Abstract
Chimeric antigen receptor (CAR) T cell therapy for the treatment of acute myeloid leukemia (AML) has the risk of toxicity to normal myeloid cells. CD7 is expressed by the leukemic blasts and malignant progenitor cells of approximately 30% of AML patients but is absent on normal myeloid and erythroid cells. Since CD7 expression by malignant blasts is also linked with chemoresistance and poor outcomes, targeting this antigen may be beneficial for this subset of AML patients. Here, we show that expression of a CD7-directed CAR in CD7 gene-edited (CD7KO) T cells effectively eliminates CD7+ AML cell lines, primary CD7+ AML, and colony-forming cells but spares myeloid and erythroid progenitor cells and their progeny. In a xenograft model, CD7 CAR T cells protect mice against systemic leukemia, prolonging survival. Our results support the feasibility of using CD7KO CD7 CAR T cells for the non-myeloablative treatment of CD7+ AML.
Keywords: acute myeloid leukemia, chimeric antigen receptors, CAR T cells, mouse model, CD7
CD7 is expressed in T cells and in some subtypes of AML. Gomes-Silva and colleagues show that CRISPR-edited CD7 knockout T cells expressing a CD7-specific CAR resist fratricide and control AML while sparing the non-malignant myeloid compartment.
Introduction
Although the standard-of-care treatment for acute myeloid leukemia (AML) commonly induces complete remissions, in many patients the disease will relapse with poor prognosis and few options for targeted therapy. Chimeric antigen receptor (CAR) T cells targeting myeloid-lineage antigens such as CD33, CD123, Lewis Y, CLL-1, CD44v6, FLT3, and folate receptor β have produced promising results in preclinical models of AML.1, 2, 3, 4, 5, 6, 7, 8, 9 However, evidence of sustained complete responses in patients treated with CD33 CAR, CD123 CAR, or Lewis Y CAR T cells has been lacking.10, 11, 12 In addition, because T cells expressing these CARs do not discriminate between malignant cells and normal cells expressing the same antigen, clinical application is associated with toxicity against normal hematopoietic progenitor cells.9, 12
Alternatives to the above approach are to target antigens that are selectively expressed on leukemic and mature normal cell subpopulations but are absent on critical primitive progenitors (e.g., CLL-1Ref.5) or to choose an antigen expressed by malignant myeloid cells but that is absent on the normal members of that lineage. Both these approaches mitigate on-target toxicity against critical myeloid precursors, but it is not yet known which is superior. In this study, we describe the targeting of a lineage-restricted antigen, CD7, that is absent on normal myeloid cells but becomes aberrantly expressed by leukemic clones. This aberrant expression allows selective elimination of the malignant cells but spares normal myeloid cells and their precursors.
CD7 is a transmembrane glycoprotein expressed by 30% of AML, and its expression is associated with more aggressive disease and resistance to standard therapy.13, 14, 15, 16, 17, 18 Normal CD7 expression is largely limited to T and NK cells and their precursors, where it acts as a costimulatory receptor for T- and B-lymphocyte interactions during lymphoid development. The function of CD7 in mature T cells is likely redundant, as CD7-deficient mice demonstrate largely unperturbed peripheral T cell function. CD7 is also expressed in a subset of myeloid progenitors in cord blood, although its role in these cells has not yet been defined.19, 20, 21
Although the expression pattern of CD7 suggests it can be used to target AML with high selectivity and limited toxicity against normal myeloid cells, its presence on normal T cells means that expression of a CD7 CAR on these cells would not be feasible, since it would prove fratricidal.22, 23, 24 We therefore developed a means of editing the CD7 gene in T cells prior to CD7 CAR expression and have showed that such edited T cells expand well and retain functionality through both their native and chimeric receptor.22
Here, we demonstrate that CD7-edited (CD7KO) CD7 CAR T cells can selectively eliminate AML cell lines, primary leukemia blasts, and AML precursor cells in vitro and in a xenograft model of the disease, without evident toxicity against normal myeloid cells and hematopoietic progenitors. These results support the feasibility of targeting AML with CD7 CAR T cells.
Results
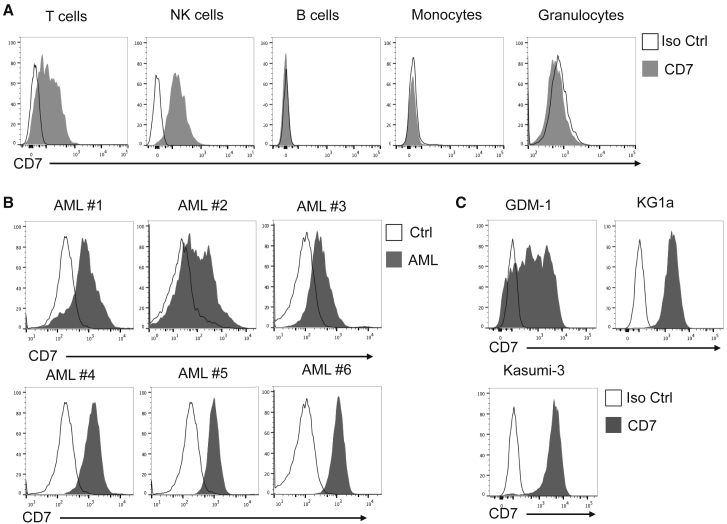
CD7 Is Expressed by AML Blasts but Is Absent on Normal Myeloid Cells in Peripheral Blood
CD7 is stably expressed in T- and NK-cell precursors and is maintained in most of their peripheral progeny but is absent from most B cell and myeloid subsets. We detected no expression of CD7 in peripheral monocytes, granulocytes, or B cells, though most T and NK cells were CD7 positive (Figure 1A). We then analyzed CD7 expression in 20 primary AML samples collected from patients at Texas Children’s Hospital and Houston Methodist Hospital. We detected surface expression of CD7 in six out of 20 samples (Table 1), albeit with varying intensities (Figure 1B). CD7 expression was also detected in AML cell lines KG-1a, Kasumi-3, and GDM-1 (Figure 1C). These data indicate that CD7 is expressed in leukemic, but not normal, myeloid cells and may be suited for the selective targeting of AML.
Figure 1.
CD7 Expression in Normal and Malignant Cells
(A) Representative histograms of CD7 expression in immune subsets from peripheral blood of healthy donors. (B) Surface expression of CD7 measured by flow cytometry in primary AML samples collected from pediatric and adult patients. (C) CD7 expression in AML cell lines. Iso Ctrl, Isotype control.
