Abstract
Introduction
Surgical site infiltration with bupivacaine results in short-lived analgesia. The MATRIX-1 and MATRIX-2 studies examined the efficacy and safety of the bioresorbable bupivacaine HCl collagen-matrix implant (INL-001) for postsurgical pain after open inguinal hernia repair. INL-001, designed to provide early and extended delivery of bupivacaine, provides prolonged duration of perioperative analgesia.
Methods
In two phase 3 double-blind studies [MATRIX-1 (ClinicalTrials.gov identifier, NCT02523599) and MATRIX-2 (ClinicalTrials.gov identifier, NCT02525133)], patients undergoing open tension-free mesh inguinal hernia repair were randomized to receive 300-mg bupivacaine (three INL-001 100-mg bupivacaine HCl collagen-matrix implants) (MATRIX-1 n = 204; MATRIX-2 n = 213) or three placebo collagen-matrix implants (MATRIX-1 n = 101; MATRIX-2 n = 106) during surgery. Postsurgical medication included scheduled acetaminophen and as-needed opioids.
Results
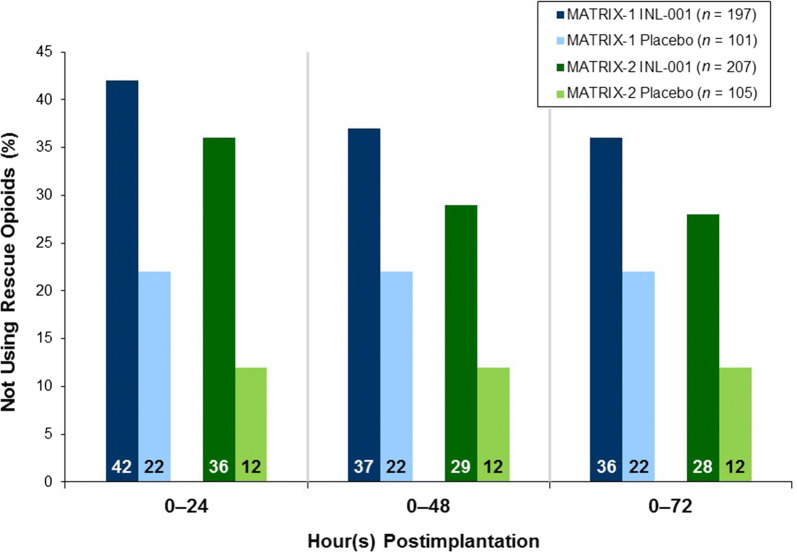
Patients who received INL-001 in both studies reported statistically significantly lower pain intensity (P ≤ 0.004; primary end point) and opioid analgesic use (P < 0.0001) through 24-h post-surgery versus those who received a placebo collagen-matrix. Patients who received INL-001 reported lower pain intensity through 72 h (P = 0.0441) for the two pooled studies. In both studies, more of the patients (28–42%) who received INL-001 used no opioid medication 0–24, 0–48, and 0–72 h post-surgery versus those who received a placebo collagen-matrix (12–22%). Among patients who needed opioid medication, patients receiving INL-001 used fewer opioids than those who received a placebo collagen-matrix through 24 h in both studies (P < 0.0001) and through 48 h in MATRIX-2 (P = 0.0003). Most adverse events were mild or moderate, without evidence of bupivacaine toxicity or deleterious effects on wound healing.
Conclusion
These findings indicate that INL-001 results in post-inguinal hernia repair analgesia that is temporally aligned with the period of maximal postsurgical pain and may reduce the need for opioids while offering a favorable safety profile.
Trial Registration
ClinicalTrials.gov identifiers, NCT02523599; NCT02525133.
Funding
Innocoll Pharmaceuticals.
Plain Language Summary
Plain language summary available for this article.
Keywords: Bupivacaine HCl collagen-matrix implant, INL-001, Postoperative pain intensity, Rescue opioid analgesia
Plain Language Summary
Bupivacaine has been used to manage pain after surgery for many years. Surgical pain can last for days, but pain control only lasts for a few hours with bupivacaine. Therefore, opioid narcotics are often needed to decrease pain after surgery. There are risks of opioid use, including negative side effects and potential for abuse. INL-001 is an implant designed to provide extended delivery of bupivacaine to the area around the surgical wound. The effectiveness and safety of INL-001 were studied in two clinical trials involving patients undergoing hernia repair surgery. These two clinical trials were evaluated both separately and together (combined) to increase the number of patients studied. Patients who received INL-001 in both studies reported significantly lower pain intensity and opioid use through 24 h post-surgery versus those who received an implant without bupivacaine (placebo). When the data from these clinical trials were combined, patients who received INL-001 reported lower pain intensity through 72 h. In both studies, more of the patients receiving INL-001 did not use opioid medication up to 72 h post-surgery versus those administered a placebo. Most side effects seen with INL-001 were mild or moderate. These findings indicate that INL-001 is safe and effective at extending postsurgical pain control and decreasing opioid use for patients undergoing hernia repair surgery.
Introduction
Achieving adequate pain control following surgery is a major concern for patients and physicians. Inadequate acute postsurgical pain control can result in increased patient morbidity or mortality and higher healthcare costs [1–3]. Postsurgical pain is generally most severe during the first 1–3 days after surgery and improves over time [4, 5]. Historically, opioid medication has been the mainstay of postsurgical pain management; however, opioids are associated with well-known risks. Opioids are commonly associated with adverse events (AEs), such as constipation, nausea, and vomiting, and occasionally more serious effects, such as respiratory depression, all of which can negatively impact recovery from surgery [6–8]. Furthermore, use of opioids for as few as 3 days, especially in opioid-naive patients, is associated with risk of long-term use, which can result in tolerance, dependence, and addiction [9, 10].
A desire to limit opioid use and improve postsurgical pain control has led to the development of multimodal approaches to postsurgical pain management [11, 12]. Infiltration of surgical wounds with local anesthetics, such as bupivacaine, has become a widely accepted component of multimodal approaches to the management of acute pain after soft tissue surgery [11–16]. Bupivacaine, however, has a limited duration of effect (4–8 h), a duration that is not well aligned with the temporal profile of maximal postsurgical pain and is dependent primarily on contact with nerves in the surgical wound [17–20]. Various attempts have been made to extend the delivery of bupivacaine to the tissues in the surgical site, such as administration through a catheter with a pump, the addition of epinephrine, and alternative formulations. However, all available bupivacaine formulations are liquid, and each approach presents limitations with respect to administration, analgesic duration, and/or safety [20–24]. Bupivacaine’s most serious safety issue, local anesthetic systemic toxicity (LAST), is most often caused by inadvertent intravascular injection during administration of bupivacaine into the surgical wound and manifests with central nervous system (CNS) and cardiovascular signs and symptoms that can be serious or fatal [20, 21, 25]. Formulations that safely deliver bupivacaine over time into the surgical site for prolonged postsurgical pain are needed.
