Abstract
Objective
The aim of this study was to evaluate the clinical results of T-plate fixation and anterior sternoclavicular ligament repair in proximal clavicle fractures.
Methods
Between August 2013 and August 2016, a total 12 patients (10 men and 2 women; mean age: 44.1 ± 9.1 years (range, 25–59 years)) with unstable proximal clavicle fractures (Throckmorton, type D) were treated with T-type plate fixation, bridging the sternoclavicular joint, and anterior sternoclavicular ligament repair. Average operative time, associated injuries, postoperative complications, postoperative fracture healing time and follow-up time were recorded. The outcomes were evaluated with radiographic assessment, visual analog scale (VAS) pain score and Rockwood SCJ scoring system. All the patients were evaluated on postoperative 3rd, 6th, and 12th months.
Results
The average surgery time was 78.0 ± 8.47 minutes while fracture healing time was 4.51 ± 0.95 months. According to Rockwood SCJ scoring system, 9 cases (75%) were in excellent, 2 cases (16.7%) in good and 1 case (8.3%) in fair condition at 12 months follow-up. The average Rockwood SCJ score was 7.7 ± 0.75 preoperatively, 12.7 ± 0.86 by 3 months, 13.0 ± 0.73 by 6 months and 13.3 ± 0.49 by 12 months. The VAS pain score was 7.9 ± 1.15 (preoperative score), 3.4 ± 1.52 (3 months follow-up), 3.0 ± 1.32 (6 months follow-up) and 2.1 ± 1.07 (12 months follow-up). The VAS and Rockwood SCJ scores were significantly improved postoperatively (p < 0.05). There was no intraoperative complication, while one patient had redislocation of the sternoclavicular joint after implant removal.
Conclusion
T-type plate fixation with anterior sternoclavicular ligament repair might be a reliable and effective treatment method in unstable proximal clavicle fractures (type D) with few complications and satisfactory clinical results after 12 months follow-up.
Level of evidence
Level IV, therapeutic study.
Keywords: Clavicula fracture, Proximal, Sternoclavicular ligament, Plate, Internal fixation
Introduction
Treatment of proximal clavicula fractures remains a controversial topic in orthopedics. Proximal clavicula fractures have lower incidence than fractures of the middle third and distal clavicula fractures, accounting for approximately 5% of all clavicula fractures.1 Proximal clavicula fractures were first described by Robinson, who classified proximal fractures into 2 types, The majority of these cases could be successfully managed conservatively.2 However, type D (Comminuted fracture, proposed by Throckmorton) poses a challenging problem.3 The fracture can be significantly displaced as a result of strong forces-the sternocleidomastoid muscle pulls the medial fragment superiorly.4 Consequently, malunion and sternoclavicular joint pain are common with conservative treatment. In addition, the recover period can be prolonged with nonsurgical treatment. Therefore, surgical management of proximal clavicula fracture is an attractive alternative method.
Currently, there are no standard methods for managing unstable and comminuted fractures of proximal clavicula fractures, although various techniques have been described, including Kirschner wires and plates fixation.5 However, complications of these methods are relatively common, such as artery and vein injuries, sternoclavicular joint mobility.6
In order to overcome these problems, T-type plate fixation and anterior sternoclavicular ligament repair were applied in this study to assess the clinical therapeutic outcomes for the treatment of proximal clavicula fractures.
Patients and methods
Patients
Between August 2013 and August 2016, a total of 12 patients including 10 males and 2 females with unstable proximal clavicula fractures were treated with T-type plate fixation and anterior sternoclavicular ligament repair in our hospital for this prospective study (Table 1).
Table 1.
Gender/age (Years), Operative time (Min), Cause, Associated, Follow-up (Months) in 12 patients.
