Abstract
Dental treatment of young pediatric patients can be confounded by lack of cooperation for dental rehabilitation procedures and even examination and/or radiographs. With the recent US Food and Drug Administration warning applied to many anesthetic/sedative agents for children less than 3 years old, a retrospective review of general anesthesia (GA) cases from 1 private pediatric dental practice was studied for age, gender, body mass index, anesthetic duration, airway management used, extent of dental surgical treatment, recovery time, and cardiac/pulmonary complications. For the 2016 calendar year, 351 consecutive GA cases were identified with patients aged 2–13 years. Of these, 336 underwent nasal endotracheal intubation. Forty-six of 351 patients (13%) were younger than 3 years. Median anesthesia duration was approximately 1.7 hours for all age groups. Dental treatment consisting of 8–9 teeth including crowns, fillings, and extractions was most frequently encountered. One hundred sixty-eight patients (48%), however, required care for 10–18 teeth. There were no episodes of significant oxygen desaturation. The overall complication rate was 1.1%, with 2 cases of postextubation croup, 1 case of mild intraoperative bronchospasm, and 1 case of intraoperative bradycardia. Complications did not correlate with children being overweight or obese.
Key Words: Brain developmental delay, General anesthesia, Pediatrics anesthesia, Endotracheal intubation, Laryngeal mask airway, Recovery time from anesthesia
General anesthesia (GA) or deep sedation is often required to complete necessary dental radiographs and/or treatment in young, uncooperative children. Treatment can be completed in either the hospital, ambulatory surgery center, or office setting. Despite the low incidence of adverse outcomes from GA, deep sedation, or moderate sedation in the dental office setting, treatment can be safely and efficiently completed with well-trained providers following established protocols and guidelines.
The maximum dental surgical working time for the most commonly used pediatric enteral moderate sedation technique with midazolam can be as short as 20–30 minutes, be only partially effective but allow treatment completion, or be ineffective. If the treatment plan cannot be completed in 1 sedation visit, alternatives may include physical immobilization, using a different moderate sedation technique, or GA. Supplemental dosing with additional or different oral medication(s) is ill advised for moderate sedation because gastric absorption is very unpredictable and unintended deep sedation is more likely. With GA, all necessary dental procedures can be completed in just 1 visit.
Recently, a US Food and Drug Administration (FDA) warning of December 14, 2016, announced that exposure to certain sedatives and general anesthetics may affect brain development of children under the age of 3, especially for procedures longer than 3 hours.1 For several years now, the potential for either reversible or even permanent impairment of brain development has been discussed without definitive conclusions.2 Although the data in animals and humans are still being developed, expert opinion differs as to what recommendations should be made.3 Some studies have not found a relationship between anesthetic exposure and age,4 whereas others have shown effects only with multiple exposures.5 This official warning has recently been included in manufacturers' package inserts for 11 commonly used GA and sedative drugs: volatile inhalation agents including halothane, desflurane, isoflurane, and sevoflurane; intravenous anesthetics including propofol, methohexital, and etomidate; ketamine; and sedative hypnotics including lorazepam (injection), midazolam (injection and syrup), and pentobarbital.1 How this will affect clinical dental anesthesia practice in the future is unclear.
We therefore reviewed 1 year of GA cases in our private practice to determine:
The number of children who would be impacted by the FDA warning with respect to age and duration of GA.
Patient demographics, including height, weight, and body mass index (BMI), which may affect the course of anesthesia.
The type of airway management technique utilized along with the type of anesthetics used.
The number of airway, pulmonary, and/or cardiac complications.
METHODS
A retrospective review of 1 year's pediatric GA cases from January 1 to December 31, 2016, was undertaken. Records were reviewed from 1 office-based practice with 2 locations. All dental treatment was performed by 1 of 2 board-certified pediatric dentists or 1 general dentist who treats children and adults. GA was provided by 1 of 2 dentist anesthesiologists. GA for dental examination, radiographs, and complete treatment was deemed necessary in our practice if children were considered unable to cooperate, precooperative, or with physical and/or mental impairment that inhibited cooperation based on the expert opinion of the treating dentist. All chart identifiers were redacted from the studied charts. Informed consent was not deemed necessary for this deidentified retrospective study.
