Abstract
Objective:
Colorectal cancer is one of the most common causes of death in the world. Despite of remarkable advances in medical sciences, cancer is an important disease and the second cause of death after cardiovascular diseases. The present study was aimed at determining the survival rate of colorectal cancer in Iran.
Methods:
The present study is a systematic review of national and international electronic databases. Studies that had the inclusion criteria were included in the study, electronically published articles over December 2007 and March 2015 were retrieved. The collected data were analyzed by meta-analytic method through stata 11.0 Software, and the survival rate was measured.
Results:
The 1-, 2-, 3-, 4-, and 5-year survival rates of colorectal cancer in Iran were respectively calculated as 85, 75.10, 65, 55.40, and 52. The results indicated that there is a significant relationship between anatomic location of tumor and survival rate. According to the results of this examination, survival rate of the patients with rectal cancer was 41.9 times higher than those with colorectal cancer.
Conclusion:
Due to the relative high prevalence of this cancer among young people in Iran and the low survival rate, early diagnosis of colorectal neoplasms is necessary before they become symptomatic through more effective diagnosis programs of enhancing the patients’ health and survival rate. Moreover, it is necessary to conduct more specialized and relevant studies in order to determine genetic or environmental causes of cancer such as diet and cultural and behavioral habits at the national level and with different ethnicities.
Keywords: Colorectal cancer, survival rate, meta, analysis, Iran
Introduction
Colorectal cancer (colon and rectum) is a common disease with different incidence in different areas of the world and is considered as a health problem in communities (Ansari et al., 2007; Khazaei et al., 2015). Despite of remarkable advances in medical sciences, cancer is an important disease and the second cause of death after cardiovascular diseases (Farzianpour et al., 2014; Jafari et al., 2015; Khazaei et al., 2016; Moradi et al., 2016). The results of different genetic, experimental, and epidemiological studies indicated that colorectal cancer develops as a result of mutual effects of genetic talent, environmental factors, and lifestyle (Ansari et al., 2007; Shadmani et al., 2017). The commonest symptoms in patients with colorectal cancer include stomachache, change in bowel habits, bleeding from rectum, weakness, anemia, and weight loss (Ford et al., 2008).
There have been reported 4,000 new cases of colorectal cancer and 1,150 deaths from it in Iran every year (Moradi et al., 2009). The age specific rate among women and men in Iran is 8.1 and 7.6 per 100,000; respectively (Akhoond et al., 2010). The prevalence of colorectal cancer is increasing in Asian and Western countries (Ponz de Leon et al., 2004). There has been a steady increase in colorectal cancer in Europe (Ponz de Leon et al., 2004; Sung et al., 2005) while in the US, the trend is increasing (Zheng et al., 2014). About 143,460 new cases of colorectal cancer are diagnosed in the United States every year. Approximately 51,690 Americans die of colorectal cancer every year, which accounts for 9% of all deaths caused by cancer in the United States (Jemal et al., 2013). Globally, progression of colorectal cancer is different, and this difference is over 10%. The highest rate of prevalence is related to Australia, New Zealand, Europe, and North America and the lowest to Africa and Central and South Asia. The prevalence rate of colorectal cancer in Iran is lower than Western Countries (Akhoond et al., 2010). It seems that geographical differences can lead to differences in diet and environment, which are obtained aster a background of genetic talent (Jemal et al., 2011). Incidence of colorectal cancer in ages below 40 years is not common. In Western countries, only 2-8% of all colorectal cancer cases occur in under-40 individuals while this figure is 15-35% in Middle Eastern countries and 17% in Iran (Angell-Andersen et al., 2004). This high rate of prevalence of colorectal cancer among young people is attributed to the age structure of the young in these countries and the rate of prevalence among the elderly compared to Western countries (Ansari et al., 2007). The reported 5-Year survival in Europe is 56% for men and 60% for women (Angell-Andersen et al., 2004; Omejc et al., 2004) [In their study conducted in England, Anwar et al., (2012) reported 5-year survival rate to be 50%. Farzianpour et al., (2013) indicated that the general quality of life among patients with cancer is low in Iran. Hosseini et al., (2014) carried out a review of clinical and pathological features and survival rate among 37,901 patients and reported 5-year survival rate to be 52.2%. Abbasi Asl et al., (2015) analyzed survival rate of patients with colorectal and prognostic factors and determined 1- and 5-year survival rates as 79.2 and 39.6 percent, respectively. Akhond et al., (2010) studied the effective factors on survival rate of patients with colon and rectum cancer and reported 1-, 2-, 3-, 4-, and 5-year survival rates of patients with colon cancer as respectively 88.7, 77.9, 68.5, 61.4, and 56.8 and for those with rectum cancer as 89.1, 74.2, 60.7, 47.1, and 41.9, respectively.
Survival rate in western countries has taken an increasing trend as a result of accurate diagnosis methods and prevention of tumor progression; therefore, the rate of mortality caused by cancer has dropped (Abbasi Asl et al., 2015). Recent studies indicated that colorectal cancer in Iran has remarkably increased, which is attributed to the change in lifestyle, tendency of diet toward western style, and advances in diagnosis methods (Ansari et al., 2007). Early diagnosis of this cancer in highly important because it is one of the most curable diseases if diagnosed early, and a major part of incidence of colorectal cancer is related to amendable diagnostic factors (Parsaee et al., 2015).
There are different results for the impacts of effective factors and survival rate of colon and rectum cancers in different studies. It is necessary to evaluate the total survival rate and the effect of clinical factors on colorectal cancer in order to inform the community to quickly refer to doctor and conduct examinations. Since meta-analysis is an important approach for combining the results (Moosazadeh, 2013; Moosazadeh et al., 2013) the present study was carried out in order to measure the survival rate of patients with colorectal cancer in Iran through meta-analysis.
Materials and Methods
Search strategy
To find the articles in the present study, prestigious national databases like SID, Magiran, and Irandoc and international ones such as PubMed, Google Scholar, Scopus, and Science Direct were visited and keywords like Iran, survival rate, rectum, colon, colorectal cancer, and their Persian equivalent were utilized. Moreover, the references of the articles were also employed to make sure about retrieving the whole articles. Electronically published articles over December 2007 and March 2015 were extracted.
Choosing the articles
All of the articles that studied the survival rate in colorectal, rectum, and colon cancers were included in the study without any restrictions. Repetitive and irrelevant cases were crossed out after their title, abstract and full text were examined. Moreover, in order to prevent the bias caused by republishing (transverse and longitudinal publication bias), the results of the studies published in 2 journals were utilized and one of them was crossed out.
