Abstract
Background
As of 2011, among 250 administrative districts in Korea, 54 districts did not have obstetrics and gynecology clinics or hospitals providing prenatal care and delivery services. The Korean government designated 38 regions among 54 districts as “Obstetric Care Underserved Areas (OCUA).” However, little is known there are any differences in pregnancy, prenatal care, and outcomes of women dwelling in OCUA compared to women in other areas. The purposes of this study were to compare the pregnancy related indicators (PRIs) and adequacy of prenatal care between OCUA region and non-OCUA region.
Methods
Using National Health Insurance database in Korea from January 1, 2012 to December 31, 2014, we constructed the whole dataset of women who terminated pregnancy including delivery and abortion. We assessed incidence rate of 17 PRIs and adequacy of prenatal care. All indicators were compared between OCUA group and non-OCUA group.
Results
The women dwelling in OCUA regions were more likely to get abortion (4.6% in OCUA vs. 3.6% in non-OCUA) and receive inadequate prenatal care (7.2% vs. 4.4%). Regarding abortion rate, there were significant regional differences in abortion rate. The highest abortion rate was 10.3% and the lowest region was 1.2%. Among 38 OCUA regions, 29 regions' abortion rates were higher than the national average of abortion rate (3.56%) and there were 10 regions in which abortion rates were higher than 7.0%. In addition, some PRIs such as acute pyelonephritis and transfusion in obstetric hemorrhage were more worse in OCUA regions compared to non-OCUA regions.
Conclusion
PRIs are different according to the regions where women are living. The Korean government should make an effort reducing these gaps of obstetric cares between OCUA and non-OCUA.
Keywords: Medically Underserved Area, Rural Area, Abortion, Prenatal Care, Preterm Delivery, National Health Insurance
Graphical Abstract
INTRODUCTION
Medically underserved area (or physician shortage area) is defined as geographic area with insufficient health resources such as manpower and/or facilities for the society.1 In terms of manpower, medically underserved area can be classified into area without any doctors and area with shortage of doctors.2 The former one (without any doctors) may be rare in developed countries, but obstetrically underserved areas without any obstetric doctors are present in Korea.3,4 As of 2011, 54 districts did not have obstetrics and gynecology clinics or hospitals providing prenatal care and delivery services, among 250 administrative districts in Korea. The Korean government designated 38 regions among the 54 districts as “Obstetric Care Underserved Areas (OCUA).”3,4 Residents in medically underserved are in trouble because of limited access to medical care. Actually, there have been numerous reports on adverse medical outcome in medically underserved area, and the presence of specialist in medical care is known to be the key point in improved outcome.5,6,7 The extreme form of medically underserved area, which is the OCUA without any obstetric doctor in Korea, can be a real threat to pregnant women. More serious thing is that these districts are mostly located in rural or remote areas. The Korean government recognizes OCUA could be a serious public health concern.
The limited access to obstetric care has been reported to be associated with adverse obstetric outcomes such as maternal mortality, even in developed countries.8,9 However, there is a paucity of information on any differences in pregnancy, prenatal care, and outcomes of women dwelling in OCUA compared to women in other areas. The purposes of this study were to investigate pregnancy related indicators (PRIs) and to compare the PRIs according to OCUA region and non-OCUA region.
METHODS
Data source
In order to grasp the whole scale of pregnancy, prenatal care, and delivery among all of mothers in Korea, we used the National Health Insurance Service (NHIS) database. NHIS is the sole healthcare insurer in Korea that provides health insurance to all Korean citizens. NHIS has been accumulating the all medical records including personal information based on medical claim data submitted from healthcare providers.
Operational definitions of mother, abortion, delivery, and maternal complications
In this study, mothers refer women who aged fewer than forty-five at the time of terminating pregnancy. Abortion, type of delivery, and maternal complications were defined based on the International Classification of Diseases-10th Revision and Electronic Data Interchange (EDI) code (Table 1).