The children were grouped into 3 age brackets: group 1, less than 3 years of age; group 2, 3 to 6 years of age; and group 3, over 6 up to 13 years of age.
Collected data included the physical characteristics of height, weight, age, and gender as well as calculated BMI from pediatrician medical evaluations. Additional collected data included type of airway management, duration of GA, duration of recovery room stay, and the amount of dental treatment documented based on the number of teeth crowned, filled, or extracted (CFXT). The complexities of the specific dental surgery and which teeth were treated were not studied.
Airway management techniques included nasal endotracheal intubation, flexible laryngeal mask airway (LMA), or open (natural) airway with nasal cannula. Cases estimated to take longer than 45 minutes were planned for intubation, but the decision of which technique would be used was ultimately determined by the dentist anesthesiologist in consultation with the dental surgeon.
Endotracheal GA was performed with sevoflurane mask induction, and after obtaining intravenous access, atropine or glycopyrrolate and rocuronium for intubation, with isoflurane maintenance with the addition of propofol continuous infusion at 50 mcg/kg/min. When an LMA was utilized, sevoflurane induction was performed prior to LMA placement with titrated propofol infusion for maintenance. In the open-airway group, sevoflurane was used for induction only, and after intravenous access was obtained, propofol was infused at approximately 75 mcg/kg/min with intermittent boluses as needed. Opioids and benzodiazepines were not used in any patient in an attempt to reduce recovery time and to promote rapid awakening and timely discharge. Local anesthesia use was at the discretion of the operating dentist. Generally, infiltration local anesthesia was always utilized when pulpotomies, stainless steel crowns, or extractions were performed. Local anesthesia was rarely utilized for teeth requiring routine restorative treatment.
A pulmonary anesthetic complication was considered significant if any patient developed episode(s) of oxygen desaturation lower than 92% for longer than 30 seconds, and this was recorded. Significant cardiovascular events were also recorded.
RESULTS
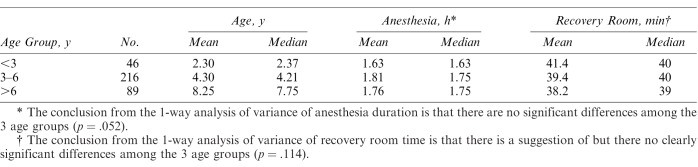
This review identified 351 ASA 1 or 2 patients who required GA out of a total of 3661 patients (9.6%) seen in that year. The age breakdown included 46 in group 1 (13.1%), including 4 children younger than 2 years; 216 in group 2; and 89 in group 3 (Table 1). In group 3, there were 11 children age 9 to 13 years who were classified as physically and/or intellectually impaired because of severe autism or cerebral palsy as well as Rhett, Angelman, or Down syndrome with no underlying cardiac or pulmonary disease. There were 208 boys and 143 girls (Table 2). BMI was calculated from height and weight. Thirty-three (9.4%; Figure 1) had a BMI of 21 or higher. Patients were considered overweight or obese based upon BMI and age-related Centers for Disease Control and Prevention predictive growth charts (Table 2). Greater than 95th percentile was considered obese and 85th–95th percentile was considered overweight (Table 2). Based on these criteria, of the 33 patients with BMI over 20, 21 were overweight and 12 were obese.
Table 1.
Duration of Anesthesia and Recovery Room Time
Table 2.
Number of Treated Subjects: Gender, Weight
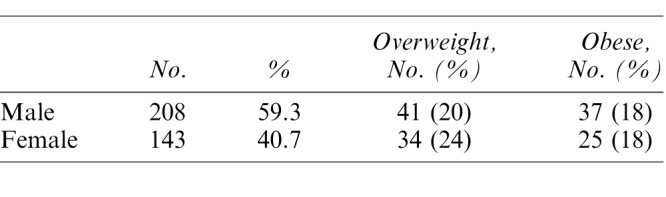
Figure 1.