The bioresorbable bupivacaine HCl collagen-matrix implant (INL-001) is a single-application extended bupivacaine delivery technology designed for the management of acute postsurgical pain associated with soft tissue surgery [26–29]. INL-001 is a combination product consisting of one active moiety, bupivacaine HCl, and a drug delivery component of type I bovine collagen designed to be placed in the surgical site. The type I collagen used in INL-001 is purified from bovine Achilles tendons, which are sourced from closed herds that have been certified as transmissible spongiform encephalopathy free and negligible for the risk of bovine spongiform encephalopathy. Degradation of INL-001 via chemical and enzymatic hydrolysis occurs within 2 months after implantation, as demonstrated in preclinical studies. Bovine type I collagen, which is used in numerous clinical applications, shares a common amino acid structure and surface epitopes with human type I collagen, presenting a negligible risk for an immune response [30–33]. Each bupivacaine HCl collagen-matrix contains 100 mg bupivacaine HCl dispersed evenly within the matrix. INL-001 has been demonstrated to be compatible with common surgical materials, including mesh.
The extended bupivacaine delivery profile of INL-001 was demonstrated via postimplantation plasma concentrations [20]. Use of INL-001 300 mg results in bupivacaine blood levels that are quantifiable within 30 min after implantation and through 96 h (first and last time points measured) in patients undergoing open inguinal hernia repair with mesh [34]. The extended delivery of bupivacaine from INL-001 is further demonstrated by a longer time to maximum plasma concentration (Tmax) and terminal elimination half-life (t1/2) compared with 0.25% bupivacaine HCl 175 mg infiltration (3.0 h vs. 1.0 h and 19.0 h vs. 9.1 h, respectively), with a comparable Cmax (663.4 ng/ml vs. 641.0 ng/ml) [34]. The highest individual plasma bupivacaine concentration reported in the INL-001 development program was 1230 ng/ml, a level well below the ≥ 2000 ng/ml that has been reported to be associated with bupivacaine systemic toxicity [34, 35]. Phase 1 and 2 clinical studies supported the safety and tolerability of INL-001 and found reductions in selected measures of pain intensity (PI) and opioid analgesia use in patients undergoing inguinal hernia repair or hysterectomy [26–29]. Based on dose ranging in these studies, a dose of three implants (300 mg total) was identified to be evaluated in the phase 3 studies (MATRIX-1 and MATRIX-2).
We hypothesized that the INL-001 implant would lead to less pain and less opioid consumption than a control placebo collagen-matrix implant. Two phase 3 studies, MATRIX-1 (ClinicalTrials.gov identifier, NCT02523599) and MATRIX-2 (ClinicalTrials.gov identifier, NCT02525133), were conducted as part of a regulatory strategy to examine the efficacy and safety of INL-001 300 mg in the treatment of postsurgical pain in the surgical model of open inguinal hernia repair with mesh.
Methods
Two similar phase 3, multicenter, randomized, double-blind, placebo-controlled studies (MATRIX-1 and MATRIX-2) were performed in patients scheduled for unilateral inguinal hernia repair. MATRIX-1 was conducted from August 2015 to April 2016 and MATRIX-2 from September 2015 to April 2016 in the USA. Thirty-nine unique centers participated across the two studies.
Eligible patients were ≥ 18 years of age and undergoing elective open mesh tension-free inguinal hernia repair under general anesthesia. Operations were performed according to standard surgical technique. Randomization was stratified by sex and history of previous ipsilateral hernia repair using mesh. Patients were randomized just prior to surgery in a 2:1 ratio to either INL-001 or placebo collagen-matrix implants to ensure the required number of INL-001 300 mg patient exposures for the regulatory approval process. A centralized block randomization was performed using an electronic randomization system.
The protocol and statement of informed consent were approved by an Institutional Review Board (IRB) prior to each center’s initiation. All procedures were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The studies were also conducted in compliance with the International Council for Harmonisation (ICH) principles of Good Clinical Practice (GCP; including archiving of essential study documents) and other applicable local regulations and guidelines. Informed consent was obtained from all individual participants included in the study.
Patients in the INL-001 group received a total of three INL-001 100-mg bupivacaine HCl collagen-matrix implants for a total dose of 300-mg bupivacaine HCl. The placebo collagen-matrix group received three collagen-matrix implants without bupivacaine (placebo collagen-matrix implants). Both the INL-001 bupivacaine HCl and placebo collagen-matrix implants were approximately 5 × 5 cm, off-white to white, lyophilized, porous matrices of type I bovine collagen. Investigators and patients were blinded as to whether a patient received INL-001 or matched placebo collagen-matrix implants, and the investigators were not aware of the size of the randomization block. When a patient had an AE that required the investigator to be unblinded, the investigator was able to obtain the treatment assignment.
For both groups, the three collagen-matrix implants were placed at specific protocol-prescribed locations in the surgical site prior to incision closure. After the hernia sac was reduced and the mesh was ready for insertion, each of the three 5 × 5-cm test article matrices were cut in half for a total of six half matrices measuring approximately 2.5 × 5 cm in size. Three half matrices were placed into the hernia repair site below the site of mesh placement. The mesh placement was completed per the surgeon’s typical technique. The external oblique aponeurosis was closed, and the remaining three half matrices were placed between the fascia/muscle closure and skin closure. The subcutaneous tissue and skin were closed per the surgeon’s preference.
In the immediate postsurgical period, parenteral morphine was available, as needed, for the treatment of pain. When able to tolerate oral medication, patients were required to take oral acetaminophen 650 mg three times daily for 3 days and were also prescribed immediate-release (IR) morphine to manage pain to be taken on an as-needed basis only. All use of acetaminophen and rescue opioid analgesia was recorded.
Efficacy Assessments
At predetermined time points (1, 2, 3, 5, 8, 12, 24, 48, and 72 h after implantation of study drug), the current PI was assessed by the patient via an electronic diary, using an 11-point numerical rating scale (NRS), where 0 indicated “no pain” and 10 indicated “worst pain possible.” PI was also assessed immediately before taking scheduled acetaminophen and immediately before the use of any parenteral or oral opioid analgesia. The primary efficacy end point was the sum of PI (SPI) from 0 to 24 h (SPI24; the area under the NRS PI curve from 0 to 24 h). Key secondary efficacy assessments included SPI from 0 to 48 h (SPI48) and 0–72 h (SPI72) and total use of opioid analgesia (TOpA) from time 0 through 24, 48, and 72 h (TOpA24, TOpA48, TOpA72) reported in mg IV morphine equivalents.
Safety Assessments
Safety assessments included AEs and vital sign measurements that were evaluated throughout the 30-day study period. Questionnaires were used to help assess AEs specifically suggestive of systemic bupivacaine toxicity, including nervous system and cardiac treatment-emergent AEs (TEAEs; somnolence, dizziness, dysgeusia, restlessness, vision impairments, anxiety, depression, tremors, dysarthria, numbness or tingling, altered state of consciousness, dyspnea, tinnitus, bradycardia, tachycardia) and AEs as related to the incision site or wound healing (incision-site complication, erythema, inflammation, pain, swelling, seroma, wound dehiscence).