Table 1. The definition of abortion, delivery, and maternal (obstetrical) complications.
| Variables | ICD-10 code | |
|---|---|---|
| Abortion | O00–O08 (O00–O089) | |
| Delivery | ||
| Cesarean section | O82 (O820–O829), O842 | |
| Vaginal delivery | O80 (O800–O809), O81 (O810–O815), O83 (O830–O839), O840, O841 | |
| Maternal (obstetrical) complications | ||
| Preeclampsia | O14 (O140–O149) | |
| Eclampsia | O15 (O150–O159) | |
| Gestational hypertension | O13 | |
| Gestational diabetes mellitus | O244 | |
| Placenta previa | O44 (O440–O441) | |
| Abruptio placentae | O45 (O450–O459) | |
| Obstructed labor | O64–O66 (O640–O669) | |
| Preterm delivery | O601 | |
| Still birth | O364 | |
| APN | O23 (O230–O239), N10, N12, N159 | |
| Perineal laceration | O702, O703 | |
| Obstetric hemorrhage | O67 (O670–O679), O72 (O720–O723) | |
| Fetal stress | O68 (O680–O689) | |
| Transfusion | X1001, X1002, X2011, X2012, X2021, X2022, X2031, X2032, X2131, X2132, X2091, X2092, X2515, X2512 | |
| Admission to ICU | AJ110, AJ210, AJ120, AJ220, AJ130, AJ230, AJ140, AJ240, AJ150, AJ250, AJ100, AJ200, AJ300, AJ180, AJ280, AJ380 | |
| Uterine artery embolization | M6644 | |
| Cesarean hysterectomy | R4507, R4508, R4509, R4510, R5001, R5002 | |
ICD = International Classification of Diseases, APN = acute pyelonephritis, ICU = intensive care unit.
Patient selection and data processing
Using the NHIS database, we selected women who terminated pregnancy including delivery and abortion from January 1, 2013 to December 31, 2013. Total subjects were 371,341 women; and we divided the mothers into mother group living in rural area (4,239) and others (367,102). Then we connected each person's medical record and personal information from NHIS database from 2012 and 2014.
Also, we assessed incidence rates of 17 PRIs, including abortion, acute pyelonephritis (APN), preeclampsia, eclampsia, gestational hypertension, gestational diabetes, placenta previa, placental abruption, obstructed labor, preterm delivery, still birth, and obstetric hemorrhage. We also calculated incidences of transfusion, intensive care unit admission, uterine artery embolization, and hysterectomy. All PRIs were compared OCUA group to non-OCUA group.
