Abstract
Background
The care of elderly patients with comorbid dementia poses an increasing challenge in the acute inpatient setting, yet there remains a lack of representative studies on the prevalence and distribution of dementia in general hospitals.
Methods
We conducted a cross-sectional study of patients aged 65 and older in randomly selected general hospitals in southern Germany. Patients were excluded if they were in an intensive care unit or isolation unit or if they were on specialized wards for psychiatry, neurology, or geriatric medicine. The findings are derived from patient interviews, neuropsychological testing, standardized rating scales, questioning of nursing staff, and the patients’ medical records.
Results
1469 patients on 172 inpatient wards of 33 hospitals were studied. 40.0% of them (95% confidence interval, [36.2; 43.7]) had at least mild cognitive impairment. The point-prevalence of dementing illnesses was 18.4% [16.3; 20.7]. Delirium, most often on the basis of dementia, was present in 5.1% [3.9; 6.7]. 60.0% had no cognitive impairment. Dementia was more common among patients of very advanced age, those who were dependent on nursing care, those who lived in old-age or nursing homes, and those with a low level of education. Among patients with dementia, only 36.7% had a documented diagnosis of dementia in the medical record. Patients with dementia were treated more often for dehydration, electrolyte disturbances, urinary tract infections, contusions, and bone fractures, as well as for symptoms and findings of an unknown nature, and much less often for cancer or musculoskeletal diseases.
Conclusion
Two out of five elderly patients in general hospitals suffer from a cognitive disturbance. Patients with severe impairments such as dementia or delirium often need special care. Guidelines and model projects offer approaches by which the inpatient care of patients with comorbid dementia can be improved.
In 2016, 8.56 million older patients were treated on an inpatient basis in general hospital departments in Germany. This is equivalent to 44.7% of all inpatients of all age groups. The length of hospital stay of patients aged 65 or older was considerably longer compared with that of younger patients (8.1 days versus 4.9 days); as the result, older patients accounted for 57.1% of all days of inpatient treatment, making them the largest group of inpatients (1). A considerable number of older hospitalized patients with physical illnesses also suffer from dementia and related cognitive impairments. However, the exact number of patients experiencing these health problems is currently not known. Previous studies were almost impossible to compare because the methods they used varied widely and they typically comprised small, non-representative samples and arrived at widely divergent prevalence estimates which are only of limited use for dementia-related healthcare planning (2, 3). Hospital stays can be very stressful for patients with comorbid dementia and complications may arise (4, 5). A rapid decline in cognitive and functional skills is commonly observed (6). The risk of institutionalization and mortality is about twice as high as in patients without cognitive impairment (7– 9). This lack of knowledge about the prevalence and distribution of cognitive disorders is an obstacle to improved care which is tailored to the specific needs of these patients.
The aim of this study is to determine the point prevalence of comorbid cognitive disorders and dementia based on a representative sample of general hospital patients aged 65 or older. In addition, distribution of dementia shall be described according to demographic characteristics, departments and reasons for seeking treatment.
Methods
A more detailed description of the methods of sampling, investigation and statistical analysis used in this study is provided in the eMethods section und in eFigure 1.
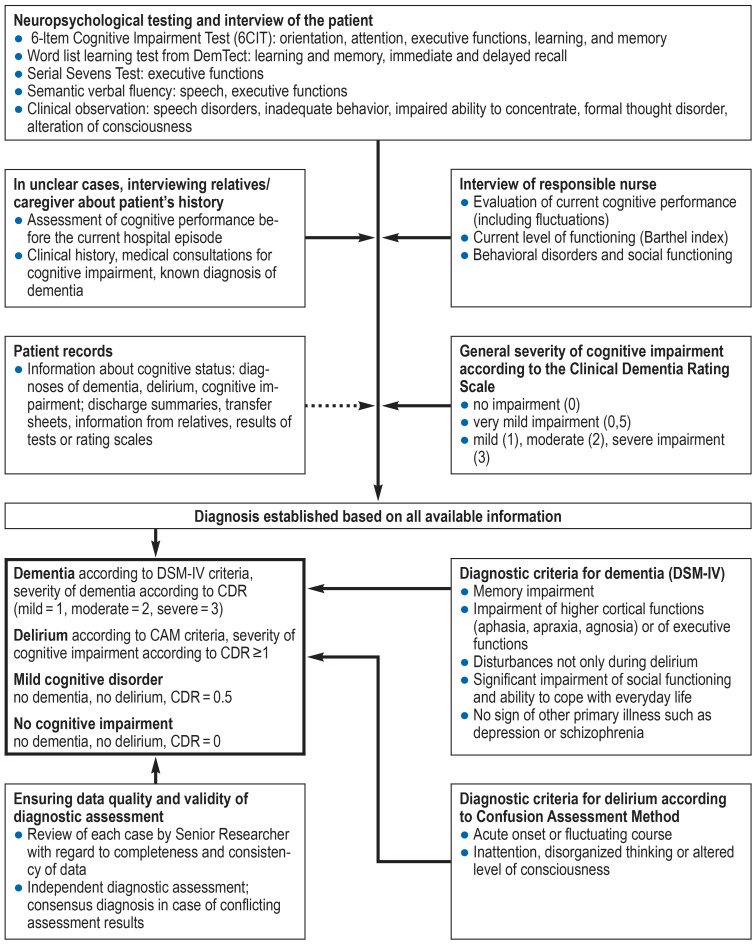
eFigure 1.
Data collection and diagnostic process
Diagnosis of dementia according to DSM-IV criteria
CDR, Clinical Dementia Rating
CAM, Confusion Assessment Method
Sampling
The aim of this study was to achieve representativeness for the German federal states of Baden-Württemberg and Bavaria. In these federal states (10, 11), general hospitals and related wards were drawn randomly. All patients aged 65 or older who were inpatients on the selected wards on the day of survey were invited to participate in the study.
Hospitals with less than 150 in-patient beds, private and specialty hospitals as well as rehabilitation and day or night clinics were excluded. Besides neurology and psychiatry where dementia usually is not a comorbid condition but the primary diagnosis, geriatrics was also not included in this analysis because detailed studies on dementia are already available for this branch of medicine (12, 13).
Patients in intensive care units and on isolation wards were not included because of the critical condition they were in or the infectious nature of their illness. Another exclusion criterion was met when the patient was moribund or did not speak German.
The Ethics Committee of the Faculty of Medicine of the Technical University of Munich approved the study protocol on 21 March 2014 (No. 66/14). In the German Registry of Clinical Studies, this study is registered under DRKS00006028. Following informed consent discussion about the content and aims of this study and provision of written information material, the written consent to participation in the study was obtained from the patients or the legal representatives.
Data collection
Data were obtained in standardized form by means of personal examination of the patient, an interview with the responsible nurse and documentation of study-relevant information from medical records. In unclear cases, additional interviews were conducted with relatives or the legal representative (eMethods section).
The cognitive status was assessed using a test battery designed for bedside assessment. This battery comprised the screening tool 6-Item Cognitive Impairment Test (14) as well as established methods of measuring primary and secondary memory, verbal fluency, attention, and executive functions (15). Dementia was diagnosed according to DSM-IV criteria, delirium according to the criteria of the Confusion Assessment Method (16, 17). Global severity of cognitive impairment was assessed using the five-point Clinical Dementia Rating (CDR) scale (18). A value of 0.5 on the CDR scale was interpreted as mild dementia (19, 20).
Statistical analysis
Point prevalence rates were calculated with 95% confidence intervals, taking intra-cluster correlations (ICC) into account (21). In order to determine the extent to which the prevalence of dementia in the hospital setting differs from that in the general population, the indirect standardized rate ratio (IRR) was calculated. For comparison with the age- and sex-specific prevalence in the older general population, the EuroCoDe data were used which are based on European field studies (22). Age- and sex-adjusted analyses of the association between dementia and demographic variables, departments or reasons for seeking treatment were performed. The cluster structure of the data was taken into account by means of logistic Generalized Estimation Equation (GEE) models (23). Data analyses were performed using OpenEpi (24), the R package (25) and SPSS 25.
Results
Description of sample
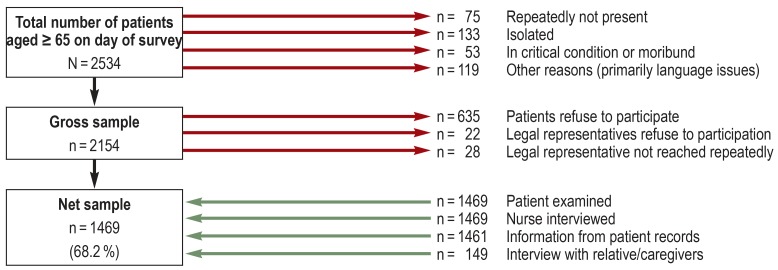
Of the 55 contacted hospitals, 33 (60%) participated in this study. A response rate breakdown is provided in Figure 1. Of the altogether 2534 patients aged 65 or older who were present on one of the 172 wards on the day of survey, 380 met an exclusion criterion or were not available on the ward at that day. From the gross sample of 2154 inpatients, 635 patients capable of consenting to participation in this study refused to take part; in another 50 cases, the legal representative did not consent or could not be contacted. Finally, the net sample comprised 1469 participants, corresponding to a participation rate of 68.2%. In all cases, a nurse was interviewed and information from the patient records was available for 99.5% of study participants. In addition, relatives or legal representatives of 149 patients were interviewed. There was no statistically significant difference between participating and non-participating patients with regard to age and sex.
