Abstract
Objective
The aim of this study was to define a quantitative parameter to indicate which cases of plantar fasciitis will benefit from local corticosteroid injection or ESWT and to compare the efficacy of two different treatment modalities.
Methods
Seventy patients (mean age: 49.10; range: 41–58) with chronic plantar fasciitis unresponsive to conservative treatment for 3 months were treated with either betamethasone injection or extracorporeal shock wave therapy (ESWT). Correlation between AOFAS scores, fascia thickness, duration of symptoms, age and calcaneal spur length were assessed.
Results
Degree of fascial thickening (mean 4.6 mm for all patients) did not influence baseline AOFAS scores (r = −0.054). Plantar fascia thickness significantly decreased in both groups after treatment (1.2 mm for steroid, 1.2 mm for ESWT) (p < 0.01 for both groups). Percentage of change in AOFAS scores (68% for steroid and 79% for ESWT, p = 0.069) and fascial thickness (24% for steroid and 26% for ESWT, p = 0.344) were similar between two groups. Functional recovery was not correlated with baseline fascial thickness (r = 0.047) or degree of fascial thinning after treatment (r = −0.099). Percentage of change in AOFAS scores was correlated only with baseline AOFAS scores (r = −0.943).
Conclusions
Plantar fascia thickness increases significantly in plantar fasciitis and responds to treatment. Both ESWT and betamethasone injection are effective in alleviating symptoms and reducing plantar fascia thickness in chronic plantar fasciitis. However, the only predictive factor for functional recovery in terms of AOFAS scores is patients' functional status prior to treatment. Measuring of plantar fascia is not helpful as a diagnostic or prognostic tool and MRI imaging should be reserved for differential diagnosis.
Level of evidence
Level III, Therapeutic study.
Keywords: Plantar fasciitis, ESWT, Prognosis, Steroid injection, AOFAS score
Introduction
Plantar fasciitis is the most common cause of inferior heel pain.1 It is estimated that 10% of the general population will develop plantar fasciitis over a lifetime.2, 3 People with reduced ankle dorsiflexion, pes planus, BMI > 30 kg/m2, and individuals who spend the majority of their workday on their feet are at increased risk for the development of plantar fasciitis.1, 2 Plantar fascia is an important stabilizer of the longitudinal arch of the foot and,4, 5, 6, 7 it is prone to repetitive excessive loads at the proximal insertion, leading to fibrosis or degeneration, hence the common usage of the term “plantar fasciopathy”.5, 6
Diagnosis is based on clinical examination. The most typical symptom is a sharp pain around the insertion of plantar fascia near the medial tubercle of the calcaneus, which is worse with first steps in the morning or after periods of inactivity.1, 6, 8 Imaging may be necessary in cases with chronic or extended pain. Patients with heel pain are likely to have a thickened plantar fascia, with linear bands or lobules of increased signal and associated fluid collection on MRI. Some authors consider thickness values > 4 mm diagnostic of plantar fasciitis.5, 7, 9, 10
It is generally a self-limited disease, with more than 80% of patients having resolution of symptoms within 12 months, regardless of therapy.1 However, it may run a prolonged course and cause serious impact on life quality, causing 65% of patients to require repeating doctor visits during this time. Most common treatments are NSAID and stretching, followed by physical therapy, heel pads, arc supports, night splints, extracorporeal shock wave therapy (ESWT), cushioned-sole footwear; surgery is rarely needed and may be complicated with persistent pain, pseudoaneurism, transfer metatarsalgia and collapse of the longitudinal arch.2
Even though some patient characteristics, such as plantar fascia thickness, BMI, age, psychological status, DM, presence of diffuse hyperemia on bone scintigrams, and presence of inflammatory disorders have been proposed to have influence on patient outcome, results have been inconclusive.4, 6, 11 Among these characteristics, plantar fascia thickness is of particular interest, as it is been shown to increase significantly in plantar fasciitis, to respond to treatment, and can be analyzed quantitatively.6, 10, 12, 13, 14
We hypothesize that plantar fascia thickness is correlated with the functional outcome of plantar fasciitis patients, and it is predictive for which of the ESWT or the steroid injection treatments the patients will benefit more from.