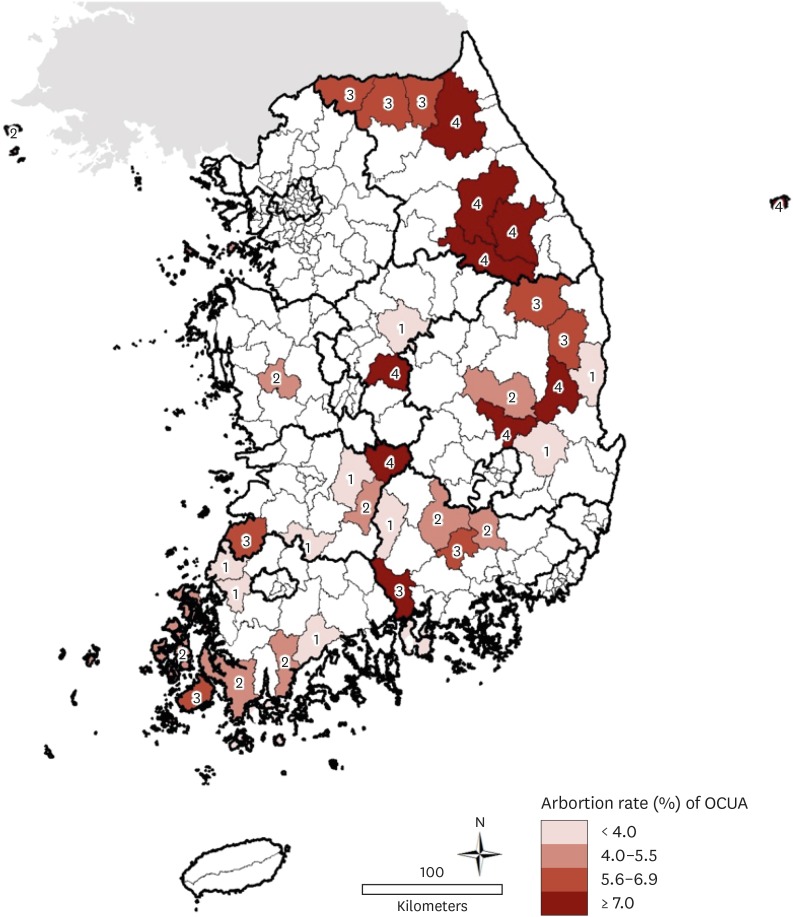
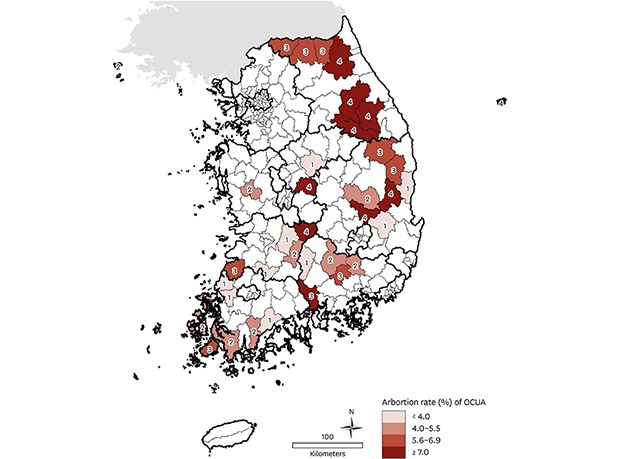
We assessed the adequacy of prenatal care using the Kessner Index which is based on the total number of visits for prenatal cares during pregnancy; if a pregnant woman saw a doctor more than 9 occasions, it would be evaluated as ‘adequate,’ if visited 5–8 occasions ‘intermediate,’ and if they visited less than 4 times it was evaluated as ‘inadequate.’10 The level of income was categorized as three levels using the national health insurance premium as a proxy indicator; high level (upper 25% of premium), intermediate level (middle 50%), and low level (lower 25%). According to abortion rate, we categorized each OCUA regions from level 1 to level 4—level 1 (less than 4.0%), level 2 (4.0%–5.5%), level 3 (5.5%–7.0%), and level 4 (more than 7.0%).
Statistical analysis
Frequency analyses were performed to describe pregnancy outcomes, prenatal care utilization, and maternal complications. Pearson's χ2 test and Student's t-test were conducted to examine the difference between OCUA and non-OCUA group and other groups. All the analyses were completed using SAS, version 10.2 (SAS Institute Inc., Cary, NC, USA). All statistical tests were two-sided and a P value < 0.05 was considered statistically significant.
Ethics statement
The present study was exempted from approval from the institutional Review Board (IRB No. E-1504-075-665) because it deals with anonymous public data, provided by NHIS and Statistics Korea. Therefore, we could not identify the subjects of the study, and there was no need for obtaining informed consent from the patient in the present study.
RESULTS
General characteristics and main pregnancy outcomes
In demographic characteristics, mothers were more likely to live in OCUA and to affiliate low income family when compared to other non-OCUA group (Table 2). In pregnancy outcomes, mothers in OCUA also showed higher rates of abortion and stillbirth when compared to control (non-OCUA mothers).