Statistical Analysis
The sample size for each study was determined based on achieving 90% power to detect the difference between the INL-001 and placebo collagen-matrix in the primary efficacy variable (SPI24). With a 2:1 randomization ratio, it was determined that a sample size of 300 would provide the study with 90% power to detect a difference between the INL-001 and placebo collagen-matrix in SPI24 with an effect size of 0.40 or greater.
For SPI over time analysis through various time points, all available NRS PI scores (scheduled, pre-acetaminophen, and pre-rescue) were included in the calculation. There was a data management rule that if a pre-rescue or pre-acetaminophen PI assessment fell within the time window of a scheduled assessment, the pre-rescue or pre-acetaminophen assessment replaced the scheduled assessment. Missing pre-rescue NRS PI values were imputed using the worst observed NRS PI value (across all scheduled, unscheduled, pre-acetaminophen, and pre-rescue PI scores). Missing scheduled or pre-acetaminophen NRS PI values were imputed using linear interpolation between the two closest observed NRS PI scores before and after the missing time point or using the last-observation-carried-forward method. If a patient was terminated from the study prior to 72 h, the total amount of opioid used before termination was used for all analyses of time points after termination.
The intent-to-treat (ITT) population consisted of all randomized patients, whether or not they received any dose of INL-001 or placebo collagen-matrix. The modified ITT (mITT) population consisted of all randomized patients who received any dose of INL-001 or placebo collagen-matrix and had at least one NRS PI score prior to hospital discharge, as needed to compute SPI. The mITT population was the primary population for efficacy assessments. The safety population consisted of all patients who received any dose of INL-001 or placebo collagen-matrix.
The primary efficacy variable was analyzed using an analysis of variance (ANOVA) model with treatment and randomization strata as the main effects. Treatment effect was examined once at a two-sided 0.05 significance level. To control the overall type-I error rate, key secondary efficacy end points were tested sequentially in a fixed hierarchical order at the 0.05 significance level. The order of statistical testing was: (1) TOpA from time 0 through 24 h (TOpA24), (2) SPI from time 0 through 48 h (SPI48), (3) TOpA from time 0 through 48 h (TOpA48), (4) SPI from time 0 through 72 h (SPI72), and (5) TOpA from time 0 through 72 h (TOpA72). If any secondary end point variable failed to reach statistical significance, no additional statistical testing was performed on subsequent end point variables. Other secondary end points included percentage of patients using oral opioid analgesia at multiple time points postimplantation (24, 48, and 72 h) and time to first use of opioid analgesia.
To increase statistical power and further understand and better characterize the key secondary efficacy end points, data from MATRIX-1 and MATRIX-2 were pooled. The designs of MATRIX-1 and MATRIX-2 allowed for this pooling, which was proactively planned during protocol development. Individual study data as well as pooled data analyses are presented.
Results
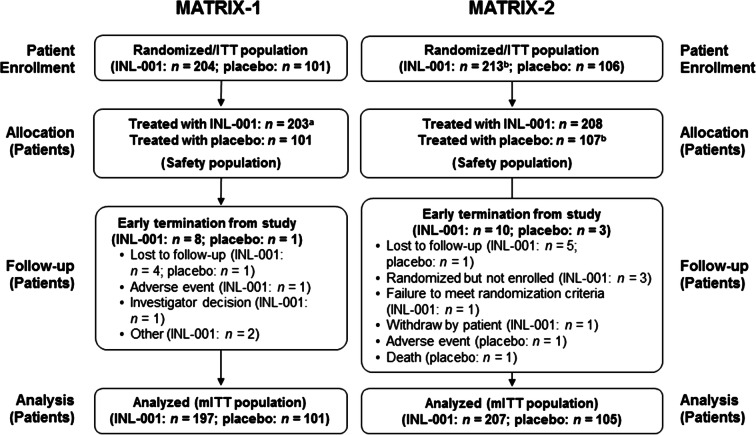
Demographics and baseline characteristics were similar between groups in MATRIX-1 and MATRIX-2 (Table 1). Patients’ sex ratios and percentages of patients with a history of previous ipsilateral hernia repair were comparable across treatment groups in both studies, reflecting the stratified randomization method. In MATRIX-1, 305 patients were randomized (INL-001 = 204; placebo collagen-matrix = 101), and in MATRIX-2, 319 patients were randomized (INL-001 = 213; placebo collagen-matrix = 106) and therefore comprised the ITT population (Fig. 1). The mITT (analysis) population included 297 MATRIX-1 patients and 312 MATRIX-2 patients.
Table 1.
Demographics and baseline characteristics (ITT population)
| Parameter | MATRIX-1 | MATRIX-2 | ||
|---|---|---|---|---|
| INL-001 (n = 204) | Placebo collagen-matrix (n = 101) | INL-001 (n = 213) | Placebo collagen-matrix (n = 106) | |
| Age (years) | ||||
| Mean (SD) | 53.1 (12.82) | 53.3 (14.01) | 50.7 (13.69) | 48.5 (13.94) |
| Median | 55.0 | 54.0 | 52.0 | 50.0 |
| Minimum, maximum | 19, 83 | 21, 86 | 18, 85 | 19, 75 |
| Sex, n (%) | ||||
| Male | 196 (96) | 97 (96) | 208 (98) | 103 (97) |
| Female | 8 (4) | 4 (4) | 5 (2) | 3 (3) |
| Ethnicity, n (%) | ||||
| Hispanic or Latino | 77 (38) | 38 (38) | 44 (21) | 23 (22) |
| Not Hispanic or Latino | 127 (62) | 62 (61) | 169 (79) | 83 (78) |
| Missing | 0 | 1 (1) | 0 | 0 |
| Race, n (%) | ||||
| American Indian or Alaskan Native | 1 (< 1) | 1 (1) | 2 (< 1) | 1 (< 1) |
| Asian | 2 (1) | 2 (2) | 4 (2) | 3 (3) |
| Black or African American | 15 (7) | 7 (7) | 23 (11) | 12 (11) |
| Native Hawaiian or Pacific Islander | 1 (< 1) | 0 | 1 (< 1) | 0 |
| White | 185 (91) | 91 (90) | 182 (85) | 90 (85) |
| Missing | 0 | 0 | 1 (< 1) | 0 |
| Body mass index (kg/m2) | (n = 202) | (n = 100) | (n = 209) | (n = 106) |
| Mean (SD) | 27.05 (3.899) | 27.26 (4.596) | 26.84 (4.025) | 27.22 (5.062) |
| Median | 26.60 | 26.49 | 26.66 | 26.64 |
| Minimum, maximum | 18.7, 39.6 | 19.2, 42.1 | 17.8, 40.8 | 17.4, 45.9 |
| Previous ipsilateral hernia repair using mesh, n (%) | ||||
| Yes | 20 (10) | 12 (12) | 22 (10) | 10 (10) |
| No | 184 (90) | 89 (88) | 189 (89) | 96 (91) |
| Missing | 0 | 0 | 2 (< 1) | 0 |
| Multiple hernias, n (%) | ||||
| Yes | 13 (6) | 4 (4) | 5 (2) | 4 (4) |
| No | 190 (93) | 96 (95) | 204 (96) | 102 (96) |
| Missing | 1 (< 1) | 1 (1) | 4 (2) | 0 |
| Incision duration (h) | (n = 203) | (n = 100) | (n = 209) | (n = 106) |
| Mean (SD) | 0.80 (0.432) | 0.75 (0.379) | 0.80 (0.327) | 0.84 (0.352) |
| Median | 0.72 | 0.67 | 0.75 | 0.77 |
| Minimum, maximum | 0.2, 3.0 | 0.2, 1.8 | 0.2, 2.1 | 0.2, 2.5 |
SD standard deviation, ITT intent-to-treat
Fig. 1.