Material and methods
This prospective cohort study was performed between years 2012 and 2014. Seventy patients presenting to orthopedics clinic with chronic plantar fasciitis unresponsive to conservative treatment were treated with either single intra-lesional steroid injection or 3 sessions of ESWT. We have performed simple randomization by drawing a lot before assigning patients to treatment groups. The diagnosis of chronic plantar fasciitis was made on history and clinical examination. Patients had MRI of their feet taken prior to treatment and any differential diagnoses were ruled out. Subjects were followed prospectively and were asked to complete AOFAS hindfoot score.
The subjects gave informed consent and the study was approved by the Institutional Ethics Committee. Inclusion criteria were: 1) To have symptoms of plantar fasciitis for more than 3 months not responding to conservative treatment. 2) Being over 18 years old. 3) To have showed up at the follow-up visit scheduled for weeks six from the beginning of treatment. Patients who had prior steroid injection or ESWT were excluded. Conservative treatment was defined as the use of NSAID, heel pad or stretching exercises for a minimum period of 8 weeks.
Sample size was selected to detect an effect size of 61% between the groups with respect to the primary variable, AOFAS hindfoot score, a type I error of 0.05 and a power of 0.80, and was based on a pilot study with 20 patients. Data from the pilot study (mean score for steroid = 55 and mean score for ESWT = 51, SD = 6.5) showed that 34 patients were required in each group, but 35 were included to compensate for possible dropouts.
Seven mg betamethasone was injected near the medial tubercle of the calcaneus as described by Genc et al,6 with the patient in prone position and knee flexed at 90°. ESWT was performed with NT10 Novalith (NovaMEDTEK, Ankara, Turkey), an electrohydraulic-type device. The energy intensity applied ranged from 10 to 16 kV, 1500 pulses for each session at weekly intervals for 3 consecutive weeks. All patients tolerated the treatment intensity and no ecchymosis or other important adverse effect was observed. All patients were instructed to continue eccentric stretching exercises and were evaluated at 6 weeks from the time of steroid injection or last ESWT session. AOFAS scores and MRI of treated feet were obtained.
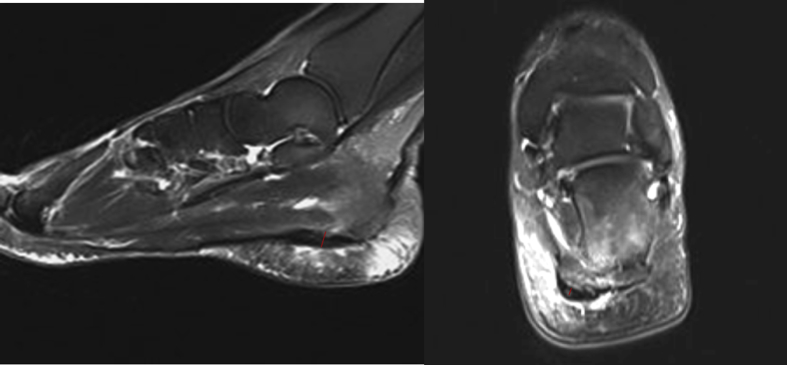
The MRI images were reviewed by a senior radiologist blinded to the study. The thickness of the plantar fascia was measured at the calcaneal origin where the fascia is thickest using both sagittal and coronal T2-weighted sequences (3-mm-thick sections). Highest value at any of the planes was recorded as the maximum plantar fascia thickness (Fig. 1). Heel spur length was measured on T1-weighted sagittal images.
Fig. 1.
Measuring the fascial thickness on two planes using T2-weighted sequences with 3 mm slices. Fascial thickness at the calcaneal origin is 5.14 mm in the sagittal section and 5.04 mm in the coronal section.
All statistical analyses were performed with IBM SPSS ver. 22.0. Descriptive data were expressed as median (minimum–maximum) or proportions as indicated. Shapiro Wilk test was used as normality test. Continuous variables were compared using Mann–Whitney U test when the data were not normally distributed. Paired data were analyzed using Paired t-test and Wilcoxon signed rank test when data were not normally distributed. Correlations between variables were tested using Spearman correlation coefficient. A p-value < 0.05 was considered as significant.
Results
Patient demographics, baseline AOFAS scores and fascia thicknesses, calcaneal spur length and duration of symptoms prior to treatment are outlined in Table 1. Patients in the corticosteroid group had significantly higher baseline AOFAS scores (p = 0.02). No patients had abnormal MRI findings supporting differential diagnosis.