Table 1.
Characteristics of AML
| AML Sample ID | Age | Sex | Cytogenetics |
|---|---|---|---|
| 1 | 12 years | M | 46, XY |
| 2 | 44 years | F | inv(16)(p13.1q22) |
| 3 | 13 years | M | 46, XY |
| 4 | 8 years | M | t(9;11), MLL-R |
| 5 | 13 years | M | t(6:11), MLL-R |
| 6 | 16 months | M | Trisomy8, MLL-R |
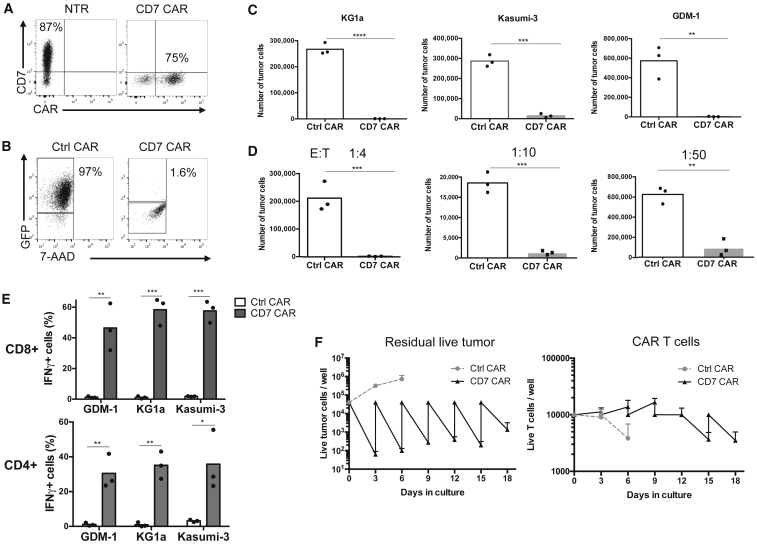
CD7 CAR T Cells Are Highly Cytotoxic against CD7+ AML Cell Lines
Generation and expansion of functional CD7 CAR T cells requires CD7 removal prior to CAR expression to minimize T cell fratricide. We have previously shown that by CRISPR/Cas9-mediated disruption of the CD7 gene in primary activated T cells, we could generate CD7KO CD7 CAR T cells (hereafter CD7 CAR T cells) with specific cytolytic activity against CD7+ T-lymphoblastic leukemia.22 We have used this approach to generate CD7-edited T cells expressing a second-generation CD7 CAR with the CD28 costimulatory endodomain. Following gammaretroviral transduction, the expanded T cells were uniformly CD7 negative, and >70% were CD7 CAR positive (Figure 2A).
Figure 2.
CD7-Edited CD7 CAR T Cells Are Cytotoxic against AML Cell Lines
(A) Expression of CD7 in non-treated (NTR) and CD7 and CAR in CD7-edited T cells. (B) Frequency of residual live GFP+ KG-1a AML cells upon coculture with control or CD7 CAR T cells for 3 days at a 1:40 effector-to-target (E:T) ratio. (C) Absolute counts of live AML cells at the end of the coculture are plotted on the bar graphs. (D) Absolute counts of residual live KG-1a cells after coculture with CD7 CAR T cells at the indicated E:T ratios. (E) IFNγ production by CD8+ and CD4+ CD7 CAR T cells upon 4-hr coculture with indicated AML cell lines by intracellular cytokine staining and flow cytometry. Individual data points for each donor are shown. (F) Repeated cytotoxicity against KG-1a AML cells in a sequential killing assay. CD7 CAR T cells were plated with KG-1a AML cells at a 1:4 E:T ratio, and the ratio was restored every 3–4 days after quantification of residual live tumor cells (left) and CAR T cells (right). Data are shown as mean ± SD. Data represent 2–3 independent experiments. *p < 0.05; **p < 0.01; ***p < 0.001; ****p < 0.0001 by unpaired Student’s t test.
To assess the CD7-directed activity of the CAR T cells against AML blasts, we cocultured T cells expressing CD7 CAR or an irrelevant CAR with fluorescently labeled CD7+ AML cell lines KG-1a, Kasumi-3, and GDM-1 for 3–5 days. To model physiologic conditions, we used a low effector-to-target ratio of 1:40 and analyzed the number of residual live tumor cells at the end of coculture. We observed a 2–3 log reduction in the counts of residual malignant cells upon coculture with CD7 CAR T cells, but not with control T cells (Figures 2B and 2C). CD7 CAR T cells retained cytotoxicity against AML cells at effector-to-target ratios ranging from 1:4 to 1:50 (Figure 2D), indicating CD7 CAR T cells have high cytolytic potential. We also detected robust production of interferon gamma (IFNγ) by both CD4+ and CD8+ CD7 CAR T cells upon incubation with AML blasts (Figure 2E). To establish whether the CD7 CAR T cells were resistant to functional exhaustion, we used a sequential killing assay in which T cells were plated with KG-1a cells at a 1:4 effector-to-target ratio and replated every 3 days with fresh tumor cells to restore the initial ratio. Unlike control T cells, CD7 CAR T cells repeatedly eliminated AML tumor cells for at least six rounds (Figure 2E). Collectively, CD7 CAR T cells demonstrate robust and sustained cytotoxicity against AML cell lines in vitro.