| Patient number | Gender/age (Years) | Operation time (Min) | Cause | Associated injury | Follow-up (Months) |
|---|---|---|---|---|---|
| 1 | M/42 | 79 | motor vehicle accident | No | 23 |
| 2 | M/37 | 68 | falling off bicycles | No | 12 |
| 3 | F/52 | 75 | motor vehicle accident | No | 24 |
| 4 | M/50 | 70 | falling off bicycles | No | 27 |
| 5 | M/25 | 72 | motor vehicle accident | No | 18 |
| 6 | M/48 | 82 | falling down | femoral neck fracture | 26 |
| 7 | M/41 | 80 | motor vehicle accident | No | 16 |
| 8 | M/40 | 68 | motor vehicle accident | No | 21 |
| 9 | F/59 | 78 | falling off bicycles | No | 30 |
| 10 | M/36 | 83 | falling down | calcaneus fracture. | 25 |
| 11 | M/51 | 98 | falling down | femoral neck fracture | 24 |
| 12 | M/49 | 84 | falling off bicycles | No | 27 |
Inclusion criteria and exclusion criteria
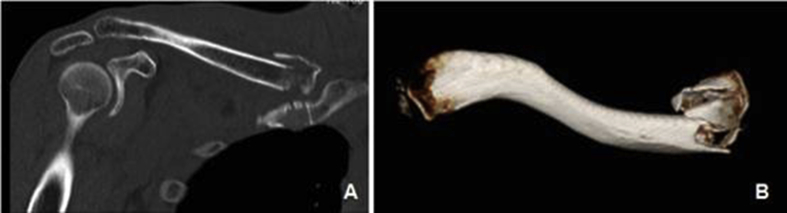
Selection criteria: (1) Type D fresh proximal clavicula fracture according to Throckmorton classification (Fig. 1); (2) the range of age was 25–60 years old; (3) patients without underlying diseases such as cardiac diseases. Exclusion criteria: (1) patho-logical fractures; (2)open fractures; (3) combined with injuries of blood vessels or nerves.
Fig. 1.
A: Preoperative CT scan; B: 3-dimentional CT of proximal clavicle fracture.
Standard protocol approvals and patient consents
All human studies were authorized by the Hospital Ethics Committee and conducted in accordance with the ethical standards. The written informed consent was obtained from all study patients.
Surgical procedures
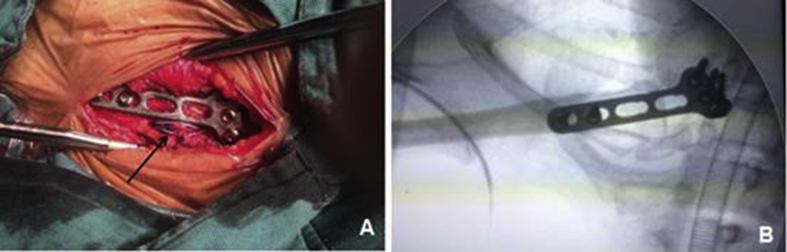
Surgery was performed under general anesthesia in the semi-sitting position. All patients underwent the same surgical procedure (T plate fixation combining with repairing anterior sternoclavicular ligament). A traverse small incision was made at the medium end of clavicula and sternoclavicular joint. The fracture was fully exposed and anatomically reduced by reduction forceps. After anatomic reduction, one 2-0 Ethibond Excel suture (Johnson Inc, New Brunswick, NJ, USA) was used to cross suture to repair anterior sternoclavicular ligament (Fig. 2A). Then a T-type locking plate (AO, Swiss) was bridged the sternoclavicular joint. A 2.5 mm limited depth drill was used to create 2 and 3 screw channels in proximal clavicula and manubrium sterni respectively to protect deep tissue (such as ascending and descending aorta, subclavicle aorta). Finally, the locking plate was fixed with screws. X-ray radiography below the shoulder was routinely used to examine the reduction of fracture and the location of plate (Fig. 2B). Moreover, similar medicine treatments before and after the operation were used to the patients.
Fig. 2.
A: repaired sternoclavicular ligament; B: Intraoperative X-ray showed good reduction of proximal clavicle fracture.
Postoperative management
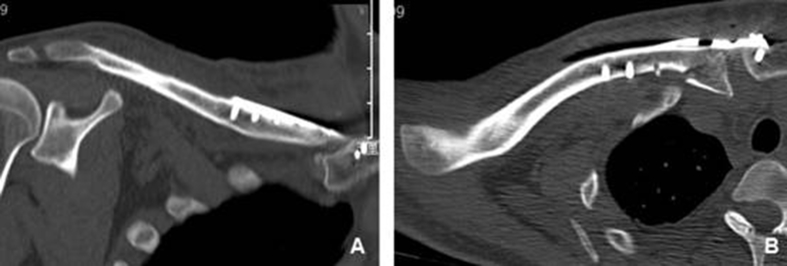
All 12 consecutive patients were enrolled in the study. All patients were treated with arm sling for 6 weeks after operation. In addition, 3 days after operation, patients were permitted to do passive anteflexion and abduction motion of shoulder joint under the guidance of physiotherapists, and the motion range could be increased gradually depending on the degree of pain and postoperative X-ray and CT scan images (Fig. 3, Fig. 4). However, the weight-bearing exercise was not allowed. The weight-bearing exercise was begun gradually after 6 weeks postoperatively. The postoperative follow-up visits were scheduled every four weeks until bone union and every 3 months after bone union.
