Publisher's Note: There is a Blood Commentary on this article in this issue.
Key Points
Venetoclax plus decitabine or azacitidine showed tolerable safety and favorable overall response rate (CR + CRi rate: 67%) in elderly patients with AML.
This novel combination regimen produced favorable responses in high-risk groups, such as age 75 or older, poor cytogenetics, and secondary AML.
Abstract
Older patients with acute myeloid leukemia (AML) respond poorly to standard induction therapy. B-cell lymphoma 2 (BCL-2) overexpression is implicated in survival of AML cells and treatment resistance. We report safety and efficacy of venetoclax with decitabine or azacitidine from a large, multicenter, phase 1b dose-escalation and expansion study. Patients (N = 145) were at least 65 years old with treatment-naive AML and were ineligible for intensive chemotherapy. During dose escalation, oral venetoclax was administered at 400, 800, or 1200 mg daily in combination with either decitabine (20 mg/m2, days 1-5, intravenously [IV]) or azacitidine (75 mg/m2, days 1-7, IV or subcutaneously). In the expansion, 400 or 800 mg venetoclax with either hypomethylating agent (HMA) was given. Median age was 74 years, with poor-risk cytogenetics in 49% of patients. Common adverse events (>30%) included nausea, diarrhea, constipation, febrile neutropenia, fatigue, hypokalemia, decreased appetite, and decreased white blood cell count. No tumor lysis syndrome was observed. With a median time on study of 8.9 months, 67% of patients (all doses) achieved complete remission (CR) + CR with incomplete count recovery (CRi), with a CR + CRi rate of 73% in the venetoclax 400 mg + HMA cohort. Patients with poor-risk cytogenetics and those at least 75 years old had CR + CRi rates of 60% and 65%, respectively. The median duration of CR + CRi (all patients) was 11.3 months, and median overall survival (mOS) was 17.5 months; mOS has not been reached for the 400-mg venetoclax cohort. The novel combination of venetoclax with decitabine or azacitidine was effective and well tolerated in elderly patients with AML (This trial was registered at www.clinicaltrials.gov as #NCT02203773).
Visual Abstract
Introduction
Acute myeloid leukemia (AML) commonly affects the elderly, with a median age of 67 years at diagnosis.1 Elderly patients (≥65 years) with AML often respond poorly to induction chemotherapy as a result of a higher frequency of adverse genomic features and increased resistance to treatments.2 Furthermore, because of comorbidities, compromised organ function, and poor performance status, older patients may not be candidates for conventional cytotoxic induction therapies.3-5 Lower-intensity regimens, which are standard of care for patients unfit for induction chemotherapy, consist predominately of hypomethylating agents (HMAs) azacitidine or decitabine or low-dose cytarabine. Azacitidine or decitabine monotherapy yields low response rates (10%-50%, including hematologic improvement), require 3.5 to 4.3 months to achieve best response, and are not curative, with a median overall survival (OS) of less than 1 year.6-9 Thus, there is a critical need to develop targeted therapies capable of rapidly inducing a high rate of clinical response, with better tolerability and durable responses for elderly patients with AML.
The B-cell lymphoma 2 (BCL-2) protein plays an important role in the survival and persistence of AML blasts, as it is a key regulator of the mitochondrial apoptotic pathway.10-13 BCL-2 maintains myeloblast survival by sequestering pro-apoptotic BAX, resulting in mitochondrial dependence on BCL-2. BAX is released when BCL-2 is antagonized, resulting in mitochondrial outer membrane permeabilization and cell death. Venetoclax, a potent, selective, oral inhibitor of BCL-2, has demonstrated single-agent clinical activity and a tolerable safety profile in patients with relapsed or refractory AML.14 Venetoclax in combination with azacitidine has demonstrated a synergistic effect in preclinical models of AML cells.15 Furthermore, azacitidine may reduce levels of MCL-1, an anti-apoptotic protein critical in AML pathogenesis and a possible source of resistance to venetoclax.16,17 With this rationale, we evaluated the safety and efficacy of venetoclax in combination with azacitidine or decitabine in elderly patients with treatment-naive AML ineligible for intensive chemotherapy. Preliminary safety and efficacy data from the dose-escalation portion of this study have been previously published.18 Here, we report efficacy and safety data from the combined dose-escalation and expansion phases of this study, with extended follow-up. In addition, preliminary results of key exploratory analyses, such as measurable residual disease (MRD), are described.
Materials and methods
Study design
The dose-escalation stage used a 3 + 3 design to establish the maximum-tolerated dose of venetoclax.18 Venetoclax was administered with a short ramp-up during cycle 1 from 20 mg (early cohorts of escalation stage) or 100 mg (expansion stage) to a target dose of 400, 800, or 1200 mg daily. All patients were hospitalized during venetoclax ramp-up in cycle 1 for at least 3 to 5 days, depending on the cohort, and received prophylaxis for tumor lysis syndrome at least 72 hours before dosing. On the basis of the preliminary safety and efficacy data,18 2 venetoclax dosing schedules (400 mg and 800 mg) were evaluated separately in the expansion stage, in combination with either decitabine or azacitidine.
Patients
Eligible patients had histologically confirmed AML, according to World Health Organization criteria,19 were at least 65 years old at diagnosis, and were ineligible for standard induction chemotherapy because of the presence of various comorbidities, such as age older than 75 years, cardiac disease or prior anthracycline use, secondary AML, or high probability of treatment-related mortality. Patients had not received prior therapy for AML and had an Eastern Cooperative Oncology Group (ECOG) performance status (PS) of 0 to 2, adequate renal and hepatic function, and a white blood cell (WBC) count of 25 × 109/L or less. The use of leukapheresis or hydroxyurea before treatment initiation to achieve this was permitted.
Key exclusion criteria were prior HMA treatment or chemotherapy for antecedent hematologic disorders (treatment with other agents excluding hydroxyurea for myelodysplastic syndrome or myeloproliferative neoplasm was permitted), favorable-risk cytogenetics (per 2014 National Comprehensive Cancer Network Guidelines),20 known active central nervous system involvement, and concomitant use of strong or moderate CYP3A inducers or inhibitors within 7 days before study drug administration.
Efficacy and safety assessments
Reponses were evaluated per the International Working Group criteria for AML.21 Efficacy was assessed as rate of objective response (complete remission [CR] + CR with incomplete blood count recovery [CRi] + partial remission [PR]), and OS. Morphologic leukemia-free state (MLFS) was defined as less than 5% blasts in an aspirate sample with marrow spicules and with a count of at least 200 nucleated cells. In addition to OS, the duration of response (DOR) for patients who achieved a CR or CRi was evaluated.