Quality evaluation
To evaluate the quality of the selected articles, an inventory that was used in previous studies was employed (Moosazadeh et al., 2014). This inventory was developed by examining STROBE checklist (Von Elm et al., 2007) statement and composed of 12 questions that cover different aspects of methodology including determination of proper sample size, the type of the study, sampling method, study population, data collection method, definition of the variables, the method of examining the samples, data collection instruments, statistical tests, study objectives, presentation of the findings in an appropriate form, and presentation of the results according to the study objectives. Each question was given one score, and any study that received a minimum of 9 scores (Moosazadeh et al., 2014) was included for meta-analysis.
Inclusion criteria
All of the English and Persian articles that had determined 1-, 2-, 3-, 4-, and 5-year survival rates and gained the required score during quality evaluation were chosen.
Exclusion criteria
Studies that had not determined the survival rate and did not have enough data, abstracts whose full text format was not provided, articles whose sample size was not specified, articles that did not obtain the minimum evaluation score, and those that were case report, experimental-control group type, and interventional were crossed out.
Data extraction
The data of each article were extracted based on the study title, the first author, the study year, the study location, sample size, 1-, 2-, 3-, 4-, 5-, 7-, and 10-year survival rates, the significance level of the relationship between colorectal cancer survival rate and the variables of degree of cellular differentiation, type of morphology, family background, BMI, smoking background, alcohol consumption, age, gender, disease stage, tumor metastasis, metastasis to nearby lymph nodes, the type of the first treatment, tumor location, marital status, and the extent of penetration into intestinal wall. Moreover, two of the researchers registered the collected data into Excel.
Analysis
Stata Software was utilized to analyze the collected data. In the present study survival rate was examined among 15,877 colorectal cancer cases. In studies where the size of the female and male samples were registered separately, 8,688 men and 5,348 women participated. The median of survival rate ranged from 7.75 in the study conducted by Akhond et al., (2010) to 95.53 in the one carried out by Moghimi Dehbokri et al., (2008). Meta-regression test indicated that there was a significant relationship between cancer location and survival rate. According to the results of this test, the survival rate of rectum cancer was 41.9 times higher than that colon cancer, and that of colon cancer was 41.9 units more than those with colorectal cancer (colon and rectum were considered in one unit) (P-value<0.001, β =41.9).
The results of the Systematic research
The initial search in national and international databases led to finding 19,530 documents which decreased to 2,076 after the search strategy was changed and the features increased. By examining the title and summary of the articles, the number of the articles became 484. Moreover, 270 cases were crossed out due to the overlap among the databases. Afterwards, the full text version of 214 articles were considered for examining inclusion and exclusion criteria, which led to crossing out 185 cases that were not relevant or did not possess inclusion criteria. Moreover, 4 articles were retrieved by reviewing the references. Finally 28 articles (Zampino, 2004; Birgisson et al., 2005; Ansari et al., 2007; Moghimi et al., 2008; Asghari-Jafarabadi et al., 2009; Mehrkhani et al., 2009; Moradi et al., 2009; Razavi et al., 2009; Akhoond et al., 2010; Nasiri et al., 2010; Safaee et al., 2010; Karimi Zarchi et al., 2011; Tabatabaie et al., 2011; Esna-Ashari et al., 2012; Mehrabani et al., 2012; Saki Malehi et al., 2012; Abadi et al., 2013; Aryaie et al., 2013; Fekri, 2013a; Heidarnia et al., 2013; Omidvari et al., 2013; Sanei, 2013; Ahmadi et al., 2014; Akhavan et al., 2014; Gohari, 2014; Roshanaei et al., 2014; Vakili et al., 2014; Abbasi Asl, 2015; Parsaee et al., 2015) were considered for meta-analysis and systematic review (See Figure 1). Moreover, 3 articles (Asghari-Jafarabadi et al., 2009; Akhoond et al., 2010; Asghari Jafarabadi et al., 2013) were entered the study twice because they had reported survival rate of rectum and colon cancers separately.
Figure 1.
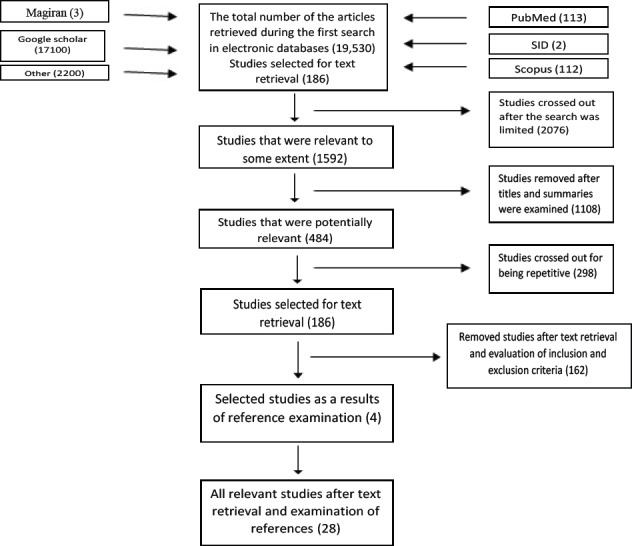
Search Procedure and Selection of the Initial Studies
Table 1.