Figure 1.
Response rate
The age of the assessed patients ranged between 65 and 105 years, the mean age was 78.6 years (s = 7.4). Slightly more than half of the participants were female (53.8%). Most patients were treated on medical wards (50.2%), followed by trauma surgery (20.1%), general surgery (17.0%), and other specialties, such as orthopedics, urology, gynecology, and ENT, each accounting for a percentage share of less than 4%. One third of the patients had been in hospital for up to 2 days at the time of survey, one third for 3 to 7 days, and another third for 8 or more days. The median length of inpatient stay prior to the survey day was 5 days.
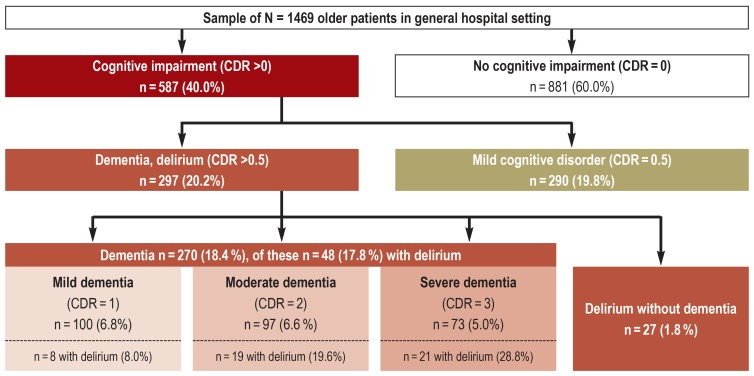
Figure 2 provides an overview of the distribution of the sample broken down by type and severity of the cognitive disorder. Altogether 60.0% of patients were assessed, using the CDR scale, as having no cognitive impairments, while the remaining 40.0% (95% confidence interval (CI): [36.2; 43.7]) experienced, in equal parts, mild (CDR = 0.5) or severe (CDR = 1) cognitive impairments. The prevalence of dementia was 18.4% [16.3; 20.7]. Mild dementia was present in 6.8% [5.4; 8.5], moderate dementia in 6.6% [5.3; 8.2] and severe dementia in 5.0% of participants [3.7; 6.6]. Seventy-five (5.1% [3.9; 6.7]) patients were diagnosed with delirium. The intracluster correlation coefficients were ICC = 0.006 for dementia, ICC = 0.014 for mild cognitive disorder and ICC = 0.012 for delirium.
Figure 2.
Distribution of patient sample by type and severity of cognitive impairment.
Information about diagnostic distribution is based on n = 1468 patients; in 1 case, diagnostic assessment not possible due to incomplete data; diagnosis of dementia according to DSM-IV criteria; diagnosis of delirium according to Confusion Assessment Method (CAM) criteria.
CDR, Clinical Dementia Rating (severity of cognitive impairment)
In two-thirds of cases, delirium was associated with underlying dementia. Only 27 patients (1.8% of the total sample) were diagnosed with delirium without underlying dementia. Among the assessed patients with dementia, the risk of delirium was significantly increased (odds ratio [OR]: 9.34 [5.13; 17.00]). With increasing severity of dementia, the percentage of associated delirium episodes increased, rising from 8.0% with mild dementia to 28.8% with severe dementia.
The percentage of participants without cognitive impairment decreased with increasing age from 85.8% among the 65-to 69-year olds to 32.0% among participants older than 90 years, while the prevalence of dementia simultaneously rose from 6.4% to 41.0% (table 1). Only in 36.7% of these patients with dementia, the diagnosis of dementia was listed in the medical records. However, with increasing severity, the percentage of known dementia rose from 12.0% to 37.1% to 69.9% for existing mild, moderate and severe dementia, respectively.
Table 1. Patients without cognitive impairment and age-specific point prevalence of mild cognitive disorder, dementia and delirium.
| Age | Sample | Number of patients (age-specific prevalence rate in %) | |||
| N |
No cognitive disorder n (%) |
Mild cognitive disorder n (%) |
Dementia*1 n (%) |
Delirium*2 n (%) |
|
| 65–69 | 204 | 175 (85.8) | 16 (7.8) | 13 (6.4) | 0 (0.0) |
| 70–74 | 277 | 206 (74.4) | 45 (16.2) | 23 (8.3) | 3 (1.1) |
| 75–79 | 382 | 261 (68.3) | 65 (17.0) | 47 (12.3) | 9 (2.4) |
| 80–84 | 291 | 131 (45.0) | 85 (29.2) | 71 (24.4) | 4 (1.4) |
| 85–89 | 214 | 76 (35.5) | 56 (26.2) | 75 (35.0) | 7 (3.3) |
| ≥ 90 | 100 | 32 (32.0) | 23 (23.0) | 41 (41.0) | 4 (4.0) |
| ≥ 65 | 1468 | 881 (60.0) | 290 (19.8) | 270 (18.4) | 27 (1.8) |
*1 including the 48 patients with dementia and concomitant delirium; *2 without the 48 patients with delirium and concomitant dementia
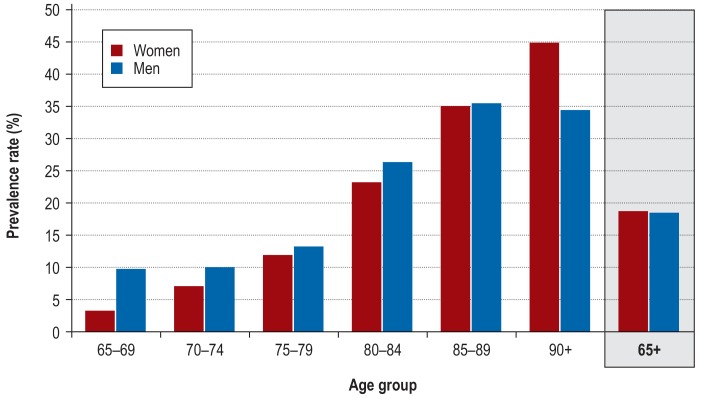
In eFigure 2, the prevalence of dementia in the sample is depicted, broken down by age and sex. Among the 65- to 84-year-olds, men experienced dementia more frequently than women, while in the age group 90 years or older, a female preponderance was noted. Overall, there was no difference between the prevalence rates for male and female patients (18.3% vs. 18.5%).
eFigure 2.
Age- and sex-specific prevalence of dementia in the patient sample
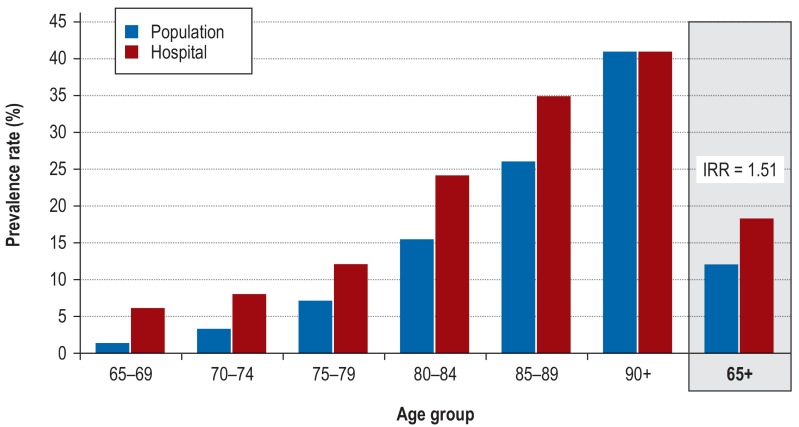
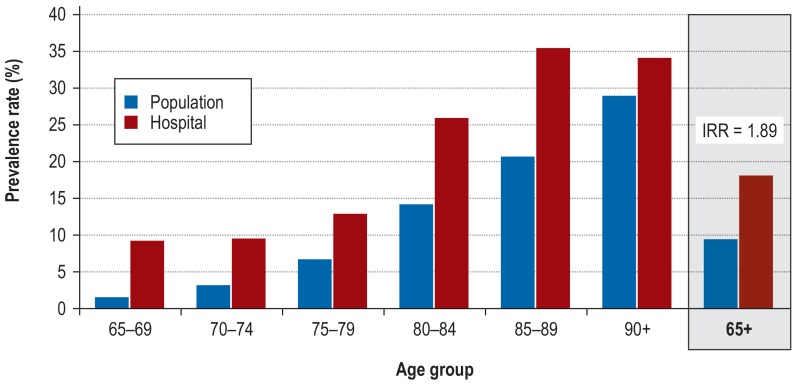
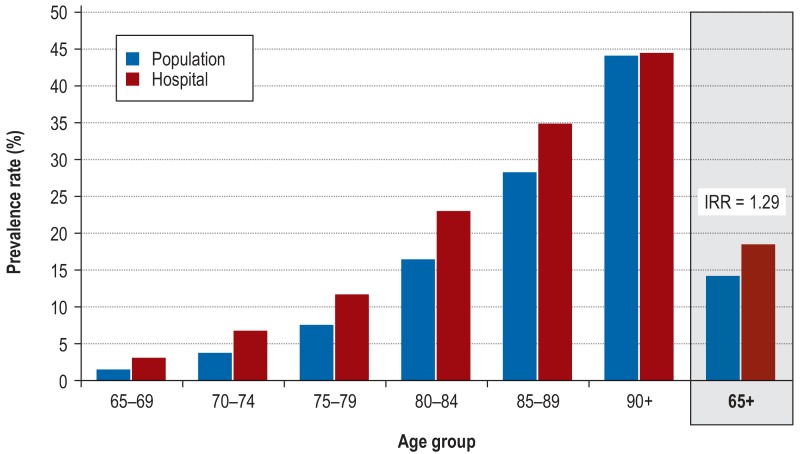
In comparison with the general population, the age- and sex-specific point prevalence rates in the general hospital setting (efigure 3) were found significantly increased, especially in the lower age groups. Among the 65- to 69-year-olds, the rates were 4-times higher compared to the general population. With increasing age, they gradually converged to become identical in the oldest age group. Overall, with an IRR = 1.51 [1.33; 1.70] for the general hospital setting, the prevalence of dementia was found increased by 51% compared to the rate to be expected on the basis of the demographic composition of the participants. A significant overrepresentation by 89% was found among male patients (efigure 4) (IRR: 1.89 [1.57; 2.25]), while the prevalence of dementia among female patients (efigure 5) was only increased by 29% (IRR: 1.29 [1.09; 1.52]).