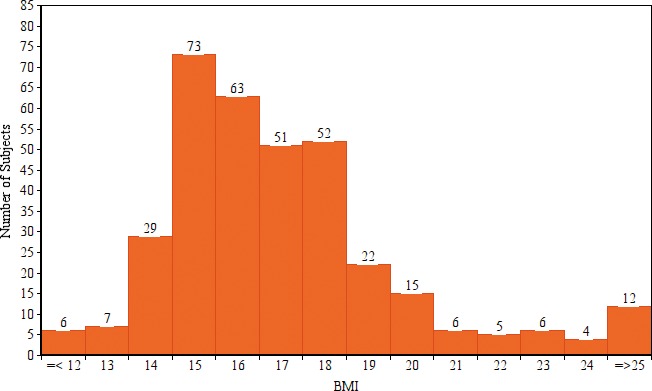
Number of treated subjects by body mass index (BMI).
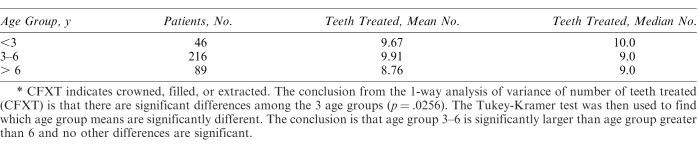
The average and median durations of GA were 1.77 and 1.75 hours (Table 1), and durations ranged from 0.8 to over 3 hours (Figure 2). Eighty-nine patients (25.4%) required less than 1.5 hours of GA. There were 3 patients, a 10-year-old girl and two 6-year-old girls, requiring longer than 3 hours of GA. Over 98.6% of the 351 patients underwent GA for more than 45 minutes (Figure 2). The average number of teeth CFXT was approximately 9 in all age groups (Table 3, Figure 3). However, 168 patients (48%) had dental procedures on 10–18 teeth (Figure 3).
Figure 2.
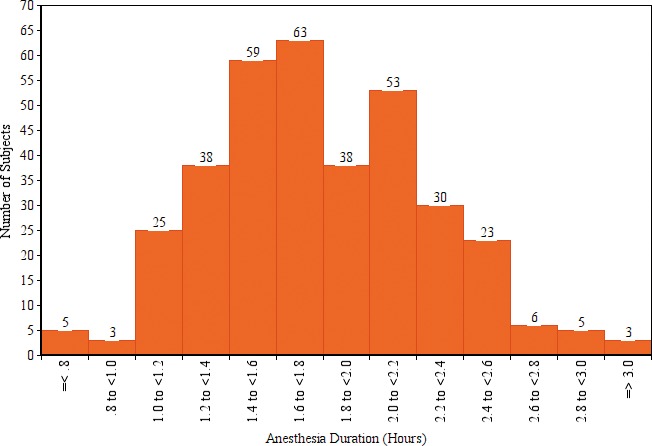
Number of treated subjects with general anesthesia duration (hours).
Table 3.
No. of Teeth Treated (CFXT) by Age Group*
Figure 3.
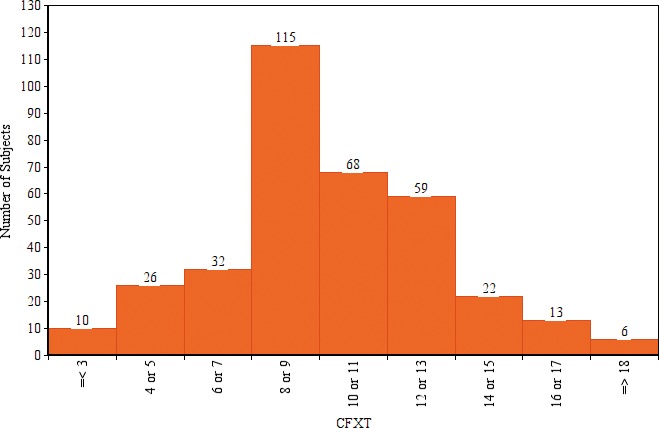
Number of treated subjects by number of teeth treated (crowned, filled, or extracted [CFXT]).