Table 2. General characteristics.
| Variables | No. of women (%) | |||
|---|---|---|---|---|
| OCUA | Non-OCUA | Total | ||
| Total | 4,239 (1.14) | 367,102 (98.86) | 371,341 (100.0) | |
| Age | ||||
| Mean ± SD | 31.55 ± 4.34 | 31.50 ± 4.03 | 31.5 ± 4.19 | |
| Areaa | ||||
| Metropolitan | 238,416 (64.95) | 238,416 (64.20) | ||
| City | 361 (8.52) | 109,054 (29.71) | 109,415 (29.50) | |
| Rural | 3,878 (91.48) | 19,632 (5.35) | 23,510 (6.30) | |
| Type of insurancea | ||||
| NHI | 4,194 (98.9) | 364,985 (99.40) | 369,179 (99.30) | |
| MA | 45 (1.10) | 2,117 (0.60) | 2,162 (0.70) | |
| Level of Incomeb | ||||
| High (upper 25%) | 1,292 (30.48) | 62,835 (17.12) | 64,127 (17.26) | |
| Medium (25%–75%) | 2,690 (63.46) | 244,922 (66.72) | 247,612 (66.68) | |
| Low (lower 25%) | 257 (6.06) | 59,345 (16.17) | 59,602 (16.05) | |
OCUA = obstetric care underserved areas, SD = standard deviation, NHI = National Health Insurance, MA = medical aid.
aP < 0.05 calculated by χ2 test or t-test between rural area and other groups; bLevel of income was categorized as high level (upper 25% of premium), intermediate level (middle 50%), and low level (lower 25%) based on their national health insurance premium.
Prenatal care utilization and its adequacy
OCUA mothers less utilized prenatal care than other non-OCUA groups. Their average occasion of prenatal care was 11.99 while that of other group was 13.74. More serious thing was that 2.34% of OCUA mothers had never received prenatal care during the whole pregnant period. Regarding adequacy of prenatal care, OCUA mothers receiving inadequate prenatal care was significantly higher (7.24%) than other groups (4.39%) (Table 3).
Table 3. Prenatal care utilization and its adequacy.
| Variables | No. of women (%) | ||||
|---|---|---|---|---|---|
| OCUA | Non-OCUA | Total | |||
| Total | 4,239 | 367,102 | 371,341 (100.0) | ||
| Frequency of prenatal care | |||||
| Mean ± SDa | 11.99 ± 4.68 | 13.74 ± 4.72 | 12.86 ± 4.70 | ||
| Frequencya | |||||
| 0 | 99 (2.34) | 5,879 (1.60) | 5,978 (1.61) | ||
| 1 | 49 (1.16) | 2,933 (0.80) | 2,982 (0.80) | ||
| 2 | 51 (1.20) | 2,544 (0.69) | 2,595 (0.69) | ||
| 3 | 44 (1.04) | 2,369 (0.65) | 2,413 (0.65) | ||
| 4 | 64 (1.51) | 2,379 (0.65) | 2,443 (0.66) | ||
| Adequacy of prenatal carea | |||||
| Adequate (≥ 9) | 3,246 (76.57) | 321,109 (87.47) | 324,355 (87.35) | ||
| Intermediate (5–8) | 686 (16.18) | 29,889 (8.14) | 30,575 (8.23) | ||
| Inadequate (≤ 4) | 307 (7.24) | 16,104 (4.39) | 16,411 (4.42) | ||
We assessed the adequacy of prenatal care using the Kessner Index which is based on the total number of visits for prenatal cares during pregnancy; if a pregnant woman saw a doctor more than 9 occasions, it would be evaluated as ‘adequate,’ if visited 5–8 occasions ‘intermediate,’ and if they visited less than 4 times it was evaluated as ‘inadequate.’
OCUA = obstetric care underserved areas, SD = standard deviation.
aP < 0.05 calculated by χ2 test or t-test between rural area group and other groups.
Maternal complications and Abortion rate according to each 38 OCUA regions
Women in OCUA had higher rate of maternal complications such as APN during pregnancy and transfusion than those in non-OCUA (P < 0.05) (Table 4). Table 5 and Fig. 1 show the abortion rate according to 38 OCUA regions. The highest region's abortion rate was 10.3% and the lowest region was 1.2%. Among 38 OCUA regions, 29 regions' abortion rates were higher than the national average of abortion rate (3.56%) and there were 10 regions which abortion rates were higher than 7.0%.