Patient disposition for MATRIX-1 and MATRIX-2. aOne patient was randomized to INL-001 but not treated because of investigator decision. bOne patient was randomized to INL-001 but received placebo; the patient included in INL-001 mITT population and placebo safety population. ITT intent-to-treat, mITT modified intent-to-treat
Efficacy
Patients treated with INL-001 reported a statistically lower mean SPI24 (the primary end point) compared with patients treated with placebo collagen-matrix in both MATRIX-1 and MATRIX-2 (P = 0.0004, P < 0.0001, respectively) (Table 2). These reductions in PI were coupled with significantly less opioid analgesic usage in the INL-001 group compared with the placebo collagen-matrix group throughout the first 24 h (TOpA24) in both studies (P < 0.0001) (Table 2).
Table 2.
Primary end point and key secondary end points (mITT population)
| Parameter | MATRIX-1 | MATRIX-2 | ||
|---|---|---|---|---|
| INL-001 (n = 197) | Placebo collagen-matrix (n = 101) | INL-001 (n = 207) | Placebo collagen-matrix (n = 105) | |
| Primary end point | ||||
| SPI24 | ||||
| Mean (SEM) | 85.9 (3.36) | 106.8 (4.80) | 88.3 (3.27) | 116.2 (4.30) |
| Median | 82.2 | 107.5 | 84.4 | 119.3 |
| Observed P valuea vs. placebo collagen-matrix | 0.0004 | < 0.0001 | ||
| Key secondary end points | ||||
| TOpA24 (mg IV morphine eq) | ||||
| Median | 5.0 | 10.0 | 5.0 | 14.0 |
| Observed P valueb vs. placebo collagen-matrix | < 0.0001 | < 0.0001 | ||
| SPI48 | ||||
| Mean (SEM) | 179.3 (6.77) | 201.3 (9.34) | 192.6 (6.39) | 216.8 (8.88) |
| Median | 165.7 | 190.1 | 188.1 | 214.9 |
| Observed P valuea vs. placebo collagen-matrix | 0.0568 | 0.0270 | ||
| TOpA48 (mg IV morphine eq) | ||||
| Median | 5.0 | 14.0 | 10.0 | 20.0 |
| Observed P valueb vs. placebo collagen-matrix | NTc | 0.0003 | ||
| SPI72 | ||||
| Mean (SEM) | 257.8 (9.93) | 281.1 (13.90) | 277.6 (9.59) | 301.2 (8.88) |
| Median | 245.2 | 263.3 | 264.5 | 299.7 |
| Observed P valuea vs. placebo collagen-matrix | NTc | 0.1490 | ||
| TOpA72 (mg IV morphine eq) | ||||
| Median | 5.0 | 14.0 | 10.0 | 20.0 |
| Observed P valueb vs. placebo collagen-matrix | NTc | NTc | ||
ANOVA analysis of variance, IV intravenous, eq equivalents, mITT modified intent-to-treat, NT not tested, SEM standard error of the mean, SPI24, SPI48, SPI72 sum of pain intensity from time 0 through 24, 48, and 72 h, TOpA24, TOpA48, TOpA72 total use of opioid analgesia from time 0 through 24, 48, and 72 h
aP value represents the difference least-squares means between treatment groups from the ANOVA model with treatment, study, gender, and history of previous ipsilateral hernia repair as main effects
bP value from Wilcoxon rank sum test
cStatistical significance not tested based on statistical sequential testing algorithm
In MATRIX-2, patients who received INL-001 also reported statistically significantly less pain and opioid analgesic usage throughout the 48-h postsurgical period (SPI48; TOpA48) compared with patients who received placebo collagen-matrix (P = 0.0270, P = 0.0003, respectively) (Table 2). For MATRIX-1, the mean SPI48 score difference between the INL-001 and placebo collagen-matrix was similar in magnitude to that seen in MATRIX-2 (22.0 versus 24.2); however, this difference was not statistically significant (P = 0.0568). The statistical significance of TOpA48 was not tested based on the statistical sequential testing algorithm employed for analysis of the studies, but there was a numeric difference in favor of INL-001 (Table 2). Similarly, because of this sequential testing algorithm, the statistical significance of differences between treatment groups for SPI72 and TOpA72 was not tested in either study, but there were numeric differences in favor of INL-001 for both end points (Table 2).
At all time periods assessed (0–24, 0–48, and 0–72 h) in both studies, more patients who received INL-001 did not use any rescue opioid medication (42%, 37%, 36%, respectively, for MATRIX-1; 36%, 29%, 28%, respectively, for MATRIX-2) versus those receiving placebo collagen-matrix (22% for all time points for MATRIX-1; 12% for all time points for MATRIX-2) (Fig. 2). Of the patients using opioids, INL-001 patients in both studies had a statistically significantly longer time to first use of opioid analgesia (FOpA) compared with placebo collagen-matrix patients; median hours (95% CI) to FOpA was 10.7 (5.2, 17.8) versus 1.0 (0.9, 1.1) for MATRIX-1 and 6.2 (2.0, 12.0) versus 0.9 (0.8, 1.0) for MATRIX-2; P < 0.0001 for both).
Fig. 2.
Patients who did not use rescue opioid analgesia (mITT population). mITT modified intent-to-treat
The pooled analysis of MATRIX-1 and MATRIX-2 demonstrated findings similar to those in the individual studies. Patients treated with INL-001 reported significantly less pain from time 0 through 24, 48, and 72 h (P < 0.0001, P = 0.0033, P = 0.0441, respectively) and used significantly less opioid analgesia from time 0 through the same time points (P < 0.0001; P < 0.0001; P = 0.0004, respectively) (Table 3).
Table 3.