Fig. 3.
Postoperative A-P X-rays.
Fig. 4.
Postoperative CT scan images.
Evaluation of therapeutic efficiency
The operative data were recorded and analyzed, including operation time, postoperative complications. The standards of bone union included no tenderness of the fracture ends when performing active exercises and weight-bearing activities on the clinical examinations, the formation of continuous callus and the disappearance of fracture line. The evaluation was made by an independent surgeon, who was blinded to the operation and implants. The improvement of subjective pain was assessed with visual analog scale (VAS) pain score, sternoclavicular joint function was assessed with the Rockwood scoring system of sternoclavicular joint (range: 0–15 points, best: 15) at the consecutive follow-up. In detail, Rockwood scoring system of sternoclavicular joint is categorized as follows: excellent (13–15), good (10–12), satisfactory (7–9), and fair (<7).7
Statistical analysis
All the statistical analysis was performed with SPSS version 18.0 software (SPSS Inc, Chicago, IL, USA). The values were presented as mean ± SD. The data were analyzed using the method of paired t-test and P < 0.05 was considered statistically significant.
Results
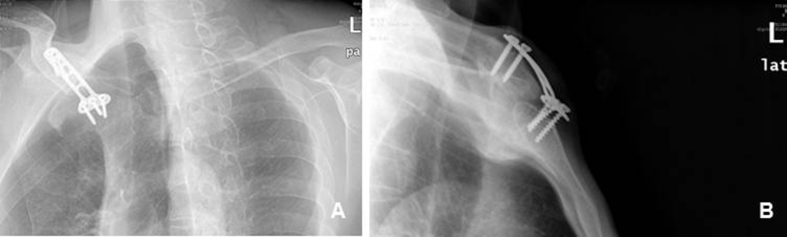
In this study, the average age was 44.1 ± 9.1 years (range, 25–59 years), 7 patients were in right proximal clavicular fracture and 5 in left. The causes of fractures included motor vehicle accident (5 cases), injuries of falling off bicycles (4 cases), falling down (3 cases) (Table 1). Two cases had unilateral femoral neck fracture, one patient had unilateral calcaneus fracture. The average operative time was 78.0 ± 8.47 min (range from 70 min to 98 min). All the cases were evaluated by the clinical function and imaging during the follow-up time (Fig. 5, Fig. 6, Fig. 7). The mean follow-up period was 22.7 months (range: 12–30 months). No nonunion case was found in all the patients. The mean time of bone union was 4.51 ± 0.95 months. Postoperative complications, such as infection, incision numbness, withdrawal of screws, were not found. The T-plates were removed after a mean time of 15 months after operation, no re-fracture occurred after removal. 11 cases were found with no reduction failure during postoperative follow-up, whereas 1 patient was revealed redislocation of the sternoclavicular joint after removing implants.
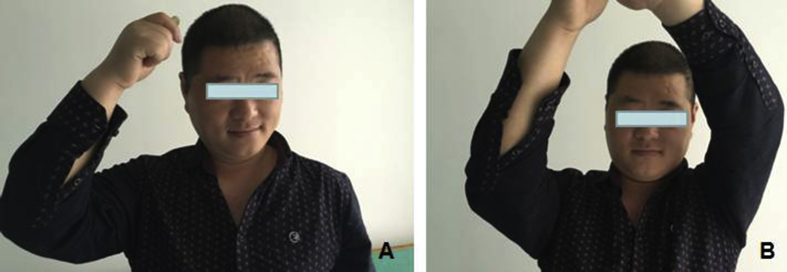
Fig. 5.
A: Postoperative A-P X-ray of the patient after 3 months follow up; B: lateral chest X-ray.
Fig. 6.
A, B: General views of the patients after 3 months follow up.
