Abstract
Background
Cesarean rates are higher in women admitted to labor ward during early stages rather than at later stages of labor. In a study in Germany, crude cesarean rates among Turkish and Lebanese immigrant women were low compared to non-immigrant women. We evaluated whether these immigrant women were admitted during later stages of labor, and if so, whether this explains their lower cesarean rates.
Methods
We enrolled 1413 nulliparous women with vertex pregnancies, singleton birth, and 37+ week of gestation, excluding elective cesarean deliveries, in three Berlin obstetric hospitals. We applied binary logistic regression to adjust for social and obstetric factors; and standardized coefficients to rank predictors derived from the regression model.
Results
At the time of admission to labor ward, a smaller proportion of Turkish migrant women was in the active phase of labor (cervical dilation: 4+ cm), compared to women of Lebanese origin and non-immigrant women. Rates of cesarean deliveries were lower in women of Turkish and Lebanese origin (15.8 and 13.9%) than in non-immigrant women (23.9%). In the logistic regression analysis, more advanced cervical dilatation was inversely associated with the outcome cesarean delivery (OR: 0.76, 95%CI: 0.70–0.82). In addition, higher maternal age (OR: 1.06, 95%CI: 1.04–1.09), application of oxytocic agents (OR: 0.55, 95%CI: 0.42–0.72), and obesity (OR: 2.25, 95%CI: 1.51–3.34) were associated with the outcome. Ranking of predictors indicate that cervical dilatation is the most relevant predictor derived from the regression model.
Conclusions
Advanced cervical dilatation at the time of admission to labor ward does not explain lower emergency cesarean delivery rates in Turkish and Lebanese migrant women, despite the fact that this is the strongest among the predictors for emergency cesarean delivery identified in this study.
Keywords: Maternal obesity, Gestational weight gain, Fetal macrosomia, Cesarean delivery, Immigrant women
Background
Rates of cesarean delivery worldwide are high and still rising. Depending on study region rates between 27.3 and 33.0% are reported [1–7]. Evidence shows that cesarean rates are higher in women admitted to the labor ward during the early stages of labor (i.e. with beginning cervical dilatation) than in those who were admitted at a later stage (i.e. with advanced cervical dilatation) [8–11], e.g. 10.3% vs. 4,2% [8] and 21.8% vs. 14.5% [11]. Moreover, Cheng et al. [12] found an increasing risk of cesarean delivery in association with the length of the first stage of labor; the longer the first stage, the higher the risk.
Cesarean rates are often higher in women who immigrated than in women born in the receiving country [13]. However, rates are not homogeneous in immigrant women of different origin. For example, women from sub-Saharan Africa are more likely to deliver by cesarean delivery than immigrant women from other low- and middle-income countries [14]. Disparities in cesarean birth rates between immigrant and non-immigrant women may occur because of non-medical factors such as communication barriers, less support and/or care practices during labor and delivery, female genital cutting, or cultural preference [15–17]. A different ethnicity or race thus is seen as a risk marker for cesarean delivery in women even if they have no obstetric risk factors [18, 19].
Findings regarding migrant status as risk factor for cesarean delivery are not consistent, however. David et al. [20] report that 1st generation immigrant women from Turkey and Lebanon delivering in Berlin/Germany had considerably lower crude rates of cesarean delivery (21.9 and 22.2%) than non-immigrant women (39.2%); the cesarean rates among 2nd and 3rd generation women were similar to those of non-immigrant women. To identify possible reasons for these unexpected findings we here assess 1) whether immigrant women from Turkey and Lebanon were admitted during later stages of labor (measured by advanced cervical dilatation) than non-immigrant women; and 2) whether later admission can explain lower cesarean rates in immigrant women – taking potential confounders (age, educational attainment, body weight, oxytocic agent) into account.