SPI and TOpA: MATRIX-1 and MATRIX-2 populations combined (mITT population)
| Parameter | MATRIX-1 and MATRIX-2 combined | |
|---|---|---|
| INL-001 (n = 404) | Placebo collagen-matrix (n = 206) | |
| SPI24 | ||
| Mean (SEM) | 87.1 (2.34) | 111.6 (3.22) |
| Median | 82.5 | 112.3 |
| Observed P valuea vs. placebo collagen-matrix | < 0.0001 | |
| TOpA24 (mg IV morphine eq) | ||
| Median | 5.0 | 12.3 |
| Observed P valueb vs. placebo collagen-matrix | < 0.0001 | |
| SPI48 | ||
| Mean (SEM) | 186.1 (4.65) | 209.2 (6.44) |
| Median | 180.5 | 208.8 |
| Observed P valuea vs. placebo collagen-matrix | 0.0033 | |
| TOpA48 (mg IV morphine eq) | ||
| Median | 7.0 | 15.0 |
| Observed P valueb vs. placebo collagen-matrix | < 0.0001 | |
| SPI72 | ||
| Mean (SEM) | 268.0 (6.91) | 291.3 (9.55) |
| Median | 253.0 | 274.9 |
| Observed P valuea vs. placebo collagen-matrix | 0.0441 | |
| TOpA72 (mg IV morphine eq) | ||
| Median | 9.0 | 17.0 |
| Observed P valueb vs. placebo collagen-matrix | 0.0004 | |
ANOVA analysis of variance, IV intravenous, eq equivalents, mITT modified intent-to-treat, NT not tested, SEM standard error of the mean, SPI24, SPI48, SPI72 sum of pain intensity from time 0 through 24, 48, and 72 h, TOpA24, TOpA48, TOpA72 total use of opioid analgesia from time 0 through 24, 48, and 72 h
aP value represents the difference least-squares means between treatment groups from the ANOVA model with treatment, study, sex, and history of previous ipsilateral hernia repair as main effects
bP value from Wilcoxon rank sum test
Safety
For MATRIX-1, at least one TEAE was reported in 68% of patients given INL-001 300 mg and 66% of those given the placebo collagen-matrix implant; for MATRIX-2, at least one AE was reported in 57% of patients treated with INL-001 300 mg and 71% of patients treated with a placebo collagen-matrix implant (Table 4). The two most commonly reported AEs in MATRIX-1 were incision-site swelling and somnolence and in MATRIX-2 were somnolence and dizziness (Table 4). No patient in either study experienced an AE that led to treatment discontinuation. The incidence of TEAEs judged to be related to the study drug was low in the pooled studies [14/411 INL-001 (3%), 6/208 placebo (2%); Table 5]. All TEAEs judged treatment-related were considered mild in intensity for MATRIX-1 and mild (93%) or moderate (7%) in intensity for MATRIX-2. In MATRIX-1, two patients in the INL-001 group and, in MATRIX-2, six patients (three in each treatment group) experienced serious AEs; however, no patient experienced a serious AE considered related to the test article. One death occurred in the placebo collagen-matrix group in the MATRIX-2 study because of acute myocardial infarction that was not considered related to the test article.
Table 4.
TEAEs occurring in ≥ 5% in any treatment group (safety population)
| Preferred term, n (%) | MATRIX-1 | MATRIX-2 | ||
|---|---|---|---|---|
| INL-001 (n = 203) | Placebo collagen-matrix (n = 101) | INL-001 (n = 208) | Placebo collagen-matrix (n = 107)a | |
| Patients reporting any AE | 138 (68) | 67 (66) | 118 (57) | 76 (71) |
| Incision-site swelling | 42 (21) | 19 (19) | 18 (9) | 11 (10) |
| Somnolence | 36 (18) | 20 (20) | 33 (16) | 19 (18) |
| Incision-site pain | 34 (17) | 19 (19) | 19 (9) | 13 (12) |
| Dizziness | 31 (15) | 12 (12) | 34 (16) | 22 (21) |
| Nausea | 23 (11) | 15 (15) | 16 (8) | 19 (18) |
| Constipation | 17 (8) | 12 (12) | 18 (9) | 19 (18) |
| Post-procedural discharge | 15 (7) | 6 (6) | 5 (2) | 4 (4) |
| Dysgeusia | 14 (7) | 3 (3) | 17 (8) | 10 (9) |
| Restlessness | 14 (7) | 9 (9) | 16 (8) | 10 (9) |
| Incision-site complication | 10 (5) | 10 (10) | 13 (6) | 6 (6) |
| Incision-site erythema | 9 (4) | 4 (4) | 4 (2) | 7 (7) |
| Anxiety | 6 (3) | 3 (3) | 6 (3) | 8 (8) |
| Vomiting | 5 (3) | 3 (3) | 4 (2) | 7 (7) |
| Tinnitus | 4 (2) | 2 (2) | 3 (1) | 7 (7) |
AE adverse event, mITT modified intent-to-treat
aOne patient was randomized to INL-001, but received placebo; patient included in INL-001 mITT population and placebo safety population
Table 5.
All Treatment-related TEAEs: MATRIX-1 and MATRIX-2 populations combined (safety population)
| Preferred term, n (%) | INL-001 (n = 411) | Placebo collagen-matrix (n = 208) |
|---|---|---|
| Patients reporting any treatment-related TEAE | 14 (3) | 6 (3) |
| Dysgeusia | 6 (2) | 2 (1) |
| Dizziness | 4 (1) | 1 (< 1) |
| Incision-site complicationa | 3 (< 1) | 0 |
| Headache | 1 (< 1) | 0 |
| Somnolence | 1 (< 1) | 0 |
| Tremor | 1 (< 1) | 0 |
| Tinnitus | 1 (< 1) | 1 (< 1) |
| Vision blurred | 1 (< 1) | 1 (< 1) |
| Constipation | 0 | 1 (< 1) |
| Hypoesthesia oral | 0 | 1 (< 1) |
| Paresthesia oral | 0 | 1 (< 1) |
| Anxiety | 0 | 1 (< 1) |
| Restlessness | 0 | 1 (< 1) |
TEAE treatment-emergent adverse event
aFor these events, verbatim terms include sensation of warmth at the incision site, hardness at incision site, and popping sensation at surgical site
A review of TEAEs possibly suggestive of bupivacaine toxicity did not indicate that any patient experienced the constellation of signs and symptoms indicative of bupivacaine toxicity. The incidence of TEAEs classified as nervous system disorders was generally similar between the INL-001 and placebo collagen-matrix groups for both studies (INL-001 30%, placebo collagen-matrix 27% for MATRIX-1; INL-001 35%, placebo collagen-matrix 39% for MATRIX-2). The most commonly reported nervous system symptom in both studies was somnolence, which was experienced by 18% of patients given INL-001 300 mg and 20% of patients given a placebo collagen-matrix implant in MATRIX-1 and 16% of patients given INL-001 300 mg and 18% of patients given a placebo collagen-matrix implant in MATRIX-2. Similarly, the incidence of TEAEs classified as cardiac disorders was low; no treatment group in either study experienced cardiac disorders at a rate > 1%. No clinically meaningful effect on vital sign parameters [systolic blood pressure (BP), diastolic BP, heart rate (HR), respiratory rate, temperature] was observed for either study population.