Table 1.
Patient demographics and preoperative and postoperative findings.
| Treatment method | Age | Duration of symptoms (months) | Spur length (mm) | Baseline AOFAS | Final AOFAS | Baseline fascial thickness (mm) | Final fascial thickness (mm) |
|---|---|---|---|---|---|---|---|
| Total N: 70 | 49.10 (41–58) | 8.46 (4–12) | 5.44 (2.20–9.81) | 53.10 (40–69) | 90.26 (75–100) | 4.64 (2.7–7.0) | 3.48 (1.60–5.50) |
| Steroid N: 35 | 49.40 (41–58) | 8.71 (6–12) | 5.85 (2.40–9.71) | 55.17 (44–69) | 91.09 (75–100) | 4.74 (3.0–7.0) | 3.59 (2.0–5.5) |
| ESWT N: 35 | 48.80 (41–58) | 8.20 (4–12) | 5.04 (2.20–9.81) | 51.03 (40–67) | 89.43 (80–100) | 4.55 (2.7–6.3) | 3.36 (1.6–5.5) |
| p | 0.693 | 0.426 | 0.09 | 0.02∗ | 0.537 |
∗P < 0.05.
Baseline AOFAS scores were higher in the steroid injection group.
Following treatment, patients in both groups had significantly higher AOFAS scores at week six compared to baseline values (p < 0.01) (Table 2). Similarly, plantar fascia thickness significantly decreased in both groups (p < 0.01) (Table 2). Percentage of change in AOFAS scores and fascial thickness were similar between two treatment methods (p = 0.069 and 0.344 respectively) (Table 3).
Table 2.
Significance of changes in AOFAS scores and plantar fascia thickness following treatment.
| Treatment method | Baseline AOFAS | Final AOFAS | p | Baseline fascial thickness (mm) | Final fascial thickness (mm) | p |
|---|---|---|---|---|---|---|
| Steroid | 55.17 (44–69) | 91.09 (75–100) | 0.01∗ | 4.74 (3.0–7.0) | 3.59 (2.0–5.5) | 0.01∗ |
| ESWT | 51.03 (40–67) | 89.43 (80–100) | 0.01∗ | 4.55 (2.7–6.3) | 3.36 (1.6–5.5) | 0.01∗ |
∗p < 0.05.
Both treatment groups showed significant functional recovery and reduction in plantar fascia thickness.
Table 3.
Between group comparison of percentage of changes in AOFAS scores and plantar fascia thickness.
| Steroid | ESWT | p | |
|---|---|---|---|
| Change in AOFAS | 0.6798 | 0.7866 | 0.069 |
| Change in fascial thickness | −0.2385 | −0.2634 | 0.344 |
Percentage of change in AOFAS scores and fascia thickness was similar in both treatment groups.
Degree of fascial thickening did not influence baseline AOFAS scores (r = −0.054). Percentage of change in AOFAS scores after treatment was correlated only with baseline AOFAS scores (r = −0.943). Patients with lower AOFAS scores tended to show less improvement, regardless of therapy. Functional recovery was not correlated with baseline fascial thickness, degree of fascial thinning after treatment, age, duration of symptoms or length of calcaneal spur. When treatment groups were assessed separately, the only predictive factor was again baseline AOFAS scores (r = −0.902 for steroid and r = −0.941 for ESWT group). Increased age was positively correlated with baseline fascial thickness (r = 0.390) and calcaneal spur length (p < 0.01) (Table 4).
Table 4.
Correlation between variables.