The Properties of the Initial Studies Included in Meta-analysis in Relation with the Survival Rate of Colorectal Cancer
| Id | First author | publication year | Sample size | age average | Primary tumor site | Mean Survival | Median Survival | Overall Survival Rates,% | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1-y | 2-y | 3-y | 4-y | 5-y | ||||||||
| 1 | Moghimi Dehkordi | 2008 | 1127 | 53.59 | Colorectal | 105.1 | 95.53 | 91.1 | --- | 73.1 | --- | 61 |
| 2 | Mehrabani | 2012 | 243 | --- | Colorectal | --- | 36.06 | 9309 | --- | 50.3 | --- | 27.2 |
| 3 | Vakili | 2014 | 604 | 58.9 | Colorectal | 77.50 | 60 | 72.2 | --- | --- | --- | 50.1 |
| 4 | Tabatabai | 2011 | 26 | 56 | Colorectal | --- | --- | 48 | --- | --- | --- | 43 |
| 5 | Saki Malehi | 2012 | 739 | 59.7 | Colorectal | 42.46 | 22.8 | --- | --- | --- | --- | 63.3 |
| 6 | Roshanai | 2014 | 169 | --- | Colorectal | --- | 40 | 89 | --- | 54 | --- | 31 |
| 7 | Moradi | 2009 | 2192 | --- | Colorectal | --- | --- | 84 | 68 | 54 | 43 | 41 |
| 8 | Mehrkhani | 2009 | 1090 | --- | Colorectal | 42.84 | 44.3 | 72 | --- | 54 | --- | 47 |
| 9 | Heidarnia | 2013 | 559 | 63 | Colorectal | --- | --- | --- | --- | --- | --- | 68.3 |
| 10 | AsnaAshari | 2009 | 2342 | 58.13 | Colorectal | --- | --- | --- | --- | --- | --- | 47.36 |
| 11 | Abasiasl | 2015 | 88 | 56.6 | Colorectal | --- | 38.8 | 79.2 | --- | --- | --- | 39.6 |
| 12 | Ansari | 2007 | 237 | 58.15 | Colorectal | --- | --- | 80 | --- | --- | --- | 49 |
| 13 | Parsaee | 2015 | 241 | 56.62 | Colorectal | 3.09 | 39.35 | 81 | 66 | 53 | 44 | --- |
| 14 | Nasiri | 2010 | 109 | 50.5 | Colorectal | 42.8 | 44.3 | 72 | --- | 54 | --- | 47 |
| 15 | Ahmadi | 2013 | 1127 | 53.5 | Colorectal | --- | 68.83 | --- | --- | --- | --- | --- |
| 16 | Aryaie | 2013 | 227 | Colorectal | 43.4 | 42.8 | --- | --- | --- | --- | --- | |
| 17 | Gohari | 2014 | 724 | 53.03 | Colorectal | --- | 104 | --- | --- | --- | --- | --- |
| 18 | Safaee | 2010 | 110 | --- | Colorectal | 91.51 | 48.6 | 92.6 | --- | 80.1 | --- | 41.3 |
| 19 | Karimi Zarchi | 2011 | 241 | 59.7 | Colorectal | 56.5 | --- | --- | --- | --- | --- | --- |
| 20 | Akhond | 2010 | 1194 | --- | Colon | --- | 7.75 | 88.7 | 77.9 | 68.5 | 61.4 | 56.8 |
| 21 | Razavi | 2009 | 91 | --- | Colon | --- | --- | --- | --- | --- | --- | --- |
| 22 | Fekri | 2013 | 131 | 57.36 | Colon | 36.03 | 43.73 | 76 | 62 | 56 | 44 | --- |
| 23 | Asghari Jafarabadi | 2013 | 67 | --- | Colon | --- | --- | 82.6 | --- | 58.51 | --- | 46.79 |
| 24 | Asghari Jafarabadi | 2009 | 817 | 53.56 | Colon | 111.82 | --- | 91.7 | 83.7 | 75.9 | 69 | 63.3 |
| 25 | Ababi | 2013 | 580 | --- | Colon | --- | --- | --- | --- | --- | --- | 67.06 |
| 26 | Akhond | 2010 | 1194 | --- | Rectum | --- | 3.917 | 89.1 | 74.2 | 60.7 | 47.1 | 41.9 |
| 27 | Asghari Jafarabadi | 2013 | 27 | --- | Rectum | --- | --- | 91.52 | --- | 76.65 | --- | 65.58 |
| 28 | Asghari Jafarabadi | 2009 | 402 | 55.3 | Rectum | 135.95 | --- | 96 | 91.2 | 84 | 78.2 | 76 |
| 29 | Akhavan | 2014 | 119 | --- | Rectum | --- | --- | 97 | --- | 88 | --- | 55 |
| 30 | Omidvari | 2013 | 153 | 57.15 | Rectum | --- | --- | --- | --- | --- | --- | 53.4 |
| 31 | Sanei | 2013 | 101 | --- | Rectum | 64.45 | 72 | --- | --- | --- | --- | --- |
Results
Degree of cellular differentiation
Six studies (Ansari et al., 2007; Akhoond et al., 2010) (Moghimi et al., 2008; Mehrkhani et al., 2009; Nasiri et al., 2010; Saki Malehi et al., 2012) reported that there was a significant relationship between survival rate of patients with colorectal cancer and degree of cellular differentiation, such that patients with higher differentiation degree had the highest survival rate and those with lower differentiation degree had the lowest survival rate.
Morphology type
Three articles (Moghimi et al., 2008; Saki Malehi et al., 2012; Roshanaei et al., 2014) reported that there is a significant relationship between morphology and survival rate in a way that the morphology of tumor has been introduced as a prognostic factor for colorectal cancer (Saki Malehi et al., 2012).
Family background
Three articles (Moghimi et al., 2008; Safaee et al., 2010; Ahmadi et al., 2014) reported that there is a relationship between family background and survival rate. For example the study of Ahmadi et al., (2014) showed that 36.8% of the patients with colorectal cancer had positive family background.
BMI
Four studies (Moghimi et al., 2008; Asghari-Jafarabadi et al., 2009; Akhoond et al., 2010; Omidvari et al., 2013) reported that there is a relationship between BMI and survival rate in a way that patients with a BMI lower than 18.5 had a shorter survival time (Asghari-Jafarabadi et al., 2009).
Table 2.
Evaluation of Survival Rate of Patients with Colorectal Cancer in Iran Through Meta-analysis
| survival | Percent of survival | Heterogeneity | ||
|---|---|---|---|---|
| Q | I-squared (%) | P-Value | ||
| One year | 85 (82-88) | 452.02 | 95.8 | <0.001 |
| Two year | 75.1 (68.2-81.9) | 240.1 | 97.5 | <0.001 |
| Three year | 65 (59-71) | 505.9 | 97 | <0.001 |
| Four year | 55.4 (45.1-65.7) | 397.7 | 98.5 | <0.001 |
| Five year | 52 (47-56) | 709.4 | 96.9 | <0.001 |
Smoking background
Four studies (Ansari et al., 2007; Moghimi et al., 2008; Vakili et al., 2014; Parsaee et al., 2015) reported that there is a relationship between smoking background and survival rate. The mortality risk of smoking patients was 3.356 times more than non-smoking ones (Parsaee et al., 2015).
Diagram 2.
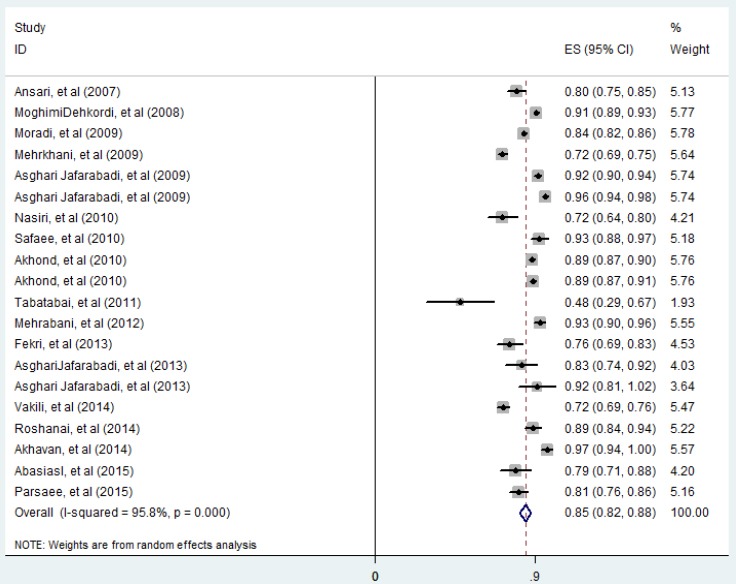
One-year Survival
Diagram 3.