Methods
Setting, instruments, sample
We recruited women delivering in three secondary and tertiary care maternity hospitals of Berlin/Germany ((1) the Virchow Campus site of the Charité University Hospital, (2) the Vivantes Klinikum am Urban, and (3) the Vivantes Klinikum Neukölln) in a 12-month period 2011/12 (n = 8157). Minors (n = 105, 1.3%), tourists not resident in Germany (n = 24, 0.3%), women terminating a pregnancy, and women with miscarriages and stillbirths (fetal death in utero ascertained at hospital admission and before onset of labor, n = 106, 1.3%) were excluded. It was not possible to contact 363 women despite multiple attempts. Of the remaining 7559 women 381 declined to participate. We conducted face-to-face interviews and linked them with highly standardized obstetric process and outcome data from hospital databases. Linkage of available interview data with obstetric process and outcome data failed in 72 cases. Six women did not consent to the linkage of data sources. In total, 7100 women participated (response rate of 89.6%). This corresponded to 7334 birth data records because of twin and triplet births.
For the analysis presented here, we considered only nulliparous women with vertex pregnancies and singleton birth, 37th week of gestation onwards. Women with elective cesarean delivery were excluded as they are not informative for our study question. We further restricted the sample to women with own migration experience (1st generation immigrants). Migrant women are a heterogeneous group. Health differences in this group might be larger than between migrant and non-migrant women. For this reason we selected women originating from Turkey and Lebanon (the two largest and only immigrant groups that allow separate analysis) and to women without a migration history (non-immigrant women). Also, 63 women without data on cervical dilatation were removed from analyses (see Fig. 1).
Fig. 1.

Flowchart of case recruitment, Berlin Perinatal study, 2011/12
In the original study, interviews were conducted with each subject at two time points: on admission to the delivery room (T1) and on the second or third day postpartum in the maternity wards (T2). Questionnaires were available in German, Turkish, Kurdish, Arabic, and other languages. Translators were involved in case of language barriers. Nearly all women with migration background (193 of 205) were able to communicate with the obstetrician in German. For this analysis, only T1 data was used. Formally, the analyses reported here are secondary analyses as the original study question related to pregnancy outcomes such as frequeny of cesarean deliveries [20].
Variables and statistical analysis
Cesarean delivery
The outcome variable was dichotomized, with “yes” comprising emergency cesarean delivery incl. crash cesarean; and “no” comprising normal vaginal delivery, forceps, and vacuum extraction.
Covariates
Covariates comprised known medical risk factors for the outcome. BMI (at admission) was coded as dummy variable: < 25 kg/m2, 25 - < 30 kg/m2, and ≥ 30 kg/m2. Medical treatment with an oxytocic agent was included as dichotomous variable. Age of pregnant women (continuous) and migration status (non-immigrant women, Turkish migrant women, Lebanese migrant women) were also included as covariates. Furthermore, we adjusted for confounding by socioeconomic factors by the best available proxy, educational attainment, measured by the highest graduation level. The variable was categorized into low (no education/primary school), medium (secondary education), and high attainment (technical collage/vocational school, a-level vocational diploma). Additionally, documented values of cervical dilatation (ranged from 0 cm to 10 cm) were used as continuous variable in the multivariate analysis.
Treatment of missing data
Among the final sample (n = 1413) information on maternal weight at the time of birth was missing in 8.6% (n = 122), and information on height in 11.0% (n = 156) of women. We assumed that missing data had occurred at random, i.e., that missings were not influenced by unobserved data. We applied imputation procedures using the average of five iterations with IVEware [21]. Imputation of maternal height was based on migration status and age; imputations of maternal weight were based on migration status, age, and height. Results of an analysis without imputed data do not differ substantially from the results given in Table 1 and Table 2 (see appendix, Table 4 and Table 5).
Table 1.