Exploratory objectives included analysis of molecular markers using peripheral blood and/or bone marrow (BM) specimens collected at baseline. Mutations associated with AML were detected by next-generation sequencing using the FoundationOne Heme panel (Foundation Medicine, Cambridge, MA) for patients in the dose-escalation cohort, the MyAML panel (Invivoscribe, San Diego, CA) for BM aspirate specimens of patients in the expansion cohort, and/or the TruSight Myeloid panel (Illumina, San Diego, CA) for peripheral blood. MRD was assessed in BM aspirates using a multiparameter flow cytometry (MFC) assay performed by Covance Central Laboratory Services Corporation. The assay was designed to detect abnormal cells based on the immunophenotypic expression of lineage and/or maturation markers associated with AML. The MFC assessment was performed independent of knowledge of the patients’ clinical response, and an MRD cutoff of 10−3 was used for all responders, consistent with that reported in other AML trials22-24 and European LeukemiaNet guidelines.25
Investigator-assessed adverse events (AEs) were summarized according to the National Cancer Institute Common Terminology Criteria for Adverse Events Version 4.0. In the absence of residual morphologic leukemia and in the presence of ongoing cytopenias at the completion of cycle 1, venetoclax could be interrupted for up to 14 days to allow for count recovery. For management of myelosuppression, if a patient achieved CRi or had an MLFS after completion of cycle 1, venetoclax was interrupted, and the subsequent cycle of HMA was delayed to allow for absolute neutrophil count recovery from day 29 until absolute neutrophil count reached at least 500/µL or up to 14 days. Recurrent events of neutropenia were addressed with reduction in venetoclax to 21 days for subsequent cycles, and/or azacitidine dose reduction per label.
All patients were able to receive supportive care measures, including transfusions, antimicrobial agents (excluding CYP3A4 inhibitor antifungal agents), and growth factor support administered per institutional standards. This study was approved by local institutional review boards, and all patients provided written informed consent. The study was designed according to Good Clinical Practice Guidelines and the Declaration of Helsinki.
Statistical analysis
The number of patients required for the 3 + 3 dose-escalation phase was dependent on the toxicities observed as the trial progressed,18 with 45 patients enrolled. The expansion stage consisted of 100 additional patients, with 25 patients in each dose level of 400 and 800 mg venetoclax, treated with each HMA combination. Safety and efficacy analyses were performed per protocol on all patients who received at least 1 venetoclax dose. Demographics were analyzed by descriptive statistics. Duration of CR + CRi and OS were analyzed using Kaplan-Meier methodology. All statistical analyses were performed using SAS (Cary, NC), version 9.3 or higher.
To determine baseline prognostic factors that may influence clinical outcomes, we performed univariate and multivariate logistic regression for CR + CRi rate, using the following covariates: age (<75, ≥75 years), ECOG PS (0, 1, 2), type of AML (primary, secondary), cytogenetic risk (intermediate, poor, or unknown), type of regimen (azacitidine or decitabine), mutation status (IDH1/2 [yes, no], FLT3 [yes, no], NPM1 [yes, no], and TP53 [yes, no]). Stepwise selection for covariates was performed for the multivariate analysis. A 2-sided P < .05 was considered statistically significant.
Data sharing statement
This clinical trial data can be requested by any qualified researchers who engage in rigorous, independent scientific research, and will be provided after review and approval of a research proposal and Statistical Analysis Plan and execution of a Data Sharing Agreement. Data requests can be submitted at any time, and the data will be accessible for 12 months, with possible extensions considered. For more information on the process, or to submit a request, visit the following link: https://www.abbvie.com/our-science/clinical-trials/clinical-trials-data-and-information-sharing/data-and-information-sharing-with-qualified-researchers.html.
Results
Patient characteristics
The data cutoff date for this analysis was July 7, 2017. Sixty patients received venetoclax 400 mg (29 with azacitidine, 31 with decitabine), 74 received venetoclax 800 mg (37 each azacitidine or decitabine), and 11 received venetoclax 1200 mg (6 azacitidine, 5 decitabine). Among all treated patients (N = 145), the median age was 74 years (range, 65-86 years), and the majority of patients (62%) had an ECOG PS of 1. Fifty-one percent had intermediate-risk cytogenetics, and 49% had poor-risk cytogenetics; 36 (25%) had secondary AML. Baseline FLT3, IDH1/2, NPM1, and TP53 mutations were performed by central laboratories (Table 1).
Table 1.
Patient demographics and baseline characteristics
| Characteristic | Dose-escalation phase | Dose-expansion phase | Dose-escalation + expansion phase | ||
|---|---|---|---|---|---|
| Arm A,VEN + DEC (n = 23) | Arm B,VEN + AZA (n = 22) | Arm D,VEN + DEC (n = 50) | Arm E, VEN + AZA (n = 50) | Total (N = 145)* | |
| Median age (range), y | 74 (68–85) | 75 (65–82) | 73 (65–86) | 74 (65–86) | 74 (65–86) |
| Age >75 y, n (%) | 10 (44) | 9 (41) | 17 (34) | 16 (32) | 52 (36) |
| Sex, n (%) | |||||
| Male | 9 (39) | 11 (50) | 30 (21) | 31 (62) | 81 (64) |
| Female | 14 (61) | 11 (50) | 20 (40) | 19 (38) | 64 (44) |
| ECOG PS, n (%) | |||||
| 0 | 2 (9) | 4 (18) | 12 (24) | 14 (28) | 32 (22) |
| 1 | 17 (74) | 14 (64) | 30 (60) | 29 (58) | 90 (62) |
| 2 | 4 (17) | 4 (18) | 8 (16) | 7 (14) | 23 (16) |
| Cytogenetics, n (%)† | |||||
| Intermediate risk | 15 (65) | 12 (55) | 26 (52) | 21 (42) | 74 (51) |
| Poor risk | 8 (35) | 10 (45) | 24 (48) | 29 (58) | 71 (49) |
| De novo AML, n (%) | 20 (87) | 16 (73) | 39 (76) | 35 (70) | 109 (75) |
| Secondary AML, n (%) | 3 (13) | 6 (27) | 12 (24) | 15 (30) | 36 (25) |
| Mutation, n (%)‡ | |||||
| FLT3§ | 6 (26) | 1 (5) | 6 (12) | 5 (10) | 18 (12) |
| IDH1 or 2‖ | 8 (35) | 7 (32) | 9 (18) | 11 (22) | 35 (24) |
| NPM1 | 9 (39) | 2 (9) | 6 (12) | 6 (12) | 23 (16) |
| TP53 | 3 (13) | 3 (14) | 13 (26) | 17 (34) | 36 (25) |
| Antecedent hematologic disorder, n (%) | 2 (9) | 3 (14) | 9 (18) | 12 (24) | 26 (18) |
| Baseline BM blast count, n (%) | |||||
| <30% | 5 (22) | 6 (27) | 10 (20) | 14 (28) | 35 (24) |
| ≥30% to <50% | 7 (30) | 9 (41) | 22 (44) | 17 (34) | 55 (38) |
| ≥50% | 11 (48) | 7 (32) | 18 (36) | 19 (38) | 55 (38) |
| Hydroxyurea before study initiation, n (%) | 6 (26) | 2 (9) | 4 (8) | 5 (10) | 17 (12) |
| Median time on study (range), months¶ | 7.0 (0.26-31.7) | 5.4 (0.9-30.0) | 11.8 (0.2-16.5) | 9.3 (0.5-16.2) | 8.9 (0.2-31.7) |
Includes 11 patients treated with VEN 1200 mg.