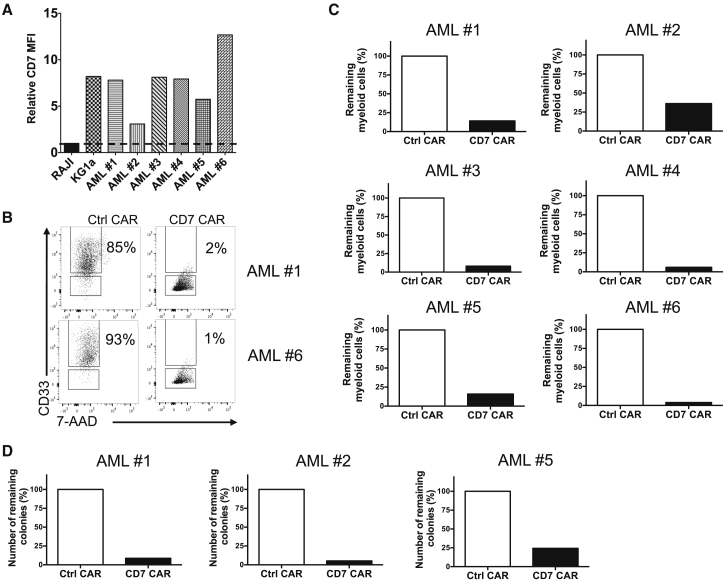
CD7 CAR T Cells Eradicate Primary AML Blasts and Leukemia Colony-Forming Cells
To evaluate the activity of CD7 CAR T cells against primary AML, we measured cytotoxicity against several primary AML samples expressing varying levels of CD7 (Figure 3A). We observed between 3- and 30-fold reductions in the counts of residual live myeloid cells after 48 hr of coculture with CD7 CAR T cells at a 1:2 effector-to-target ratio (Figures 3B and 3C). We then cocultured CD7 CAR T cells with AML samples for 5 hr and plated the surviving cells on a methylcellulose medium that supports long-term expansion of myeloid colonies. We observed decreased numbers of colonies after a coculture with CD7 CAR T cells compared with control T cells (Figure 3D), indicating the cytotoxic activity of CD7 CAR T cells extends to leukemic colony-forming cells that commonly contain chemoresistant leukemic stem cells (LSCs).25, 26 These results suggest CD7 CAR T cells target both AML blasts and primitive colony-forming cells, although additional functional characterization is required to confirm the LSC-specific activity.
Figure 3.
Elimination of Primary AML Blasts and Colony-Forming Cells by CD7 CAR T Cells
(A) Normalized MFI of CD7 in primary AML blasts compared with KG-1a (positive control) and Raji (negative control). (B) Representative dot plots showing frequencies of live primary AML blasts after 48 hr coculture with control or CD7 CAR T cells at a 1:1 E:T ratio. (C) Absolute counts of residual CD33+ myeloid cells from individual patients at the end of coculture with control or CD7 CAR T cells. (D) Control or CD7 CAR T cells were cocultured with AML blasts for 5 hr at a 5:1 E:T ratio and plated on MethoCult media. The bar graphs show relative numbers of colonies (pooled duplicate measurements) formed after 14 days of culture.
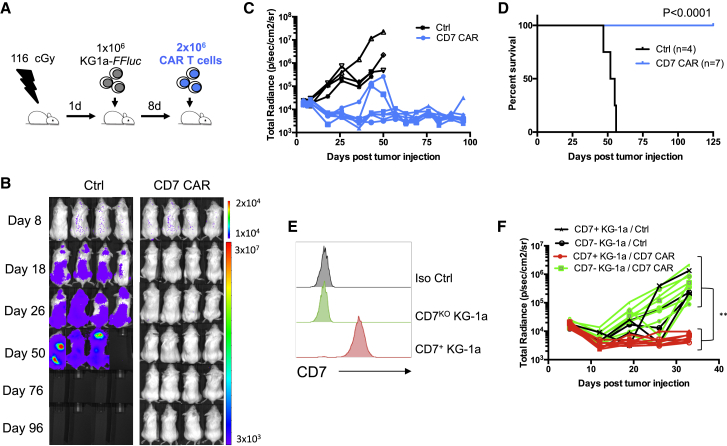
CD7 CAR T Cells Protect against Systemic AML In Vivo
Next, we assessed the ability of CD7 CAR T cells to control the progression of AML in vivo. We used a mouse xenograft model of AML in which sub-lethally irradiated NOD.SCID.IL2rg−/− (NSG) mice were engrafted via intravenous injection of 1 × 106 KG-1a AML cells expressing firefly luciferase (FFluc). After 8 days, we injected a single dose of non-transduced or CD7 CAR T cells intravenously (Figure 4A). Tumor burden was monitored weekly by in vivo luminescence imaging, and surviving animals were euthanized 125 days after T cell injection. Mice receiving control T cells developed systemic leukemia (Figures 4B and 4C), and all succumbed to the disease with median survival of 54 days (Figure 4D). In contrast, injection of CD7 CAR T cells reversed leukemia progression and resulted in no observed tumor growth for the duration of the experiment. Of note, injection of CD7 CAR T cells earlier (on day 5) resulted in tumor relapses in some mice, shortening median survival to 97 days (Figure S1). Emerging tumor cells in CD7 CAR T cell-treated mice retained CD7 expression, suggesting the relapses were likely due to transient activity of CD7 CAR T cells (Figure S1).
Figure 4.
CD7 CAR T Cells Are Protective in a Mouse Xenograft Model of AML
(A) General outline of the experiment. NSG mice received FFluc-expressing KG-1a cells 24 hr after sublethal irradiation with 116 cGy. Eight days later, mice received a single injection of control or CD7 CAR T cells intravenously and were monitored for tumor progression. (B) Representative images showing leukemia progression in individual mice. (C) Kinetics of leukemia progression in individual mice that received either control or CD7 CAR T cells by IVIS imaging. (D) Kaplan-Meier curves showing survival of mice in each experimental group. p < 0.0001 by Mantel-Cox log rank test. (E) Expression of CD7 in residual unmodified and CRISPR/Cas9-edited CD7KO KG-1a AML. (F) Kinetics of leukemia progression in CD7 CAR T-treated mice receiving unmodified (CD7+) or CD7KO KG-1a leukemia. **p < 0.01 by unpaired Student’s t test.
To rule out allogeneic rejection of leukemia by expanded CD7 CAR T cells in vivo, we evaluated the anti-tumor activity of CD7 CAR T cells against a CD7-edited KG-1a cell line, in which the CD7 gene was disrupted using CRISPR/Cas9 (Figure 4E). CD7 CAR T cells suppressed leukemic progression only in mice engrafted with unmodified (CD7+) KG-1a but not with CD7-edited tumor cells (Figure 4F) indicating the anti-leukemic activity of CD7 CAR T cells in vivo was CD7-specific.