Characteristics of the selected subsample of women, by migration status
| Turkish origin | Lebanese origin | Non-immigrants | |
|---|---|---|---|
| N | 133 | 72 | 1208 |
| Age in years *** 1) | |||
| Median (range) | 25 (18–45) | 24 (18–41) | 30 (18–44) |
| Highest educational level (%) *** 2) | |||
| No qualification/primary school | 36 (27.1%) | 14 (19.4%) | 28 (2.3%) |
| Secondary school | 72 (54.1%) | 34 (47.2%) | 530 (43.9%) |
| University / technical collage / vocational school / a-level vocational diploma | 25 (18.8%) | 24 (33.3%) | 650 (53.8%) |
| Body Mass Index at admission (%) n.s. 2) | |||
| BMI < 25 kg/m2 | 17 (12.8%) | 17 (23.6%) | 235 (19.5%) |
| BMI < 30 kg/m2 | 66 (49.6%) | 28 (38.9%) | 546 (45.2%) |
| BMI ≥30 kg/m2 | 50 (37.6%) | 27 (37.5%) | 427 (35.4%) |
| Oxytocic agent n.s. 2) | |||
| Yes (%) | 74 (55.6%) | 33 (45.8%) | 611 (50.6%) |
| Cervical dilatation * 2) | |||
| Median (range) in cm | 2 (0–8) | 2 (0–10) | 2 (0–10) |
| Active phase of labor (≥4 cm) in % | 21 (15.8%) | 19 (26.4%) | 315 (26.1%) |
| Delivery mode (%) ** 2) | |||
| Normal vaginal delivery | 75 (56.4%) | 52 (72.2%) | 685 (56.7%) |
| Vacuum extraction / forceps | 37 (27.8%) | 10 (13.9%) | 234 (19.4%) |
| Emergency cesarean delivery | 21 (15.8%) | 10 (13.9%) | 289 (23.9%) |
| Obstetric complications | All participants (1403) | ||
| HELLP-Syndrome | 6 (0.4%) | ||
| Eclampsia | 0 | ||
| Hemorrhage > 1000 ml | 23 (1.6%) | ||
| Sepsis | 0 | ||
| Cardiovascular complications | 0 | ||
| Uterine rupture | < 5 ** | ||
* p < 0.05, ** p < 0.01, *** p < 0.001
1) Kruskal-Wallis test
2) Chi-square test
** no detailed data due to data protection
Table 2.
Indications for cesarean delivery
| Rank | Turkish origin | N (%) | Lebanese origin | N (%) | Non-immigrant women | N (%) |
|---|---|---|---|---|---|---|
| 1 | Pathological CTG or auscultatory bad fetal heart tones | 40 (30.1) | Pathological CTG or auscultatory bad fetal heart tones | 17 (23.6) | Pathological CTG or auscultatory bad fetal heart tones | 317 (26.8) |
| 2 | Protracted labor/obstructed labor in the expulsion stage | 18 (13.5) | Green amniotic fluid | 5 (6.9) | Protracted labor/obstructed labor in the expulsion stage | 148 (12.3) |
| 3 | Protracted labor/obstructed labor in the dilation stage | 9 (6.8) | Chorioamnionitis syndrome | 4 (6.0) | Protracted labor/obstructed labor in the dilation stage | 72 (6.6) |
| 4 | Chorioamnionitis syndrome | 6 (4.5) | Protracted labor/obstructed labor in the dilation stage | 4 (6.0) | Green amniotic fluid | 43 (3.6) |
| 5 | Green amniotic fluid | 3 (2.3) | Protracted labor/obstructed labor in the expulsion stage | 4 (6.0) | Absolute or relative imbalance between child‘s head and mother‘s pelvis | 29 (2.4) |
Category “other birth risks” was not considered
Table 4.