NCCN risk categorization: NCCN Guidelines. Acute myeloid leukemia. Version 2.2014.15
Central laboratory. FLT3, IDH1/2, and TP53 mutational testing results were evaluable for 141/145 patients, with no data available for 1 patient from arm B and 3 patients from arm D.
FLT3-ITD mutations were identified in 10 patients, and FLT3-TKD in 6 patients; 1 patient had both FLT3-ITD and TKD, 1 patient had atypical TKD mutation at S451, and 1 patient had an amplification of FLT3.
IDH1R132 mutations were identified in 15 patients, IDH2R140 in 13 patients, IDH2R172 in 6 patients, and 1 patient in a nonhotspot mutation in IDH2K282.
The median time on study was calculated from the time of first dose of study drug to either the cutoff date (for active patients) or the date a patient discontinued the study.
Safety
Hematological and gastrointestinal AEs were the most common toxicities observed (Table 2). Gastrointestinal AEs were primarily grade 1/2, and no patients discontinued venetoclax because of these AEs. Common grade 3/4 AEs included febrile neutropenia (43%), decreased WBC count (31%), anemia (25%), thrombocytopenia (24%), neutropenia (17%), and pneumonia (13%).
Table 2.
Treatment-emergent adverse events of any grade occurring in more than 25% of patients
| Adverse event (N = 145) | Venetoclax 400 mg (n = 60) | Venetoclax 800 mg (n = 74) | Venetoclax 1200 mg (n = 11) | Total (N = 145) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| DEC (n = 31) | AZA (n = 29) | DEC (n = 37) | AZA (n = 37) | DEC (n = 5) | AZA (n = 6) | |||||||||
| Any grade | Gr3/4 | Any grade | Gr3/4 | Any grade | Gr3/4 | Any grade | Gr3/4 | Any grade | Gr3/4 | Any grade | Gr3/4 | Any grade | Gr3/4 | |
| Any event, n (%) | 31 (100) | 24 (77) | 29 (100) | 25 (86) | 37 (100) | 34 (92) | 37 (100) | 30 (81) | 5 (100) | 4 (80) | 6 (100) | 5 (83) | 145 (100) | 122 (84) |
| Nausea | 17 (55) | 0 | 18 (62) | 1 (3) | 23 (62) | 1 (3) | 23 (62) | 0 | 4 (80) | 0 | 3 (50) | 0 | 88 (61) | 2 (1) |
| Diarrhea | 13 (42) | 2 (6) | 15 (52) | 1 (3) | 22 (60) | 2 (5) | 18 (49) | 2 (5) | 4 (80) | 0 | 4 (67) | 0 | 76 (52) | 7 (5) |
| Constipation | 14 (45) | 0 | 17 (59) | 2 (7) | 15 (41) | 0 | 18 (49) | 0 | 2 (40) | 0 | 4 (67) | 0 | 70 (48) | 2 (1) |
| Febrile neutropenia | 19 (61) | 19 (61) | 11 (38) | 11 (38) | 15 (41) | 15 (41) | 13 (35) | 13 (35) | 2 (40) | 2 (40) | 3 (50) | 3 (50) | 63 (43) | 63 (43) |
| Fatigue | 12 (39) | 3 (10) | 10 (34) | 0 | 13 (35) | 3 (8) | 13 (35) | 1 (3) | 4 (80) | 1 (20) | 2 (33) | 0 | 54 (37) | 8 (6) |
| Hypokalemia | 10 (32) | 4 (13) | 5 (17) | 2 (7) | 17 (46) | 5 (14) | 11 (30) | 3 (8) | 3 (60) | 1 (20) | 3 (50) | 0 | 49 (34) | 15 (10) |
| Decreased appetite | 8 (26) | 0 | 8 (28) | 1 (3) | 13 (35) | 1 (3) | 14 (38) | 1 (3) | 3 (60) | 0 | 2 (33) | 0 | 48 (33) | 3 (2) |
| Decreased WBC count | 13 (42) | 13 (42) | 7 (24) | 7 (24) | 10 (27) | 10 (27) | 12 (32) | 12 (32) | 2 (40) | 2 (40) | 1 (17) | 1 (17) | 45 (31) | 45 (31) |
| Vomiting | 10 (32) | 0 | 9 (31) | 0 | 10 (27) | 0 | 10 (27) | 0 | 3 (60) | 0 | 2 (33) | 0 | 44 (30) | 0 |
| Anemia | 7 (23) | 7 (23) | 9 (31) | 9 (31) | 11 (30) | 10 (27) | 11 (30) | 9 (24) | 2 (40) | 1 (20) | 0 | 0 | 40 (28) | 36 (25) |
| Cough | 10 (32) | 0 | 6 (21) | 0 | 11 (30) | 0 | 10 (27) | 0 | 2 (40) | 0 | 2 (33) | 0 | 41 (28) | 0 |
| Peripheral edema | 7 (23) | 0 | 10 (34) | 0 | 12 (32) | 0 | 10 (27) | 0 | 1 (20) | 0 | 1 (17) | 0 | 41 (28) | 0 |
Because patients with baseline cytopenias were included in the safety analysis, occurrence of many of the hematological AEs began before study drug initiation and were attributed to underlying hematologic disease. At baseline, of 145 patients, 103 (71%) had grade 3/4 neutropenia, 78 (54%) had grade 3/4 thrombocytopenia, and 40 (28%) had grade 3/4 anemia. No dose-limiting toxicities were observed, and no events of laboratory or clinical tumor lysis syndrome were reported. To mitigate any potential tumor lysis syndrome, patients were required to have a WBC count of at least 25 × 109/L at study initiation, with the use of hydroxyurea allowed to meet this criterion, and all patients required hospitalization, hydration, and treatment with a uric acid-reducing agent before and during the first few days of treatment.
Infections of all grades were reported in 74% of patients (45% grade 3/4), with pneumonia (18%) being most common. Grade 3/4 infections occurring in at least 3% of patients included pneumonia (13%), bacteremia and sepsis (10%), lung infection (6%), cellulitis, fungal pneumonia, and urinary tract infection (3% each). Grade 3/4 fungal infections were reported in 8% of patients; grade 5 infections included 1 case each of bacteremia, lung infection, fungal pneumonia, septic shock, necrotizing pneumonia, and Pseudomonas sepsis, and 2 cases each of pneumonia and sepsis, resulting in 10 (7%) deaths caused by infection.