eFigure 3.
Prevalence of dementia in the general hospital versus in the population
Prevalence rate in the general hospital: according to this study; age- and sex-specific prevalence rate in the elderly population: according to EuroCoDe (22)
IRR, indirect standardized rate ratio
eFigure 4.
Prevalence of dementia among men in the general hospital versus in the population
Prevalence rate among male general hospital patients: according to this study; age-specific prevalence rate in the male elderly population: according to EuroCoDe (22)
IRR, indirect standardized rate ratio
eFigure 5.
Prevalence of dementia among women in the general hospital versus in the population
Prevalence rate among female general hospital patients: according to this study; age-specific prevalence rate in the female elderly population: according to EuroCoDe (22)
IRR, indirect standardized rate ratio
Nursing home residents and persons requiring nursing care were among the patient groups most frequently affected by dementia. Among the nursing home residents, 67.2% of patients had dementia, while among the patients with a nursing care level (“Pflegestufe”) the prevalence was 43.7% (table 2). By department, the highest prevalence of dementia was found in internal medicine departments with 21.3%, followed by trauma surgery departments with 19.7%. The rates were significantly lower in general surgery and the remaining departments where patients with dementia account for just over 12% of patients.
Table 2. Distribution of mild cognitive disorders, dementia and delirium by demographic characteristics, nursing care needs and departments.
| Characteristic*1 |
No cognitive
disorder (n = 881) |
Mild cognitive disorder (n = 290) |
Dementia (n = 270) |
Delirium (n = 27) |
| Age in years, M (SD) | 76.4 (6.9) | 80.7 (6.7) | 83.3 (7.1) | 82.3 (6.5) |
| Sex, n (%): male female |
415 (61.2) 466 (59.0) |
161 (19.0) 129 (20.4) |
124 (18.3) 146 (18.5) |
10 (1.5) 17 (2.1) |
| Marital status, n (%): single married divorced widowed |
44 (57.1) 504 (67.0) 62 (66.0) 271 (49.9) |
20 (26.0) 125 (16.6) 20 (21.3) 125 (23.0) |
12 (15.6) 111 (14.8) 11 (11.7) 134 (24.7) |
1 (1.3) 12 (1.6) 1 (1.1) 13 (2.4) |
| School-leaving qualification, n (%): No school-leaving certificate Lower secondary school-leaving certificate Secondary school-leaving certificate General/technical university entrance qualification |
11 (27.5) 562 (56.5) 167 (71.4) 140 (72.9) |
16 (40.0) 210 (21.1) 35 (15.0) 28 (14.6) |
11 (27.5) 207 (20.8) 27 (11.5) 20 (10.4) |
2 (5.0) 16 (1.6) 5 (2.1) 4 (2.1) |
| Residential living arrangement, n (%): Alone in private home With partner in private home With other relatives/other persons in private home Assisted living Retirement or nursing home |
297 (65.1) 475 (70.2) 62 (37.3) 28 (58.3) 19 (16.0) |
99 (21.7) 115 (17.0) 47 (28.3) 12 (25.0) 17 (14.3) |
53 (11.6) 76 (11.2) 52 (31.3) 7 (14.6) 80 (67.2) |
7 (1.5) 11 (1.6) 5 (3.4) 1 (2.1) 3 (2.5) |
| Nursing care needs pursuant Social Insurance Code XI, n (%): No nursing care level Applied for nursing care level Nursing care level approved |
741 (74.3) 24 (38.1) 112 (30.0) |
170 (17.1) 23 (36.5) 88 (23.6) |
74 (7.4) 14 (22.2) 163 (43.7) |
12 (1.2) 2 (3.2) 10 (2.7) |
| Department, n (%): Internal Medicine Trauma surgery General surgery Other departments (orthopedics, urology, gynecology, ENT, etc.) |
403 (54.8) 172 (58.3) 170 (68.0) 136 (72.7) |
158 (21.5) 59 (20.0) 46 (18.4) 27 (14.4) |
157 (21.3) 58 (19.7) 32 (12.8) 23 (12.3) |
18 (2.4) 6 (2.0) 2 (0.8) 1 (0.5) |
*1 In some cases, data are missing; each stated line percentage is based on the valid cases; *2 including the 48 patients with dementia and concomitant delirium
*3 without the 48 patients with delirium and concomitant dementia
Age, education, residential living arrangement and need of assistance were associated with dementia (etable 1). Most affected were patients aged older than 80 years or in need of nursing care, with low school-leaving qualifications, living together with family or other caregivers, or living in a nursing home. Sex and marital status were not associated with dementia.
eTable 1. Association of demographic variables, nursing care needs and department with comorbid dementia.
| Characteristic |
Unadjusted odds ratio [95% CI] |
Adjusted odds ratio* [95% CI] |
| Age group: 65–69 70–74 75–79 80–84 85–89 90+ |
1.0 (reference) 1.50 [0.79; 2.86] 2.42 [1.24; 4.74] 7.30 [3.92; 13.59] 13.46 [7.44; 23.72] 17.25 [8.53; 34.87] |
1.0 (reference) 1.52 [0.80; 2.88] 2.44 [1.25; 4.77] 7.39 [3.94; 13.83] 13.59 [7.66; 24.10] 17.90 [8.75; 36.61] |
| Sex: female male |
1.0 (reference) 0.95 [0.75; 1.21] |
1.0 (reference) 1.18 [0.89; 1.57] |
| School-leaving qualification: Lower secondary school-leaving certificate No school-leaving certificate Secondary school-leaving certificate General/technical university entrance qualification |
1.0 (reference) 2.71 [1.16; 6.35] 0.44 [0.29; 0.66] 0.39 [0.22; 0.68] |
1.0 (reference) 2.63 [0.92; 7.51] 0.46 [0.29; 0.73] 0.34 [0.18; 0.65] |
| Marital status: widowed single married divorced |
1.0 (reference) 0.55 [0.29; 1.07] 0.45 [0.33; 0.60] 0.36 [0.16; 0.81] |
1.0 (reference) 1.01 [0.53; 1.94] 0.76 [0.54; 1.08] 0.85 [0.34; 2.10] |
| Residential living arrangement: Alone in private home With partner in private home With other relatives/other persons in private home Assisted living Retirement or nursing home |
1.0 (reference) 0.90 [0.56; 1.43] 4.70 [2.65; 8.33] 1.40 [0.52; 3.87] 23.60 [11.63; 47.87] |
1.0 (reference) 1.14 [0.65; 2.01] 4.72 [2.24; 9.23] 1.19 [0.42; 3.39] 21.29 [9.28; 48.85] |
| Need for nursing care pursuant SGB XI: No nursing care level Applied for nursing care level Nursing care level approved |
1.0 (reference) 5.84 [3.32; 10.27] 14.57 [9.87; 21.51] |
1.0 (reference) 4.26 [2.41; 7.50] 10.13 [6.54; 15.68] |
| Department: Internal medicine Trauma surgery General surgery Other departments (orthopedics, urology, gynecology, ENT, et cetera) |
1.0 (reference) 0.87 [0.59; 1.27] 0.48 [0.32; 0.73] 0.43 [0.25; 0.77] |
1.0 (reference) 0.93 [0.58; 1.49] 0.58 [0.38; 0.88] 0.60 [0.34; 1.07] |
*adjusted for age in years and sex; Patients without cognitive impairment (CDR = 0) constitute the reference group (odds ratios with p<0.05 in bold). 95% CI, 95% confidence interval; ENT, Ear, Nose and Throat; SGB XI, Book 11 of the German Social Insurance Code
In eTable 2, the reasons for seeking treatment were compared between patients with dementia versus cognitively unimpaired patients. Even after adjustment for age and sex, diagnoses from four key groups, created based on ICD-10, were significantly more common among patients with dementia, while diagnoses from two groups were rarer. In patients with dementia, dehydration and electrolyte imbalances as well as urinary tract infections and lower respiratory tract infections were more common. They also experienced signs and symptoms such as vomiting, fever, dysphagia, and urinary retention more frequently. In addition, general physical decline, injuries and bruises, as well as rib and hip fractures were more common in this patient group. By contrast, patients with dementia less frequently presented for inpatient treatment because of cancer and various types of musculoskeletal disorders.