Table 4. Abortion, stillbirth, and maternal (obstetrical) complications.
| Maternal (obstetrical) complications | No. of women (%) | ||||
|---|---|---|---|---|---|
| OCUA (4,239) | Non-OCUA (367,102) | Total (371,341) | P value | ||
| Totala | 682 (16.09) | 62,266 (16.77) | 62,948 (16.95) | ||
| Cesarean section | 1,424 (35.38) | 124,337 (35.29) | 125,761 (33.86) | 0.988 | |
| Stillbirth | 21 (0.50) | 1,720 (0.47) | 1,741 (0.46) | 0.065 | |
| Abortionb | 193 (4.55) | 13,061 (3.56) | 13,254 (3.56) | < 0.001 | |
| APN during pregnancyb | 249 (5.87) | 17,640 (4.81) | 17,889 (4.81) | < 0.001 | |
| Preeclampsia | 15 (0.35) | 911 (0.25) | 926 (0.24) | 0.170 | |
| Eclampsia | 1 (0.02) | 44 (0.01) | 45 (0.01) | 0.495 | |
| Gestational hypertension | 18 (0.42) | 1,154 (0.31) | 1,172 (0.31) | 0.203 | |
| Gestational diabetes mellitusb | 210 (4.95) | 25,762 (7.02) | 25,972 (6.99) | < 0.001 | |
| Placenta previa | 22 (0.52) | 1,540 (0.42) | 1,562 (0.42) | 0.320 | |
| Placental abruption | 0 (0.0) | 103 (0.03) | 103 (0.02) | 0.275 | |
| Obstructed labor | 5 (0.12) | 459 (0.13) | 464 (0.12) | 0.897 | |
| Preterm delivery | 54 (1.27) | 5,165 (1.41) | 5,219 (1.40) | 0.690 | |
| Spontaneous preterm delivery | 52 (1.23) | 4,913 (1.34) | 4,965 (1.33) | 0.590 | |
| Indicated preterm delivery | 2 (0.05) | 252 (0.07) | 254 (0.06) | 0.576 | |
| Obstetric hemorrhage | 3 (0.07) | 288 (0.08) | 291 (0.08) | 0.860 | |
| Transfusionb | 136 (3.21) | 8,368 (2.28) | 8,504 (2.29) | < 0.001 | |
| Uterine artery embolization | 4 (0.09) | 564 (0.15) | 568 (0.15) | 0.326 | |
| Cesarean hysterectomy | 1 (0.02) | 121 (0.03) | 122 (0.03) | 0.738 | |
| Admission to ICU | 11 (0.26) | 614 (0.17) | 625 (0.17) | 0.145 | |
OCUA = obstetric care underserved areas, ICU = intensive care unit.
aThis number is the actual number of pregnant women, thus the total number could be less than the sum of the total eight obstetrical complications; bP < 0.05 calculated by χ2 test or t-test between OCUA and Non-OCUA regions.
Table 5. Abortion rates according to each 38 OCUA regions.
| OCUA | Abortion rate, % | Level for underserved area |
|---|---|---|
| Jeongseon-gun | 10.3 | 4 |
| Inje-gun | 8.1 | |
| Pyeongchang-gun | 8.1 | |
| Boeun-gun | 7.9 | |
| Yeongwol-gun | 7.7 | |
| Cheongsong-gun | 7.5 | |
| Muju-gun | 7.5 | |
| Ulleung Island | 7.4 | |
| Gunwi-gun | 7.4 | |
| Hadong-gun | 7.0 | 3 |
| Hwacheon-gun | 6.9 | |
| Uiryeong-gun | 6.9 | |
| Yanggu-gun | 6.3 | |
| Jindo-gun | 6.2 | |
| Cheongwon-gun | 6.1 | |
| Bonghwa-gun | 5.9 | |
| Yeongyang-gun | 5.7 | |
| Gochang-gun | 5.6 | |
| Jangheung-gun | 5.0 | 2 |
| Shinan-gun | 4.9 | |
| Jangsu-gun | 4.9 | |
| Cheongyang-gun | 4.9 | |
| Ongjin-gun | 4.9 | |
| Hapcheon-gun | 4.4 | |
| Changryeong-gun | 4.3 | |
| Haenam-gun | 4.3 | |
| Uiseong-gun | 4.3 | |
| Goesan-gun | 3.7 | 1 |
| Yeongcheon-si | 3.6 | |
| Wando-gun | 3.5 | |
| Yeongdeok-gun | 3.3 | |
| Yeonggwang-gun | 3.2 | |
| Sunchang-gun | 3.1 | |
| Hamyang-gun | 3.1 | |
| Namhae-gun | 3.0 | |
| Boseong-gun | 2.8 | |
| Jinan-gun | 2.7 | |
| Hampyeong-gun | 1.2 |
OCUA = obstetric care underserved areas.