Sensitivity analysis: Characteristics of the selected subsample of women, by migration status
| Turkish origin | Lebanese origin | Non-immigrants | |
|---|---|---|---|
| N | 109 | 53 | 1046 |
| Age in years *** 1) | |||
| Median (range) | 25 (19–45) | 24 (19–40) | 30 (18–44) |
| Highest educational level (%) *** 2) | |||
| No qualification/primary school | 27 (24.8%) | 10 (18.9%) | 23 (2.2%) |
| Secondary school | 64 (58.7%) | 24 (45.3%) | 446 (42.6%) |
| University / technical collage / vocational school / a-level vocational diploma | 16 (16.5%) | 19 (35.9%) | 557 (55.2%) |
| Body Mass Index at admission (%) n.s. 2) | |||
| BMI < 25 kg/m2 | 14 (12.8%) | 13 (25.5%) | 198 (18.9%) |
| BMI < 30 kg/m2 | 53 (48.6%) | 21 (39.6%) | 484 (46.3%) |
| BMI ≥30 kg/m2 | 42 (38.5%) | 19 (35.9%) | 364 (34.8%) |
| Oxytocic agent n.s. 2) | |||
| Yes (%) | 60 (55.1%) | 24 (45.3%) | 517 (49.4%) |
| Cervical dilatation * 2) | |||
| Median (range) in cm | 1 (0–8) | 2 (0–10) | 2 (0–10) |
| Active phase of labor (≥4 cm) in % | 17 (15.6%) | 14 (26.4%) | 275 (26.3%) |
| Delivery mode (%) * 2) | |||
| Normal vaginal delivery | 60 (55.1%) | 37 (69.8%) | 591 (56.5%) |
| Vacuum extraction / forceps | 30 (27.5%) | 9 (17.0%) | 198 (18.9%) |
| Emergency cesarean delivery | 19 (17.4%) | 7 (13.2%) | 257 (23.9%) |
* p < 0.05, ** p < 0.01, *** p < 0.001
1) Brown-Mood test
2) Chi-square test
Table 5.
Sensitivity analysis: Odds ratios of emergency cesarean delivery among selected subsample of women, adjusted logistic regression model
| Variable | OR | 95% CI | p-Value | Standardized estimates |
|---|---|---|---|---|
| Cervical dilatation (continuous) | 0.78 | 0.72–0.84 | < 0.0001 | 0.305 |
| Maternal age (continuous) | 1.06 | 1.03–1.09 | < 0.0001 | 0.195 |
| 1st generation Turkish migrants * | 0.64 | 0.36–1.14 | 0.1305 | 0.071 |
| 1st generation Lebanese migrants * | 0.59 | 0.26–1.37 | 0.2224 | 0.059 |
| Oxytocic agent (yes) ** | 0.61 | 0.46–0.81 | < 0.0006 | 0.137 |
| BMI 25 to < 30 *** | 1.04 | 0.68–1.57 | 0.8782 | 0.009 |
| BMI ≥ 30 | 2.22 | 1.46–3.39 | < 0.0002 | 0.210 |
| Educational attainment (medium) **** | 0.66 | 0.32–1.35 | 0.2543 | 0.115 |
| Educational attainment (high) | 0.65 | 0.30–1.39 | 0.2671 | 0.119 |
References: * = non-immigrant women, ** = oxytocic agent (no), *** = BMI < 25, **** = Educational attainment (low)
Statistical analysis
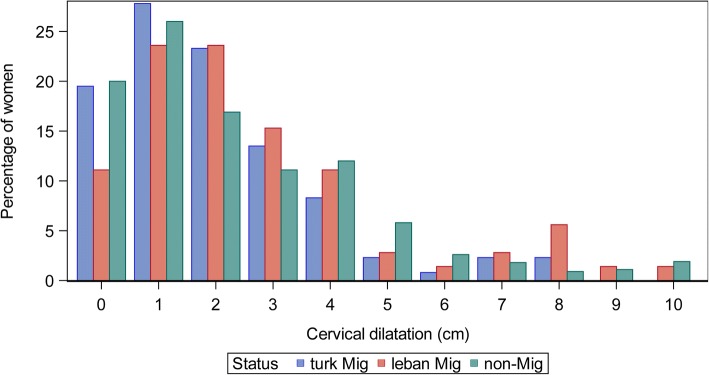
Statistical distribution of cervical dilatation by migration status was plotted.