The venetoclax 1200-mg cohort experienced a trend toward a higher frequency of hematological and gastrointestinal AEs compared with the 400-mg and 800-mg cohorts (not statistically significant, all P > .05; supplemental Table 1, available on the Blood Web site), which limited the ability for continuous therapy and led to a venetoclax dose reduction to 800 mg in 5 of 12 patients. The frequency of AEs was generally similar between the azacitidine and decitabine cohorts at given doses of venetoclax, although the incidence of hypokalemia, decreased WBC count, and cough were lower in the 400-mg venetoclax + azacitidine group vs other cohorts (Table 2). Serious AEs occurred in 70% of patients at all doses. Serious AEs occurring in at least 3% of patients were febrile neutropenia (32%), pneumonia (12%), bacteremia and sepsis (10%), lung infection (5%), and hypotension, diarrhea, fatigue, and mental status changes (3% each). Common AEs in the venetoclax 400-mg group occurring in more than 25% of patients included nausea (58%), constipation (52%), febrile neutropenia (50%), and diarrhea (47%; supplemental Table 1).
Overall, 101 patients (70%) discontinued the study, with progressive disease (PD) being the most common reason for discontinuation; 22% of patients in the venetoclax + azacitidine cohorts and 34% of patients in the venetoclax + decitabine cohorts discontinued venetoclax because of PD (supplemental Table 2). The median time on study for 41 patients who discontinued because of PD was 6.7 months (range, 0.1-14.6 months). Venetoclax was discontinued in 7 patients (5%) because of AEs that included hepatic candidiasis, respiratory tract infection, sepsis, malignant neoplasm progression, embolic stroke, and respiratory failure (n = 1 each). In total, 21 patients discontinued from study to receive stem cell transplant. Discontinuations were equally distributed between the azacitidine and decitabine cohorts.
Of the 68/145 (47%) of patients who had an AE that led to venetoclax dose interruption, 27 also had neutropenia. In addition, of the 63 patients with neutropenia, 21 had a delay of cycle 2 treatment to allow for absolute neutrophil count recovery. Notably, these 21 patients each achieved a CRi before the cycle 2 delay, and all but 1 remained in either CR/CRi or MLFS at the time of the data cutoff.
Five deaths (3%) occurred 30 days or less after the first dose of study drug; causes were sepsis (n = 2), bacteremia (n = 1), respiratory failure (n = 1), or multiorgan dysfunction (n = 1). Eleven (8%) deaths occurred at ≤60 days; causes for deaths occurring between 30 to 60 days were PD (n = 4), respiratory failure (n = 1), and sepsis (n = 1). Overall, 46 patients (32%) died during survival follow-up (>30 days after the last dose of study drug).
Efficacy
At the cutoff date of July 7, 2017, the median time on study was 8.9 months (range, 0.2-31.7 months), and the median duration of follow-up was 15.1 months (range, 9.8-31.7 months). The median number of completed venetoclax cycles was 5 (range, 1-25 cycles). In the intent-to-treat population (N = 145), the CR and CRi rates were 37% and 30%, respectively, with an overall response rate (ORR; CR + Cri + PR) of 68% (99/145) and an overall leukemia response rate (CR + Cri + PR + MLFS) of 83% (120/145). The median time to first response was 1.2 months (range, 0.8-13.5 months), and median time to best response (CR) was 2.1 months (range, 0.9-13.5 months). Of the patients who had responses of CRi, 34 of 43 achieved red cell transfusion independence while receiving therapy, as did 7 of 21 patients with MLFS. Similarly, 40 of 43 patients with CRi and 10 of 21 with MLFS achieved platelet transfusion independence from baseline. The CR + CRi rate for the venetoclax 400 mg + HMA cohort was 73% and 65% for the venetoclax 800 mg + HMA cohort (P = .35; Table 3). The ORR for the venetoclax 400 mg + HMA cohort was 73% compared with 68% in the venetoclax 800 mg + HMA cohort (P = .57). Response rates were similar between the venetoclax 400 mg + azacitidine and venetoclax 400 mg + decitabine cohorts (76% vs 71%, respectively).
Table 3.
Response rates by study cohorts (dose escalation + dose expansion)
| Cohort | N | Composite response rate (CR + CRi) [n], n (%) | Overall response rate (CR + CRi + PR) [n], n (%) | Leukemia response rate (CR + CRi + PR + MLFS) [n], n (%) | Median duration of CR + CRi (95% CI) | Median OS (95% CI) |
|---|---|---|---|---|---|---|
| All patients | 145 | [54 + 43], 97 (67) | [54 + 43 + 2], 99 (68) | [54 + 43 + 2 + 21], 120 (83) | 11.3 (8.9-NR) | 17.5 (12.3-NR) |
| VEN 400 mg + HMA | 60 | 44 (73) | 44 (73) | 49 (82) | 12.5 (7.8-NR) | NR (11.0-NR) |
| VEN 400 mg + AZA | 29 | 22 (76) | 22 (76) | 24 (83) | NR (5.6-NR) | NR (9.0-NR) |
| VEN 400 mg + DEC | 31 | 22 (71) | 22 (71) | 25 (81) | 12.5 (5.1-NR) | 14.2 (7.7-NR) |
| VEN 800 mg + HMA | 74 | 48 (65) | 50 (68) | 63 (85) | 11.0 (6.5-12.9) | 17.5 (10.3-NR) |
| VEN 800 mg + AZA | 37 | 21 (57) | 22 (59) | 31 (84) | 11.7 (4.6-12.9) | 15.2 (9.1-NR) |
| VEN 800 mg + DEC | 37 | 27 (73) | 28 (76) | 32 (86) | 9.2 (5.9-NR) | 17.5 (10.3-NR) |
| VEN 1200 mg + HMA | 11 | 5 (45) | 5 (45) | 8 (73) | 9.4 (4.1-NR) | 11.4 (0.9-NR) |
| VEN 1200 mg + AZA | 6 | 2 (33) | 2 (33) | 4 (67) | 6.7 (4.1-9.4) | 8.8 (0.9-NR) |
| VEN 1200 mg + DEC | 5 | 3 (60) | 3 (60) | 4 (80) | NR (NR-NR) | NR (12.4-NR) |
Patients undergoing SCT (n = 21) were not censored from CR/CRi and OS analyses.
The median duration of CR + CRi (n = 97) for all patients was 11.3 months (95% CI, 8.9 months-not reached [NR]), with 45% of responders maintaining a response of more than 12 months (Figure 1). Patients with a best response of CR had a median DOR of 12.5 months (95% CI, 11 months-NR), and patients with a best response of CRi had a median DOR of 6.8 months (95% CI, 4.1 months-NR). The median duration of CR + CRi for the venetoclax 400 mg + HMA cohort was 12.5 months (95% CI, 7.8 months-NR) vs 11 months (95% CI, 6.5-12.9 months) for the venetoclax 800 mg + HMA cohort. The median duration of CR + CRi was NR (95% CI, 5.6 months-NR) for venetoclax 400 mg + azacitidine and was 12.5 months (95% CI, 5.1 months-NR) for venetoclax 400 mg + decitabine (Table 3).
Figure 1.
Duration of CR + CRi by venetoclax dose levels (dose escalation + dose expansion cohorts). CR + CRi duration for all patients on study (black), the venetoclax 400 mg cohort (orange), the venetoclax 800 mg cohort (green), and the venetoclax 1200 mg cohort (blue). VEN, venetoclax.