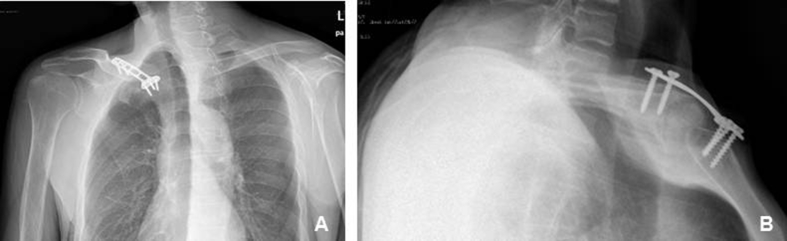
Fig. 7.
A, B: Postoperative A-P X-ray of the patient after 12 months follow up; B: lateral chest X-ray.
According to Rockwood SCJ scoring system, the average score was 7.7 ± 0.75 (preoperative score), 12.7 ± 0.86 (3 months follow-up), 13.0 ± 0.73 (6 months follow-up) and 13.3 ± 0.49 (12 months follow-up) (Table 2). Meanwhile, VAS pain score was 7.9 ± 1.15 (preoperative score), 3.4 ± 1.52 (3 months follow-up), 3.0 ± 1.32 (6 months follow-up) and 2.1 ± 1.07 (12 months follow-up). Statistics differences was showed between preoperative and 3,6,12 months follow-up score of Rockwood SCJ score and VAS pain score (p < 0.05). According to Rockwood SCJ scoring system, 75% patients showed excellent results, 16.7% showed good results, 8.3% showed fair results.
Table 2.
Rockwood scoring system of sternoclavicular joint of preoperation, 3,6,12 months follow-up.
| Patient number | Rockwood score (pre-op) | Rockwood score (3 months post-op) | Rockwood score (6 months post-op) | Rockwood score (12 months post-op) |
|---|---|---|---|---|
| 1 | 7 | 12 | 13 | 14 |
| 2 | 8 | 13 | 13 | 13 |
| 3 | 7 | 14 | 14 | 14 |
| 4 | 9 | 12 | 12 | 13 |
| 5 | 7 | 14 | 14 | 14 |
| 6 | 8 | 12 | 13 | 13 |
| 7 | 8 | 12 | 12 | 13 |
| 8 | 7 | 13 | 13 | 13 |
| 9 | 9 | 14 | 14 | 14 |
| 10 | 8 | 12 | 13 | 13 |
| 11 | 7 | 12 | 12 | 13 |
| 12 | 8 | 13 | 13 | 13 |
| Mean ± s | 7.7 ± 0.75 | 12.7 ± 0.86 | 13.0 ± 0.73 | 13.3 ± 0.49 |
| t | 15.08 | 17.23 | 21.48 | |
| P | 0.00 | 0.00 | 0.00 |
Data are presented as mean ± SD or number, pre-op: preoperation, post-op: postoperation.
Discussion
Proximal clavicula fractures are rare in clinical activities. In general, proximal clavicula fractures can be treated non-operatively except for comminuted proximal clavicula fractures.8, 9 However, there is no standard method to deal with comminuted proximal clavicula fracture. Proximal clavicula fracture was proposed by Robinson, Throckmorton refined the classification of proximal clavicula fractures, which were divided into five types.3 On the other hand, the sternoclavicular joint (SCJ) allows clavicle movement in three planes, the most common mechanism of SCJ injury is a direct blow to the shoulder from a fall or during sports-related activities.10 A direct lateral impact might have caused proximal clavicula fracture and disrupted the sternoclavicular ligaments according to a lever mechanism at the end of medial clavicula head.11, 12 Similar to other medial clavicula injuries, the proximal clavicula fractures and sternoclavicular ligaments injuries are difficult to detect through plain X-ray alone. Thus, early CT scanning is recommoned to confirm the injury types.
