Abstract
Current evidence indicates that although they are correlated, health literacy (HL) and patient activation (PA) are distinct. This article describes how HL, PA and their determinants intersect and diverge and how these concepts might inform the development of self-management interventions. The concepts of HL and PA contribute to self-management interventions in different ways. HL includes the skills and confidence required for self-management while PA focuses more on motivation and ability to take action. In this light, communication of concepts on HL and PA needs to be more widely understood by academics, researchers and policy experts as each of them plays a unique role in promoting self-management for long-term conditions such as chronic obstructive pulmonary disease.
Keywords: Behaviour, chronic obstructive pulmonary disease, health literacy, patient activation, self-management
Background
COPD self-management
Chronic obstructive pulmonary disease (COPD) self-management involves self-recognition and management of symptoms, taking medication and eating a healthy diet, coping with breathlessness, quitting smoking and engaging in regular physical exercise to maintain good health.1 Self-management interventions improve COPD health-related quality of life compared to usual care.2However, patients are often not involved in self-management activities.3,4
Patient activation (PA) (having the knowledge, skills and confidence to self-manage chronic illness and collaborate with healthcare providers5) and health literacy (HL) (understanding health information and accessing health services6) have been demonstrated to influence self-management behaviours.3
What is HL and what are its determinants?
The World Health Organization defined HL as ‘the personal characteristics and social resources needed for individuals and communities to access, understand, appraise and use information and services to make decisions about health’.7
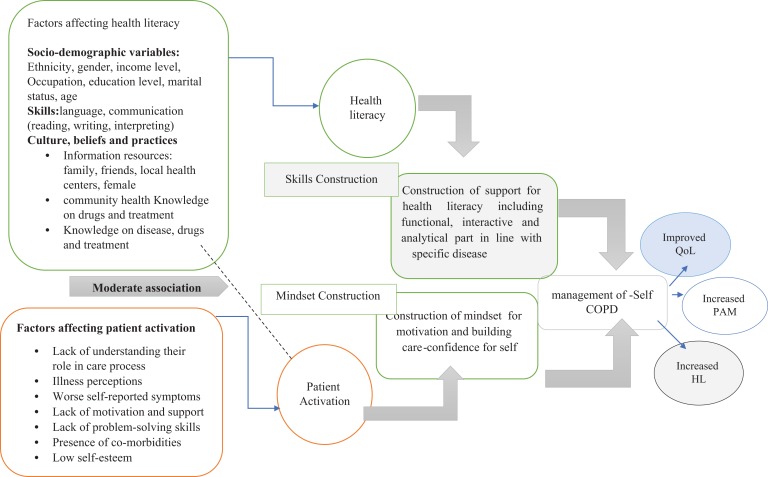
Previous researchers have identified determinants of low HL including age, educational attainment and socioeconomic status, culture beliefs and practices (Figure 2) and communication skills (including language barriers) between professionals and patients.8,9 This directly affects individual decisions, actions and their lifestyle behaviours and plays a key role in the prevention and management of chronic illness.8,10
Figure 2.
Role of health literacy and patient activation in self-management of chronic obstructive pulmonary disease (COPD).
What is PA and what are its determinants?
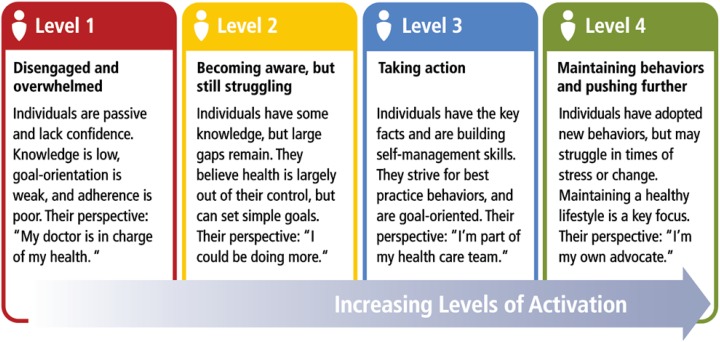
PA refers to the knowledge, skills and confidence a person has in managing their own health and care. Activation involves four stages (Figure 1): (i) believing in the patient role, (ii) building patient confidence and knowledge for self-care, (iii) taking action to maintain and improve one’s health and (iv) staying the course even under stress. Measurement of PA informs tailoring confidence building strategies.11
Figure 1.