Fig. 1. Regional abortion rates according to 38 OCUA regions.
OCUA = obstetric care underserved areas.
DISCUSSION
The principal findings of the current study are 1) women dwelling in OCUA regions were more likely to get abortion and receive inadequate prenatal care; 2) women in OCUA regions had more obstetric complications such as APN and transfusion compared to non-OCUA regions.
As the obstetric hospitals in rural area had decreased in recent decades, pregnant women in rural area can be in limited access to obstetric unit. Hung et al.11 reported that small obstetric unit closures are more common in rural area than in urban areas in the Unites States and raised the concerns about continuity of rural maternal care. In Korea, the closure of obstetric unit for delivery service is more dramatic, and the number of hospitals providing delivery services had dropped to 777 units in 2014 from 1,311 units in 2011, rating 41% reduction.12 The most frequently cited reasons for obstetric closure are the low volume of deliveries, financial vulnerability due to low delivery cost, and legal problems.13 According to the Korean government report, the closure rate of obstetric unit is more common in small volume hospitals, which are more prevalent form of hospitals in rural areas.12 This phenomenon resulted in 54 districts without any obstetrics and gynecology clinics or hospitals providing prenatal care and delivery services, among 250 administrative districts in Korea. Among these 54 districts, 38 districts are those in which 30% or more populations (15–49 age) cannot reach to any obstetrics and gynecology clinics (more than 50 case per year) AND in which 30% or under cases using hospitals timely within 60 minutes, and the Korean government designated these 38 districts as OCUA.2,3,4
The mothers in OCUA should travel to get access to obstetric care, such as prenatal care and labor/delivery services. The increased distance between home and obstetric unit is associated not only with financial, social, and psychological stress, but also with increased risk for obstetric complications.8 Rapid access to hospital is most important in the emergent management of obstetric complications,14 and long distance between home and hospital may affect the medical decision in complicated pregnancies. Therefore, the poor accessibility contributes to social inequalities in the context of medical care.15 In maternal health, the frequency of low birthweight increased in area where hospitals closed obstetric services in rural areas.8 Furthermore, the density of obstetric doctor (maternal-fetal medicine specialist) was inversely associated with maternal mortality, proving the importance of qualified care in maternal health.16
In the current study, we confirmed that some obstetric outcomes are different according to the regions where women are living. First of all, the frequency of prenatal care and the proportion of adequate prenatal visit were lower in mothers of OCUA regions. As adequate prenatal visit is crucial in maternal health,17 national policies should focus on the improvement of adequate prenatal visit in OCUA regions. Second, the abortion rate was higher in OCUA regions. Furthermore, the abortion rate was highest in underserved area. The difference in abortion rate is very important information for the Korean government to set the priority for intervening OCUA regions: 9 districts more than 7.5% in abortion rate. Now, the Korean government should seek the reason what factors are affecting on differences in abortion rate among OCUA groups; and based on the results, they will set up what to do for these 9 regions. Third, the risk of APN during pregnancy and transfusion (as an indicator of obstetric hemorrhage) was higher in OCUA regions. Urinary tract infection is common complication in medically underserved pregnant women, and inadequate prenatal care was a risk factor of urinary tract infection in teenage mothers, who are another representative of medical inequality.16,18 Obstetric hemorrhage is one of the most important reasons for maternal mortality. Although some of acute postpartum hemorrhage may be unpreventable, adequate prenatal care may reduce the need for transfusion, by prenatal iron supplementation, adequate care of labor and delivery, or planned delivery in high risk pregnancies. In contrast to other obstetric complications, the rate in gestational diabetes was lower in OCUA. This may suggest the demographic differences between people in OCUA and those in non-OCUA, such as body mass index or physical activities, but the data on these demographic characteristics are not available in our study population. However, this lower rate of gestational diabetes may represent the lower detection rate of gestational diabetes, by inadequate prenatal visit in OCUA regions. In addition, several obstetric complications such as placenta previa, placental abruption, and preterm delivery were not different between OCUA and non-OCUA regions. The similar rate of preterm delivery between OCUA and non-OCUA regions is interesting finding, because preterm delivery is known to be increased in specific social conditions, such as poverty, working long hours, and low socioeconomic status.