Proximal clavicula fractures (Throckmorton type A, B, C) were treated with nonsurgical methods.13 As for type D, Early techniques (kirschner wires, plate fixation) combined with high rates of relative complications.14, 15 Painful sternoclavicular joint and malunion frequently occurred with kirschner wires fixation. In addition, implant migration, irritation of screws were common, most researchers recommend the removal in all patients once fracture healing is confirmed.16, 17 On the other hand, the anterior sternoclavicular ligament was the most affected structure during retraction and depression.18 Many fixation techniques were available. According to previous researches, some techniques were used to repair capsuloligament through ligamentoplasty by means of natural or synthetic implants, internal fixation devices such as cerclage wirings, cannulated screws with subclavious muscle tendon.19, 20
T-type plate fixation with repairing anterior sternoclavicular ligament presented a challenge to surgeons because of anatomic complexity of the area (such as ascending and descending aorta, subclavicle aorta). However, the previous studies also indicated that it was safe and feasible to place three 2.7 mm screws on presternum.21
The indications of this technique include comminuted fracture of the medium end of clavicle, dislocation of sternoclavicular joint, revision operation (such as malunion or nonunion of proximal clavicula fracture).
The clinical results of 12 patients validate the use of T-type plate and repairing anterior sternoclavicular ligament for type D proximal clavicula fracture. Fracture union was observed in all cases, Statistics difference was showed between preoperative and 3,6,12 months follow-up Rockwood SCJ score and VAS pain score (p < 0.05).whereas 1 patient was revealed redislocation of the sternoclavicular joint after removing implants. Excellent clinical results were obtained in 9 cases, whereas 2 good results and 1 fair result were also showed in the cases.
The causes of redislocation of the sternoclavicular joint after removing implants in one case may be related to premature weight bearing in the patient due to incomplete healing of the sternoclavicular ligament and overweight of the patient (BMI = 29). We recommend preventive measures as follows: (1) reconstructing sternoclavicular ligament closely; (2) full suspension for ligament repair; (3) removing the internal fixation gently to avoid damage to the repair of the sternoclavicular ligament and articular capsule.
There are some limitations in the current study. Due to lack of randomized control group, the problems of whether our technique was better than other methods used in the treatment of unstable proximal clavicula fractures (type D) should be further studied in the future clinical practice. Besides, small sample size and short follow-up time were also the limitations in the study. Thereby, a study of large population and long follow-up time should be performed to assess the clinical values of our methods in the treatment of unstable proximal clavicula fractures. In addition, more biomechanical study of rotational and axial stability of the implant should be researched in the future.
Conclusion
T-type plate fixation with repairing anterior sternoclavicular ligament might be a reliable and effective treatment for unstable proximal clavicula fractures (type D) with few complications and satisfactory clinical effects in more than 12 months follow-up.
Acknowledgement
This study was supported by Ningbo science and technology enriching people project (No. 2015C50034) and Ningbo Natural Science Foundation (No. 2016A610142).
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
Contributor Information
Yi Zheng, Email: 260315546@qq.com.
Xin-Hua Yuan, Email: fixboner@163.com.
References
- 1.Sidhu V.S., Hermans D., Duckworth D.G. The operative outcomes of displaced medial-end clavicle fractures. J Shoulder Elbow Surg. 2015;24:1728–1734. doi: 10.1016/j.jse.2015.04.011. [DOI] [PubMed] [Google Scholar]
- 2.Ahmadreza M., Mirmostafa S., Mohammadreza G. Distal clavicular fracture treatment with suture anchor method. Acta Orthop Traumatol Turc. 2016;50:298–302. doi: 10.3944/AOTT.2015.15.0023. [DOI] [PubMed] [Google Scholar]
- 3.Ropars M., Thomazeau H., Huten D. Clavicle fractures orthopaedics & traumatology. Surg Res. 2017;103:s53–s59. doi: 10.1016/j.otsr.2016.11.007. [DOI] [PubMed] [Google Scholar]