eTable 2. Association between reason for seeking treatment and comorbid dementia.
|
Diagnostic category (ICD-10 code; diagnosis frequency in %) |
unadjusted odds ratio [95% CI] |
adjusted* odds ratio[95% CI] |
| Infectious diseases (A0-B99; 4,4 %) | 1.00 [0.47; 2.12] | 1.12 [0.48; 2.61] |
| Neoplasms (C0-D48; 9.9 %) | 0.30 [0.17; 0.52] | 0.37 [0.21; 0.66] |
| Diseases of the blood (D50-D89; 2.6 %) | 0.64 [0.27; 1.56] | 0.62 [0.25; 1.55] |
| Endocrine diseases (E0-E90; 7.0 %) | 2.51 [1.54; 4.08] | 2.23 [1.38; 3.61] |
| Diseases of the nervous system (G0-G99; 2.1 %) | 1.63 [0.51; 5.29] | 1.68 [0.46; 6.17] |
| Diseases of the circulatory system (I0-I99; 22.5 %) | 1.43 [1.04; 1.97] | 1.25 [0.92; 1.72] |
| Diseases of the respiratory system (J0-J99: 9.2 %) | 1.77 [1.15; 2.72] | 1.50 [0.93; 2.42] |
| Diseases of the digestive system (K0-K99; 12.9 %) | 0.56 [0.32; 0.98] | 0.58 [0.32; 1.07] |
| Diseases of the skin (L0-L99; 2.1 %) | 2.55 [0.85; 7.65] | 2.80 [0.92; 8.50] |
| Diseases of the musculoskeletal system (M0-M99; 14.5 %) | 0.09 [0.04; 0.24] | 0.11 [0.04; 0.30] |
| Diseases of the genitourinary system (N0-N99; 7.7 %) | 1.65 [0.92; 2.98] | 1.79 [1.00; 3.24] |
| Symptoms, abnormal findings (R0-R99; 26.9 %) | 1.97 [1.56; 2.50] | 1.60 [1.24; 2.06] |
| Injuries, intoxications (S0-T99; 19.9 %) | 1.75 [1.25; 2.45] | 1.66 [1.09; 2.54] |
* adjusted for age in years and sex; patients without cognitive impairment (CDR = 0) constitute the reference group
(odds ratios with p<0.05 in bold)
95% CI, 95% confidence interval
Discussion
In general hospitals, comorbid dementia and cognitive disorders are common. Altogether, 40% of older patients had cognitive disorders, ranging from mild impairments to severe dementia; 60% showed no cognitive impairment. These estimates refer to patients from general departments, excluding the departments of psychiatry, neurology and geriatrics as well as intensive care units and isolation wards.
In our sample, the prevalence of dementia of 18.4% was about twice as high compared to the general German population aged 65 or older where it was, according to epidemiological estimates, 9.1% (26). Indirect standardization of the prevalence rate by age and sex showed that half of this overrepresentation of dementia was explained by the older age of the hospital patients. When the inpatients’ age structure was taken into account, the expected value was only surpassed by 51%. This residual increase in the prevalence of dementia is primarily explained by male patients and the age groups below 90 years of age. It could be brought about by the fact that older patients with dementia are more frequently admitted and their duration of hospital stay is longer. According to health insurance data from the federal state of Saxony, the increase is primarily the result of an increased risk of admission for patients with dementia and not due to longer duration of stay (27).
One fifth of hospital patients had mild cognitive disorders. So far, hardly any research has been conducted to clarify whether these mild impairments are already associated with treatment complications and require special healthcare measures. However, it appears to be advantageous to also study the impact of mild cognitive disorders on the course and outcome of inpatient treatment.
Even though delirium was not uncommon in our sample, the prevalence of 5.1% which we found was still at the lower end of the estimates reported so far (28). However, it should be noted that the point prevalence of our study cannot be directly compared with the period prevalence of the delirium studies. Due to its relapsing and remitting course which tends to fluctuate throughout the day, delirium is a disorder which cannot be fully captured by an examination performed at one point in time. In this case, it would be more appropriate to determine the period prevalence over the entire length of inpatient stay, closely monitoring the patient so that short and night-time episodes of delirium are captured
The results were as expected for the risk groups. Dementia was especially common among at least 80-year-olds, patients requiring nursing care and nursing home residents. The departments of internal medicine and trauma surgery had the highest percentages of patients with dementia. By paying more attention to so-called ambulatory care sensitive conditions, opportunities to reduce dementia prevalence in hospitals may open up. As described in numerous other studies (29– 31), patients with dementia were often admitted for health problems which could have been treated on an outpatient basis or ideally even prevented.
The strengths of our study include the large sample size and the use of multiple sources of information, contributing to the high external and internal validity of the results. Generalizability is limited by the fact that participation rates of hospitals and patients were under 70% and that small hospitals, intensive care units and isolation wards, as well as moribund patients and patients who did not speak German were excluded.
Analyzing sample failures and effects of the study design, no indication of systematic bias was found. There was no difference between participants and non-participants with regard to age and sex. The refusal rates among patients capable of consenting to participation was as high as the non-participation rates among patients with legal representatives. The number of beds of the hospitals was not correlated with the prevalence rates of dementia, delirium or mild cognitive disorders, making potential bias due to variations in hospital size unlikely. The excluded hospitals with less than 150 in-patient beds account for only 9% of the days of stay (1). The prevalence of dementia was not higher among patients assessed after surgery than among the remaining patients (data not shown). This could indicate that transient postoperative cognitive dysfunction was not misdiagnosed as dementia. In addition, our results are in line with those of other primary studies (table 3).
Table 3. Dementia prevalence rates of earlier studies compared with the prevalence rate in this study for the matching dementia severity levels, departments and patient age groups.
|
Authors (year), country, sample size |
Dementia severity, department |
Age |
Prevalence rate (%) in in comparable patient groups |
|
|
earlier study |
this study (GHoSt) |
|||
| Erkinjuntti et al. 1986, Finland, N = 1492 (32) |
moderate and severe, internal medicine |
≥ 65*1 | 11.9 | 12.2 |
| Erkinjuntti et al. 1988, Finland, N = 282 (33) |
moderate and severe, internal medicine |
≥ 65 | 12.1 | 12.2 |
| Bickel et al. 1993, Germany, N = 626 (34) |
moderate and severe, (dementia and delirium), internal medicine |
65–80 | 9.1 | 9.0 |
| Kolbeinsson et al. 1993, Iceland, N = 272 (35) |
mild to severe, internal medicine |
≥ 70 | 18.4 | 22.5 |
| Wancata et al. 1996, Austria, N = 228 (36) |
mild to severe, internal medicine, surgery, gynecology |
≥ 65 | 23.7 | 19.1 |
| Arolt et al. 1997, Germany, N = 211 (37) |
mild to severe, internal medicine, surgery |
≥ 65 | 18.0 | 19.4 |
| Sampson et al. 2009, United Kingdom, N = 617 (9) |
mild to severe (delirium without dementia excluded), acute admission to general hospital*2 |
≥ 70 | 42.4 | 25.7 |
| Travers et al. 2013, Australia, N = 493 (38) |
mild to severe, internal medicine, general surgery, orthopedics |
≥ 70 | 20.7 | 21.0 |
| Timmons et al. 2015, Ireland, N = 598 (39) |
mild to severe, 5 general hospitals*3 |
≥ 70 | 24.9 | 20.3 |
| Reynish et al. 2017, Scotland, N = 10 014 (40) |
mild to severe, general hospital*4 |
≥ 65 | 17.3 | 18.4 |
*1 own calculations; *2 all departments excluding psychiatry, gynecology, ENT, ophthalmology, special surgical departments
*3 Public hospitals without detailed specification of departments; *4 district general hospital without detailed specification of departments
When subgroups are formed and dementia prevalence rates are calculated for the same patient groups which the other primary studies referred to, the values are almost identical. This fact indicates an almost equal prevalence of comorbid dementia across the hospitals of industrialized countries. For the 3 earlier studies evaluating moderate and severe dementia, the median prevalence was 11.9% (32– 34); in our study, the rate for severe dementia is 12.2%. For all levels of dementia severity, from mild to severe, the median in seven earlier studies was 20.7% (9, 35– 40) compared to 20.3% in our study. A large Scottish study has recently reported a prevalence for the entire spectrum of cognitive disorders among older patients of 38.5% (40). This value is almost identical with our rate of 40.0%.
According to the hospital statistics, in Germany in 2016 about on average 190 000 at least 65-year-olds received inpatient treatment in general departments (without psychiatry/psychosomatics) (1). When the point prevalence rates are applied to these patient numbers, every day on average about 76 000 older patients with comorbid cognitive impairments are treated in hospital, including approximately 35 000 with dementia and 38 000 with mild cognitive disorders. There is an urgent need to take greater account of the special healthcare needs of this vulnerable patient group.