Normal Myeloid Progenitor and Mature Cells Are Spared by CD7 CAR T
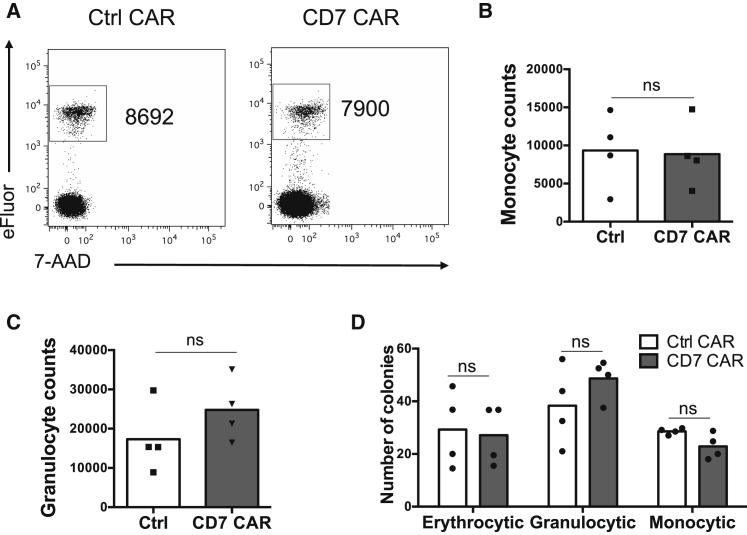
CD7 is absent on most normal mature myeloid and erythroid cells, and we observed no toxicity of CD7 CAR T cells against peripheral monocytes (Figures 5A and 5B) or granulocytes (Figure 5C) after in vitro coculture.
Figure 5.
Lack of Reactivity of CD7 CAR T Cells against Mature Myeloid Cells and Cord Blood Precursors
(A) CD14+ monocytes were purified from PBMC using magnetic beads and labeled with eFluor 670 prior to coculture with control or CD7 CAR T cells at a 1:1 ratio. Representative dot plots show the numbers of residual live monocytes after 24 hr of coculture. (B) Data from four donors are summarized in a bar graph. (C) Total blood cells after RBC lysis were cocultured with autologous CD7 CAR T cells for 24 hr. Live granulocytes were quantified at the end of coculture by flow cytometry. (D) Cord blood cells were cocultured with control or CD7 CAR T cells at a 10:1 E:T ratio for 5 hr and plated on the MethoCult media. Numbers of erythrocytic, granulocytic, and monocytic colonies were quantified 14 days later. Data from individual donors are shown. Data represent two independent experiments. ns, Not significant by unpaired Student’s t test.
Since CD7 may be transiently upregulated on some hematopoietic progenitors that are enriched in cord blood, we measured the cytolytic activity of CD7 CAR T cells against hematopoietic progenitor cells from cord blood. We cocultured CD7 CAR T cells with cord blood cells for 5 hr followed by a 12-day expansion on a methylcellulose medium supporting both myeloid and erythroid differentiation. CD7 CAR T cells had no impact on monocytic, granulocytic, and erythrocytic colony counts compared to coculture with control T cells. These data indicate primitive myeloid and erythroid progenitors are not inhibited by CD7-edited CD7 CAR T cells (Figure 5D).
Discussion
The risk of unwanted myeloablation complicates the development of safe targeted therapies of AML, as few surface antigens are selectively expressed in malignant cells but absent in critical non-malignant myeloid and erythroid cells. Here, we demonstrate that T cells expressing a CD7-specific CAR can effectively target a subset of aggressive AML expressing CD7 without cytotoxicity against normal myeloid and erythroid cells. Therefore, the CD7-directed targeting can be used for non-myeloablative therapy of AML.
CD7 is expressed in ∼30% of AML, most of which are intermediate-to-high-risk disease by cytogenetics.13, 14 Some, but not all, studies reported CD7 positivity correlates with chemoresistance and higher incidence of relapse post-stem-cell-transplant15, 16, 17, 18 and is associated with poor prognosis in myelodysplastic syndromes.27, 28 CD7 expression in malignant myeloid cells is an indicator of their immaturity29 and a more “primitive” CD34+ phenotype that is often associated with chemoresistant leukemia-initiating cells.30, 31, 32 In cord blood, a fraction of Lin− CD34+ CD38− hematopoietic cells coexpress CD7; these cells constitute multilymphoid and common lymphoid progenitors.19, 20, 21 In the bone marrow, however, CD7 expression on these lymphoid progenitors has not been detected;19, 20, 33 although CD7 can be expressed at a low level on a small fraction of CD38+ CD34+ Lin− cells with an unknown function.34, 35 Later in hematopoiesis, CD7 expression is restricted only to T- and NK-cell progenitors and their descendants.36, 37 Thus, the cytotoxic activity of CD7 CAR T cells within the myeloid compartment should be limited primarily to leukemic cells, whereas normal myeloid and erythroid lineage cells will be largely spared.
Although the predicted effect of CD7 CAR T cells on non-malignant myeloid and erythroid cells is minimal, elimination of normal CD7+ T- and NK-cells can be expected.22 Prolonged aplasia of these critical immune cells can result in immunosuppression with a particular increase in the risk of viral infections and reactivation of latent viruses. Thus, CD7 CAR T cells may be used as a transient transplant-enabling therapy in patients with refractory or relapsed disease. In this scenario, the transient activity of CAR T cells would minimize the tumor burden and serve as a bridge to the curative stem cell transplant, which would terminate CAR T cell activity and reset normal T/NK lymphopoiesis. To facilitate robust-yet-transient activity of CD7 CAR T cells, we have used a second-generation CAR backbone with CD28 costimulation, which has been shown in clinical studies to promote rapid expansion and high cytotoxicity with limited persistence of CD19 CAR T cells.38, 39, 40, 41 Alternatively, fratricide-resistant CD7-edited T cells may substitute normal T cells and provide protection against pathogens commonly arising in T-cell-depleted patients.22 Additional studies are required to evaluate whether coadministration of the fratricide-resistant lymphocytes or other strategies to mitigate T/NK cell aplasia could enable the CD7-directed therapy of AML outside of the stem cell transplant setting.
Removal of CD7 expression from the surface of T cells is essential to mitigate fratricide of CD7 CAR T cells and enable their expansion.22, 24 As we demonstrated in a previous report, CRISPR/Cas9-mediated disruption of the CD7 gene in T cells prior to CD7 CAR transduction results in permanent removal of the CD7 gene in 85%–90% of T cells with no detected off-target activity; the remaining CD7+ T cells are eliminated by fratricide after CAR transduction.22 Genome editing, however, is not the only way to conceal CD7 from the cell surface. A recent report showed that the CD7 protein can be “trapped” inside the T cell when bound to an engineered CD7-specific single chain variable fragment (scFv) anchored in the endoplasmic reticulum of the cell.23 This interaction prevents CD7 from trafficking to the cell surface and effectively reduces fratricide of CD7 CAR T cells. While such method would obviate the need for genome editing in T cells, the long-term efficacy and feasibility of both methods to generate fratricide-resistant CD7 CAR T cells need to be compared in clinical studies.