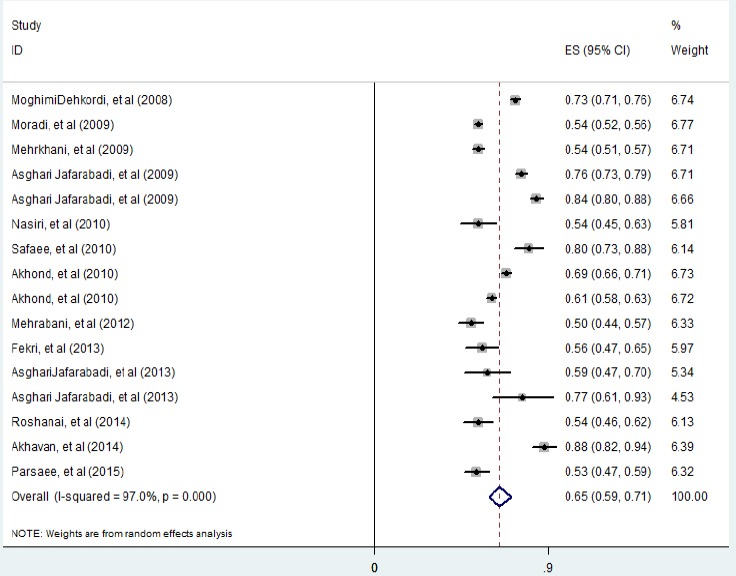
Three-year Survival
Diagram 4.
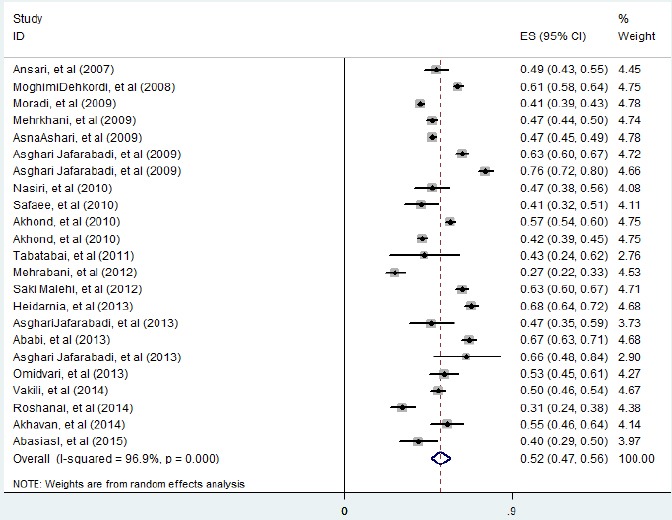
Five-year Survival
Alcohol consumption
Three articles reported a relationship between alcohol consumption and survival rate (Akhoond et al., 2010; Mehrabani et al., 2012; Fekri N, 2013b) in a way that survival rate in the non-alcoholic group was significantly higher than the patients who had alcohol consumption background (Mehrabani et al., 2012).
Age
Twelve studies (Ansari et al., 2007; Moghimi et al., 2008; Mehrkhani et al., 2009; Nasiri et al., 2010; Safaee et al., 2010; Tabatabaie et al., 2011; Mehrabani et al., 2012; Saki Malehi et al., 2012; Abadi et al., 2013; Omidvari et al., 2013; Roshanaei et al., 2014; Vakili et al., 2014) reported a relationship between age and survival rate of patients with colorectal cancer in a way that 11.8% of patients with colorectal cancer were under 40 years old at the time of diagnosis (Ansari et al., 2007).
Gender
Six articles (Ansari et al., 2007; Moghimi et al., 2008; Safaee et al., 2010; Tabatabaie et al., 2011; Mehrabani et al., 2012; Vakili et al., 2014) indicated that there is relationship between gender and survival rate of the patients in a way that the number of male patients was more than female ones, and women’s diagnosis age of patients was lower than men’s (Ahmadi et al., 2014; Norouzirad et al., 2017).
Disease stage
A significant relationship was reported between disease stage and survival rate of the patients in 8 articles (Ansari et al., 2007; Moghimi et al., 2008; Asghari-Jafarabadi et al., 2009; Mehrkhani et al., 2009; Nasiri et al., 2010; Saki Malehi et al., 2012; Fekri N, 2013a; Parsaee et al., 2015) such that in a stage that there is distant metastasis, the lowest survival rate was observed (Ansari et al., 2007). The mortality risk of patients in stage III was 5.043 times than that of those in stage I. Moreover, the mortality risk for patients in stage II was 1.148 times higher than those in stage I. And, the mortality risk of patients in stage II was 1.036 times higher than those in stage I (Ansari et al., 2007).
Tumor metastasis
Eight articles (Moghimi et al., 2008; Asghari-Jafarabadi et al., 2009; Akhoond et al., 2010; NASIRI et al., 2010; Mehrabani et al., 2012; Omidvari et al., 2013; Roshanaei et al., 2014; Abbasi Asl, 2015) reported a relationship between tumor metastasis and survival rate of the patients in a way that the mortality risk of individuals with metastasis who have referred to other centers was 3.26 times more that those without it (Abbasi Asl, 2015). The study conducted by Akhond et al., (2010) reported that the mortality risk of individuals with tumor metastasis that referred to other centers was 3.577 for colon cancer and 2.646 for rectum cancer compared to those without it.
Metastasis to nearby lymph nodes
The relationship between metastasis to nearby lymph nodes and survival rate of the patients is mentioned in 3 articles (Moghimi et al., 2008; Tabatabaie et al., 2011; Saki Malehi et al., 2012) in a way that there was a significant relationship between presence of various metastases and a reduction in survival rate of patients (Tabatabaie et al., 2011). Patients with more metastases had a lower 1-year survival rate (Tabatabaie et al., 2011).
First treatment type
Five articles (Moghimi et al., 2008; Asghari-Jafarabadi et al., 2009; Akhoond et al., 2010; Mehrabani et al., 2012; Abbasi Asl, 2015) reported a relationship between first treatment type and survival rate of the patients in a way that first treatment type affects the improvement in the patients’ survival, and the patients insistence in order to complete the treatment stages and also supplement medicines can be effective in enhancing the survival rate of the patients(Abbasi Asl, 2015).