Supplementary Material
eMETHODS
Sampling
This sample was chosen to achieve representativeness for the two German federal states Baden-Württemberg and Bavaria where more than 23 million people (29% of the total German population) live. A multi-step sampling strategy was used. First, the general hospitals of both federal states were arranged in a random sequence, contacted in this sequence and invited to participate. In each of the hospitals willing to cooperate, five wards and one substitute ward were selected. All patients aged 65 or older who were inpatients on the selected wards on the day of survey and met the inclusion criteria were invited to participate in the study. Where the number of participants was less than 40, patients of a substitute ward were additionally included in the analysis.
For an estimation accuracy of ± 2%, a sample size of at least 1200 patients is required, assuming a prevalence of dementia of 15%. Based on this lower limit, it was necessary to ensure participation of at least 30 hospitals, each with 40 or more surveyed patients.
The following inclusion and exclusion criteria were defined for hospitals, wards and patients, respectively: General hospitals were identified based on the respective hospital plan of each of the two federal states. In Bavaria, they were the hospitals of the first, second and third level of care (10) and in Baden-Württemberg, they were the approved hospitals with at least two departments at one hospital location (11). According to this definition, altogether 301 general hospitals were found in the two federal states. Specialty hospitals and entirely private hospitals as well as rehabilitation and day or night clinics were excluded from sampling. For survey-economic reasons, 92 general hospitals with less than 150 inpatient beds were excluded (30.6%), leaving a basic set of 209 general hospitals and university hospitals.
In hospitals with less than 150 beds, a relatively small proportion of the patients is treated on an inpatient basis. Although nationwide, they make up 42.7% of the general hospitals, they only account for 9.0% of the days of inpatient care (1). Since in Southern Germany the proportion of smaller hospitals is with 30.6% even below the nationwide level of 42.7%, it can be assumed that no relevant bias is introduced by their exclusion.
On the ward level, intensive care units and isolation wards were excluded. Since in geriatric hospitals detailed studies on dementia have already been conducted (12, 13), this branch of medicine was excluded as were neurology and psychiatry where dementia usually is a primary diagnosis, not a comorbidity.
On the patient level, inclusion criteria comprised a minimum age of 65 years and the written consent to participation by the patient or their legal representative. Patients were excluded if they:
The study protocol was approved by the Ethics Committee of the Faculty of Medicine of the Technical University of Munich (TUM) on 21 March 2014 (No. 66/14). The study is registered in the German Clinical Trials Register (DRKS) under DRKS00006028. The written consent to participation in the study was obtained from the patients or their legal representatives following informed consent discussion about the content and aims of this study and provision of written information material.
Data collection
Five trained research assistants carried out the survey from June 2014 to end of May 2015. All assistants were qualified by having graduated in psychology, gerontology or social work and had previous research or clinical experience in gerontopsychiatry. Prior to the start of the study, the research assistants were extensively trained in the use of the survey instruments and application of the diagnostic criteria. All interviews were reviewed for completeness, plausibility and conformity of the assessment with the diagnostic criteria by the Senior Researchers of the project. During regular case conferences, the diagnostic assessments were discussed. Any disagreements were resolved by consensus decision.
Data were obtained in standardized form by personal examination of the patient, an interview with the responsible nurse and documentation of study-relevant information from medical records. In unclear cases, additional interviews were conducted with relatives or the legal representative of the patient (efigure1).
Because all patients of a ward were usually examined on the same survey date, it was possible to complete data collection on the selected wards of a hospital within 1 week. Examinations were only conducted on business days and from Monday to Friday in the sequence in which the wards had been randomly selected.
Cognitive status was assessed using a bedside test battery, comprising the screening tool 6-Item Cognitive Impairment Test (14) and established tests to assess primary and secondary memory, verbal fluency, attention and executive functions (15). Global severity of cognitive impairment was assessed using the Clinical Dementia Rating (CDR) scale (18). With this instrument, the degree of impairment in six domains of performance (memory, orientation, judgment & problem solving, community affairs, home & hobbies, and personal care) is externally assessed on a 5-point scale and a global rating derived:
After having examined the patient, the interviewer rated the severity of the cognitive disorders using the CDR scale.
The nurse responsible for the patient was asked about:
If the nursing staff was not yet familiar enough with a patient or if the cognitive status was unclear, the patient’s relative or caregiver was contacted to obtain further information. In addition, we retrieved from the patient records, besides information about the reason for seeking treatment and about the medication, study-relevant information, such as known diagnoses of dementia and delirium or other signs of cognitive disorders.
Taking into account all available information, patients were assigned to one of four categories of diagnosis (efigure 1). Dementia was diagnosed using DSM-IV criteria. Besides memory impairments, these include at least one other higher cortical function and one impairment of social functioning or of the ability to cope with everyday life.
Delirium was diagnosed using the Confusion Assessment Method (CAM) (16, 17) which is based on the criteria inattention, altered level of consciousness and disorganized thinking. CAM requires these symptoms to have an acute onset or fluctuating course over the day. Based on the reports of the nursing staff, relatives and caregivers and taking into account information from the patient records, we differentiated between delirium with dementia and delirium without severe preexisting cognitive deficits.
A rating of 0.5 on the CDR scale was regarded as a mild cognitive disorder (19). This score indicates an impairment in the transition zone between normal-for-age cognitive performance and mild dementia which is characterized by a high risk of developing dementia later in life. A prospective study, comparing older individuals with normal cognitive performance to patients with this level of cognitive impairment, found that the latter had a 25-times increased risk of conversion to dementia (20).
Patients with no impairments, scoring 0 on the CDR scale, make up the category of persons without cognitive impairments.
Statistical analysis
The correlation of patients among each other within the 33 included hospitals (Intracluster Correlation Coefficient, ICC) was estimated using the method described by Goldstein et al. (21). As recommended for binary variables (23), statistical analyses were performed using logistic Generalized Estimation Equation (GEE) models to ensure intracluster correlation was taken into account. For point prevalence rate estimates, models without influencing variable (intercept-only) were adapted to the data in order to ensure that the cluster structure is taken into account when estimating confidence intervals. For calculating associations between demographic variables, departments, reasons for seeking treatment, and other relevant variables with the endpoint dementia, the respective characteristics were used as the independent variable and the binary endpoint dementia as the dependent variable in the models (eTables 1 and 2). Analyses were performed with and without adjustment for the a priori defined variables age and sex. When adjusting for the effect of age, the age in years (two decimal places) at the time of examination was used as the independent variable. The few values missing for certain analyses were not replaced. The results exclusively refer to patients where complete data for the respective analysis were available. Data analyses were performed using OpenEpi (24), the R package (25) and SPSS 25 for Windows, Version 25.
Hospital diagnoses obtained from the patient records on survey day were classified according to the ICD-10 major diagnostic categories. Using this strategy, it was possible to identify associations between dementia and the reasons for seeking treatment. For each of the ICD major diagnostic categories, each starting with a capital letter, a binary variable with the value 0 for absence of a diagnosis and 1 for the presence of at least one diagnosis was created. ICD major diagnostic categories found at a rate of less than 2.0% were not included in the further analyses. Associations between diagnostic category and dementia were calculated with and without adjustment for age and sex (etable 2). If the adjusted odds ratio indicated with a probability of more than 95% an increased or reduce occurrence of the respective diagnostic category among patients with dementia, it was assessed based on more detailed ICD diagnoses which specific diagnoses of this diagnostic category had contributed most to the differences. These noses are named in the text as less or more common reasons for seeking treatment.
Indirect standardization was performed to assess whether the prevalence of dementia in the hospital differed from that in the general population when age and sex structure of hospital patients were taken into account. For comparison of dementia prevalence among hospital patients, the age- and sex-specific rates according to EuroCoDe (22) were used which are based on European field studies. In the eFigures 3–5, the age-specific prevalence rates found in the hospital setting are compared with the expected rates from the general population. The indirect standardized rate ratio (IRR) expresses by which factor the prevalence observed in the hospital setting differs from the prevalence in the general population of the same age.
were moribund
were in a critical condition according to medical staff where interviewing and examination could have a detrimental effect
had been isolated because of an infectious disease
did not speak German.
Global score 0 connotes no cognitive disorders or impairments in everyday life
Global score 0.5 is characterized by constant forgetfulness and very mild or questionable impairment of judgement and coping with domestic and external tasks. Orientation and personal care remain intact.
Global score 1 indicates cognitive impairments of a severity equivalent to mild dementia, with difficulties in performing basic activities of daily life.
Global score 2 indicates moderate dementia. It is associated with severe memory loss, impaired orientation, inability to perform activities outside the home and the need for assistance with everyday activities, such as getting dressed and washing.
Global score 3 indicates severe dementia with almost complete loss of memory and orientation as well as full dependence on third-party care.
impairment of cognitive performance of the patient
changes in cognition and consciousness during the hospital stay
functional impairments
behavioral abnormalities.
The clinical perspective.
Comorbid dementia imposes a considerable burden on those affected, their relatives and the hospital staff as well as other patients. Typically, it is associated with increased care requirements and costs. There is a risk of severe secondary damage to the health of these patients. At the same time, hospitals are not adequately prepared for the special needs of the growing number of patients with dementia (e1).