Although adoptive cell therapy approaches for AML have been under active development for many years, clinical benefit has been only modest and largely dwarfed by the resounding success of CARs directed to B cell antigens, such as CD19. As many of the targetable antigens are also expressed by critical hematopoietic precursors (CD33, CD123, etc.), the activity of CAR T cells directed to those antigens has to be carefully dosed to avoid prolonged systemic myeloablation. Combinatorial antigen targeting to enable specific targeting of malignant myeloid cells while maximally restraining the activity against normal cells represents one attractive therapeutic strategy of AML.42, 43 As CD7 is largely absent on normal myeloid cells and their progenitors, complementary targeting of the lymphoid lineage-restricted CD7 and a pan-myeloid marker in a Boolean “AND” gate could potentially enable highly specific targeting of dual antigen-positive leukemic cells while sparing single-positive myeloid and lymphoid cells. The approach presented in this study is directed at CD7, which is not known to be expressed on critical myeloid and erythroid progenitors and mature cells, and thus CD7 CAR T cells alone may benefit patients with CD7+ disease.
Materials and Methods
Generation of CD7 CAR T Cells
A CD7-specific single-chain variable fragment derived from clone 3A1e of CD7-specific antibody was created using commercial gene synthesis (Bio Basic) and cloned into a second-generation CAR backbone containing CD28 and CD3z endodomains and the CH3 domain from immunoglobulin G1 (IgG1) Fc as a spacer region.22, 44 A truncated CD7 CAR lacking signaling endodomains was used as a control. T cells were activated by plate-bound OKT3 and anti-CD28 antibodies, and the CD7 gene was removed using CRISPR/Cas9 before transduction as previously described.22, 45 In brief, T cells were electroporated with 0.4 μg of guide RNA (gRNA) and 1 μg of Cas9 protein (Integrated DNA Technologies) with 0.25 × 106 of activated T cells by using the Neon Transfection System (Thermo Fisher Scientific) in 10 μL of buffer T and using 3 1600-V 10-ms pulses. Following electroporation, T cells were incubated in cytotoxic T-lymphocyte (CTL) media supplemented with 20% fetal bovine serum (FBS) in the presence of interleukin-7 (IL-7) and IL-15 overnight after electroporation. T cells were then expanded in CTL media in the presence of IL-7 and IL-15 and 10% FBS for 3 days and transduced with gammaretroviral vectors encoding CD7 CARs.
Flow Cytometry
Anti-human CD7 (Biolegend); CD4, CD8, CD14, CD15, CD33, IFNγ (BD Biosciences); and CD45 (Beckman Coulter) were used to stain cells. Anti-IgG Fc (Jackson ImmunoResearch) was used for CAR detection in all assays. All flow cytometry data were obtained in a BD fluorescence-activated cell sorter (FACS) Canto II (BD Biosciences) and Gallios (Beckman Coulter) and analyzed with FlowJo software (FlowJo).
Cytotoxicity Assay
Cell lines GDM-1 (ATCC CRL-2627) and Kasumi-3 (ATCC CRL-2725) were purchased from ATCC. KG-1a cell line was a gift from Dr. Stephen Gottschalk. The cells were expanded according to ATCC recommendations. Tumor cell lines stained with eFluor670 (Thermo Fisher Scientific) or permanently transduced with GFP and incubated with CD7 CAR T cells for 3 days without exogenous cytokines, unless stated otherwise. Cells from individual wells were collected at indicated time points. 7-aminoactinomycin D (7-AAD) was added to exclude dead cells, and cells were quantified using CountBright Absolute Counting Beads (Thermo Fisher Scientific). For the sequential killing assay, the numbers of residual T cells and AML cells were quantified every 3 days using flow cytometry with counting beads, as previously described.44 Tumor cells were then added to the wells with CAR T cells to restore the original effector:target (E:T) ratio of 1:4. Frozen peripheral blood mononuclear cells (PBMCs) from AML patients at Methodist Hospital and Texas Children’s Hospital were used for the cytotoxicity assay at the E:T ratio of 1:1 for 48 hr. AML patients and healthy donors gave written informed consent to participate on protocols approved by the Baylor College of Medicine Institutional Review Board, in accordance with the Declaration of Helsinki.
Intracellular Staining Assay
CD7 CAR T cells were cultured with tumor cells for 5 hr at a 1:4 E:T ratio. Brefeldin A (BD GolgiPlug) was added 1 hr after plating. At the end of coculture, cells were incubated with antibodies for surface antigens and permeabilized for 10 min using BD FACS Permeabilizing Solution 2, followed by incubation with IFNγ antibody and analyzed by flow cytometry, as previously described.22
AML Mouse Xenograft Model
Five- to seven-week-old nonobese diabetic (NOD)-Cg-Prkdcscid Il2rgtm1Wjl/SzJ (NSG) mice were purchased from the Jackson Laboratory and maintained at the Baylor College of Medicine Animal Facility. All procedures were done in compliance with the Institutional Animal Care and Usage Committee of Baylor College of Medicine. Mice were sublethally irradiated (116–200 cGy) and injected intravenously 24 hr later with 1 × 106 KG-1a-FFluc cells followed by a single injection of 2 × 106 of CD7 CAR T cells 5 or 8 days later. Tumor burden was monitored using an IVIS Imaging system (Caliper Life Sciences) by recording bioluminescence from mice injected with 150 mg/kg of D-luciferin intraperitoneally at indicated time points. Living Image software (PerkinElmer) was used to visualize and calculate total luminescence. For analysis of tumor cells in peripheral blood, 100 μL of blood was collected by tail-vein bleeding. After red blood cell lysis, cells were incubated with anti-human CD45 and CD3, and CD7 antibodies for subsequent flow cytometric analysis.
Colony Formation Assay
CD7 CAR T cells or control CAR were incubated with mononuclear cells from cord blood (CB) of healthy donors (E:T ratio of 10:1) or PBMCs from patients with AML (E:T ratio of 5:1) for 5 hr.5, 44 Cells were then plated in duplicates (50,000 cells per well) in methylcellulose-based medium supplemented with recombinant cytokines (MethoCult H4434 Classic; STEMCELL Technologies). After 12 days of culture, the numbers of granulocytic, monocytic, and erythrocytic colony-forming units in CB or leukemic colonies in AML samples were assessed using an inverted microscope.