- 4.Robinson C.M., Goudie E.B., Murray I.R. Open reduction and plate fixation versus nonoperative treatment for displaced midshaft clavicular fractures: a multicenter, randomized, controlled trial. J Bone Joint Surg Am. 2013;95:1576–1584. doi: 10.2106/JBJS.L.00307. [DOI] [PubMed] [Google Scholar]
- 5.Wang Y., Jiang J., Dou B. Inverted distal clavicle anatomic locking plate for displaced medial clavicle fracture. Arch Orthop Trauma Surg. 2015;135:1241–1245. doi: 10.1007/s00402-015-2259-x. [DOI] [PubMed] [Google Scholar]
- 6.McKenna M. Plating of a periarticular medial clavicle fracture. Orthopedics. 2009;32:366–368. doi: 10.3928/01477447-20090501-08. [DOI] [PubMed] [Google Scholar]
- 7.Ryan C., Robert B., James S. Operative treatment of the painful sternoclavicular joint: a new technique using interpositional arthroplasty. J Shoulder Elbow Surg. 2006;15:60–66. doi: 10.1016/j.jse.2005.04.005. [DOI] [PubMed] [Google Scholar]
- 8.Khan L.A.K., Bradnock T.J., Scott C. Fractures of the clavicle. J Bone Joint Surg. 2009;91:447–460. doi: 10.2106/JBJS.H.00034. [DOI] [PubMed] [Google Scholar]
- 9.Luke R., Riyad G., Ron A. Sports participation and radiographic findings of adolescents treated nonoperatively for displaced clavicle fractures. Injury. 2015;46:1372–1376. doi: 10.1016/j.injury.2015.04.019. [DOI] [PubMed] [Google Scholar]
- 10.Fu Beigang. Minimally invasive intramedullary nailing of clavicular fractures by a new titanium elastic nail. Acta Orthop Traumatol Turc. 2016;50:494–500. doi: 10.1016/j.aott.2016.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yi J.W., Kim D.H., Heo Y.M. Bilateral sternoclavicular joint dislocation due to sternal fracture: is it a dislocation or a separation? Arch Orthop Trauma Surg. 2016;136:605–608. doi: 10.1007/s00402-016-2433-9. [DOI] [PubMed] [Google Scholar]
- 12.Hwang W.J., Lee Y., Yoon Y.S. Surgical treatment of sternoclavicular joint dislocation using a T-plate. Korean J Thorac Cardiovasc Surg. 2016;49:221–223. doi: 10.5090/kjtcs.2016.49.3.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sinan Z., Murat C., Ercan S. Comparison between locked intramedullary nailing and anatomical locking plating in the treatment of displaced clavicular midshaft fractures. Acta Orthop Traumatol Turc. 2016;50:291–297. doi: 10.3944/AOTT.2015.15.0220. [DOI] [PubMed] [Google Scholar]
- 14.Siebenlist S., Sandmann G., Kirchhoff C. Anatomically precontoured LCP for delayed union of a medial third clavicle fracture. Case report with review of the literature. Acta Chir Orthop Traumatol Cech. 2013;80:407–410. [PubMed] [Google Scholar]
- 15.Bartonícek J., Fric V., Pacovský V. Displaced fractures of the medial end of the clavicle: report of five cases. J Orthop Trauma. 2010;24:e31–e35. doi: 10.1097/BOT.0b013e3181aa5505. [DOI] [PubMed] [Google Scholar]
- 16.Tennent T.D., Pearse E.O., Eastwood D.M. A new technique for stabilizing adolescent posteriorly displaced physeal medial clavicular fractures. J Shoulder Elbow Surg. 2012;21:1734–1739. doi: 10.1016/j.jse.2011.12.002. [DOI] [PubMed] [Google Scholar]
- 17.Al-Yassari G., Hetzenauer M., Tauber M. Novel method to treat sterno-clavicular joint instability and medial clavicle fracture symptomatic nonunion. J Shoulder Elbow Surg. 2009;18:553–555. doi: 10.1016/j.jse.2008.11.011. [DOI] [PubMed] [Google Scholar]
- 18.Negri J.H., Malavolta E.A., Assunção J.H. Assessment of the function and resistance of sternoclavicular ligaments: a biomechanical study in cadavers. Orthopaedics Traumatol Surg Res. 2014;100:727–731. doi: 10.1016/j.otsr.2014.07.011. [DOI] [PubMed] [Google Scholar]
- 19.Morell D.J., Thyagarajan D.S. Sternoclavicular joint dislocation and its management: a review of the literature. World J Orthop. 2016;7:244–250. doi: 10.5312/wjo.v7.i4.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Katthagen J.C., Tahal D.S., Menge T.J. Minimum 2-year outcomes and return to sport following resection arthroplasty for the treatment of sternoclavicular osteoarthritis. J Shoulder Elbow Surg. 2017;26:e37–e43. doi: 10.1016/j.jse.2016.07.008. [DOI] [PubMed] [Google Scholar]
- 21.Yousefifard M., Baikpour M., Ghelichkhani P. Comparison of ultrasonography and radiography in detection of thoracic bone fractures; a systematic review and meta-analysis. Emerg (Tehran) 2016;4:55–64. [PMC free article] [PubMed] [Google Scholar]