The following recommendations for improved inpatient care are derived from guidelines and model projects (e2– e5):
Identification of cognitive disorders on admission and during the hospital course, using adequate screening instruments (15, 18, e6)
Use of information sheets, providing information about habits, competency limitations, and remaining abilities of the patient (e7)
Education of medical and nursing staff about dementia, how to establish contact and adequate communication, even with challenging behavior (e8– e11)
Establishing programs for delirium prevention (e.g. the Hospital Elder Life Program [e6, e12]) which can be carried out by qualified nursing staff; improved sleep, pain and medication management; assurance of adequate food and fluid intake (e13– e15)
Reducing anxiety and disorientation by providing orientation support (information about time and place, availability of personal items, such as glasses or hearing aids), structuring the day’s activities, giving personal attention and offering continuous support by patient attendants, training volunteers, integrating family members (rooming-in), and creating a familiar-looking, non-threatening environment (e6)
Training and appointing of dementia commissioners, increased engagement of gerontopsychiatric professionals and utilization of gerontopsychiatric liaison services, setting up interdisciplinary wards for dementia patients (processes adapted to changed perception and individual diurnal rhythm, creation of dementia-friendly setting, staff trained in gerontopsychiatry) (e3, e16)
Key messages.
Of all general hospital patients aged 65 or older in the sample analyzed in this study, 18.4% suffered from comorbid dementia and 19.8% had mild cognitive disorders.
On average, in Germany about 35 000 patients with comorbid dementia receive inpatient care in general hospital departments (without psychiatry) on any given day
Half of this high prevalence of dementia is explained by the age composition of the patients, the other half by higher admission rates and longer length of stay for patients with dementia.
Internal medicine and trauma surgery are the departments with the highest prevalence of dementia.
Patients with dementia are often admitted for inpatient treatment of urinary tract infection and pneumonia, injuries and fractures as well as physical decline, dehydration and fever.
Neoplasia and musculoskeletal disorders occur less frequently compared to patients without cognitive impairment.
Acknowledgments
Translated from the original German by Ralf Thoene, MD.
Acknowledgement The Robert Bosch Foundation enabled us to carry out the project “Dementia and Delirium in the General Hospital: Prevalence and Care Situation“. We received additional funding from the German Alzheimer‘s Association (Deutsche Alzheimer Gesellschaft). We extend our sincere thanks to the participating patients and their relatives, the hospital staff members and the hospitals for their cooperation. We appreciate very much the practical support of the Ministry of Employment and Social Order, Family, Women and Senior Citizens, Baden-Württemberg, the Bavarian State Ministry of Health and Care, the regional hospital associations of Baden-Württemberg and Bavaria as well as the German Alzheimer’s Association. We would also like to thank the healthcare experts who supported us with their advice during the planning stage of the study.
Footnotes
Conflict of interest
Dr. Bickel received reimbursement of travel expenses and study support (third-party funding) from the Robert Bosch Foundation. Mrs. Hendlmeier received reimbursement of congress fees and travel expenses, lecture fees, and study support (third-party funding) from the Robert Bosch Foundation. Prof. Schäufele received reimbursement of travel expenses and study support (third-party funding) from the Robert Bosch Foundation.
The remaining authors declare no conflict of interest.
References
- 1.Statistisches Bundesamt (Destatis) Gesundheit, Grunddaten der Krankenhäuser. 2016 Fachserie 12, Reihe 6.1.1, 2017. [Google Scholar]
- 2.Mukadam N, Sampson EL. A systematic review of the prevalence, associations and outcomes of dementia in older general hospital inpatients. Int Psychogeriatr. 2011,;23:344–355. doi: 10.1017/S1041610210001717. [DOI] [PubMed] [Google Scholar]
- 3.Pinkert C, Holle B. Menschen mit Demenz im Akutkrankenhaus Literaturübersicht zu Prävalenz und Einweisungsgründen. Z Gerontol Geriat. 2012;45:728–734. doi: 10.1007/s00391-012-0319-1. [DOI] [PubMed] [Google Scholar]
- 4.Jackson TA, Gladman JRF, Harwood RH, et al. Challenges and opportunities in understanding dementia and delirium in the acute hospital. PLoS Med. 2017,;14 doi: 10.1371/journal.pmed.1002247. e1002247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dewing J, Dijk S. What is the current state of care for older people with dementia in general hospitals? A literature review. Dementia (London) 2016,;15:106–124. doi: 10.1177/1471301213520172. [DOI] [PubMed] [Google Scholar]
- 6.Hartley P, Gibbins N, Saunders A, et al. The association between cognitive impairment and functional outcome on hospitalised older patients: a systematic review and meta-analysis. Age Ageing. 2017,;46:559–567. doi: 10.1093/ageing/afx007. [DOI] [PubMed] [Google Scholar]
- 7.Briggs R, Dyer A, Nabeel S, et al. Dementia in the acute hospital: the prevalence and clinical outcomes of acutely unwell patients with dementia. QJM. 2017,;110:33–37. doi: 10.1093/qjmed/hcw114. [DOI] [PubMed] [Google Scholar]
- 8.Fogg C, Meredith P, Bridges J, Gould GP, Griffiths P. The relationship between cognitive impairment, mortality and discharge characteristics in a large cohort of older adults with unscheduled admissions to an acute hospital: a retrospective observational study. Age Ageing. 2017,;46:794–801. doi: 10.1093/ageing/afx022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sampson EL, Blanchard MR, Jones L, Tookman A, King M. Dementia in the acute hospital: prospective cohort study of prevalence and mortality. Brit J Psychiatry. 2009,;195:61–66. doi: 10.1192/bjp.bp.108.055335. [DOI] [PubMed] [Google Scholar]
- 10.Bayerisches Staatsministerium für Umwelt und Gesundheit. Krankenhausplan des Freistaates Bayern. Stand: 1. Januar 2013 (38. Fortschreibung) www.bkg-online.de/media/file/11606.khplan13.pdf (last accessed on 21 March 2014) [Google Scholar]
- 11.Ministerium für Arbeit und Sozialordnung. Krankenhausplan 2014. Verzeichnis der zugelassenen Krankenhäuser. www.sozialministerium.baden-wuerttemberg.de/fileadmin/redaktion/m-sm/intern/downloads/Publikationen/KH-Plan_2014_A3_Verzeichnis-Kliniken.pdf (last accessed on 21 March 2014) [Google Scholar]
- 12.Trauschke T, Werner H, Gerlinger T. Zur Diagnostik und Häufigkeit von demenziellen Erkrankungen Eine prospektive Untersuchung im Alltag einer geriatrischen Klinik (PAOLA-Studie) Z Gerontol Geriat. 2009;42:385–390. doi: 10.1007/s00391-009-0043-7. [DOI] [PubMed] [Google Scholar]
- 13.von Renteln-Kruse W, Neumann L, Klugmann B, et al. Geriatric patients with cognitive impairment—patient characteristics and treatment results on a specialized ward. Dtsch Arztebl Int. 2015;112:103–112. doi: 10.3238/arztebl.2015.0103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brooke P, Bullock R. Validation of a 6 item cognitive impairment test with a view to primary care usage. Int J Geriat Psychiatry. 1999;14:936–940. [PubMed] [Google Scholar]
- 15.Hessler JB, Schäufele M, Hendlmeier I, et al. The 6-Item Cognitive Impairment Test as a bedside screening for dementia in general hospital patients: results of the General Hospital Study (GHoSt) Int J Geriat Psychiatry. 2017,;32:726–733. doi: 10.1002/gps.4514. [DOI] [PubMed] [Google Scholar]
- 16.Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the Confusion Assessment Method. Ann Intern Med. 1990;113:941–948. doi: 10.7326/0003-4819-113-12-941. [DOI] [PubMed] [Google Scholar]
- 17.Bickel H. Deutsche Version der Confusion Assessment Method (CAM) zur Diagnose eines Delirs. Psychosomatik und Konsiliarpsychiatrie. 2007;1:224–228. [Google Scholar]
- 18.Hughes CP, Berg L, Danziger WL, Coben LA, Martin RL. A new clinical scale for the staging of dementia. Br J Psychiatry. 1982,;140:566–572. doi: 10.1192/bjp.140.6.566. [DOI] [PubMed] [Google Scholar]
- 19.Morris JC. The Clinical Dementia Rating (CDR): Current version and scoring rules. Neurology. 1993,;43:2412–2414. doi: 10.1212/wnl.43.11.2412-a. [DOI] [PubMed] [Google Scholar]
- 20.Woolf C, Slavin MJ, Draper B, et al. Can the Clinical Dementia Rating Scale identify mild cognitive impairment and predict cognitive and functional decline? Dement Geriatr Cogn Disord. 2016,;41:292–302. doi: 10.1159/000447057. [DOI] [PubMed] [Google Scholar]
- 21.Goldstein H, Browne H, Rasbash J. Partitioning variation in multilevel methods. Understanding Statistics. 2002,;1:223–231. [Google Scholar]
- 22.Alzheimer Europe. Prevalence of dementia in Europe. www alzheimer-europe org/Research/European-Collaboration-on-Dementia/Prevalence-of-dementia/Prevalence-of-dementia-in-Europe (last accessed on 9 February 2018) [Google Scholar]
- 23.Donner A, Klar N. Arnold. London: 2000. Design and analysis of cluster randomized trials in health research. [Google Scholar]