| Baseline AOFAS | Baseline fascial thickness | Change in AOFAS | Change in fascial thickness | Spur length | Duration of symptoms | Age | ||
|---|---|---|---|---|---|---|---|---|
| Baseline AOFAS | −0.054 | −0.943b | 0.016 | 0.095 | 0.017 | −0.110 | Total steroid ESWT | |
| −0.236 | −0.902b | −0.075 | −0.023 | −0.013 | −3.81a | |||
| 0.031 | −0.941b | −0.023 | 0.137 | −0.033 | 0.054 | |||
| Baseline fascial thickness | −0.054 | 0.047 | 0.019 | 0.111 | 0.017 | 0.390b | Total steroid ESWT | |
| −0.236 | 0.149 | −0.060 | 0.042 | 0.077 | 0.338 | |||
| 0.031 | −0.058 | 0.067 | 0.173 | −0.075 | 0.406 | |||
| Change in AOFAS | 0.943b | 0.047 | −0.099 | −0.076 | −0.063 | 0.110 | Total steroid ESWT | |
| −0.902b | 0.149 | −0.027 | 0.079 | −0.074 | 0.341 | |||
| −0.941b | −0.058 | −0.125 | −0.185 | −0.002 | −0.111 | |||
| Change in fascial thickness | 0.016 | 0.019 | −0.099 | −0.047 | 0.074 | 0.107 | Total steroid ESWT | |
| −0.075 | −0.060 | −0.027 | −0.037 | 0.105 | 0.011 | |||
| −0.023 | 0.067 | −0.125 | −0.151 | −0.002 | 0.143 | |||
Functional recovery is dependent on only baseline AOFAS scores. Neither baseline values nor changes of plantar fascia thickness predict functional recovery. Older age is related to thicker plantar fascia.
Values expressed are r values of Spearman's correlation coefficient.
Correlation is significant at the 0.05 level.
Correlation is significant at the 0.01 level (2-tailed).
Between group differences and correlations remained the same after alignment domain of the AOFAS was discarded and questionnaires were scored on pain and function domains, with a maximum point of 90.
Discussion
The most common findings on MRI are: perifascial soft-tissue edema, changes in plantar fascia signal intensity, thickening of the plantar fascia, calcaneal bone marrow edema and calcaneal spur.15 Of these, thickening of the plantar fascia is a prominent and frequent manifestation of chronic plantar fasciitis. We have chosen to evaluate the correlation between fascial thickness and patient outcome because it can be assessed quantitatively and majority of the studies in the literature reports mean fascial thickness of plantar fasciitis patients to be over 4 mm.6, 10, 11, 12, 13, 14, 16 In our study, mean fascial thickness of patients was 4.70 mm prior to treatment (4.74 for steroid, 4.55 for ESWT group), well above the widely accepted threshold of 4 mms.10, 14 Our results are close to data from Liang et al's study12 where they have observed fascial thickness of 4.6 and 4.7 mm measured with USG. Genç et al6 have reported much higher values (6.2 mm), however, their patient sample was smaller and they have recruited only government officials who stand on their feet all day long. Thus, we believe our study is more representative of general population.
Following treatment with ESWT or corticosteroid injections, plantar fasciitis symptoms usually regress and patients tend to have functional recovery.13, 17, 18, 19, 20, 21, 22 In our study, patients in both groups had significantly higher AOFAS scores at week 6 compared to baseline values. In their study on plantar fasciitis patients refractory to treatment, Shetty et al21 have reported significant improvement in FADI and AOFAS scores at 3 months following triamcinolone injection. Say et al23 have reported similar improvement in AOFAS scores of patients with chronic fasciitis at 6 weeks and 6 months with methylprednisolone injection. Radwan et al22 have treated chronic cases symptomatic for at least 6 months with electrohydraulic ESWT and reported improvement at AOFAS scores beginning on week 3.
Reduction of plantar fascial thickness following corticosteroid injection or ESWT is another characteristic of plantar fasciitis.6, 12, 13 Similarly, plantar fascia thickness of both groups in our study decreased significantly following treatment. An exception is Ryan et al's study24 where fascial thickness did not change on week 6 and 12 following corticosteroid injection. Main difference between our study and Ryan et al's was that they used dexamethasone and involved only patients who stood on their feet more than five hours a day.
Even though literature exhibits the efficacy of both ESWT and corticosteroid injection to alleviate symptoms of plantar fasciitis and reduce fascial thickness, there remains a disagreement on which treatment modality is superior. Lack of a standardized study design, a variety of injectable forms of corticosteroids and differences in assessment of outcomes make direct comparison of the studies difficult. Our results indicate that ESWT and corticosteroid injection provide an equal percentage point of improvement from baseline AOFAS scores and fascial thickness. On the contrary, Mardani et al25 and Porter et al26 have favored corticosteroid over ESWT in terms of improvement of VAS scores; the patients enrolled in both studies had shorter duration of symptoms in contrast to the chronic cases in our study. Because repetitive trauma and subsequent inflammation are thought to occur early in the pathogenesis of the disease, it is likely that the patients in these studies benefit from anti-inflammatory effects of steroid more rather than tissue regenerating effects of ESWT.