The strength of the current study is that the data is from NHIS database. The NHIS is the only healthcare insurer covering all people in Korea, and the database is well-organized national database. Even though we use NHIS database, we have some limitation in this study. First, there is possible to include data which origin address of mother is not consistent with actual address when she visits hospital, maybe resulting in overestimation of the OCUA regions. Second, the number of prenatal cares was estimated from NHIS database, and the prenatal care which was not paid by NHIS may not be counted in the number of prenatal cares. Third, the abortion was diagnosed by ICD-10 codes (O00–O08) including heterogeneous type of abortion, such as spontaneous and artificial abortion and ectopic pregnancies. Forth, in this study, defining obstetric hemorrhage was very difficult because NHIS database did not provide the amount of transfusion and the severity of hemorrhage. Nevertheless, to conduct this study, we had to define obstetric hemorrhage based on the diagnosis of O67 (O670–O679), O72 (O720–O723). But the frequency of obstetric hemorrhage was 1.17%, lower than previously reported in other studies. To overcome this problem and to depict real frequency of hemorrhage during labor and delivery, we added other variables such as transfusion, uterine artery embolization, and cesarean hysterectomy. Lastly, this research was based on cross-sectional descriptive study design so that we could not reveal what factors affecting these differences. For example, we have just revealed that abortion rate of OCUA regions were higher than non-OCUA regions but we did not analyze what factors were associated with this phenomenon. In addition, maternal (obstetrical) complications were simply compared between OCUA and non-OCUA. In order to deal with these issues, further study is needed.
However, this study showed meaningful information that obstetric outcomes were different according to the regions where women are living. The Korean government should make an effort reducing these gaps of obstetric cares between OCUA and non-OCUA
Footnotes
Funding: This study was supported by a research fund from the National Health Insurance Service in Korea (HIRE 15-39).
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Kwak MY, Lee SM, Eun SJ, Lee JY, Kim Y.
- Data curation: Kwak MY, Lee TH.
- Formal analysis: Kwak MY, Lee TH.
- Investigation: Eun SJ, Lee JY.
- Methodology: Lee JY.
- Writing - original draft: Kwak MY, Lee SM.
- Writing - review & editing: Kwak MY, Lee SM, Lee TH, Eun SJ, Lee JY, Kim Y.
References
- 1.MeSH term definition of medically underserved area. [Updated 2017]. [Accessed May 28, 2017]. https://www.ncbi.nlm.nih.gov/mesh/?term=physician+shortage+area.