Airway Management
The decision on the type of airway technique used was generally based on the complexity of the dental surgery, estimated length of anesthesia/surgery time, and anticipated airway difficulty during surgery. Nasal endotracheal intubation was performed on 336 patients, flexible LMA on 13 patients, and open airway with capnographic/O2 nasal cannula on 2 patients. Two of the 4 patients under the age of 2 were treated with nasal cannula and the other 2 with flexible LMA. The CFXT treatment needs of these 4 precooperative children under age 2 were considered extensive for their age and included treatment for 8 teeth in 2 patients and 7 teeth and 5 teeth each in 1 patient.
Once the anesthesia was induced, there were no significant changes needed in airway technique in any of the 351 cases reviewed. In 1 case a larger, 6.0-mm uncuffed endotracheal tube was placed because of excessive air leak with a 5.5-mm internal diameter tube. There were no other airway technique difficulties in any of the 3 groups.
Anesthesia Recovery
The postanesthesia recovery time ranged from less than 25 to over 65 minutes, with a median of approximately 40 minutes (Figure 4). Patients were considered ready for discharge when vital signs were stable, chest auscultation was normal, and they could drink water or eat a popsicle. The average time spent in the recovery room did not vary significantly based on age (Table 1). Prolonged stay (considered over 60 minutes) was documented in only 3 patients, all of whom were in the older group.
Figure 4.
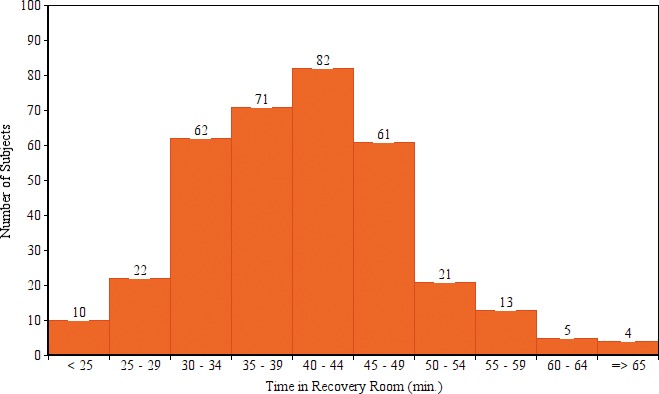
Number of treated subjects by time in recovery room (minutes).
Complications
No patients developed episodes of oxygen desaturation for longer than 30 seconds or lower than 92% during either induction or emergence. All 3 airway complications occurred in the intubation group. Postextubation croup was successfully treated with racemic epinephrine in 2 patients (0.6%). These 2 patients, a 2.4-year-old girl and a 3.6-year-old boy, were monitored in the recovery room for longer than the average. One patient, a 4.6-year-old girl, developed mild wheezing intraoperatively and was successfully treated with in-line albuterol nebulization between the endotracheal tube and the anesthesia circuit. A 12-year-old patient with Down syndrome developed significant bradycardia into the low 40s beats per minute within 2 minutes after mask sevoflurane induction, which occurred just prior to intravenous line placement with subsequent administration of atropine. This was a sudden but not unexpected complication with this medical condition.6,7 Considering these 4 cases, the overall complication rate was 4/351 (1.1%).
DISCUSSION
The FDA warning about possible impaired brain development after exposure of children under age 3 to certain general anesthetics or sedatives, particularly for procedures lasting more than 3 hours, has generated interest across the anesthesia-provider community. It is not clear whether the anesthetic agents alone, the stress of the surgical procedure, or some adverse anesthetic event, such as short periods of arterial oxygen desaturation or hypotension, may contribute to possible impaired brain development. Data are still inconclusive regarding both susceptible age and duration of anesthetic exposure. Several studies are currently being done to shed more information on these concerns.