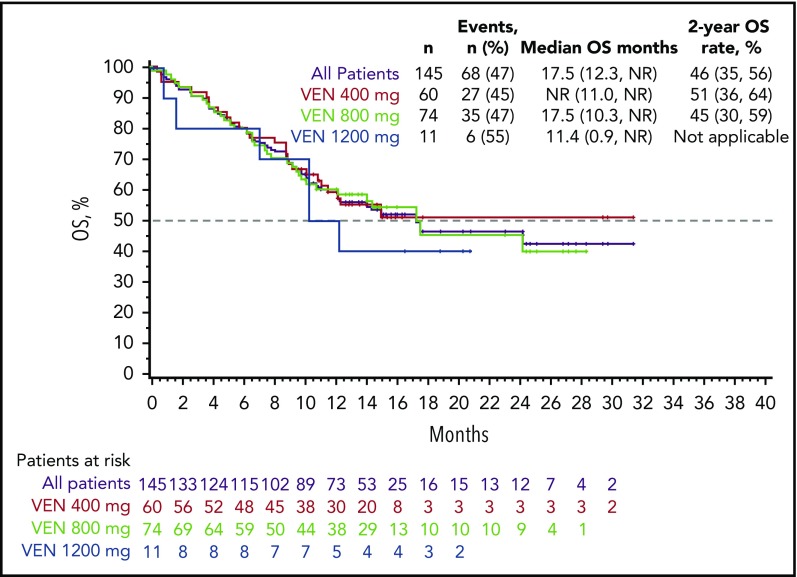
At a median follow-up of 15.1 months, the median OS for all patients was 17.5 months (95% CI, 12.3 months-NR; Figure 2). The estimated 6-month, 1-year, and 2-year OS rates for all patients were 80%, 59%, and 46%, respectively. The median OS for venetoclax 400 mg + HMA and 800 mg + HMA cohorts was NR (95% CI, 11 months-NR) and 17.5 months (95% CI, 10.3 months-NR), respectively. The median OS for venetoclax 400 mg with azacitidine was NR (95% CI, 9.0 months-NR), and for decitabine it was was 14.2 months (95% CI, 7.7 months-NR; Table 3). Median OS for venetoclax 800 mg with azacitidine was 15.2 months (95% CI, 9.1 months-NR), and it was 17.5 months with decitabine (95% CI, 10.3 months-NR; Table 3). The CR + CRi rate was 76% (16/21) for the 21 patients who received SCT poststudy, with a median duration of CR + CRi of 9.2 months (95% CI, 7.8-9.2 months), and a median OS of 24.4 months.
Figure 2.
OS by venetoclax dose levels (dose escalation + dose expansion cohorts). OS for all study patients (black), the venetoclax 400-mg cohort (orange), the venetoclax 800-mg cohort (green), and the venetoclax 1200-mg cohort (blue).
On-therapy MRD data were evaluable for 83 (86%) of the 97 patients achieving a CR/CRi and 15 (71%) of the 21 patients achieving MLFS; missing data are the result of either no samples collected (3 with CR/CRi, 1 with MLFS) or a technical assay failure (11 with CR/CRi, 5 with MLFS). Among the patients with CR/CRi, 29% (28/97) had at least 1 assessment with an MRD of less than 10−3; 17 were in the azacitidine group, and 11 were in the decitabine group (17 at 400 mg, 10 at 800 mg, and 1 at 1200 mg venetoclax; Table 4; supplemental Figure 1). In addition, 1 patient with MLFS also achieved an MRD of less than 10−3 at least at 1 assessment (1200 mg). Among the 28 patients with CR/CRi achieving MRD less than 10−3, the median DOR and OS have not been reached; the median OS has also not been reached for the 55 patients with CR/CRi achieving MRD greater than 10−3 with a median DOR of 11.3 months.
Table 4.
MRD assessments for CR/CRi patients
| CR/CRi, n = 97 | MRD < 10−3 | MRD ≥ 10−3 | Nonevaluable |
|---|---|---|---|
| n (%) | 28 (29) | 55 (57) | 14 (14) |
| DOR, mo | NR | 11.3 | 6.4 |
| OS, mo | NR | NR | 10.6 |
MRD assessments any time on therapy: after the initial dose, but before discontinuation of therapy (+7 days) or progressive disease, whichever came first.
Subgroup efficacy analysis
Cytogenetic findings provided by investigators were used to establish National Comprehensive Cancer Network risk categories. Efficacy outcomes by subgroups are shown in Table 5. The CR + CRi rates in patients with poor- and intermediate-risk cytogenetics were 60% and 74%, with a median duration of CR + CRi of 6.7 months (95% CI, 4.1-9.4 months) vs 12.9 months (95% CI, 11.0 months-NR), and median OS of 9.6 months (95% CI, 7.2-12.4 months) vs NR (95% CI, 17.5-NR), respectively (Table 5; supplemental Figures 2 and 3). Responses were observed in patients carrying the TP53 mutation, with CR + CRi rates of 47%, median duration of CR + CRi of 5.6 months (95% CI, 1.2-9.4 months), and median OS of 7.2 months (95% CI, 3.7 months-NR). Among the baseline prognostic factors tested in a post hoc exploratory analysis, TP53 status was found to be a statistically significant predictor for CR + CRi using univariate (P = .005), but not by the multivariate logistics regression models (P = .052; supplemental Table 3), with patients harboring the mutations achieving lower rates of CR/CRi. Notably, patients harboring the FLT3 mutation (10 ITD, 5 TKD, 1 ITD + TKD, 2 others) exhibited CR + CRi rates of 72%, median duration of CR + CRi of 11 months (95% CI, 6.5 months-NR), and median OS was NR (95% CI, 8.0 months-NR), demonstrating that the presence of FLT3 mutation was not a statistically significant predictor of outcome (P = .731). Patients with IDH1/2 mutations had a CR + CRi rate of 71%, median duration of CR + CRi of NR (95% CI, 6.8 months-NR), and median OS of 24.4 months (95% CI, 12.3 months-NR), which also was not a statistically significant predictor of outcomes (P = .802). Patients with NPM1 mutations showed a CR + CRi rate of 91.5%, median duration of CR + CRi of NR (95% CI, 6.8 months-NR), and median OS of NR (95% CI, 11.0 months-NR); NPM1 mutation status was a statistically significant predictor of favorable outcome in both the univariate (P = .015) and multivariate (P = .049) analyses.
Table 5.