A review of TEAEs having to do with the incision site or wound healing revealed that the most commonly reported incision-site TEAEs in both MATRIX-1 and MATRIX-2 were incision-site swelling (INL-001 21%, placebo collagen-matrix 19% for MATRIX-1; INL-001 9%, placebo collagen-matrix 10% for MATRIX-2) and incision-site pain (INL-001 17%, placebo collagen-matrix 19% for MATRIX-1; INL-001 9%, placebo collagen-matrix 12% for MATRIX-2) (Table 4). Other incision-site TEAEs reported were incision-site complication (MATRIX-1 INL-001 5%, placebo collagen-matrix 10%; MATRIX-2 INL-001 6%, placebo collagen-matrix 6%), incision-site erythema (MATRIX-1 INL-001 4%, placebo collagen-matrix 4%; MATRIX-2 INL-001 2%, placebo collagen-matrix 7%), incision-site inflammation (MATRIX-1 INL-001 2%, placebo collagen-matrix 3%; MATRIX-2 INL-001 1%, placebo collagen-matrix 3%), seroma (MATRIX-1 INL-001 3%, placebo collagen-matrix 2%; MATRIX-2 INL-001 3%, placebo collagen-matrix 3%), and wound dehiscence (MATRIX-1 INL-001 3%, placebo collagen-matrix 3%; MATRIX-2 INL-001 1%, placebo collagen-matrix 2%). Three patients each had one TEAE pertaining to the incision site that was judged treatment related, all receiving INL-001. These TEAEs had the verbatim terms of sensation of warmth at the incision site, hardness at incision site, and popping sensation at surgical site.
A review of TEAEs defined as opioid-related, based on those listed as commonly reported in the prescribing information for morphine sulfate (nausea, constipation, and vomiting), was conducted for the MATRIX-1 and MATRIX-2 pooled study population. Patients treated with INL-001 reported significantly fewer opioid-related TEAEs over the postimplantation period compared with patients receiving placebo collagen-matrix (17% vs. 30%; P = 0.0004).
Discussion
INL-001 is a bupivacaine delivery technology designed to be implanted in the surgical site at the time of soft tissue surgery to produce extended postoperative analgesia and result in reduced opioid use. In both MATRIX-1 and MATRIX-2, treatment with INL-001 was associated with significant reductions in postsurgical PI over the first 24 h compared with the placebo collagen-matrix, thus meeting the primary end point in both studies conducted with patients undergoing unilateral open inguinal hernioplasty. In addition, INL-001 treatment resulted in significantly less total opioid analgesic usage during the first 24 h compared with the placebo collagen-matrix in both studies.
Both PI and opioid use were statistically significantly reduced during the first 48 h with INL-001 compared with placebo collagen-matrix in MATRIX-2. The magnitude of effect on the mean SPI48 score was similar in MATRIX-1 to that seen in MATRIX-2, but there was a slightly higher variability in the score, and statistical significance on this end point was barely missed in MATRIX-1. Assessment of PI is inherently variable given its subjective nature. There is also the likelihood of increasing variability in PI assessment among patients further from the surgical event, because patients recover at different rates. In addition, it is recognized that the use of opioid rescue medication can make assessment of PI challenging in clinical trials. Given this, it is useful to consider the reductions in PI in the context of reductions in opioid use.
A statistical test for median TOpA48 was not performed for the MATRIX-1 study due to the fixed hierarchical testing order of the key secondary end points; however, the numerical reduction in opioid use (median mg IV morphine equivalents) in favor of INL-001 compared with the placebo collagen-matrix was actually greater in MATRIX-1 compared with MATRIX-2 48 h post-surgery. In addition, the percentage of opioid-free patients treated with INL-001 was approximately double that of patients receiving the placebo collagen-matrix at 48 h, with similar results seen at 72 h.
Pooling the data from the two studies limited the statistical impact of increasing variability over time post-surgery in the mean SPI score, and analysis of this data set demonstrated that patients treated with INL-001 showed a significant reduction in mean SPI through 24, 48, and 72 h compared with those receiving a placebo collagen-matrix, with the same result seen for the median TOpA.
INL-001 was well tolerated in these studies. The most common TEAEs were those that would be expected after anesthesia or with opioid use, and treatment-related TEAEs occurred at a low rate. Because both the placebo and treatment groups received a collagen-matrix implant, to assess the true risk of the collagen-matrix implant, it is useful to consider the rate of complications frequently reported after inguinal hernia repair. Patients in a national hernia registry reported via questionnaire that the most common AEs experienced after inguinal or femoral hernia repair were hematoma (14%), severe pain (12%), testicular pain (8%), postoperative infections (7%), wound rupture (4%), and constipation (4%) [37]. Postsurgical AEs required 12% of patients to visit a healthcare provider [37]. A systematic review of open inguinal hernia repair studies found infection rates ranging from 3 to 5% [38]. In another study, 6% of patients undergoing open mesh inguinal hernia repair developed a wound hematoma, 5% developed a scrotal hematoma, and 2% developed seroma [39]. When the types and rates of AEs commonly associated with open inguinal hernia repair are compared with the AE profiles seen in the studies for both INL-001 and the placebo collagen-matrix, it would appear that delivery of bupivacaine in the surgical site via a collagen-matrix is well tolerated. The pooled analysis also demonstrated a statistically significant reduction in AEs associated with opioid medication.
The reductions in opioid use and opioid-related adverse drug events (ORADEs) seen with INL-001 are clinically meaningful findings. One study of surgical inpatients found that ORADEs following surgery increased median hospitalization costs by 7% and the median length of stay by 10% [8]. A recent report suggests that, among opioid-naive patients, opioid use for as short as 3 days may increase the likelihood of long-term use and that an increased length of initial exposure (higher total dose, longer duration of first use) is associated with an increased risk of long-term use [9]. A review of a nationwide data set of insurance claims, which included 36,177 patients, found that new persistent opioid use (i.e., opioid prescriptions filled) between 90 and 180 days after major surgical procedures, such as hernia repair, occurred at a rate of 7% in patients who were opioid-naive at the time of surgery [36].
While a limitation of this study is that it did not include a comparison with bupivacaine infiltration, the use of INL-001 collagen technology to deliver bupivacaine avoids the greatest risk of bupivacaine use in a surgical wound, that of unintended intravascular injection, which can lead to serious systemic bupivacaine toxicity [20, 21, 25]. No injection technique is known to eliminate this risk [20]. There was no evidence that any patient experienced systemic bupivacaine toxicity in either study.
The generalizability of these findings may be limited by the fact that the study population was almost entirely male and predominantly white. However, the large number of patients across both studies and the number of unique study centers support the potential clinical efficacy, utility, and safety of INL-001.
Conclusion
Two pivotal phase 3 studies of INL-001 met their primary end points, both demonstrating statistically significant reductions in acute postsurgical pain during the first 24 h after open inguinal hernia repair compared with the placebo collagen-matrix. The analgesic efficacy of INL-001 was further supported by a significantly lower use of opioid analgesics in the INL-001 group compared with the placebo collagen-matrix group through 24 h. One of the studies also demonstrated statistically significant and clinically meaningful reductions in mean SPI and median opioid use through 48 h with INL-001, with the other study demonstrating a similar magnitude of effect with INL-001 treatment, almost reaching statistical significance. When the data from the two studies were pooled, statistically significant differences were seen in reductions in mean SPI and median opioid use through 24, 48, and 72 h. INL-001 was well tolerated, and no safety issues emerged during these studies that were related to the use of the collagen-matrix. These results support the use of INL-001 as an alternative treatment for the management of acute postsurgical pain following open inguinal hernia repair.