Not knowing the scope of the dental population that might be affected by this warning, a retrospective record review from a busy pediatric dental practice was undertaken. Most patients identified for GA in this retrospective record review were between 3 and 6 years in age and thus not affected by the FDA warning. However, 13% (46/351) were under age 3 and, after evaluation, considered unable to cooperate for extensive dental treatment. This is a significant number of patients that could potentially have care withheld if the warnings dissuade practitioners from treating this group of children with GA.
All age groups had an average of nearly 10 teeth per patient treated. This would require multiple oral sedations with unpredictable effectiveness. In our study 48% had 10–18 teeth treated; such cases are considered extensive treatment plans, frequently requiring GA. It is possible that in selected cases, the application of topical silver diamine fluoride might have either allowed decreased operative time or delayed treatment until a patient attained 3 years of age. However, once the patient was determined to require GA, definitive dental treatment was deemed preferable because of extensive caries.
When considering whether to use open-airway versus flexible LMA versus endotracheal intubation, the anesthesia care provider must consider potential complications that are uniquely different. Nasal intubation and LMA placement were generally uncomplicated in this study. However, 2 patients did develop postextubation croup, which was easily managed. Passage of a nasal endotracheal tube by expert dentist anesthesiologists only very occasionally produces nasal bleeding or requires passage of the tube over a catheter into the oropharynx to negotiate the adenoids or posterior pharyngeal wall obstruction prior to the tube's eventual placement into the trachea. The LMA can produce mild trauma to the soft palate or epiglottis or inaccurate placement over the glottic opening. In this situation, mild to moderate airway obstruction can occur. Laryngospasm and/or aspiration are the main risks of open-airway anesthesia.
In 1 study reviewing nearly 50,000 “medical” open-airway propofol sedation/anesthetics with other drugs added, 1 in 65 cases was associated with stridor, laryngospasm, obstruction, wheezing, or apnea necessitating airway interventions.8 In a dental oral sedation study of 111 healthy children 24–84 months old, mean age 47 months, with a 3-drug cocktail, 3% had adverse events, 23% had unsatisfactory outcomes, and 5% were stopped because of disruptive behavior and later returned for repeat sedation attempts.9
Another study compared 922 oral sedations with a variety of drugs to a cohort group of 140 general anesthetics with endotracheal intubation or LMA for MRI or CT examination without an invasive radiologic intervention being performed. In the oral sedation group, there was an overall 28% failure rate to complete the imaging. Of the 28%, there was inadequate sedation in 16%, failed sedation in 7%, desaturation-hypoxemia in 3%, and in 2% other reasons for failure. In contrast, in all 140 general anesthetic cases with LMA or endotracheal intubation, there was only 1 incident of laryngospasm in 140 cases (0.7%), and it was the only complication to occur.10 All the scans were successfully completed. Radiographic examination is not considered as invasive as dental surgery.
Although only 2 of our cases were open airway, we find that success with that technique requires continuous support of the airway by either the anesthesia care provider, the operating dentist, or the assistant. Airway readjustment is often required, which might be especially challenging for lengthy cases, as was commonly seen in this study. Augmenting ventilation, should the need arise, requires interruption of the dental procedure and can obviously not be done during dental treatment.
Some literature references correlate being overweight and/or obese with an increased incidence of perioperative complications, particularly difficult airway management, upper-airway obstruction, and prolonged stays in the postanesthesia care unit of more than 3 hours.11 This cited study included 6094 children with a mean BMI of 21.6 and combined incidence of overweight and obesity of 31.6%. Another study of 2170 children undergoing adenotonsillectomy positively correlated intraoperative desaturation, multiple attempts at laryngoscopy, and difficult mask ventilation with being overweight or obese.12 The overall incidence of overweight/obese children was 20.7%. However, in our study, there were no similar perioperative complications in the overweight or obese patients to support these study findings.