Efficacy outcomes by subgroups
| Subgroup | Evaluable for response/OS, n (%) | CR + CRi, n (%) | n for Median duration of CR + CRi | Median duration of CR + CRi, mo (95%CI) | Median OS, mo (95%CI) |
|---|---|---|---|---|---|
| All patients | 145 | 97 (67) | 97 | 11.3 (8.9, NR) | 17.5 (12.3-NR) |
| Cytogenetic risk | |||||
| Intermediate | 74 (51) | 55 (74) | 55 | 12.9 (11, NR) | NR (17.5-NR) |
| Poor | 71 (49) | 42 (60) | 42 | 6.7 (4.1, 9.4) | 9.6 (7.2-12.4) |
| Age | |||||
| ≥75 y | 62 (43) | 40 (65) | 40 | 9.2 (6.4, 12.5) | 11 (9.3-NR) |
| <75 y | 83 (57) | 57 (69) | 57 | 12.9 (9.2, NR) | 17.7 (14.2-NR) |
| AML | |||||
| De novo | 109 (75) | 73 (67) | 73 | 9.4 (7.2, 11.7) | 12.5 (10.3-24.4) |
| Secondary | 36 (25) | 24 (67) | 24 | NR (12.5, NR) | NR (14.6-NR) |
| Mutations* | |||||
| FLT3† | 18 (12) | 13 (72) | 13 | 11 (6.5, NR) | NR (8-NR) |
| IDH1 or 2‡ | 35 (24) | 25 (71) | 25 | NR (6.8, NR) | 24.4 (12.3-NR) |
| NPM1 | 23 (16) | 21 (91) | 21 | NR (6.8, NR) | NR (11-NR) |
| TP53 | 36 (25) | 17 (47) | 17 | 5.6 (1.2, 9.4) | 7.2 (3.7-NR) |
ITD, internal tandem duplication; TKD, tyrosine kinase domain.
Determined by central laboratory in 141/145 of patients.
FLT3-ITD mutations were identified in 10 patients, FLT3-TKD in 6 patients; 1 patient had both FLT3-ITD and TKD, 1 patient had atypical TKD mutation at S451, and 1 patient had an amplification of FLT3.
IDH1R132 mutations were identified in 15 patients, IDH2R140 in 13 patients, IDH2R172 in 6 patients, and 1 patient in a nonhotspot mutation in IDH2K282.
Among other prognostic factors studied, patients with de novo AML had the same CR + CRi rates as patients with secondary AML (both 67%), with median duration of CR + CRi of 9.4 months (95% CI, 7.2-11.7 months) vs NR (95% CI, 12.5 months-NR) and median OS of 12.5 months (95% CI, 10.3-24.4 months) vs NR (95% CI, 14.6 months-NR) for de novo vs secondary AML, respectively; Table 5).
Discussion
Venetoclax in combination with azacitidine or decitabine was well tolerated, with similar safety profiles within all arms of the dose escalation and expansion phases in elderly patients with previously untreated AML ineligible for standard induction therapy. Similar frequencies of AEs were observed in the decitabine and azacitidine groups, with the lowest incidences of gastrointestinal symptoms, such as nausea, diarrhea, and decreased appetite, seen in the 400-mg venetoclax + azacitidine cohort. Common grade 3/4 AEs were mostly hematologic and similar to those reported with single-agent azacitidine or decitabine in phase 3 studies.6,8 On confirmation of morphologic clearance of leukemia, grade 4 neutropenia was managed with delay in treatment cycle. Recurrent grade 3/4 neutropenia in subsequent cycles was managed with venetoclax dose interruptions, reduction in duration, delay in treatment cycles, and intermittent growth factor use per institutional standards. The low frequency of fungal infections (8% grade 3/4), despite exclusion of CYP3A inhibitor azole antifungals, can be attributed to the prophylactic use of alternative antifungals such as echinocandins in 46% of patients and/or the relatively low rate of invasive fungal infection found in patients given HMA-based therapies (4.1%).7-9,26 Notably, early mortality was low, with 5 (3%) deaths occurring within 30 days after initiation of study drug, which may indicate the clinical importance of obtaining an early remission.
This study demonstrated a high CR + CRi rate of 67% (ORR, 68%) and a tolerable safety profile for venetoclax in combination with azacitidine or decitabine. Notably, the venetoclax 400 mg + HMA cohort achieved a CR + CRi rate of 73%, a median duration of CR + CRi of 12.5 months, and median OS not reached. These results warrant further evaluation of 400-mg venetoclax + HMA in a larger population.
The response rates for low-intensity therapy such as decitabine and azacitidine in patients with AML who were at least 65 years old are 10% to 50%,6,8,9,27 corresponding to a median OS of 6 to 12 months.28,29 The CR + CRi rate of 67% and the median OS of 17.5 months achieved with the venetoclax combinations compare favorably with HMA monotherapy, although it is important to note the limited number of patients examined in this study. In addition, the rapid attainment of best response of CR + CRi at median of 1.8 months with venetoclax + HMA combinations is notable compared with 4.3 months with decitabine8 or 3.5 months with azacitidine alone.9
Venetoclax plus decitabine or azacitidine was effective in high-risk subgroups tested, including age 75 years or older, poor cytogenetic risk, and secondary AML. Although these observations are drawn from a relatively small subset of patients, the remission rates achieved by our low-intensity regimen are encouraging in light of the traditionally lower remission rates in the elderly AML population (40%-50%) compared with young patients receiving chemotherapy (60%-70%)30 and the relatively short duration of these remissions.31
The biomarker analyses performed in our study demonstrate that venetoclax in combination with decitabine or azacitidine was effective in most subgroups, including in patients harboring high-risk molecular features. Mutations such as TP5332 and FLT3-ITD33,34 have been associated with poor prognosis in patients with AML. Although those with poor-risk cytogenetics and TP53 mutations did fare less well than other groups in this study, meaningful responses were achieved. Patients with TP53 mutations achieved a CR/CRi rate of 47%, which may suggest improvement over historical controls that report CR rates as low as 28%, although DOR was short, consistent with what has been reported elsewhere.35,36 In addition, the FLT3 mutations were not prognostic of poor outcomes in this study in either the multivariate or univariate analyses. Study patients with NPM1 mutations appeared to have an especially good outcome with venetoclax-based therapy. IDH1/2 mutations have been shown to have a favorable prognosis in some studies,14,37 whereas the prognosis was neutral, unfavorable, or dependent on the type of IDH mutation in other studies.38 Patients in this study with IDH1/2 had a median survival of 24.4 months, which may suggest increased sensitivity of venetoclax in IDH-mutated patients, as reported previously.14
MFC is a sensitive technique that can detect low levels of disease burden that remain after therapy. The data obtained by MFC demonstrate deep responses, with 28/97 (29%) of patients with CR/CRi achieving residual disease below the level of 10−3 at least once during study treatment. These preliminary MRD data are encouraging and require further analysis in a larger patient population to understand the relationship between achieving low levels of disease burden and the durability of response. In addition, the optimal timing of MRD assessments and its relationship to ORR and OS should be evaluated.
In summary, the low-intensity regimen of venetoclax combined with decitabine or azacitidine demonstrated promising efficacy and a tolerable safety profile in elderly patients with AML unfit for intensive chemotherapy, with a high CR + CRi rate of 73% in the 400-mg venetoclax + HMA cohort, low early mortality rates, and OS extending beyond 17 months. Responses were observed in patients with high-risk molecular features and adverse prognostic factors. A phase 3 study of venetoclax 400 mg combined with azacitidine in adults with untreated AML ineligible for induction therapy is currently underway (NCT02993523).
Supplementary Material
The online version of this article contains a data supplement.
Acknowledgments
The authors thank the patients and their families, study coordinators, and support staff.