Prognostic factors in plantar fasciitis are frequently analyzed to provide insight into the extent patients will benefit from different treatment modalities. Thickening of the plantar fascia is of particular interest, as it is a prominent and frequent manifestation of chronic plantar fasciitis and can be assessed quantitatively. Our results indicate that functional recovery (in terms of AOFAS scores) is not correlated with baseline fascial thickness, nor with the degree of fascial thinning after treatment, regardless of treatment modality. Our study is the first one in the literature to analyze the correlation between change in fascial thickness and improvement in AOFAS scores following ESWT or betamethasone treatment. Liang et al12 have conducted a similar study in which they have recruited patients with chronic plantar fasciitis and assessed patient outcome with VAS, SF-36 and Foot Function Index (FFI). They have utilized 3 weekly sessions of ESWT as in our study, but did not compare the results to an injection group. They have stated that thinner fascia predicted decreased pain, but not functional improvement, similar to our study. Chucpaiwong et al11 reported the results of high energy ESWT on large sample size of patients (246) with chronic plantar fasciitis and noted that fascial thickness and duration of symptoms do not affect the outcome of the treatment. Maki et al16 also concluded that Japanese Society for Surgery of the Foot Ankle Hindfoot scores at 6 months following ESWT were not correlated to pretreatment fascial thickness. On the contrary, Genç et al6 have reported a correlation between improvement in VAS scores and change in fascial change at month 1 and 6 following methylprednisolone injection. However, they have not clarified if their cases were chronic or not and they have included only government officials who stand on their feet all day long. Their mean duration of symptoms was 12 months, in contrast to the subjects in our study who had mean symptom duration of 8.7 months with 12 months maximum.
As with plantar fascia thickness, duration of symptoms and length of calcaneal spur also did not influence the functional outcome in this study, regardless of treatment modality. These results are comparable to Monto et al's18 study where they have found no correlation between duration of symptoms and improvement in AOFAS scores following methylprednisolone injection. Radwan et al22 have stated that patients who were symptomatic for less than 24 months had better AOFAS scores compared to those with more than 24 months of disease duration, following ESWT. Their results are hard to compare to ours, since maximum duration of symptoms in our study was 12 months. It is possible that with longer periods of disease, changes in the plantar fascia may become more intractable to treatment.
Main limitation of this study is that we have used only the AOFAS score to analyze patient outcome. Secondary tools such as VAS could have made a direct comparison with literature possible. However, the AOFAS questionnaire has a pain domain with 40 points which has substantial influence on the total score, reflecting the pain level. In order to have a better idea of the resolution of the symptoms, we have repeated the statistical analysis after excluding the alignment domain of the questionnaire and found that plantar fascia thickness still did not influence the outcome. Statistically significant difference in the pre-treatment AOFAS scores between two groups is another drawback of this study. This difference seems to occur with no clear reason. It is possible that heterogeneous distribution of certain patient characteristics like BMI or work habits not evaluated in this study might have caused this, however it cannot be proven with current data. Also, it is not clear if this difference was clinically relevant. We have used “the percentage of change in AOFAS scores” as the main parameter, not the final score itself, to avoid bias. Another limitation was the lack of a sham treatment group which would have been preferable since plantar fasciitis is a self-limited disease. However, because this was a cohort study but not a clinical trial, no such group existed.
Conclusion
In people with symptomatic plantar fasciitis, fascial thickness tends to increase, and the thickness is further correlated with older age. Functional recovery in terms of AOFAS scores is not correlated to baseline values or changes in thickness of plantar fascia when treating with betamethasone or ESWT. Only factor determining patient outcome in both treatment methods is patients' functional status prior to treatment. Measuring of plantar fascia is not helpful as a diagnostic or prognostic tool and MRI imaging should be reserved for differential diagnosis. Patients with worse symptoms should be informed about possible delays in recovery.
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
Contributor Information
Cenk Ermutlu, Email: cermutlu@hotmail.com.
Murat Aksakal, Email: draksakal@hotmail.com.