Coculture with Normal PBMCs
Monocytes were isolated from PBMCs of healthy donors using CD14+ magnetic beads (Miltenyi Biotec) according to manufacture’s instructions. Monocytes were stained with eFluor670 and cocultured with CD7 CAR T cells or control CAR T cells at an E:T ratio of 1:1 overnight. Granulocytes were collected from peripheral blood of healthy donors. After red cell lysis, immune cells were incubated with CD7 CAR T cells overnight at an E:T ratio of 1:5. Granulocytes were discriminated by side scatter (SSC) and forward scatter (FSC) and CD15 staining. Absolute cell counts were obtained for both myeloid populations using CountBright Absolute Counting Beads by flow cytometry.
Statistical Analysis
Data points from individual donors are shown in all figures. Statistical significance in pairwise comparisons was determined by an unpaired two-tailed Student’s t test and in multiple comparisons by a one-way ANOVA with post-test Bonferroni correction. Statistical significance in Kaplan-Meier survival curves was assessed with the Mantel-Cox log rank test. All p values were calculated using Prism 6 software (GraphPad).
Author Contributions
D.G.-S. designed and performed the experiments, analyzed the data, and wrote the manuscript; E.A., P.A.A., and H.T. designed and performed experiments and edited the manuscript; F.M. and M.S. designed and performed the experiments; P.L. and R.H.R. provided primary AML samples and collected patient data; J.M.S.C. and C.A.R. supported the study and edited the manuscript; M.K.B. provided feedback and edited the manuscript; M.M. conceptualized and directed the study, designed and performed experiments, analyzed the data, and wrote the manuscript.
Conflicts of Interest
The authors declare no conflicts of interest.
Acknowledgments
The authors thank Catherine Gillespie for editing the manuscript, Dimitrios Wagner, Michael Gundry, Lorenzo Brunetti for assistance with genome editing, and Stephen Gottschalk and Tim Sauer for providing the KG-1a cell line. This study was supported by a grant from the NIH National Cancer Institute (NCI) (P50 CA126752) and an American Society of Hematology (ASH) Scholar Award (to M.M.). The authors also appreciate the support of shared resources in the Dan L Duncan Comprehensive Cancer Center (support grant NCIP30CA125123 from the NIH NCI).
Footnotes
Supplemental Information includes one figure and can be found with this article online at https://doi.org/10.1016/j.ymthe.2018.10.001.
Supplemental Information
References
- 1.Kenderian S.S., Ruella M., Shestova O., Klichinsky M., Aikawa V., Morrissette J.J.D., Scholler J., Song D., Porter D.L., Carroll M. CD33-specific chimeric antigen receptor T cells exhibit potent preclinical activity against human acute myeloid leukemia. Leukemia. 2015;29:1637–1647. doi: 10.1038/leu.2015.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mardiros A., Dos Santos C., McDonald T., Brown C.E., Wang X., Budde L.E., Hoffman L., Aguilar B., Chang W.C., Bretzlaff W. T cells expressing CD123-specific chimeric antigen receptors exhibit specific cytolytic effector functions and antitumor effects against human acute myeloid leukemia. Blood. 2013;122:3138–3148. doi: 10.1182/blood-2012-12-474056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gill S., Tasian S.K., Ruella M., Shestova O., Li Y., Porter D.L., Carroll M., Danet-Desnoyers G., Scholler J., Grupp S.A. Preclinical targeting of human acute myeloid leukemia and myeloablation using chimeric antigen receptor-modified T cells. Blood. 2014;123:2343–2354. doi: 10.1182/blood-2013-09-529537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Westwood J.A., Smyth M.J., Teng M.W.L., Moeller M., Trapani J.A., Scott A.M., Smyth F.E., Cartwright G.A., Power B.E., Hönemann D. Adoptive transfer of T cells modified with a humanized chimeric receptor gene inhibits growth of Lewis-Y-expressing tumors in mice. Proc. Natl. Acad. Sci. USA. 2005;102:19051–19056. doi: 10.1073/pnas.0504312102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tashiro H., Sauer T., Shum T., Parikh K., Mamonkin M., Omer B., Rouce R.H., Lulla P., Rooney C.M., Gottschalk S., Brenner M.K. Treatment of Acute Myeloid Leukemia with T Cells Expressing Chimeric Antigen Receptors Directed to C-type Lectin-like Molecule 1. Mol. Ther. 2017;25:2202–2213. doi: 10.1016/j.ymthe.2017.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Casucci M., Nicolis di Robilant B., Falcone L., Camisa B., Norelli M., Genovese P., Gentner B., Gullotta F., Ponzoni M., Bernardi M. CD44v6-targeted T cells mediate potent antitumor effects against acute myeloid leukemia and multiple myeloma. Blood. 2013;122:3461–3472. doi: 10.1182/blood-2013-04-493361. [DOI] [PubMed] [Google Scholar]
- 7.Lynn R.C., Poussin M., Kalota A., Feng Y., Low P.S., Dimitrov D.S., Powell D.J., Jr. Targeting of folate receptor β on acute myeloid leukemia blasts with chimeric antigen receptor-expressing T cells. Blood. 2015;125:3466–3476. doi: 10.1182/blood-2014-11-612721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jetani H., Garcia-Cadenas I., Nerreter T., Thomas S., Rydzek J., Meijide J.B., Bonig H., Herr W., Sierra J., Einsele H., Hudecek M. CAR T-cells targeting FLT3 have potent activity against FLT3-ITD+ AML and act synergistically with the FLT3-inhibitor crenolanib. Leukemia. 2018;32:1168–1179. doi: 10.1038/s41375-018-0009-0. [DOI] [PubMed] [Google Scholar]