- 24.Dean AG, Sullivan KM, Soe MM. OpenEpi: Open Source Epidemiologic Statistics for Public Health, Version 23.1. www.OpenEpi.com (last accessed on 15 June. 2018) [Google Scholar]
- 25.Lesnoff M, Lancelot R. aod: Analysis of overdispersed data R package version 1.3. http://cran.r-project.org/package=aod (last accessed on 15 June. 2018) [Google Scholar]
- 26.Deutsche Alzheimer Gesellschaft. Die Häufigkeit von Demenzerkrankungen. Informationsblatt 1. www.deutsche-alzheimer.de/fileadmin/alz/pdf/factsheets/infoblatt1_haeufigkeit_demenzerkrankungen_dalzg.pdf (last accessed on 9 February 2018) [Google Scholar]
- 27.Motzek T, Werblow A, Schmitt J, Marquardt G. Administrative Prävalenz und Versorgungssituation der Demenz im Krankenhaus Eine versorgungsepidemiologische Studie basierend auf GKV-Daten sächsischer Versicherter. Gesundheitswesen. 2018 doi: 10.1055/s-0043-125071. doi: 10.1055/s-0043-125071. [DOI] [PubMed] [Google Scholar]
- 28.Siddiqi N, House AO, Holmes JD. Occurrence and outcome of delirium in medical in-patients: a systematic literature review. Age Ageing. 2006,;35:350–364. doi: 10.1093/ageing/afl005. [DOI] [PubMed] [Google Scholar]
- 29.Bail K, Berry H, Grealish L, et al. Potentially preventable complications of urinary tract infections, pressure areas, pneumonia, and delirium in hospitalised dementia patients: retrospective cohort study. BMJ Open. 2013,;3 doi: 10.1136/bmjopen-2013-002770. e002770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pimouguet C, Rizzuto D, Fastbom J, Lagergren M, Fratiglioni L, Xu W. Influence of incipient dementia on hospitalization for primary care sensitive conditions: a population-based cohort study. J Alzheimers Dis. 2016,;52:213–222. doi: 10.3233/JAD-150853. [DOI] [PubMed] [Google Scholar]
- 31.Tolppanen A-M, Taipale H, Purmonen T, Koponen M, Soininen H, Hartikainen S. Hospital admissions, outpatient visits and healtcare costs of community-dwellers with Alzheimer´s disease. Alzheimers Dement. 2015,;11:955–963. doi: 10.1016/j.jalz.2014.10.005. [DOI] [PubMed] [Google Scholar]
- 32.Erkinjuntti T, Wikström J, Palo J, Autio L. Dementia among medical inpatients Evaluation of 2000 consecutive admissions. Arch Intern Med. 1986;146:1923–1926. [PubMed] [Google Scholar]
- 33.Erkinjuntti T, Autio L, Wikström J. Dementia in medical wards. J Clin Epidemiol. 1988,;41:123–126. doi: 10.1016/0895-4356(88)90086-8. [DOI] [PubMed] [Google Scholar]
- 34.Bickel H, Cooper B, Wancata J. Psychische Erkrankungen von älteren Allgemeinkrankenhauspatienten: Häufigkeit und Langzeitprognose. Nervenarzt. 1993,;64:53–61. [PubMed] [Google Scholar]
- 35.Kolbeinsson H, Jónsson A. Delirium and dementia in acute medical admissions of elderly patients in Iceland. Acta Psychiatr Scand. 1993,;87:123–127. doi: 10.1111/j.1600-0447.1993.tb03342.x. [DOI] [PubMed] [Google Scholar]
- 36.Wancata J, Benda N, Hajji M, Lesch OM, Müller C. Psychiatric disorders in gynaecological, surgical and medical departments of general hospitals in an urban and a rural area of Austria. Soc Psychiatry Psychiatr Epidemiol. 1996,;31:220–226. doi: 10.1007/BF00785771. [DOI] [PubMed] [Google Scholar]
- 37.Arolt V, Driessen M, Dilling H. Psychische Störungen bei Patienten im Allgemeinkrankenhaus. Dtsch Arztebl. 1997,;94 A-1354-8. [Google Scholar]
- 38.Travers C, Byrne G, Pachana N, Klein K, Gray L. Prospective observational study of dementia and delirium in the acute hospital setting. Intern Med J. 2013,;43:262–269. doi: 10.1111/j.1445-5994.2012.02962.x. [DOI] [PubMed] [Google Scholar]
- 39.Timmons S, Manning E, Barrett A, et al. Dementia in older people admitted to hospital: a regional multi-hospital and observational study of prevalence, associations and case recognition. Age Ageing. 2015,;44:993–999. doi: 10.1093/ageing/afv131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Reynish EL, Hapca SM, De Souza N, Cvoro V, Donnan PT, Guthrie B. Epidemiology and outcomes of people with dementia, delirium, and unspecified cognitive impairment in the general hospital: prospective cohort study of 10,014 admissions. BMC Med. 2017;15 doi: 10.1186/s12916-017-0899-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E1.Hendlmeier I, Bickel H, Hessler JB, et al. Demenzsensible Versorgungsangebote im Allgemeinkrankenhaus: Repräsentative Ergebnisse aus der General Hospital Study (GHoSt) Z Gerontol Geriatr. 2018;51:509–516. doi: 10.1007/s00391-017-1339-7. [DOI] [PubMed] [Google Scholar]
- E2.Royal College of Psychiatrists. www.rcpsych.ac.uk/PDF/NATIONAL%20REPORT%20-%20Full%20Report%201201122.pdf (last accessed on 26 June 2018) London: 2011. Report of the National Audit of Dementia Care in General Hospitals. [Google Scholar]
- E3.Bayerisches Staatsministerium für Umwelt und Gesundheit. Betreuung von demenzkranken Menschen im Allgemeinkrankenhaus: 20 Empfehlungen für Krankenhausträger zur verbesserten Versorgung von Patienten mit kognitiven Einschränkungen. www.bkg-online.de/media/file/14766.17-2016-135-dl.pdf (last accessed on 26 June 2018) 2011 [Google Scholar]
- E4.Kirchen-Peters S, Herz-Silvestrini D. Herausforderung Demenz im Krankenhaus: Ergebnisse und Lösungsansätze aus dem Projekt Dem-i-K Saarbrücken. www.saarland.de/dokumente/thema_sozialversicherung/DEMIK_NEU_WEB.pdf (last accessed on 26 June 2018) 2014 [Google Scholar]
- E5.Timmons S, O‘Shea E, O‘Neill D, et al. Acute hospital dementia care: results from a national audit. BMC Geriatr. 2016,;16 doi: 10.1186/s12877-016-0293-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E6.Kratz T, Heinrich M, Schlauß E, Diefenbacher A. The preventing of postoperative confusion - a prospective intervention with psychogeriatric liaison on surgical wards in a general hospital. Dtsch Arztebl Int. 2015;112:289–296. [Google Scholar]
- E7.Deutsche Alzheimer Gesellschaft. Informationsbogen für Patienten mit einer Demenz bei Aufnahme ins Krankenhaus. www.deutsche-alzheimer.de/fileadmin/alz/broschueren/infobogen_krankenhaus.pdf (last accessed on 26 June 2018) [Google Scholar]
- E8.Deutsches Netzwerk für Qualitätsentwicklung in der Pflege (ed.) Expertenstandard „Beziehungsgestaltung in der Pflege von Menschen mit Demenz“. Osnabrück. Schriftenreihe des Deutschen Netzwerks für Qualitätsentwicklung in der Pflege. 2018 [Google Scholar]
- E9.Elvish R, Burrow S, Cawley R, et al. ‚Getting to Know Me‘: The development and evaluation of a training programme for enhancing skills in the care of people with dementia in general hospital settings. Aging Ment Health. 2014;18:481–488. doi: 10.1080/13607863.2013.856860. [DOI] [PubMed] [Google Scholar]
- E10.Elvish R, Burrow S, Cawley R, et al. ‚Getting to Know Me‘: The second phase roll-out of a staff training programme for supporting people with dementia in general hospitals. Dementia. 2018;17:96–109. doi: 10.1177/1471301216634926. [DOI] [PubMed] [Google Scholar]
- E11.Isfort M, Klostermann J, Gehlen D, Siegling B. Deutsches Institut für angewandte Pflegeforschung e.V. (dip) Köln: 2014. Pflege-Thermometer 2014 Eine bundesweite Befragung von leitenden Pflegekräften zur Pflege und Patientenversorgung von Menschen mit Demenz im Krankenhaus. [Google Scholar]
- E12.Singler K, Thomas C. HELP - Hospital Elder Life Program - ein multimodales Interventionsprogramm zur Delirprävention bei älteren Patienten. Internist (Berl) 2017;58:125–131. doi: 10.1007/s00108-016-0181-0. [DOI] [PubMed] [Google Scholar]
- E13.Kratz T. The diagnosis and treatment of behavioral disorders in dementia. Dtsch Arztebl Int. 2017;114:447–454. doi: 10.3238/arztebl.2017.0447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E14.Gurlit S, Möllmann M. How to prevent perioperative delirium in the elderly? Z Gerontol Geriatr. 2008;41:447–452. doi: 10.1007/s00391-008-0020-6. [DOI] [PubMed] [Google Scholar]
- E15.Hsieh TT, Yue J, Oh E, et al. Effectiveness of multicomponent nonpharmacological delirium interventions: a meta-analysis. JAMA Intern Med. 2015,;175:512–520. doi: 10.1001/jamainternmed.2014.7779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E16.Goldberg SE, Bradshaw LE, Kearney FC, et al. Care in specialist medical and mental health unit compared with standard care for older people with cognitive impairment admitted to general hospital: randomised controlled trial (NIHR TEAM trial) BMJ. 2013;347 doi: 10.1136/bmj.f4132. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMETHODS
Sampling
This sample was chosen to achieve representativeness for the two German federal states Baden-Württemberg and Bavaria where more than 23 million people (29% of the total German population) live. A multi-step sampling strategy was used. First, the general hospitals of both federal states were arranged in a random sequence, contacted in this sequence and invited to participate. In each of the hospitals willing to cooperate, five wards and one substitute ward were selected. All patients aged 65 or older who were inpatients on the selected wards on the day of survey and met the inclusion criteria were invited to participate in the study. Where the number of participants was less than 40, patients of a substitute ward were additionally included in the analysis.