A.L. was supported by P01 grant 5P01CA066996-20 from the National Institutes of Health, National Cancer Institute.
Venetoclax is being developed in a collaboration between AbbVie and Genentech. AbbVie and Genentech provided financial support for this study and participated in the design, study conduct, analysis, and interpretation of data, as well as the writing, review, and approval of this presentation. Medical writing support was provided by Swati Ghatpande, and Devon Roll of BioConnections LLC, which was funded by AbbVie.
Footnotes
Presented in part at the 59th annual meeting of the American Society of Hematology, Atlanta, GA, 10 December 2017, and the annual meeting of the European Hematology Association, Stockholm, Sweden, 17 June 2018.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Authorship
Contribution: C.D.D., K.P., V.P., B.A.J., M.A., P.S.B., O.F., M.K., A.H.W., H.M.K., J.P., D.A.P., and A.L. provided study materials or patients; C.D.D., K.P., V.P., B.A.J., M.A., P.S.B., O.F., M.K., A.H.W., H.M.K., T.X., W.-J.H., B.C., J.P., D.A.P., and A.L. provided collection and assembly of data; all authors provided data analysis and interpretation; all authors provided manuscript writing; and all authors provided final approval of manuscript.
Conflict-of-interest disclosure: C.D.D. received research funding from AbbVie/Genentech, Agios, Celgene, Daiichi Sankyo, Millennium, and Novartis and served as consultant for Agios, and an advisory board member for AbbVie, Agios, Bayer, Celgene, Karyopharm, and Medimmune; K.P. received research funding from AbbVie, Agios, Daiichi Sankyo, and Millennium and is an advisory board member for AbbVie, Astellas, and Boston BioMedical; B.A.J. served as consultant for AbbVie, Amgen, and Tolero and as an advisory board member for Celgene and received research funding to his institution from AbbVie, Incyte, Forma, Celgene, Daiichi Sankyo, Pharmacyclics, Genentech/Roche, Glycomimetics, AROG, Accelerated Medical Diagnostics, LP Therapeutics, Esanex, and Kalobios; M.A. received research funding from Cephalon Oncology; P.S.B. received research funding from AbbVie, Bristol-Myers Squibb, Glycomimetics, JW Pharmaceutical, Amgen, Novartis, Trovagene, Trethera, and Aptose and served as an advisory board member for Pfizer and CVS Caremark; O.F. served on an advisory board and speakers’ bureau for Celgene, Aggios, and Jazz and as n advisory board member for AbbVie; M.K. served as a consultant for AbbVie, Genentech, and F. Hoffman La-Roche and as an advisory board member for F. Hoffman La-Roche and holds shares from Reata Pharmaceuticals and received honoraria from Amgen, Abbvie, and Genentech and research funding from AbbVie, Genentech, Eli Lilly, Cellectis, Calithera, Stemline, Threshold, Flexus Biosciences, Novartis, Ablynx, and Agios; A.H.W. served in an advisory role for AbbVie, Celgene, Novartis, Amgen, and Servier and received research funding from AbbVie, Celgene, and Servier and honoraria from AbbVie, Celgene, Novartis, Amgen, and Servier; H.M.K. received honoraria from AbbVie, Actinium, Agios, Amgen, Immunogen, Orsinex, Pfizer, and Takeda and research grants from AbbVie, Agios, Amgen, Ariad, Astex, Bristol-Myers Squibb, Cyclacel, Immunogen, Jazz, and Pfizer; T.X. is an employee of AbbVie and may hold stock or stock options; W.-J.H. is an employee of Genentech and may hold stock or stock options; B.C. is an employee of AbbVie and may hold stock or stock options; J.P. is an employee of AbbVie and may hold stock or stock options; D.A.P. serves on the data safety monitoring board for GlycoMimetics and as an advisory board member for Pfizer, Jazz, Takeda, Curis, Argenx, Agios, Servier, Celgene, and AbbVie and received research funding from AbbVie, Celgene, and Pfizer; and A.L. serves as a consultant for and receives research funding from AbbVie, TetraLogic, AstraZeneca, and Novartis and is a cofounder of Flash Therapeutics and Vivid Bioscience. V.P. declares no competing financial interests.
Correspondence: Anthony Letai, Department of Medical Oncology, Dana-Farber Cancer Institute, 450 Brookline Ave, M430, Boston, MA 02215; e-mail: anthony_letai@dfci.harvard.edu.
REFERENCES
- 1.Almeida AM, Ramos F. Acute myeloid leukemia in the older adults. Leuk Res Rep. 2016;6:1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Krug U, Büchner T, Berdel WE, Müller-Tidow C. The treatment of elderly patients with acute myeloid leukemia. Dtsch Arztebl Int. 2011;108(51-52):863-870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pettit K, Odenike O. Defining and treating older adults with acute myeloid leukemia who are ineligible for intensive therapies. Front Oncol. 2015;5:280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kantarjian H, Ravandi F, O’Brien S, et al. Intensive chemotherapy does not benefit most older patients (age 70 years or older) with acute myeloid leukemia. Blood. 2010;116(22):4422-4429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kantarjian H, O’brien S, Cortes J, et al. Results of intensive chemotherapy in 998 patients age 65 years or older with acute myeloid leukemia or high-risk myelodysplastic syndrome: predictive prognostic models for outcome. Cancer. 2006;106(5):1090-1098. [DOI] [PubMed] [Google Scholar]
- 6.Dombret H, Seymour JF, Butrym A, et al. International phase 3 study of azacitidine vs conventional care regimens in older patients with newly diagnosed AML with >30% blasts. Blood. 2015;126(3):291-299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cashen AF, Schiller GJ, O’Donnell MR, DiPersio JF. Multicenter, phase II study of decitabine for the first-line treatment of older patients with acute myeloid leukemia. J Clin Oncol. 2010;28(4):556-561. [DOI] [PubMed] [Google Scholar]
- 8.Kantarjian HM, Thomas XG, Dmoszynska A, et al. Multicenter, randomized, open-label, phase III trial of decitabine versus patient choice, with physician advice, of either supportive care or low-dose cytarabine for the treatment of older patients with newly diagnosed acute myeloid leukemia. J Clin Oncol. 2012;30(21):2670-2677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Al-Ali HK, Jaekel N, Junghanss C, et al. Azacitidine in patients with acute myeloid leukemia medically unfit for or resistant to chemotherapy: a multicenter phase I/II study. Leuk Lymphoma. 2012;53(1):110-117. [DOI] [PubMed] [Google Scholar]
- 10.Pan R, Hogdal LJ, Benito JM, et al. Selective BCL-2 inhibition by ABT-199 causes on-target cell death in acute myeloid leukemia. Cancer Discov. 2014;4(3):362-375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vo TT, Ryan J, Carrasco R, et al. Relative mitochondrial priming of myeloblasts and normal HSCs determines chemotherapeutic success in AML. Cell. 2012;151(2):344-355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Konopleva M, Contractor R, Tsao T, et al. Mechanisms of apoptosis sensitivity and resistance to the BH3 mimetic ABT-737 in acute myeloid leukemia. Cancer Cell. 2006;10(5):375-388. [DOI] [PubMed] [Google Scholar]