Acknowledgements
We thank the patients who participated in this study and the clinical study teams. The authors wish to thank Sue Hobson, BSN, formerly of Innocoll Pharmaceuticals, for her assistance with this study and Ted Smith, PhD, for providing statistical analyses.
Funding
Funding to support this study and the journal’s article processing charges and Open Access fee was provided by Innocoll Pharmaceuticals, Monksland, Athlone, Ireland.
Medical Writing and Editorial Assistance
Jennifer Steeber, PhD, and Michelle Jones, PhD, of MedVal Scientific Information Services, LLC (Skillman, NJ) and Samantha L Dwyer, PhD, and Michele Salernitano of Scientific Connexions (Lyndhurst, NJ), an Ashfield Company, provided medical writing and editorial assistance, which was funded by Innocoll Pharmaceuticals.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published. This manuscript was prepared according to the International Society for Medical Publication Professionals’ Good Publication Practice for Communicating Company-Sponsored Medical Research: GPP3.
Author Contributions
All authors participated in the design and analytical approach of the study and contributed to the manuscript development. Results were summarized and interpreted in collaboration with all authors. All authors had full access to all of the data in this study and take complete responsibility for the integrity of the data and accuracy of the data analysis.
Prior Presentation
Data from this paper were presented at the 36th Annual Scientific Meeting of the American Pain Society and published in abstract form as: Leiman D, Minkowitz H; Despain D, Jones M, Hobson S. J Pain. 2017;18(4 suppl):S29. Abstract 214.
Disclosures
Vic Velanovich declares that he has received research funding and consultant fees from Innocoll Pharmaceuticals. Paul Rider declares that he has received consultant fees from Innocoll Pharmaceuticals. Kenneth Deck declares he is an Investigator for Innocoll Pharmaceuticals. Harold S Minkowitz declares that he has received research funding and consultant fees from Durect Corp., Heron Therapeutics, Inc., Innocoll Pharmaceuticals, and Pacira Pharmaceuticals, Inc. David Leiman declares that he has received research funding and consultant fees from Durect Corp., Heron Therapeutics, Inc., Innocoll Pharmaceuticals, and Pacira Pharmaceuticals, Inc. Nigel Jones’ affiliation at the time of the study was Innocoll, Newtown Square, PA, USA (legal entity: Innocoll Pharmaceuticals Ltd., Monksland, Athlone, Ireland). Nigel Jones is currently employed by Circadian Therapeutics, Oxford, UK. Gwendolyn Niebler declares that she is an employee of Innocoll, Newtown Square, PA, USA (legal entity: Innocoll Pharmaceuticals Limited, Monksland, Athlone, Ireland).
Compliance with Ethics Guidelines
The protocol and the statement of informed consent were approved by an Institutional Review Board (IRB) prior to each center’s initiation. All procedures were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The studies were also conducted in compliance with the International Council for Harmonisation (ICH) principles of Good Clinical Practice (GCP; including archiving of essential study documents) and other applicable local regulations and guidelines. Informed consent was obtained from all individual participants included in the study.
Data Availability
The data sets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Footnotes
Enhanced Digital Features
To view enhanced digital features for this article go to 10.6084/m9.figshare.7297253.
References
- 1.Morrison RS, Magaziner J, McLaughlin MA, Orosz G, Silberzweig SB, Koval KJ, et al. The impact of post-operative pain on outcomes following hip fracture. Pain. 2003;103(3):303–11. 10.1016/S0304-3959(02)00458-X [DOI] [PubMed] [Google Scholar]
- 2.Robinson KP, Wagstaff KJ, Sanghera S, Kerry RM. Postoperative pain following primary lower limb arthroplasty and enhanced recovery pathway. Ann R Coll Surg Engl. 2014;96(4):302–6. 10.1308/003588414X13946184900525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stephens J, Laskin B, Pashos C, Peña B, Wong J. The burden of acute postoperative pain and the potential role of the COX-2-specific inhibitors. Rheumatology (Oxford). 2003;42(suppl 3):iii40–52. [DOI] [PubMed] [Google Scholar]
- 4.Beauregard L, Pomp A, Choinière M. Severity and impact of pain after day-surgery. Can J Anaesth. 1998;45(4):304–11. 10.1007/BF03012019 [DOI] [PubMed] [Google Scholar]
- 5.Gramke HF, de Rijke JM, van Kleef M, Raps F, Kessels AG, Peters ML, et al. The prevalence of postoperative pain in a cross-sectional group of patients after day-case surgery in a university hospital. Clin J Pain. 2007;23(6):543–8. 10.1097/AJP.0b013e318074c970 [DOI] [PubMed] [Google Scholar]
- 6.Benyamin R, Trescot AM, Datta S, Buenaventura R, Adlaka R, Sehgal N, et al. Opioid complications and side effects. Pain Physician. 2008;11(2 suppl):S105–20. [PubMed] [Google Scholar]
- 7.Shaffer EE, Pham A, Woldman RL, Spiegelman A, Strassels SA, Wan GJ, et al. Estimating the effect of intravenous acetaminophen for postoperative pain management on length of stay and inpatient hospital costs. Adv Ther. 2017;33(12):2211–28. 10.1007/s12325-016-0438-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Oderda GM, Said Q, Evans RS, Stoddard GJ, Lloyd J, Jackson K, et al. Opioid-related adverse drug events in surgical hospitalizations: impact on costs and length of stay. Ann Pharmacother. 2007;41(3):400–6. 10.1345/aph.1H386 [DOI] [PubMed] [Google Scholar]
- 9.Shah A, Hayes CJ, Martin BC. Characteristics of initial prescription episodes and likelihood of long-term opioid use—United States, 2006–2015. MMWR Morb Mortal Wkly Rep. 2017;66(10):265–9. 10.15585/mmwr.mm6610a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain—United States, 2016. JAMA. 2016;315(15):1624–45. 10.1001/jama.2016.1464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Devin CJ, McGirt MJ. Best evidence in multimodal pain management in spine surgery and means of assessing postoperative pain and functional outcomes. J Clin Neurosci. 2015;22(6):930–8. 10.1016/j.jocn.2015.01.003 [DOI] [PubMed] [Google Scholar]
- 12.Fawcett WJ, Baldini G. Optimal analgesia during major open and laparoscopic abdominal surgery. Anesthesiol Clin. 2015;33(1):65–78. 10.1016/j.anclin.2014.11.005 [DOI] [PubMed] [Google Scholar]
- 13.Babst CR, Gilling BN. Bupivacaine: a review. Anesth Prog. 1978;25(3):87–91. [PMC free article] [PubMed] [Google Scholar]
- 14.Chou R, Gordon DB, de Leon-Casasola OA, Rosenberg JM, Bickler S, Brennan T, et al. Management of postoperative pain: a clinical practice guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain. 2016;17(2):131–57. 10.1016/j.jpain.2015.12.008 [DOI] [PubMed] [Google Scholar]
- 15.Apfelbaum JL, Chen C, Mehta SS, Gan TJ. Postoperative pain experience: results from a national survey suggest postoperative pain continues to be undermanaged. Anesth Analg. 2003;97(2):534–40 (table of contents). 10.1213/01.ANE.0000068822.10113.9E [DOI] [PubMed] [Google Scholar]
- 16.Tong YC, Kaye AD, Urman RD. Liposomal bupivacaine and clinical outcomes. Best Pract Res Clin Anaesthesiol. 2014;28(1):15–27. 10.1016/j.bpa.2014.02.001 [DOI] [PubMed] [Google Scholar]
- 17.Gudgeon DH. Paracervical block with bupivacaine 0.25 per cent. Br Med J. 1968;2(5602):403. 10.1136/bmj.2.5602.403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McGee DL. Local and topical anesthesia. In: Roberts JR, Hedges JR, editors. Roberts and Hedges’ clinical procedures in emergency medicine. 5th ed. Philadelphia: Saunders Elsevier; 2010. p. 481. [Google Scholar]
- 19.Svensson I, Sjöström B, Haljamäe H. Assessment of pain experiences after elective surgery. J Pain Symptom Manag. 2000;20(3):193–201. 10.1016/S0885-3924(00)00174-3 [DOI] [PubMed] [Google Scholar]
- 20.Gadsden J. Local anesthetics: clinical pharmacology and rational selection. NYSORA website. 2017. https://www.nysora.com/local-anesthetics-clinical-pharmacology-and-rational-selection. Accessed 5 Dec 2017.