For an estimation accuracy of ± 2%, a sample size of at least 1200 patients is required, assuming a prevalence of dementia of 15%. Based on this lower limit, it was necessary to ensure participation of at least 30 hospitals, each with 40 or more surveyed patients.
The following inclusion and exclusion criteria were defined for hospitals, wards and patients, respectively: General hospitals were identified based on the respective hospital plan of each of the two federal states. In Bavaria, they were the hospitals of the first, second and third level of care (10) and in Baden-Württemberg, they were the approved hospitals with at least two departments at one hospital location (11). According to this definition, altogether 301 general hospitals were found in the two federal states. Specialty hospitals and entirely private hospitals as well as rehabilitation and day or night clinics were excluded from sampling. For survey-economic reasons, 92 general hospitals with less than 150 inpatient beds were excluded (30.6%), leaving a basic set of 209 general hospitals and university hospitals.
In hospitals with less than 150 beds, a relatively small proportion of the patients is treated on an inpatient basis. Although nationwide, they make up 42.7% of the general hospitals, they only account for 9.0% of the days of inpatient care (1). Since in Southern Germany the proportion of smaller hospitals is with 30.6% even below the nationwide level of 42.7%, it can be assumed that no relevant bias is introduced by their exclusion.
On the ward level, intensive care units and isolation wards were excluded. Since in geriatric hospitals detailed studies on dementia have already been conducted (12, 13), this branch of medicine was excluded as were neurology and psychiatry where dementia usually is a primary diagnosis, not a comorbidity.
On the patient level, inclusion criteria comprised a minimum age of 65 years and the written consent to participation by the patient or their legal representative. Patients were excluded if they:
The study protocol was approved by the Ethics Committee of the Faculty of Medicine of the Technical University of Munich (TUM) on 21 March 2014 (No. 66/14). The study is registered in the German Clinical Trials Register (DRKS) under DRKS00006028. The written consent to participation in the study was obtained from the patients or their legal representatives following informed consent discussion about the content and aims of this study and provision of written information material.
Data collection
Five trained research assistants carried out the survey from June 2014 to end of May 2015. All assistants were qualified by having graduated in psychology, gerontology or social work and had previous research or clinical experience in gerontopsychiatry. Prior to the start of the study, the research assistants were extensively trained in the use of the survey instruments and application of the diagnostic criteria. All interviews were reviewed for completeness, plausibility and conformity of the assessment with the diagnostic criteria by the Senior Researchers of the project. During regular case conferences, the diagnostic assessments were discussed. Any disagreements were resolved by consensus decision.
Data were obtained in standardized form by personal examination of the patient, an interview with the responsible nurse and documentation of study-relevant information from medical records. In unclear cases, additional interviews were conducted with relatives or the legal representative of the patient (efigure1).
Because all patients of a ward were usually examined on the same survey date, it was possible to complete data collection on the selected wards of a hospital within 1 week. Examinations were only conducted on business days and from Monday to Friday in the sequence in which the wards had been randomly selected.
Cognitive status was assessed using a bedside test battery, comprising the screening tool 6-Item Cognitive Impairment Test (14) and established tests to assess primary and secondary memory, verbal fluency, attention and executive functions (15). Global severity of cognitive impairment was assessed using the Clinical Dementia Rating (CDR) scale (18). With this instrument, the degree of impairment in six domains of performance (memory, orientation, judgment & problem solving, community affairs, home & hobbies, and personal care) is externally assessed on a 5-point scale and a global rating derived:
After having examined the patient, the interviewer rated the severity of the cognitive disorders using the CDR scale.
The nurse responsible for the patient was asked about:
If the nursing staff was not yet familiar enough with a patient or if the cognitive status was unclear, the patient’s relative or caregiver was contacted to obtain further information. In addition, we retrieved from the patient records, besides information about the reason for seeking treatment and about the medication, study-relevant information, such as known diagnoses of dementia and delirium or other signs of cognitive disorders.
Taking into account all available information, patients were assigned to one of four categories of diagnosis (efigure 1). Dementia was diagnosed using DSM-IV criteria. Besides memory impairments, these include at least one other higher cortical function and one impairment of social functioning or of the ability to cope with everyday life.
Delirium was diagnosed using the Confusion Assessment Method (CAM) (16, 17) which is based on the criteria inattention, altered level of consciousness and disorganized thinking. CAM requires these symptoms to have an acute onset or fluctuating course over the day. Based on the reports of the nursing staff, relatives and caregivers and taking into account information from the patient records, we differentiated between delirium with dementia and delirium without severe preexisting cognitive deficits.
A rating of 0.5 on the CDR scale was regarded as a mild cognitive disorder (19). This score indicates an impairment in the transition zone between normal-for-age cognitive performance and mild dementia which is characterized by a high risk of developing dementia later in life. A prospective study, comparing older individuals with normal cognitive performance to patients with this level of cognitive impairment, found that the latter had a 25-times increased risk of conversion to dementia (20).
Patients with no impairments, scoring 0 on the CDR scale, make up the category of persons without cognitive impairments.
Statistical analysis
The correlation of patients among each other within the 33 included hospitals (Intracluster Correlation Coefficient, ICC) was estimated using the method described by Goldstein et al. (21). As recommended for binary variables (23), statistical analyses were performed using logistic Generalized Estimation Equation (GEE) models to ensure intracluster correlation was taken into account. For point prevalence rate estimates, models without influencing variable (intercept-only) were adapted to the data in order to ensure that the cluster structure is taken into account when estimating confidence intervals. For calculating associations between demographic variables, departments, reasons for seeking treatment, and other relevant variables with the endpoint dementia, the respective characteristics were used as the independent variable and the binary endpoint dementia as the dependent variable in the models (eTables 1 and 2). Analyses were performed with and without adjustment for the a priori defined variables age and sex. When adjusting for the effect of age, the age in years (two decimal places) at the time of examination was used as the independent variable. The few values missing for certain analyses were not replaced. The results exclusively refer to patients where complete data for the respective analysis were available. Data analyses were performed using OpenEpi (24), the R package (25) and SPSS 25 for Windows, Version 25.
Hospital diagnoses obtained from the patient records on survey day were classified according to the ICD-10 major diagnostic categories. Using this strategy, it was possible to identify associations between dementia and the reasons for seeking treatment. For each of the ICD major diagnostic categories, each starting with a capital letter, a binary variable with the value 0 for absence of a diagnosis and 1 for the presence of at least one diagnosis was created. ICD major diagnostic categories found at a rate of less than 2.0% were not included in the further analyses. Associations between diagnostic category and dementia were calculated with and without adjustment for age and sex (etable 2). If the adjusted odds ratio indicated with a probability of more than 95% an increased or reduce occurrence of the respective diagnostic category among patients with dementia, it was assessed based on more detailed ICD diagnoses which specific diagnoses of this diagnostic category had contributed most to the differences. These noses are named in the text as less or more common reasons for seeking treatment.
Indirect standardization was performed to assess whether the prevalence of dementia in the hospital differed from that in the general population when age and sex structure of hospital patients were taken into account. For comparison of dementia prevalence among hospital patients, the age- and sex-specific rates according to EuroCoDe (22) were used which are based on European field studies. In the eFigures 3–5, the age-specific prevalence rates found in the hospital setting are compared with the expected rates from the general population. The indirect standardized rate ratio (IRR) expresses by which factor the prevalence observed in the hospital setting differs from the prevalence in the general population of the same age.
were moribund
were in a critical condition according to medical staff where interviewing and examination could have a detrimental effect
had been isolated because of an infectious disease
did not speak German.
Global score 0 connotes no cognitive disorders or impairments in everyday life
Global score 0.5 is characterized by constant forgetfulness and very mild or questionable impairment of judgement and coping with domestic and external tasks. Orientation and personal care remain intact.
Global score 1 indicates cognitive impairments of a severity equivalent to mild dementia, with difficulties in performing basic activities of daily life.
Global score 2 indicates moderate dementia. It is associated with severe memory loss, impaired orientation, inability to perform activities outside the home and the need for assistance with everyday activities, such as getting dressed and washing.
Global score 3 indicates severe dementia with almost complete loss of memory and orientation as well as full dependence on third-party care.
impairment of cognitive performance of the patient
changes in cognition and consciousness during the hospital stay
functional impairments
behavioral abnormalities.