Tumor location
A significant relationship between survival rate and tumor location was reported in 3 articles (Ansari et al., 2007; Safaee et al., 2010; Mehrabani et al., 2012) in a way that comparing 1-year survival rate with different involved locations indicates that the lowest survival rate is observed among patients with rectum and recto-sigmoid (Ansari et al., 2007).
Marital status
Three articles (Moghimi et al., 2008; Asghari-Jafarabadi et al., 2009; Mehrabani et al., 2012) were reported a relationship between marital status and survival rate of the patients.
The Extent of penetration into intestinal wall
Two articles (Moghimi et al., 2008; Nasiri et al., 2010) showed that there is a relationship between the extent of penetration into intestinal wall and survival rate of the patients.
Discussion
In the present meta-analysis, the 1-, 2-, 3-, 4-, and 5-yearsurvival rate of colorectal cancer was respectively 85, 75.10, 65, 55.40, and 52. The results indicated that anatomic location of tumor had a significant effect on survival rate. According to the results of this examination, survival rate of the patients with rectum was 41.9 units more than those with colon, and the survival rate of those with colon was 41.9 units more than those with colorectal cancer (colon and rectum were considered as one unit). The results of the study carried out by Birgisson et al., (2005) in Sweden indicated that 5-year survival rate for colon and rectum cancers were respectively 57.2 and 57.6%. Labianca et al., (2004) and Zampino et al., (2004) presented similar results for colon and rectum cancers, respectively. In their study in England, van der Pool et al., (2012) reported 5-year survival rate to be over 50%. Mitry et al., (2005) carried out a study in France and reported 5-year survival rate as 56.3%. Ansari et al., (2007) indicated 5-year survival rate with involvement of different places in colon and observed the lowest survival rate in patients with rectum involvement. Rectum tumors are more accessible and show more symptoms; therefore, they are quicker to diagnose. The results of the study carried out by Rosenberg et al., (2008) indicated that rectum tumors had worse prognosis compared to colon tumors.
Degree of cellular differentiation is a significant diagnostic factor for colon cancer. Survival rate of patients whose tumors were differentiated well was 2.7 times more than those whose tumors were poorly differentiated (Asghari-Jafarabadi et al., 2009). Liang et al., (2006) reported a significant relationship between survival rate of patients with colon cancer and the degree of differentiation. Park et al., (1999) concluded that tumor degree had a stronger relationship with rectum cancer.
Different studies have reported different results in regard with the relationship between BMI and survival rate of the patients. Asghari-Jafarbadi et al., (2009) reported that individuals with BMI of 25-29.9 have the lowest rate of mortality risk caused by colon and rectum cancers while those with BMI of lower than 18.5 have the highest mortality risk. Murphy et al., (2000) concluded that obesity increases the risk of mortality from colon cancer especially among men. Shibakita et al., (2005) showed that BMIs of below 21 and over 24 are associated with an increase in mortality risk caused by colorectal cancer. Hines et al., (2009) concluded that patients with colon cancer, low weight enhances mortality while high weight and obesity reduces it. The differences between the results of the studies can be attributed to different factors related to survival rate and the selected study population.
Having metastasis is one of the variables that has a significant relationship with survival rate and is considered as one of the most important health problems of the community, and the survival rate of such patients can be improved to some extent through therapeutic methods like chemotherapy (Saletti, 2006). In the study carried out by Liang et al., (2006), metastasis to lymph node is an important factor in survival rate of patients with colon cancer.
The type of the first treatment is one of the effective factors in survival rate of colorectal cancer in a way that the survival of the patients who had received chemotherapy, radiotherapy or immunotherapy was about 2.3 times more than those who had received surgery (Asghari-Jafarabadi et al., 2009). The results of the study carried out by Lang et al., (2009) indicated that treating colon cancer through surgery and rectum cancer through a combined method (surgery, chemotherapy and radiotherapy) were commoner than other treatment methods.
Iran has a young population. The results of the study conducted by Parsaee et al., (2015) indicated that the affliction proportion among the age group below 50 years was 29.3% which is approximately high. The results of the studies carried out in European countries indicated that only lower than 20% of colorectal cancer cases occurred in individuals of below 50 years (Van der Pool et al., 2012). Rebecca et al., (2009) carried out a study in the United States and concluded that there has been an increase in the rate of colorectal cancer among young people aging 20-49 years (Siegel et al., 2009). In some studies conducted in Iran, the minimum age of colorectal cancer was reported 7 years (Yekta, 2004). The high proportion of colorectal cancer among young people can be justified through two main hypotheses: young population and genetic factors because different cancers related to genetic factors have been seen among young people (Ahdami, 2008.; Frankel and D’angelica, 2014).
The results of different studies indicated that the number of men with colorectal cancer is more than women. A study was carried out in England aimed at comparing the incidence of colorectal cancer among women and men, and the results indicated that the incidence among men was 47% more than women (Hayne et al., 2001). On the other hand, the results of another study conducted in the United States indicated that 51.1% of men were afflicted by colorectal cancer, and there was no significant difference between men and women in this regard (Rabeneck et al., 2003). Neagoe et al., (2004) studies Romanian patients. The results of their study indicated that the proportion of male to female patients was more and the gender proportion was 1.51. The hypothesis that the survival of women is higher, which can be attributed to hormonal and immune factors responsible for different rates of colon and rectum cancers among men and women. Due to secretion of steroids, women have a higher survival rate against these two cancers. The results of the study conducted by Ahmadi et al., (2014) indicated that there was a significant difference between men and women in regard with the diagnosis age in a way that women pay more attention to medical care than men and take part in screening programs than men.
The results of some studies confirm an increase in the risk of colorectal cancer caused by smoking more than its effect on rectum cancer (Nagata, 1999; Chao et al., 2000; Giovannucci, 2001). There is the assumption that smoking is an initiator of CRV (Giovannucci, 1994). A study conducted in the United States reported that smoking increases mortality risk after the diagnosis of colorectal cancer (Phipps and Newcomb, 2011). The results of some studies indicated that there is a significant relationship between alcohol consumption and mortality risk in colon cancer. In a prospective study carried out on 6,291 patients over 1985-2005 by Yi et al., (2010) it was concluded that the mortality rate among alcoholic men with colorectal cancer was 4.9 time more than non-alcoholic ones.
Development of colorectal cancer in first-degree relatives can enhance the development risk of this cancer by 2-3 times (Chan and Niedzwiecki, 2008). Fuchs reported that this increase is higher in rectum cancer (Fuchs, 1994). while Mahdavinia et al., (2005) did not observe the effect of family background on right colon cancer. In the study carried out by Ahmadi et al., (2013) the mortality rate in patients with family background of colorectal cancer was more than those without it which can be attributed togr early screening and diagnosis and preventive measures among those with family background.