Ayşem Gümüştaş, Email: ogaygu@hotmail.com.
Güven Özkaya, Email: guvenozkaya@gmail.com.
Emrah Kovalak, Email: emrahkovalak@yahoo.com.
Yüksel Özkan, Email: dryukselozkan@gmail.com.
References
- 1.Buchbinder R. Clinical practice. Plantar fasciitis. N Engl J Med. 2004;350(21):2159–2166. doi: 10.1056/NEJMcp032745. [DOI] [PubMed] [Google Scholar]
- 2.Riddle D.L., Schappert S.M. Volume of ambulatory care visits and patterns of care for patients diagnosed with plantar fasciitis: a national study of medical doctors. Foot Ankle Int. 2004;25(5):303–310. doi: 10.1177/107110070402500505. [DOI] [PubMed] [Google Scholar]
- 3.Tong K.B., Furia J. Economic burden of plantar fasciitis treatment in the United States. Am J Orthop (Belle Mead NJ) 2010;39(5):227–231. [PubMed] [Google Scholar]
- 4.Frater C., Vu D., Van der Wall H. Bone scintigraphy predicts outcome of steroid injection for plantar fasciitis. J Nucl Med. 2006;47(10):1577–1580. [PubMed] [Google Scholar]
- 5.Zhu F., Johnson J.E., Hirose C.B., Bae K.T. Chronic plantar fasciitis: acute changes in the heel after extracorporeal high-energy shock wave therapy-observations at MR imaging. Radiology. 2005;234(1):206–210. doi: 10.1148/radiol.2341031653. [DOI] [PubMed] [Google Scholar]
- 6.Genç H., Saracoglu M., Nacir B., Erdem H.R., Kacar M. Long-term ultrasonographic follow-up of plantar fasciitis patients treated with steroid injection. Joint Bone Spine. 2005;72(1):61–65. doi: 10.1016/j.jbspin.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 7.Theodorou D.J., Theodorou S.J., Resnick D. MR imaging of abnormalities of the plantar fascia. Semin Musculoskelet Radiol. 2002;6(2):105–118. doi: 10.1055/s-2002-32357. [DOI] [PubMed] [Google Scholar]
- 8.Chang K.V., Chen S.Y., Chen W.S., Tu Y.K., Chien K.L. Comparative effectiveness of focused shock wave therapy of different intensity levels and radial shock wave therapy for treating plantar fasciitis: a systematic review and network meta-analysis. Arch Phys Med Rehabil. 2012;93(7):1259–1268. doi: 10.1016/j.apmr.2012.02.023. [DOI] [PubMed] [Google Scholar]
- 9.McNally E.G., Shetty S. Plantar fascia: imaging diagnosis and guided treatment. Semin Musculoskelet Radiol. 2010;14(3):334–343. doi: 10.1055/s-0030-1254522. [DOI] [PubMed] [Google Scholar]
- 10.McMillan A.M., Landorf K.B., Barrett J.T., Menz H.B., Bird A.R. Diagnostic imaging for chronic plantar heel pain: a systematic review and meta-analysis. J Foot Ankle Res. 2009;2:32. doi: 10.1186/1757-1146-2-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chuckpaiwong B., Berkson E.M., Theodore G.H. Extracorporeal shock wave for chronic proximal plantar fasciitis: 225 patients with results and outcome predictors. J Foot Ankle Surg. 2009;48(2):148–155. doi: 10.1053/j.jfas.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 12.Liang H.W., Wang T.G., Chen W.S., Hou S.M. Thinner plantar fascia predicts decreased pain after extracorporeal shock wave therapy. Clin Orthop Relat Res. 2007;460:219–225. doi: 10.1097/BLO.0b013e31804ffd19. [DOI] [PubMed] [Google Scholar]
- 13.Hammer D.S., Adam F., Kreutz A., Rupp S., Kohn D., Seil R. Ultrasonographic evaluation at 6-month follow-up of plantar fasciitis after extracorporeal shock wave therapy. Arch Orthop Trauma Surg. 2005;125(1):6–9. doi: 10.1007/s00402-003-0591-z. [DOI] [PubMed] [Google Scholar]
- 14.Tsai W.C., Chiu M.F., Wang C.L., Tang F.T., Wong M.K. Ultrasound evaluation of plantar fasciitis. Scand J Rheumatol. 2000;29(4):255–259. doi: 10.1080/030097400750041415. [DOI] [PubMed] [Google Scholar]