- 9.Kim M.Y., Yu K.-R., Kenderian S.S., Ruella M., Chen S., Shin T.-H., Aljanahi A.A., Schreeder D., Klichinsky M., Shestova O. Genetic Inactivation of CD33 in Hematopoietic Stem Cells to Enable CAR T Cell Immunotherapy for Acute Myeloid Leukemia. Cell. 2018;173:1439–1453.e19. doi: 10.1016/j.cell.2018.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ritchie D.S., Neeson P.J., Khot A., Peinert S., Tai T., Tainton K., Chen K., Shin M., Wall D.M., Hönemann D. Persistence and efficacy of second generation CAR T cell against the LeY antigen in acute myeloid leukemia. Mol. Ther. 2013;21:2122–2129. doi: 10.1038/mt.2013.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang Q.S., Wang Y., Lv H.Y., Han Q.W., Fan H., Guo B., Wang L.L., Han W.D. Treatment of CD33-directed chimeric antigen receptor-modified T cells in one patient with relapsed and refractory acute myeloid leukemia. Mol. Ther. 2015;23:184–191. doi: 10.1038/mt.2014.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gill S. Chimeric antigen receptor T cell therapy in AML: How close are we? Best Pract. Res. Clin. Haematol. 2016;29:329–333. doi: 10.1016/j.beha.2016.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chang H., Salma F., Yi Q.L., Patterson B., Brien B., Minden M.D. Prognostic relevance of immunophenotyping in 379 patients with acute myeloid leukemia. Leuk. Res. 2004;28:43–48. doi: 10.1016/s0145-2126(03)00180-2. [DOI] [PubMed] [Google Scholar]
- 14.Ogata K., Yokose N., Shioi Y., Ishida Y., Tomiyama J., Hamaguchi H., Yagasaki F., Bessyo M., Sakamaki H., Dan K., Kuriya S. Reappraisal of the clinical significance of CD7 expression in association with cytogenetics in de novo acute myeloid leukaemia. Br. J. Haematol. 2001;115:612–615. doi: 10.1046/j.1365-2141.2001.03139.x. [DOI] [PubMed] [Google Scholar]
- 15.Chang H., Yeung J., Brandwein J., Yi Q.L. CD7 expression predicts poor disease free survival and post-remission survival in patients with acute myeloid leukemia and normal karyotype. Leuk. Res. 2007;31:157–162. doi: 10.1016/j.leukres.2006.06.001. [DOI] [PubMed] [Google Scholar]
- 16.Saxena A., Sheridan D.P., Card R.T., McPeek A.M., Mewdell C.C., Skinnider L.F. Biologic and clinical significance of CD7 expression in acute myeloid leukemia. Am. J. Hematol. 1998;58:278–284. doi: 10.1002/(sici)1096-8652(199808)58:4<278::aid-ajh5>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 17.Del Poeta G., Stasi R., Venditti A., Cox C., Aronica G., Masi M., Bruno A., Simone M.D., Buccisano F., Papa G. CD7 expression in acute myeloid leukemia. Leuk. Lymphoma. 1995;17:111–119. doi: 10.3109/10428199509051710. [DOI] [PubMed] [Google Scholar]
- 18.Kita K., Miwa H., Nakase K., Kawakami K., Kobayashi T., Shirakawa S., Tanaka I., Ohta C., Tsutani H., Oguma S., The Japan Cooperative Group of Leukemia/Lymphoma Clinical importance of CD7 expression in acute myelocytic leukemia. Blood. 1993;81:2399–2405. [PubMed] [Google Scholar]
- 19.Doulatov S., Notta F., Eppert K., Nguyen L.T., Ohashi P.S., Dick J.E. Revised map of the human progenitor hierarchy shows the origin of macrophages and dendritic cells in early lymphoid development. Nat. Immunol. 2010;11:585–593. doi: 10.1038/ni.1889. [DOI] [PubMed] [Google Scholar]
- 20.Galy A., Travis M., Cen D., Chen B. Human T, B, natural killer, and dendritic cells arise from a common bone marrow progenitor cell subset. Immunity. 1995;3:459–473. doi: 10.1016/1074-7613(95)90175-2. [DOI] [PubMed] [Google Scholar]
- 21.Hao Q.-L., Zhu J., Price M.A., Payne K.J., Barsky L.W., Crooks G.M. Identification of a novel, human multilymphoid progenitor in cord blood. Blood. 2001;97:3683–3690. doi: 10.1182/blood.v97.12.3683. [DOI] [PubMed] [Google Scholar]
- 22.Gomes-Silva D., Srinivasan M., Sharma S., Lee C.M., Wagner D.L., Davis T.H., Rouce R.H., Bao G., Brenner M.K., Mamonkin M. CD7-edited T cells expressing a CD7-specific CAR for the therapy of T-cell malignancies. Blood. 2017;130:285–296. doi: 10.1182/blood-2017-01-761320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Png Y.T., Vinanica N., Kamiya T., Shimasaki N., Coustan-Smith E., Campana D. Blockade of CD7 expression in T cells for effective chimeric antigen receptor targeting of T-cell malignancies. Blood Adv. 2017;1:2348–2360. doi: 10.1182/bloodadvances.2017009928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cooper M.L., Choi J., Staser K., Ritchey J.K., Devenport J.M., Eckardt K., Rettig M.P., Wang B., Eissenberg L.G., Ghobadi A. An “off-the-shelf” fratricide-resistant CAR-T for the treatment of T cell hematologic malignancies. Leukemia. 2018;32:1970–1983. doi: 10.1038/s41375-018-0065-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Majeti R., Park C.Y., Weissman I.L. Identification of a hierarchy of multipotent hematopoietic progenitors in human cord blood. Cell Stem Cell. 2007;1:635–645. doi: 10.1016/j.stem.2007.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jan M., Chao M.P., Cha A.C., Alizadeh A.A., Gentles A.J., Weissman I.L., Majeti R. Prospective separation of normal and leukemic stem cells based on differential expression of TIM3, a human acute myeloid leukemia stem cell marker. Proc. Natl. Acad. Sci. USA. 2011;108:5009–5014. doi: 10.1073/pnas.1100551108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ogata K., Nakamura K., Yokose N., Tamura H., Tachibana M., Taniguchi O., Iwakiri R., Hayashi T., Sakamaki H., Murai Y. Clinical significance of phenotypic features of blasts in patients with myelodysplastic syndrome. Blood. 2002;100:3887–3896. doi: 10.1182/blood-2002-01-0222. [DOI] [PubMed] [Google Scholar]