- 2.Na BJ, Lee JY, Kim HJ. Are public health physicians still needed in medically underserved rural areas in Korea? Medicine (Baltimore) 2017;96(19):e6928. doi: 10.1097/MD.0000000000006928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Na BJ, Kim HJ, Lee JY. An early stage evaluation of the supporting program for obstetric care underserved areas in Korea. J Korean Med Sci. 2014;29(6):764–770. doi: 10.3346/jkms.2014.29.6.764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim JE, Na BJ, Kim HJ, Lee JY. Why women living in an obstetric care underserved area do not utilize their local hospital supported by Korean government for childbirth. Asian Nurs Res. 2016;10(3):221–227. doi: 10.1016/j.anr.2016.07.001. [DOI] [PubMed] [Google Scholar]
- 5.Nadpara PA, Madhavan SS, Tworek C. Disparities in lung cancer care and outcomes among elderly in a medically underserved state population-a cancer registry-linked database study. Popul Health Manag. 2016;19(2):109–119. doi: 10.1089/pop.2015.0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McGinigle KL, Kalbaugh CA, Marston WA. Living in a medically underserved county is an independent risk factor for major limb amputation. J Vasc Surg. 2014;59(3):737–741. doi: 10.1016/j.jvs.2013.09.037. [DOI] [PubMed] [Google Scholar]
- 7.Selim AM, Mazurek JA, Iqbal M, Wang D, Negassa A, Zolty R. Mortality and readmission rates in patients hospitalized for acute decompensated heart failure: a comparison between cardiology and general-medicine service outcomes in an underserved population. Clin Cardiol. 2015;38(3):131–138. doi: 10.1002/clc.22372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sontheimer D, Halverson LW, Bell L, Ellis M, Bunting PW. Impact of discontinued obstetrical services in rural Missouri: 1990–2002. J Rural Health. 2008;24(1):96–98. doi: 10.1111/j.1748-0361.2008.00115.x. [DOI] [PubMed] [Google Scholar]
- 9.Pilkington H, Blondel B, Carayol M, Breart G, Zeitlin J. Impact of maternity unit closures on access to obstetrical care: the French experience between 1998 and 2003. Soc Sci Med. 2008;67(10):1521–1529. doi: 10.1016/j.socscimed.2008.07.021. [DOI] [PubMed] [Google Scholar]
- 10.Kessner DM. Infant Death: an Analysis by Maternal Risk and Health Care. Washington, DC: Institute of Medicine, National Academy of Sciences; 1973. [Google Scholar]
- 11.Hung P, Kozhimannil KB, Casey MM, Moscovice IS. Why are obstetric units in rural hospitals closing their doors? Health Serv Res. 2016;51(4):1546–1560. doi: 10.1111/1475-6773.12441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.2011 National Health Insurance Statistical Yearbook. Seoul: National Health Insurance Corporation and Health Insurance Review and Assessment Service; 2012. [Google Scholar]
- 13.The Evaluation of Supporting Methods for Reliable Antenatal Care and Birth for Pregnant Women in Obstetrically Underserved Area. Seoul: Korean Association of Obstetricians and Gynecologists; Sejong: Ministry of Health and Welfare; 2013. [Google Scholar]
- 14.Viisainen K, Gissler M, Hartikainen AL, Hemminki E. Accidental out-of-hospital births in Finland: incidence and geographical distribution 1963–1995. Acta Obstet Gynecol Scand. 1999;78(5):372–378. [PubMed] [Google Scholar]
- 15.Chishty V, Packer C. Rising emergency admissions. Age, distance from a hospital, and level of deprivation are influential factors. BMJ. 1995;310(6983):867. doi: 10.1136/bmj.310.6983.867a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sullivan SA, Hill EG, Newman RB, Menard MK. Maternal-fetal medicine specialist density is inversely associated with maternal mortality ratios. Am J Obstet Gynecol. 2005;193(3 Pt 2):1083–1088. doi: 10.1016/j.ajog.2005.05.085. [DOI] [PubMed] [Google Scholar]
- 17.Lee SH, Lee SM, Lim NG, Kim HJ, Bae SH, Ock M, et al. Differences in pregnancy outcomes, prenatal care utilization, and maternal complications between teenagers and adult women in Korea: a nationwide epidemiological study. Medicine (Baltimore) 2016;95(34):e4630. doi: 10.1097/MD.0000000000004630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leppälahti S, Gissler M, Mentula M, Heikinheimo O. Is teenage pregnancy an obstetric risk in a welfare society? A population-based study in Finland, from 2006 to 2011. BMJ Open. 2013;3(8):e003225. doi: 10.1136/bmjopen-2013-003225. [DOI] [PMC free article] [PubMed] [Google Scholar]