Among the limitations of the present study, one can refer to the fact that most studies considered colon and rectum cancers as one unit (colorectal cancer) while they need to be taken into account due to physiological and anatomic aspects, environmental carcinogens, genetic mechanism, and subsections of the large intestine, which will result in more precise results.
In conclusion, since the incidence of colorectal cancer in all age groups is lower in Iran than Western countries, it is necessary to design a screening program for colorectal cancer from young ages in Iran compared to Western countries. Administering a screening program not only leads to a reduction in the incidence of colorectal cancer but also improves the total survival. Public education of people and specialized education of doctors in order to diagnose colorectal cancer at early stages of the disease can help the healthcare policymakers and program designers have access to and provide high quality services, diagnose, and treat the patients. Moreover, it is necessary to conduct more specialized and relevant studies in order to determine genetic or environmental causes of cancer such as diet and cultural and behavioral habits at the national level and with different ethnicities.
Conflicts of interest
The authors declare no conflict of interest.
References
- 1.Abadi A, Ahmadi F, Majd HA, et al. The estimation of survival function for colon cancer data in tehran using non-parametric bayesian model. Iran J Cancer Prev. 2013;6:141. [PMC free article] [PubMed] [Google Scholar]
- 2.Abbasi Asl M BF, Gohari M, Roudbary M, Khodabakhshi R. Survival analysis of colorectal cancer patients and its prognostic factors using cox regression. Razi J Med Sci. 2015;22:21–8. [Google Scholar]
- 3.Ahdami HO HD, Trichopoulos D. Textbook of cancer epidemiology. 2008;5:275–97. [Google Scholar]
- 4.Ahmadi A, Mobasheri M, Hashemi Nazari SS. Survival time and relative risk of death in patients with colorectal cancer in an Iranian population:a cohort study. J Mazandaran Univ Med Sci. 2014;24:2–8. [Google Scholar]
- 5.Akhavan A, Binesh F, Soltani A. Survival of rectal cancer in Yazd, Iran. Asian Pac J Cancer Prev. 2014;15:4857–60. doi: 10.7314/apjcp.2014.15.12.4857. [DOI] [PubMed] [Google Scholar]
- 6.Akhoond MR, Kazemnejad A, Hajizadeh E, et al. Comparison of colon and rectum cancer:survival and prognostic factors. Gastroenterol Hepatol Bed Bench. 2010;3:177–86. [Google Scholar]
- 7.Angell-Andersen E, Tretli S, Coleman M, et al. Colorectal cancer survival trends in Norway 1958–1997. Eur J Cancer. 2004;40:734–42. doi: 10.1016/j.ejca.2003.09.034. [DOI] [PubMed] [Google Scholar]
- 8.Ansari R, Amjadi H, Norozbeigi N, et al. Survival analysis of colorectal cancer in patients underwent surgical operation in Shariati and Mehr Hospital-Tehran, in a retrospective study. Govaresh. 2007;12:7–15. [Google Scholar]
- 9.Anwar S, Fraser S, Hill J. Surgical specialization and training–its relation to clinical outcome for colorectal cancer surgery. J Eval Clin Pract. 2012;18:5–11. doi: 10.1111/j.1365-2753.2010.01525.x. [DOI] [PubMed] [Google Scholar]
- 10.Aryaie M, Roshandel G, Semnani S, et al. Predictors of colorectal cancer survival in Golestan, Iran:a population-based study. Epidemiol Health. 2013;35:1–6. doi: 10.4178/epih/e2013004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Asghari-Jafarabadi M, Hajizadeh E, Kazemnejad A, et al. Site-specific evaluation of prognostic factors on survival in Iranian colorectal cancer patients:a competing risks survival analysis. Asian Pac J Cancer Prev. 2009;10:815–21. [PubMed] [Google Scholar]
- 12.Asghari Jafarabadi M, Mohammadi SM, Hajizadeh E, et al. An evulation of 5-year survival of metastatic colon and rectal cancer patients using cumulative incidence models. Koomesh. 2013;14:207–14. [Google Scholar]
- 13.Birgisson H, Talbäck M, Gunnarsson U, et al. Improved survival in cancer of the colon and rectum in Sweden. Eur J Surg Oncol. 2005;31:845–53. doi: 10.1016/j.ejso.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 14.Chan J MJ, Niedzwiecki D. Family history of colorectal cancer:a new survival predictor of colon cancer? JAMA. 2008;299:2515–23. doi: 10.1001/jama.299.21.2515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chao A, Thun MJ, Jacobs EJ, et al. Cigarette smoking and colorectal cancer mortality in the cancer prevention study II. J Natl Cancer Inst. 2000;92:1888–96. doi: 10.1093/jnci/92.23.1888. [DOI] [PubMed] [Google Scholar]
- 16.Esna-Ashari F, Sohrabi M, Abadi A, et al. Colorectal cancer prevalence according to survival data in Iran-2007. Iran J Cancer Prev. 2012;2:15–8. [Google Scholar]
- 17.Farzianpour F, Shojaee J, Abedi G, et al. Assessment of quality of life in cancer patients. Am J Agri Biol Sci. 2014;9:147. [Google Scholar]
- 18.Fekri N P, Shahid sales S, Amini AR, Esmaeily H. detection of effective factors in the survival rate of colon cancer patients using Survival modeling. J North Khorasan Univ Med Sci. 2013a;5:629. [Google Scholar]
- 19.Fekri NP, Shahid sales S, Amini AR, Esmaeily H. detection of effective factors in the survival rate of colon cancer patients using Survival modeling. J North Khorasan Univ Med Sci. 2013b;5:621–9. [Google Scholar]
- 20.Ford AC, van Zanten SJV, Rodgers CC, et al. Diagnostic utility of alarm features for colorectal cancer:systematic review and meta-analysis. Gut. 2008;57:1545–53. doi: 10.1136/gut.2008.159723. [DOI] [PubMed] [Google Scholar]
- 21.Frankel TL, D'angelica MI. Hepatic resection for colorectal metastases. J Surgical Oncol. 2014;109:2–7. doi: 10.1002/jso.23371. [DOI] [PubMed] [Google Scholar]
- 22.Fuchs C GE, Golditz G. A prospective study of family history and the risk of colorectal cancer. N Engl J Med. 1994;331:1669–74. doi: 10.1056/NEJM199412223312501. [DOI] [PubMed] [Google Scholar]