- 21.Goyal R, Shukla RN. Local anesthetic systemic toxicity (LAST)—should we not be concerned? Med J Armed Forces India. 2012;68(4):371–5. 10.1016/j.mjafi.2012.02.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gupta A. Wound infiltration with local anaesthetics in ambulatory surgery. Curr Opin Anaesthesiol. 2010;23(6):708–13. 10.1097/ACO.0b013e32833f0dd7 [DOI] [PubMed] [Google Scholar]
- 23.Marcaine (bupivacaine hydrochloride injection, USP) [prescribing information]. Lake Forest, IL: Hospira, Inc. 2011. https://www.accessdata.fda.gov/drugsatfda_docs/label/2012/018692s015lbl.pdf. Accessed 04 Sept 2018.
- 24.Whiteman A, Bajaj S, Hasan M. Novel techniques of local anaesthetic infiltration. Contin Educ Anaesth Crit Care Pain. 2011;11(5):167–71. 10.1093/bjaceaccp/mkr026 [DOI] [Google Scholar]
- 25.Dewaele S, Santos AC. Toxicity of local anesthetics. NYSORA website. 2018. https://www.nysora.com/toxicity-of-local-anesthetics. Accessed 20 Feb 2018.
- 26.Cusack SL, Jaros M, Kuss M, Minkowitz HS, Winkle P, Hemsen L. Clinical evaluation of XaraColl®, a bupivacaine-collagen implant, for postoperative analgesia in two multicenter, randomized, double-blind, placebo-controlled pilot studies. J Pain Res. 2012;5:217–25. 10.2147/JPR.S33453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cusack SL, Minkowitz HS, Kuss M, Jaros M, Hemsen L. A randomized, multicenter, pilot study comparing the efficacy and safety of a bupivacaine-collagen implant (XaraColl®) with the ON-Q* PainBuster®) Post-op Pain Relief System following open gynecological surgery. J Pain Res. 2012;5:453–61. 10.2147/JPR.S37310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hemsen L, Cusack SL, Minkowitz HS, Kuss ME. A feasibility study to investigate the use of a bupivacaine-collagen implant (XaraColl) for postoperative analgesia following laparoscopic surgery. J Pain Res. 2013;6:79–85. 10.2147/JPR.S40158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cusack SL, Reginald P, Hemsen L, Umerah E. The pharmacokinetics and safety of an intraoperative bupivacaine-collagen implant (XaraColl®) for postoperative analgesia in women following total abdominal hysterectomy. J Pain Res. 2013;6:151–9. 10.2147/JPR.S40976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Huber A, Badylak SF. Biologic scaffolds for regenerative medicine. In: Atala A, Lanza R, Thomson JA, Nerem R, editors. Principles of regenerative medicine. 2nd ed. Boston: Academic Press; 2011. p. 623–35. [Google Scholar]
- 31.Delgado LM, Bayon Y, Pandit A, Zeugolis DI. To cross-link or not to cross-link? Cross-linking associated foreign body response of collagen-based devices. Tissue Eng Part B Rev. 2015;21(3):298–313. 10.1089/ten.teb.2014.0290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Anselme K, Bacques C, Charriere G, Hartmann DJ, Herbage D, Garrone R. Tissue reaction to subcutaneous implantation of a collagen sponge. A histological, ultrastructural, and immunological study. J Biomed Mater Res. 1990;24(6):689–703. 10.1002/jbm.820240605 [DOI] [PubMed] [Google Scholar]
- 33.Burke KE, Naughton G, Waldo E, Cassai N. Bovine collagen implant: histologic chronology in pig dermis. J Dermatol Surg Oncol. 1983;9(11):889–95. 10.1111/j.1524-4725.1983.tb01036.x [DOI] [PubMed] [Google Scholar]
- 34.Leiman D, Niebler G, Minkowitz H. Pharmacokinetics and safety of the bupivacaine collagen-matrix implant (INL-001) compared to liquid bupivacaine infiltration after open inguinal hernia repair [abstract]. Presented at World Congress on Regional Anesthesia & Pain Medicine; April 19–21, 2018; New York, New York.
- 35.Knudsen K, Beckman Suurküla M, Blomberg S, Sjövall J, Edvardsson N. Central nervous and cardiovascular effects of i.v. infusions of ropivacaine, bupivacaine and placebo in volunteers. Br J Anaesth. 1997;78(5):507–14. 10.1093/bja/78.5.507 [DOI] [PubMed] [Google Scholar]
- 36.Brummett CM, Waljee JF, Goesling J, Moser S, Lin P, Englesbe MJ, et al. New persistent opioid use after minor and major surgical procedures in US adults. JAMA Surg. 2017;152(6):e170504. 10.1001/jamasurg.2017.0504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Franneby U, Sandblom G, Nyren O, Nordin P, Gunnarsson U. Self-reported adverse events after groin hernia repair, a study based on a national register. Value Health. 2008;11(5):927–32. 10.1111/j.1524-4733.2008.00330.x [DOI] [PubMed] [Google Scholar]
- 38.Sanchez-Manuel FJ, Seco-Gil JL. Antibiotic prophylaxis for hernia repair. Cochrane Database Syst Rev. 2003;2:CD003769. [DOI] [PubMed] [Google Scholar]
- 39.Fitzgibbons RJ Jr, Giobbie-Hurder A, Gibbs JO, Dunlop DD, Reda DJ, McCarthy M Jr, et al. Watchful waiting vs repair of inguinal hernia in minimally symptomatic men: a randomized clinical trial. JAMA. 2006;295(3):285–92. 10.1001/jama.295.3.285 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data sets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.