Stages in patient activation process. ©2018 Insignia Health. Patient Activation Measure® (PAM®) Survey Levels. All rights reserved.
Previous research has reported that symptom burden, illness perception, presence of comorbidities, age, body mass index, physical health status, depression, social support, financial distress and lack of understanding their role in care process were independently associated with lower PA in COPD patients.12,13
HL and PA
Previous research was focused on the benefits of either HL or PA on health outcomes for COPD patients.14 Interventions using both concepts are limited. A clearer understanding of HL, PA and their determinants would be useful in informing COPD self-management interventions.
Evidence
HL and health outcomes
Limited HL may be a hidden problem, which could have indirect or direct impacts of health outcomes. A wealth of evidence exists which has established the link between low HL and poor health outcomes or discrepancies in health service utilization.9
A review published by Taggart et al. showed that improved HL is associated with reductions in SNAPW (smoking, nutrition, alcohol, physical activity and weight) risk behaviours for long-term chronic disease.15 Likewise, a review published in 2017 by Wang et.al showed significant reductions in COPD-related hospitalizations and patients’ emotional distress and no improvement was observed in the areas of smoking cessation, pulmonary functions and dyspnoea.16 Studies used individualized motivational interviewing and counselling; group education; combined-type intervention (combination of interventions); providing written materials; telephone coaching or counselling; and computer- or web-based online interventions.15,16 Specifically, patients with low level of HL were less likely to believe in the chronicity of their disease and more likely to have larger negative emotional representations of their illness.
PA and health outcomes
Many public health initiatives around the world have aimed at changing the behaviour of chronic disease patients by involving them in management of their own health.14
In the chronic illness care model, PA is a central concept but is the least well-developed component.17 PA leads to improvements of health outcomes among COPD patients.14 Similarly, tailored self-management programmes which are tailored to patients’ level of activation to manage their long-term conditions showed improvement in PA measured, quality of life and overall health status.18
How are HL and PA different?
Researchers have explored the association between HL and PA in both cross-sectional and prospective studies. These have shown that HL and PA are very different concepts and also function somewhat independently. Greene and colleagues showed that PA measures the patient’s self-confidence in self-management of disease whereas HL was more closely related to the ability to use information in health-relevant decisions.19 A few studies that investigated relationships of HL and PA with self-management of chronic disease conditions showed that HL and PA were weakly correlated with each other, but independently correlated with health outcomes.20,21
HL applies to broad notions of ‘declarative knowledge’ and ‘procedural knowledge’, where declarative provides factual information on health/healthcare or medicine, while procedural refers to guiding principles about the course of actions.22 PA determines the patient interest to ease them into the role of an actor in the decision-making and taking responsibility for maintaining their own health. This clearly articulates that HL provides judgemental skills and underlying knowledge about the disease conditions and their management, while PA leads to situational and psychological empowerment of patients, which is essential for behaviour change.
Programmes aimed at HL delivery assume providing a good level of knowledge/skills can empower patients, thus improves health outcomes while those aimed at PA assume that providing specific information and motivation can bring positive outcomes. This clearly posits that intervention aimed at increasing HL might not activate patient, and those aimed at improving activation need not necessarily increase HL. Figure 2 depicts the role HL and PA in self-management of COPD and is supported by concept (Figure 3) presented by Schulz et al.22
Figure 3.
Health literacy, patient activation and self-management of behaviour.
Implications for practice
In seeking to address this gap, the concepts of HL and PA need to be widely understood among the academicians, researcher and policymakers. It is equally important to use both PA and HL in self-management intervention as each of them has unique roles in improving the behaviour of the patients for management of disease.This indicates the necessity of considering both HL and PA in the design of interventions of COPD. Framing a single intervention which integrates both the concepts might result in better health outcomes.
Footnotes
Authors’ note: UNY is receipt of University International Postgraduate Scholarship (UIPA) for PhD, without which the present study could not have been completed.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The authors received financial support from Centre for Primary Health Care and Equity, UNSW for the publication of this article.