- 13.Konopleva M, Letai A. BCL-2 inhibition in AML: an unexpected bonus? Blood. 2018;132(10):1007-1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Konopleva M, Pollyea DA, Potluri J, et al. Efficacy and biological correlates of response in a phase II study of venetoclax monotherapy in patients with acute myelogenous leukemia. Cancer Discov. 2016;6(10):1106-1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bogenberger JM, Delman D, Hansen N, et al. Ex vivo activity of BCL-2 family inhibitors ABT-199 and ABT-737 combined with 5-azacytidine in myeloid malignancies. Leuk Lymphoma. 2015;56(1):226-229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tsao T, Shi Y, Kornblau S, et al. Concomitant inhibition of DNA methyltransferase and BCL-2 protein function synergistically induce mitochondrial apoptosis in acute myelogenous leukemia cells. Ann Hematol. 2012;91(12):1861-1870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bose P, Gandhi V, Konopleva M. Pathways and mechanisms of venetoclax resistance. Leuk Lymphoma. 2017;58(9):1-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.DiNardo CD, Pratz KW, Letai A, et al. Safety and preliminary efficacy of venetoclax with decitabine or azacitidine in elderly patients with previously untreated acute myeloid leukaemia: a non-randomised, open-label, phase 1b study. Lancet Oncol. 2018;19(2):216-228. [DOI] [PubMed] [Google Scholar]
- 19.Vardiman JW, Thiele J, Arber DA, et al. The 2008 revision of the World Health Organization (WHO) classification of myeloid neoplasms and acute leukemia: rationale and important changes. Blood. 2009;114(5):937-951. [DOI] [PubMed] [Google Scholar]
- 20.Creutzig U, Kaspers GJ. Revised recommendations of the International Working Group for diagnosis, standardization of response criteria, treatment outcomes, and reporting standards for therapeutic trials in acute myeloid leukemia. J Clin Oncol. 2004;22(16):3432-3433. [DOI] [PubMed] [Google Scholar]
- 21.Cheson BD, Bennett JM, Kopecky KJ, et al. ; International Working Group for Diagnosis, Standardization of Response Criteria, Treatment Outcomes, and Reporting Standards for Therapeutic Trials in Acute Myeloid Leukemia. Revised recommendations of the International Working Group for Diagnosis, Standardization of Response Criteria, Treatment Outcomes, and Reporting Standards for Therapeutic Trials in Acute Myeloid Leukemia. J Clin Oncol. 2003;21(24):4642-4649. [DOI] [PubMed] [Google Scholar]
- 22.Feller N, van der Pol MA, van Stijn A, et al. MRD parameters using immunophenotypic detection methods are highly reliable in predicting survival in acute myeloid leukaemia. Leukemia. 2004;18(8):1380-1390. [DOI] [PubMed] [Google Scholar]
- 23.Inaba H, Coustan-Smith E, Cao X, et al. Comparative analysis of different approaches to measure treatment response in acute myeloid leukemia. J Clin Oncol. 2012;30(29):3625-3632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Freeman SD, Virgo P, Couzens S, et al. Prognostic relevance of treatment response measured by flow cytometric residual disease detection in older patients with acute myeloid leukemia. J Clin Oncol. 2013;31(32):4123-4131. [DOI] [PubMed] [Google Scholar]
- 25.Schuurhuis GJ, Heuser M, Freeman S, et al. Minimal/measurable residual disease in AML: a consensus document from the European LeukemiaNet MRD Working Party. Blood. 2018;131(12):1275-1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pomares H, Arnan M, Sánchez-Ortega I, Sureda A, Duarte RF. Invasive fungal infections in AML/MDS patients treated with azacitidine: a risk worth considering antifungal prophylaxis? Mycoses. 2016;59(8):516-519. [DOI] [PubMed] [Google Scholar]
- 27.Derissen EJ, Beijnen JH, Schellens JH. Concise drug review: azacitidine and decitabine. Oncologist. 2013;18(5):619-624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Burnett AK, Milligan D, Prentice AG, et al. A comparison of low-dose cytarabine and hydroxyurea with or without all-trans retinoic acid for acute myeloid leukemia and high-risk myelodysplastic syndrome in patients not considered fit for intensive treatment. Cancer. 2007;109(6):1114-1124. [DOI] [PubMed] [Google Scholar]
- 29.Fenaux P, Mufti GJ, Hellström-Lindberg E, et al. Azacitidine prolongs overall survival compared with conventional care regimens in elderly patients with low bone marrow blast count acute myeloid leukemia. J Clin Oncol. 2010;28(4):562-569. [DOI] [PubMed] [Google Scholar]
- 30.Menzin J, Lang K, Earle CC, Kerney D, Mallick R. The outcomes and costs of acute myeloid leukemia among the elderly. Arch Intern Med. 2002;162(14):1597-1603. [DOI] [PubMed] [Google Scholar]
- 31.Mohammadi M, Cao Y, Glimelius I, Bottai M, Eloranta S, Smedby KE. The impact of comorbid disease history on all-cause and cancer-specific mortality in myeloid leukemia and myeloma - a Swedish population-based study. BMC Cancer. 2015;15(1):850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stirewalt DL, Kopecky KJ, Meshinchi S, et al. FLT3, RAS, and TP53 mutations in elderly patients with acute myeloid leukemia. Blood. 2001;97(11):3589-3595. [DOI] [PubMed] [Google Scholar]
- 33.Fathi AT, Chen YB. Treatment of FLT3-ITD acute myeloid leukemia. Am J Blood Res. 2011;1(2):175-189. [PMC free article] [PubMed] [Google Scholar]
- 34.Lazenby M, Gilkes AF, Marrin C, Evans A, Hills RK, Burnett AK. The prognostic relevance of flt3 and npm1 mutations on older patients treated intensively or non-intensively: a study of 1312 patients in the UK NCRI AML16 trial. Leukemia. 2014;28(10):1953-1959. [DOI] [PubMed] [Google Scholar]
- 35.Rücker FG, Schlenk RF, Bullinger L, et al. TP53 alterations in acute myeloid leukemia with complex karyotype correlate with specific copy number alterations, monosomal karyotype, and dismal outcome. Blood. 2012;119(9):2114-2121. [DOI] [PubMed] [Google Scholar]
- 36.Metzeler KH, Herold T, Rothenberg-Thurley M, et al. ; AMLCG Study Group. Spectrum and prognostic relevance of driver gene mutations in acute myeloid leukemia. Blood. 2016;128(5):686-698. [DOI] [PubMed] [Google Scholar]
- 37.Patel JP, Gönen M, Figueroa ME, et al. Prognostic relevance of integrated genetic profiling in acute myeloid leukemia. N Engl J Med. 2012;366(12):1079-1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Green CL, Evans CM, Zhao L, et al. The prognostic significance of IDH2 mutations in AML depends on the location of the mutation. Blood. 2011;118(2):409-412. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.