- 15.Ehrmann C., Maier M., Mengiardi B., Pfirrmann C.W., Sutter R. Calcaneal attachment of the plantar fascia: MR findings in asymptomatic volunteers. Radiology. 2014;272(3):807–814. doi: 10.1148/radiol.14131410. [DOI] [PubMed] [Google Scholar]
- 16.Maki M., Ikoma K., Imai K. Correlation between the outcome of extracorporeal shockwave therapy and pretreatment MRI findings for chronic plantar fasciitis. Mod Rheumatol. 2015;25(3):427–430. doi: 10.3109/14397595.2014.978526. [DOI] [PubMed] [Google Scholar]
- 17.Akşahin E., Doğruyol D., Yüksel H.Y. The comparison of the effect of corticosteroids and platelet-rich plasma (PRP) for the treatment of plantar fasciitis. Arch Orthop Trauma Surg. 2012;132(6):781–785. doi: 10.1007/s00402-012-1488-5. [DOI] [PubMed] [Google Scholar]
- 18.Monto R.R. Platelet-rich plasma efficacy versus corticosteroid injection treatment for chronic severe plantar fasciitis. Foot Ankle Int. 2014;35(4):313–318. doi: 10.1177/1071100713519778. [DOI] [PubMed] [Google Scholar]
- 19.Aqil A., Siddiqui M.R., Solan M., Redfern D.J., Gulati V., Cobb J.P. Extracorporeal shock wave therapy is effective in treating chronic plantar fasciitis: a meta-analysis of RCTs. Clin Orthop Relat Res. 2013;471(11):3645–3652. doi: 10.1007/s11999-013-3132-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gollwitzer H., Saxena A., DiDomenico L.A. Clinically relevant effectiveness of focused extracorporeal shock wave therapy in the treatment of chronic plantar fasciitis: a randomized, controlled multicenter study. J Bone Joint Surg Am. 2015;97(9):701–708. doi: 10.2106/JBJS.M.01331. [DOI] [PubMed] [Google Scholar]
- 21.Shetty V.D., Dhillon M., Hegde C., Jagtap P., Shetty S. A study to compare the efficacy of corticosteroid therapy with platelet-rich plasma therapy in recalcitrant plantar fasciitis: a preliminary report. Foot Ankle Surg. 2014;20(1):10–13. doi: 10.1016/j.fas.2013.08.002. [DOI] [PubMed] [Google Scholar]
- 22.Radwan Y.A., Mansour A.M., Badawy W.S. Resistant plantar fasciopathy: shock wave versus endoscopic plantar fascial release. Int Orthop. 2012;36(10):2147–2156. doi: 10.1007/s00264-012-1608-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Say F., Gürler D., İnkaya E., Bülbül M. Comparison of platelet-rich plasma and steroid injection in the treatment of plantar fasciitis. Acta Orthop Traumatol Turcica. 2014;48(6):667–672. doi: 10.3944/AOTT.2014.13.0142. [DOI] [PubMed] [Google Scholar]
- 24.Ryan M., Hartwell J., Fraser S., Newsham-West R., Taunton J. Comparison of a physiotherapy program versus dexamethasone injections for plantar fasciopathy in prolonged standing workers: a randomized clinical trial. Clin J Sport Med. 2014;24(3):211–217. doi: 10.1097/JSM.0000000000000021. [DOI] [PubMed] [Google Scholar]
- 25.Mardani-Kivi M., Karimi Mobarakeh M., Hassanzadeh Z. Treatment outcomes of corticosteroid injection and extracorporeal shock wave therapy as two primary therapeutic methods for acute plantar fasciitis: a prospective randomized clinical trial. J Foot Ankle Surg. 2015;54(6):1047–1052. doi: 10.1053/j.jfas.2015.04.026. [DOI] [PubMed] [Google Scholar]
- 26.Porter M.D., Shadbolt B. Intralesional corticosteroid injection versus extracorporeal shock wave therapy for plantar fasciopathy. Clin J Sport Med. 2005;15(3):119–124. doi: 10.1097/01.jsm.0000164039.91787.dc. [DOI] [PubMed] [Google Scholar]