- 23.Giovannucci E. An updated review of the epidemiological evidence that cigarette smoking increases risk of colorectal cancer. Cancer Epidemiol Biomarkers Prev. 2001;10:724–31. [PubMed] [Google Scholar]
- 24.Giovannucci E, Stampfer MJ, Colditz GA, et al. A prospective study of cigarette smoking and risk of colorectal adenoma and colorectal cancer in U.S. J Nat Cancer Inst. 1994;86:183–91. doi: 10.1093/jnci/86.3.183. [DOI] [PubMed] [Google Scholar]
- 25.Gohari M BA, Orooji A, Pourhosseingholi M. Estimation of prediction error for survival status with application in colorectal cancer. Sci Res J Shahed Univ. 2014;21:1–7. [Google Scholar]
- 26.Hayne D, Brown R, McCormack M, et al. Current trends in colorectal cancer:site, incidence, mortality and survival in England and Wales. Clin Oncol. 2001;13:448–52. doi: 10.1053/clon.2001.9311. [DOI] [PubMed] [Google Scholar]
- 27.Heidarnia MA, Monfared ED, Akbari ME, et al. Social determinants of health and 5-year survival of colorectal cancer. Asian Pac J Cancer Prev. 2013;14:5111–6. doi: 10.7314/apjcp.2013.14.9.5111. [DOI] [PubMed] [Google Scholar]
- 28.Hines RB, Shanmugam C, Waterbor JW, et al. Effect of comorbidity and body mass index on the survival of African-American and Caucasian patients with colon cancer. Cancer. 2009;115:5798–806. doi: 10.1002/cncr.24598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hoseini S, Moaddabshoar L, Hemati S, et al. An overview of clinical and pathological characteristics and survival rate of colorectal cancer in Iran. Ann Colorectal Res J. 2014;2:1–8. [Google Scholar]
- 30.Jafari M, Moradi Y, Khodadost M, et al. Trend of the esophageal cancer incidence in Iran. Int J Travel Med Glob Health. 2015;3:127–31. [Google Scholar]
- 31.Jemal A, Bray F, Center MM, et al. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 32.Jemal A, Simard EP, Dorell C, et al. Annual report to the nation on the status of cancer 1975–2009, featuring the burden and trends in human papillomavirus (HPV)–associated cancers and HPV vaccination coverage levels. J Natl Cancer Inst. 2013;105:175–201. doi: 10.1093/jnci/djs491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Khazaei S, Rezaeian S, Ayubi E, et al. Global prostate cancer incidence and mortality rates according to the human development index. Asian Pac J Cancer Prev. 2016;17:3791–4. [PubMed] [Google Scholar]
- 34.Khazaei S, Rezaeian S, Mansori K, et al. Effects of human development index and its components on colorectal cancer incidence and mortality:a global ecological study. Asian Pac J Cancer Prev. 2015;17:253–6. doi: 10.7314/apjcp.2016.17.s3.253. [DOI] [PubMed] [Google Scholar]
- 35.Karimi Zarchi AA, Saadat AR, Jalalian HR, Esmaeili M. Epidemiology and survival analysis of colorectal cancer and its related factors. Kowsar Med J. 2011;15:239–43. [Google Scholar]
- 36.Lang K, Korn JR, Lee DW, et al. Factors associated with improved survival among older colorectal cancer patients in the US:a population-based analysis. BMC Cancer. 2009;9:227. doi: 10.1186/1471-2407-9-227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liang H, Wang X-N, Wang B-G, et al. Prognostic factors of young patients with colon cancer after surgery. World J Gastroenterol. 2006;12:1458. doi: 10.3748/wjg.v12.i9.1458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mahdavinia M BF, Ansari R, Norouzbeigi N, et al. Family history of colorectal cancer in Iran. BMC Cancer. 2005;5:1–6. doi: 10.1186/1471-2407-5-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mahdavinia M, Bishehsari F, Ansari R, et al. Family history of colorectal cancer in Iran. BMC Cancer. 2005;5:112. doi: 10.1186/1471-2407-5-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mehrabani D, Almasi-Hashiani A, Moshfeghi K, et al. Survival rate and its predictors in colorectal cancer patients, Southern Iran. Middle East J Sci Res. 2012;12:1072–7. [Google Scholar]
- 41.Mehrkhani F, Nasiri S, Donboli K, et al. Prognostic factors in survival of colorectal cancer patients after surgery. Colorectal Dis. 2009;11:157–61. doi: 10.1111/j.1463-1318.2008.01556.x. [DOI] [PubMed] [Google Scholar]
- 42.Moghimi DB, Safaei A, Zali MR. Survival rates and prognostic factors in colorectal cancer patients. J Ilam Univ Med Sci. 2008;7:45–53. [Google Scholar]
- 43.Moosazadeh M. Meta-analysis of prevalence of smoking in 15-64-year-old population of west of Iran. Int J Prev Med. 2013;4:1108. [PMC free article] [PubMed] [Google Scholar]
- 44.Moosazadeh M, Nekoei-moghadam M, Emrani Z, et al. Prevalence of unwanted pregnancy in Iran:a systematic review and meta-analysis. Int J Health planning Manage. 2014;29:277–90. doi: 10.1002/hpm.2184. [DOI] [PubMed] [Google Scholar]
- 45.Moosazadeh M, Ziaaddini H, Mirzazadeh A, et al. Meta-analysis of smoking prevalence in Iran. Addict Health. 2013;5:140. [PMC free article] [PubMed] [Google Scholar]
- 46.Moradi A, Khayamzadeh M, Guya MM, et al. Survival of colorectal cancer in Iran. Asian Pac J Cancer Prev. 2009;10:583–6. [PubMed] [Google Scholar]
- 47.Murphy TK, Calle EE, Rodriguez C, et al. Body mass index and colon cancer mortality in a large prospective study. Am J Epidemiol. 2000;152:847–54. doi: 10.1093/aje/152.9.847. [DOI] [PubMed] [Google Scholar]
- 48.Nagata C SH, Kametani M, Takeyama N, Ohnuma T, Matsushita S. Cigarette smoking, alcohol use, and colorectal adenoma in Japanese men and women. Dis Colon Rectum. 1999;42:337–42. doi: 10.1007/BF02236350. [DOI] [PubMed] [Google Scholar]
- 49.Nasiri S, Sorush A, Karamnezhad M, et al. Prognostic factors in the survival rate of colorectal cancer patients after surgery. Iran J Surg. 2010;18:50–6. [Google Scholar]
- 50.Neagoe A, Molnar AM, Acalovschi M, et al. Risk factors for colorectal cancer:an epidemiologic descriptive study of a series of 333 patients. Rom J Gastroenterol. 2004;13:187–93. [PubMed] [Google Scholar]
