models proposed to describe the so-called learning healthcare system that also seek to improve health outcomes, the experience of giving and receiving care, and the use of resources necessary to achieve these results.18, 19 These learning healthcare system models often place information and delivery systems at their core. In contrast, the Care and Learn Model is organized by the functions of healthcare required to respond carefully to the problems of patients, and ultimately by the people who contribute to, and draw upon these functions.
Because the Care and Learn model is functional, it supports a dynamic and iterative approach to improving the organization and delivery of healthcare, providing insights about how to use and tailor interventions to align them with needs and resources.20 Because of its flexible, dynamic, and multi-function nature, AHRQ, as a research funder, can use this model to critically appraise and balance its research portfolio as a whole and in specific programmatic areas, identify gaps, develop and prioritize its research agenda, and evaluate the outcomes of its work. For example, the model can help AHRQ respond to the challenges of providing optimal care to patients with multiple chronic conditions by identifying high-priority areas of research, such as how best to support the critical role of primary care in delivering and coordinating person-centered care. The model can be used to help AHRQ identify the data, tools, and resources that are most effective at enhancing healthcare’s ability to respond to the needs of patients and populations. It can also guide AHRQ’s efforts to go beyond the production of research reports for researchers and target the dissemination of research results to decision-makers to foster learning and caring health systems.
NEXT STEPS
As our society struggles with how best to improve care while managing its costs, the model offers a way forward. In connecting the functions of caring and learning, applications of this model may improve care by promoting the use of evidence and evaluation to determine which interventions to implement and which to discontinue. The proof of the utility of this model rests with its ability to support decision-makers as they integrate evidence-based care and practice-based evidence to respond—and adapt this response—to the evolving needs of people.
Compliance with Ethical Standards
Disclaimer
The views expressed in this article are those of the authors, who are responsible for its content, and do not necessarily represent the views of AHRQ. No statement in this article should be construed as an official position of AHRQ or of the US Department of Health and Human Services.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
References
- 1.Davis K, Stremikis K, Schoen C, Squires D. Mirror, Mirror on the Wall, 2014 Update: How the U.S. Health Care System Compares Internationally. The Commonwealth Fund; 2014.
- 2.Stange KC. The problem of fragmentation and the need for integrative solutions. Ann Fam Med. 2009;7(2):100–103. doi: 10.1370/afm.971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Agency for Healthcare Research and Quality. Overview of Quality and Access in the U.S. Health Care System. 2017. https://www.ahrq.gov/research/findings/nhqrdr/nhqdr16/overview.html. Accessed Dec 2017.
- 4.Agency for Healthcare Research and Quality. Mission and Budget. 2017; https://www.ahrq.gov/cpi/about/mission/index.html, 2017.
- 5.Stokols D. Establishing and maintaining healthy environments. Toward a social ecology of health promotion. Am Psychol. 1992;47(1):6–22. doi: 10.1037/0003-066X.47.1.6. [DOI] [PubMed] [Google Scholar]
- 6.Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving chronic illness care: translating evidence into action. Health Aff (Millwood) 2001;20(6):64–78. doi: 10.1377/hlthaff.20.6.64. [DOI] [PubMed] [Google Scholar]
- 7.Bindman AB. The Agency for Healthcare Research and Quality and the Development of a Learning Health Care System. JAMA Intern Med. 2017;177(7):909–910. doi: 10.1001/jamainternmed.2017.2589. [DOI] [PubMed] [Google Scholar]
- 8.Institute of Medicine . Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: The National Academies Press; 2001. [PubMed] [Google Scholar]
- 9.Integrating Primary Care Practices and Community-based Resources to Manage Obesity. 2014. http://www.ahrq.gov/professionals/prevention-chronic-care/improve/community/obesity-pcpresources/index.html.
- 10.Adler N, Cutler D, Jonathan J, Galea S, Glymour M, Koh H, Satcher D. Addressing Social Determinants of Health and Health Disparities. Discussion Paper. Washington, DC: National Academy of Medicine;2016.
- 11.Shanafelt TD, Dyrbye LN, West CP, Sinsky CA. Potential Impact of Burnout on the US Physician Workforce. Mayo Clin Proc. 2016;91(11):1667–1668. doi: 10.1016/j.mayocp.2016.08.016. [DOI] [PubMed] [Google Scholar]
- 12.Ioannidis JP. Stealth research: is biomedical innovation happening outside the peer-reviewed literature? JAMA. 2015;313(7):663–664. doi: 10.1001/jama.2014.17662. [DOI] [PubMed] [Google Scholar]
- 13.Montori VM. Big Science for patient centred care. BMJ. 2017;j5600:359. doi: 10.1136/bmj.j5600. [DOI] [PubMed] [Google Scholar]
- 14.Atkins D, Kilbourne AM, Shulkin D. Moving From Discovery to System-Wide Change: The Role of Research in a Learning Health Care System: Experience from Three Decades of Health Systems Research in the Veterans Health Administration. Annu Rev Public Health. 2017;38:467–487. doi: 10.1146/annurev-publhealth-031816-044255. [DOI] [PubMed] [Google Scholar]
- 15.Grembowski D, Schaefer J, Johnson KE, Fischer H, Moore SL, Tai-Seale M, Ricciardi R, Fraser JR, Miller D, LeRoy L, Network AMR A conceptual model of the role of complexity in the care of patients with multiple chronic conditions. Med Care. 2014;52(Suppl 3):S7–S14. doi: 10.1097/MLR.0000000000000045. [DOI] [PubMed] [Google Scholar]
- 16.Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380(9836):37–43. doi: 10.1016/S0140-6736(12)60240-2. [DOI] [PubMed] [Google Scholar]
- 17.Gallacher K, Jani B, Morrison D, Macdonald S, Blane D, Erwin P, May CR, Montori VM, Eton DT, Smith F, Batty GD, Mair FS, International Minimally Disruptive Medicine W Qualitative systematic reviews of treatment burden in stroke, heart failure and diabetes - methodological challenges and solutions. BMC Med Res Methodol. 2013;13:10. doi: 10.1186/1471-2288-13-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bindman AB, Pronovost PJ, Asch DA. Funding Innovation in a Learning Health Care System. JAMA. 2018;319(2):119–120. doi: 10.1001/jama.2017.18205. [DOI] [PubMed] [Google Scholar]
- 19.Maddox TM, Albert NM, Borden WB, Curtis LH, Ferguson TB, Jr, Kao DP, Marcus GM, Peterson ED, Redberg R, Rumsfeld JS, Shah ND, Tcheng JE, American Heart Association Council on Quality of C, Outcomes R, Council on Cardiovascular Disease in the Y, Council on Clinical C, Council on Functional G, Translational B, Stroke C The Learning Healthcare System and Cardiovascular Care: A Scientific Statement From the American Heart Association. Circulation. 2017;135(14):e826–e857. doi: 10.1161/CIR.0000000000000480. [DOI] [PubMed] [Google Scholar]
- 20.Pfadenhauer LM, Gerhardus A, Mozygemba K, Lysdahl KB, Booth A, Hofmann B, Wahlster P, Polus S, Burns J, Brereton L, Rehfuess E. Making sense of complexity in context and implementation: the Context and Implementation of Complex Interventions (CICI) framework. Implement Sci. 2017;12(1):21. doi: 10.1186/s13012-017-0552-5. [DOI] [PMC free article] [PubMed] [Google Scholar]