ORCID iD: Uday Narayan Yadav  https://orcid.org/0000-0002-6626-1604
https://orcid.org/0000-0002-6626-1604
References
- 1. Zwerink M, Brusse-Keizer M, van der Valk PD, et al. Self management for patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2014; 3: CD002990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lenferink A, Brusse-Keizer M, van der Valk PD, et al. Self-management interventions including action plans for exacerbations versus usual care in patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2017; 8: CD011682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bos-Touwen I, Schuurmans M, Monninkhof EM, et al. Patient and disease characteristics associated with activation for self-management in patients with diabetes, chronic obstructive pulmonary disease, chronic heart failure and chronic renal disease: a cross-sectional survey study. PLoS One 2015; 10(5): e0126400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Schoen C, Osborn R, Squires D, et al. New 2011 survey of patients with complex care needs in eleven countries finds that care is often poorly coordinated. Health Aff (Millwood) 2011; 30(12): 2437–2448. [DOI] [PubMed] [Google Scholar]
- 5. Greene J, Hibbard J, Hibbard H. Why does patient activation matter? An examination of the relationships between patient activation and health-related outcomes. J Gen Intern Med 2012; 27(5): 520–526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Sorensen K, Broucke SV, Fullam J, et al. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health 2012; 12: 80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. World Health Organization. Health Promotion Track 2: health literacy and health behaviour. Available at: http://www.who.int/healthpromotion/conferences/7gchp/track2/en/ (accessed 14 June 2018).
- 8. Jayasinghe UW, Harris MF, Parker SM, et al. The impact of health literacy and life style risk factors on health-related quality of life of Australian patients. Health Qual Life Outcomes 2016; 14(1): 68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Singleton K, Krause EM. Understanding cultural and linguistic barriers to health literacy. Ky Nurse 2010; 58(4): 4, 6–9. [PubMed] [Google Scholar]
- 10. Dewalt DA, Berkman ND, Sheridan S, et al. Literacy and health outcomes: a systematic review of the literature. J Gen Intern Med 2004; 19(12): 1228–1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hibbard JH, Mahoney ER, Stockard J, et al. Development and testing of a short form of the patient activation measure. Health Serv Res 2005; 40(6 Pt 1): 1918–1930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Korpershoek Y, Bos-Touwen ID, de Man-van Ginkel JM, et al. Determinants of activation for self-management in patients with COPD. Int J Chron Obstruct Pulmon Dis 2016; 11: 1757–1766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. os-Touwen I, Schuurmans M, Monninkhof EM, et al. Patient and disease characteristics associated with activation for self-management in patients with diabetes, chronic obstructive pulmonary disease, chronic heart failure and chronic renal disease: a cross- sectional survey study. PLoS One 2015; 10(5): e0126400 DOI: 10.1371/journal.pone.0126400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Yadav UN, Hosseinzadeh H, Baral KP. Self-management and patient activation in COPD patients: an evidence summary of randomized controlled trials. Clinical Epidemiology and Global Health. 2017; 6(3): 148–154. [Google Scholar]
- 15. Taggart J, Williams A, Dennis S, et al. A systematic review of interventions in primary care to improve health literacy for chronic disease behavioral risk factors. BMC Fam Pract 2012; 13: 49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wang T, Tan JY, Xiao LD, et al. Effectiveness of disease-specific self-management education on health outcomes in patients with chronic obstructive pulmonary disease: an updated systematic review and meta-analysis. Patient Educ Couns 2017; 100(8): 1432–1446. [DOI] [PubMed] [Google Scholar]
- 17. Stuckey HL, Adelman AM, Gabby RA. Improving care by delivering the chronic care model for diabetes. Diabetes Manage 2011; 1(1): 37–52. [Google Scholar]
- 18. Turner A, Anderson JK, Wallace LM, et al. An evaluation of a self-management program for patients with long-term conditions. Patient Educ Couns 2015; 98(2): 213–219. [DOI] [PubMed] [Google Scholar]
- 19. Greene J, Hibbard J, Tusler M. How much do health literacy and patient activation contribute to older adults’ ability to manage their health? https://assets.aarp.org/rgcenter/health/2005_05_literacy.pdf (2005). [Google Scholar]
- 20. Smith SG, Curtis LM, Wardle J, et al. Skill set or mind set? Associations between health literacy, patient activation and health. PLoS One 2013; 8(9): e74373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Couture EM, Chouinard MC, Fortin M, et al. The relationship between health literacy and patient activation among frequent users of healthcare services: a cross-sectional study. BMC Fam Pract 2018; 19: 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Schulz PJ, Nakamoto K. Health literacy and patient empowerment in health communication: the importance of separating conjoined twins. Patient Educ Couns 2013; 90(1): 4–11. [DOI] [PubMed] [Google Scholar]