- 51.Norouzirad R, Khazaei Z, Mousavi M, et al. Epidemiology of common cancers in Dezful county, southwest of Iran. Immunopathologia Persa. 2017;4:1–7. [Google Scholar]
- 52.Omejc M, Stor Z, Juvan R, et al. Colorectal cancer in Slovenia at the turn of the centuryKolorektales Karzinom in Slowenien um die Jahrhundertwende. Eur Surg. 2004;36:356–9. [Google Scholar]
- 53.Omidvari S, Hamedi SH, Mohammadianpanah M, et al. Comparison of abdominoperineal resection and low anterior resection in lower and middle rectal cancer. J Egypt Natl Canc Inst. 2013;25:151–60. doi: 10.1016/j.jnci.2013.06.001. [DOI] [PubMed] [Google Scholar]
- 54.Park YJ, Park KJ, Park JG, et al. Prognostic factors in 2230 Korean colorectal cancer patients:analysis of consecutively operated cases. World J Surg. 1999;23:721–6. doi: 10.1007/pl00012376. [DOI] [PubMed] [Google Scholar]
- 55.Parsaee R, Fekri N, Shahid SS, et al. Prognostic factors in the survival rate of colorectal cancer patients. J North Khorasan Univ Med Sci. 2015;7:45–53. [Google Scholar]
- 56.Phipps AI BJ, Newcomb PA. Prediagnostic smoking history, alcohol consumption, and colorectal cancer survival:the Seattle colon cancer family registry. Cancer. 2011;117:4948–57. doi: 10.1002/cncr.26114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ponz de Leon M, Marino M, Benatti P, et al. Trend of incidence, subsite distribution and staging of colorectal neoplasms in the 15-year experience of a specialised cancer registry. Ann Oncol. 2004;15:940–6. doi: 10.1093/annonc/mdh224. [DOI] [PubMed] [Google Scholar]
- 58.Rabeneck L, El-Serag HB, Davila JA, et al. Outcomes of colorectal cancer in the United States:No change in survival (1986–1997) Am J Gastroenterol. 2003;98:471. doi: 10.1111/j.1572-0241.2003.07260.x. [DOI] [PubMed] [Google Scholar]
- 59.Razavi S, Rezaee Salim M, Attarian H, et al. Comparison of the effect of standard chemotherapy and its combination with cetuximab on the survival of patients with progressive colon cancer. Razi J Med Sci. 2009;16:1–8. [Google Scholar]
- 60.Rosenberg R, Friederichs J, Schuster T, et al. Prognosis of patients with colorectal cancer is associated with lymph node ratio:a single-center analysis of 3026 patients over a 25-year time period. Ann Surg. 2008;248:968–78. doi: 10.1097/SLA.0b013e318190eddc. [DOI] [PubMed] [Google Scholar]
- 61.Roshanaei G, Komijani A, Sadighi A, et al. Prediction of survival in patients with colorectal cancer referred to the Hamadan MRI center using of Weibull parameter model and determination of its risk factors during 2005-2013. J Arak Univ Med Sci. 2014;16:41–9. [Google Scholar]
- 62.Safaee A, Moghimi-Dehkordi B, Fatemi S, et al. Characteristics of colorectal mucinous adenocarcinoma in Iran. Asian Pac J Cancer Prev. 2010;11:1373–5. [PubMed] [Google Scholar]
- 63.Saki Malehi A, Hajizadeh E, Fatemi R. Evaluation of prognostic variables for classifying the survival in colorectal patients using the decision tree. Iran J Epidemiol. 2012;8:13–9. [Google Scholar]
- 64.Saletti P, Cavalli F. Metastatic colorectal cancer. Cancer Treat Rev. 2006;32:557–71. doi: 10.1016/j.ctrv.2006.07.005. [DOI] [PubMed] [Google Scholar]
- 65.Sanei B MM, Kolahdozan M, Mehrabi Koushki A, et al. Srvival rate and recurrence in rectal cancer patients in Isfahan. Isfahan Univ Med Sci. 2013;31:1194–207. [Google Scholar]
- 66.Shadmani FK, Ayubi E, Khazaei S, et al. Geographic distribution of the incidence of colorectal cancer in Iran:a population-based study. Epidemiol Health. 2017;39:e2017020. doi: 10.4178/epih.e2017020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Shibakita M, Yoshimura H, Tachibana M, et al. Body mass index influences long-term outcome in patients with colorectal cancer. Hepatogastroenterology. 2010;57:62–9. [PubMed] [Google Scholar]
- 68.Siegel RL, Jemal A, Ward EM. Increase in incidence of colorectal cancer among young men and women in the United States. Cancer Epidemiol Prev Biomarkers. 2009;18:1695–8. doi: 10.1158/1055-9965.EPI-09-0186. [DOI] [PubMed] [Google Scholar]
- 69.Sung JJ, Lau JY, Goh K, et al. Increasing incidence of colorectal cancer in Asia:implications for screening. Lancet Oncol. 2005;6:871–6. doi: 10.1016/S1470-2045(05)70422-8. [DOI] [PubMed] [Google Scholar]
- 70.Tabatabaie SA, Hashemi SM, Ahmadi A. Prognostic factor and survival of patients with colorectal cancer after resection of pulmonary metastases. J Isfahan Med Sch. 2011;28:1–6. [Google Scholar]
- 71.Vakili M, Aghakoochak A, Pirdehghan A, et al. The survival rate of patients with colorectal cancer in Yazd during 2001-2011. J Shaheed Sadoughi Univ Med Sci. 2014;22:1187–95. [Google Scholar]
- 72.Van der Pool A, Damhuis R, Ijzermans J, et al. Trends in incidence, treatment and survival of patients with stage IV colorectal cancer:a population-based series. Colorectal Dis. 2012;14:56–61. doi: 10.1111/j.1463-1318.2010.02539.x. [DOI] [PubMed] [Google Scholar]
- 73.Von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement:guidelines for reporting observational studies. PLoS Med. 2007;4:e296. doi: 10.1371/journal.pmed.0040296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Yekta Z MR, Norooziniya F, Mohammadi P. Epidemiology of colorectal cancer in patients with colorectal cancer in West Azarbaijan. Tbib-e-Shargh J. 2004;1:167–72. [Google Scholar]
- 75.Yi SW SJ, Linton JA, Nam CM, Ohrr H. Alcohol consumption and digestive cancer mortality in Koreans:The Kangwha cohort study. J Epidemiol. 20:204–11. doi: 10.2188/jea.JE20090077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Zampino MG LR, Beretta G, Gatta G, et al. Rectal cancer. Crit Rev Oncol Hematol. 2004;51:121–43. doi: 10.1016/j.critrevonc.2004.03.004. [DOI] [PubMed] [Google Scholar]
- 77.Zheng XE, Li T, Lipka S, et al. Location-dependent ethnic differences in the risk of colorectal adenoma:a retrospective multiethnic study. J Clin Gastroenterol. 2014;48:1–7. doi: 10.1097/MCG.0b013e3182834989. [DOI] [PubMed] [Google Scholar]