CONCLUSION
In this study, 13.1% of 351 patients who underwent GA from January 1 through December 31, 2016, in a private dental practice were under age 3, thus falling within the recent FDA warning regarding the use of anesthetics/sedatives. None of the cases was over 3 hours in duration for this age group. All the dental treatment for the 351 patients was completed uneventfully in 1 visit and no child needed to return for another anesthetic exposure. No serious anesthetic complications were encountered.
ACKNOWLEDGMENT
The statistical analysis was completed by Dennis House, MS, medical statistician, Chapel Hill, North Carolina.
REFERENCES
- 1.FDA drug safety communication: FDA review results in new warnings about using general anesthetics and sedation drugs in young children and pregnant women. Available at: www.fda.gov/drugs/drugsafety/ucm532356 Accessed December 14, 2016.
- 2.Andropoulos DB, Green MF. Anesthesia and developing brains—implications of the FDA warning. N Engl J Med. 2017;376:905–907. doi: 10.1056/NEJMp1700196. [DOI] [PubMed] [Google Scholar]
- 3.Backeljauw B, Holland SK, Altaye M, Loepke AW. Cognition and brain structure following early childhood surgery with anesthesia. Pediatrics. 2015;136:e1–e12. doi: 10.1542/peds.2014-3526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sun LS, Li G, Miller TL, et al. Association between a single general anesthesia exposure before age 36 months and neurocognitive outcomes in later childhood. JAMA. 2016;315:2312–2320. doi: 10.1001/jama.2016.6967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wilder RT, Flick RP, Sprung J, et al. Early exposure to anesthesia and learning disabilities in a population-based birth cohort. Anesthesiology. 2009;110:796–804. doi: 10.1097/01.anes.0000344728.34332.5d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kraemer FW, Striker PA, Gumaney HG, et al. Bradycardia during induction of anesthesia with sevoflurane in children with Down's syndrome. Anesth Analg. 2010;111:1259–1263. doi: 10.1213/ANE.0b013e3181f2eacf. [DOI] [PubMed] [Google Scholar]
- 7.Borland LA, Colligan J, Brandom BW. Frequency of anesthesia related complications in children with Down's syndrome under general anesthesia for noncardiac procedures. Pediatr Anesthesiol. 2004;14:733–738. doi: 10.1111/j.1460-9592.2004.01329.x. [DOI] [PubMed] [Google Scholar]
- 8.Cravero JP, Beach ML, Bilke GT, et al. The incidence and nature of adverse events during pediatric sedation/anesthesia with propofol outside the operating room: a report from the pediatric sedation research consortium. Pediatr Anesthesiol. 2009;108:795–804. doi: 10.1213/ane.0b013e31818fc334. [DOI] [PubMed] [Google Scholar]
- 9.Leelataweedwud P, Vann W. Adverse events and outcomes of conscious sedation for pediatric patients: study of an oral sedation regime. J Am Dent Assoc. 2001;132:1531–1539. doi: 10.14219/jada.archive.2001.0086. [DOI] [PubMed] [Google Scholar]
- 10.Malviya S, Voepel-Lewis OP, Eldevik DT. Sedation and general anaesthesia in children undergoing MRI and CT: adverse events and outcomes. Br J Anaesth. 2000;84:743–748. doi: 10.1093/oxfordjournals.bja.a013586. [DOI] [PubMed] [Google Scholar]
- 11.Nafiu OO, Reynolds PI, Bamgbade OA, et al. Childhood body mass index and perioperative complications. Paediatr Anaesth. 2007;17:426–430. doi: 10.1111/j.1460-9592.2006.02140.x. [DOI] [PubMed] [Google Scholar]
- 12.Nafui OO, Green GE, Walton S, et al. Obesity and risk of peri-operative complications in children presenting for adenotonsillectomy. Int J Pediatr Otorhinolaryngol. 2009;73:89–95. doi: 10.1016/j.ijporl.2008.09.027. [DOI] [PubMed] [Google Scholar]