- 28.Satoh C., Tamura H., Yamashita T., Tsuji T., Dan K., Ogata K. Aggressive characteristics of myeloblasts expressing CD7 in myelodysplastic syndromes. Leuk. Res. 2009;33:326–331. doi: 10.1016/j.leukres.2008.07.006. [DOI] [PubMed] [Google Scholar]
- 29.Lo Coco F., De Rossi G., Pasqualetti D., Lopez M., Diverio D., Latagliata R., Fenu S., Mandelli F. CD7 positive acute myeloid leukaemia: a subtype associated with cell immaturity. Br. J. Haematol. 1989;73:480–485. doi: 10.1111/j.1365-2141.1989.tb00284.x. [DOI] [PubMed] [Google Scholar]
- 30.Ishikawa F., Yoshida S., Saito Y., Hijikata A., Kitamura H., Tanaka S., Nakamura R., Tanaka T., Tomiyama H., Saito N. Chemotherapy-resistant human AML stem cells home to and engraft within the bone-marrow endosteal region. Nat. Biotechnol. 2007;25:1315–1321. doi: 10.1038/nbt1350. [DOI] [PubMed] [Google Scholar]
- 31.Bonnet D., Dick J.E. Human acute myeloid leukemia is organized as a hierarchy that originates from a primitive hematopoietic cell. Nat. Med. 1997;3:730–737. doi: 10.1038/nm0797-730. [DOI] [PubMed] [Google Scholar]
- 32.Goardon N., Marchi E., Atzberger A., Quek L., Schuh A., Soneji S., Woll P., Mead A., Alford K.A., Rout R. Coexistence of LMPP-like and GMP-like leukemia stem cells in acute myeloid leukemia. Cancer Cell. 2011;19:138–152. doi: 10.1016/j.ccr.2010.12.012. [DOI] [PubMed] [Google Scholar]
- 33.Six E.M., Bonhomme D., Monteiro M., Beldjord K., Jurkowska M., Cordier-Garcia C., Garrigue A., Dal Cortivo L., Rocha B., Fischer A. A human postnatal lymphoid progenitor capable of circulating and seeding the thymus. J. Exp. Med. 2007;204:3085–3093. doi: 10.1084/jem.20071003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tjønnfjord G.E., Veiby O.P., Steen R., Egeland T. T lymphocyte differentiation in vitro from adult human prethymic CD34+ bone marrow cells. J. Exp. Med. 1993;177:1531–1539. doi: 10.1084/jem.177.6.1531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kohn L.A., Hao Q.-L., Sasidharan R., Parekh C., Ge S., Zhu Y., Mikkola H.K., Crooks G.M. Lymphoid priming in human bone marrow begins before expression of CD10 with upregulation of L-selectin. Nat. Immunol. 2012;13:963–971. doi: 10.1038/ni.2405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Haynes B.F., Mann D.L., Hemler M.E., Schroer J.A., Shelhamer J.H., Eisenbarth G.S., Strominger J.L., Thomas C.A., Mostowski H.S., Fauci A.S. Characterization of a monoclonal antibody that defines an immunoregulatory T cell subset for immunoglobulin synthesis in humans. Proc. Natl. Acad. Sci. USA. 1980;77:2914–2918. doi: 10.1073/pnas.77.5.2914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rabinowich H., Pricop L., Herberman R.B., Whiteside T.L. Expression and function of CD7 molecule on human natural killer cells. J. Immunol. 1994;152:517–526. [PubMed] [Google Scholar]
- 38.Brentjens R.J., Davila M.L., Riviere I., Park J., Wang X., Cowell L.G., Bartido S., Stefanski J., Taylor C., Olszewska M. CD19-Targeted T Cells Rapidly Induce Molecular Remissions in Adults with Chemotherapy-Refractory Acute Lymphoblastic Leukemia. Sci. Transl. Med. 2013;5:177ra38. doi: 10.1126/scitranslmed.3005930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kochenderfer J.N., Dudley M.E., Kassim S.H., Somerville R.P.T., Carpenter R.O., Stetler-Stevenson M., Yang J.C., Phan G.Q., Hughes M.S., Sherry R.M. Chemotherapy-Refractory Diffuse Large B-Cell Lymphoma and Indolent B-Cell Malignancies Can Be Effectively Treated With Autologous T Cells Expressing an Anti-CD19 Chimeric Antigen Receptor. J. Clin. Oncol. 2014;33:540–549. doi: 10.1200/JCO.2014.56.2025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lee D.W., Kochenderfer J.N., Stetler-Stevenson M., Cui Y.K., Delbrook C., Feldman S.A., Fry T.J., Orentas R., Sabatino M., Shah N.N. T cells expressing CD19 chimeric antigen receptors for acute lymphoblastic leukaemia in children and young adults: a phase 1 dose-escalation trial. Lancet. 2015;385:517–528. doi: 10.1016/S0140-6736(14)61403-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Neelapu S.S., Locke F.L., Bartlett N.L., Lekakis L.J., Miklos D.B., Jacobson C.A., Braunschweig I., Oluwole O.O., Siddiqi T., Lin Y. Axicabtagene Ciloleucel CAR T-Cell Therapy in Refractory Large B-Cell Lymphoma. N. Engl. J. Med. 2017;377:2531–2544. doi: 10.1056/NEJMoa1707447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Perna F., Berman S.H., Soni R.K., Mansilla-Soto J., Eyquem J., Hamieh M., Hendrickson R.C., Brennan C.W., Sadelain M. Integrating Proteomics and Transcriptomics for Systematic Combinatorial Chimeric Antigen Receptor Therapy of AML. Cancer Cell. 2017;32:506–519.e5. doi: 10.1016/j.ccell.2017.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Haubner S., Perna F., Köhnke T., Schmidt C., Berman S., Augsberger C., Schnorfeil F.M., Krupka C., Lichtenegger F.S., Liu X. Coexpression profile of leukemic stem cell markers for combinatorial targeted therapy in AML. Leukemia. 2018 doi: 10.1038/s41375-018-0180-3. Published online June 26, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mamonkin M., Rouce R.H., Tashiro H., Brenner M.K. A T-cell-directed chimeric antigen receptor for the selective treatment of T-cell malignancies. Blood. 2015;126:983–992. doi: 10.1182/blood-2015-02-629527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gundry M.C., Brunetti L., Lin A., Mayle A.E., Kitano A., Wagner D., Hsu J.I., Hoegenauer K.A., Rooney C.M., Goodell M.A., Nakada D. Highly Efficient Genome Editing of Murine and Human Hematopoietic Progenitor Cells by CRISPR/Cas9. Cell Rep. 2016;17:1453–1461. doi: 10.1016/j.celrep.2016.09.092. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.