Multivariate logistic regression analysis was conducted to assess the association of cervical dilatation with the outcome “emergency cesarean delivery”. Covariates were educational attainment, BMI, oxytocic agent, maternal age, and migration status.
Linear regression analysis was performed for collinearity diagnostics. Effect measure modification was tested for with a logistic regression model. Neither collinearity nor effect measure modification were found.
We calculated standardized coefficients to rank the predictors (which had different scale levels) in the logistic regression analysis. The statistics software SAS 9.4 was used; the significance level was set at p < 0.05. Data protection regulations were observed in the survey and in the linkage to hospital data. The Charité Ethics Committee I, Berlin, approved the study (approval dated 18 February 2009; reference EA1/235/08).
Results
Characteristics of the study population are provided in Table 1. There are noticeable differences in the distribution of age and educational level between the immigrant and non-immigrant women. Differences in obesity (BMI > =30 kg/m2) prevalence between migrant and non-immigrant women were small. 55.6% of Turkish migrant women, 45.8% of Lebanese migrant women, and 50.6% of non-immigrant women received oxytocic agents. At the time of admission to labor ward, a smaller proportion of Turkish migrant women (15.8%) were in the active phase of labor, compared to Lebanese (26.4%) and non-immigrant women (26.1%). Emergency cesarean delivery rates were lower in both immigrant groups (Turkish: 15.8%; Lebanese: 13.9%) compared to non-immigrant women (23.9%). Indications for an emergency cesarean delivery were among others failure to progress in labor, multiple birth, macrosomia combined with gestational diabetes, maternal diseases such as pre-eclamsia, s/p cesarean delivery, and anomalies of fetal presentation.
Figure 2 shows that cervical dilatation at admission most often is between 0 cm and 3 cm (before or in latency phase of labor). Overall, only small differences can be observed between immigrant and non-immigrant women, (Turkish origin vs. non-migrant women: chi-square test p < 0.01, Lebanese origin vs. non-migrant women: chi-square test p = 0.95), providing no evidence of a later admittance of 1st generation Lebanese migrant women but evidence for an earlier admittance of 1st generation Turkish migrant women (0 cm - 3 cm vs. 4 cm - 10 cm). When cervical dilatation was used as a continuous variable (0 cm - 10 cm), no statistically significant differences were found (Turkish origin vs. non-migrant women: Kruskal-Wallis test (median) p = 0.20; Lebanese vs. non-migrant women: Kruskal-Wallis test (median) p = 0.11). Women with premature rupture of the membranes are known for early admission. In our study 28.5% (335 of 1174) of women without premature rupture and 8.4% of women with a premature rupture admitted with > = 4 cm of cervical dilatation. A cesarean was performed in 23.1% of women without and 20.5% of women with premature rupture of membranes.
Fig. 2.
Cervical dilatation at admission, 1st generation Turkish and Lebanese women and non-immigrant women, Berlin Perinatal study, 2011/12
The most important obstetric complication is a hemorrhage (23 women). Pathological cardiotocography (CTG) or auscultatory bad fetal heart tones is ranked first of indications for cesarean (Table 2).
In the logistic regression analysis, advanced cervical dilatation (inverse association with an adjusted Odds Ratio (aOR) of 0.76, 95% CI: 0.70–0.82), maternal age (aOR: 1.06, 95% CI: 1.04–1.09), the application of oxytocic agents (inverse association with an aOR of 0.55, 95% CI: 0.42–0.72), and a BMI ≥30 (aOR: 2.25, 95% CI: 1.51–3.34) are statistically significantly associated with the outcome “emergency cesarean delivery” (Table 3).
Table 3.
Odds ratios of emergency cesarean delivery among selected subsample of women, unadjusted and adjusted logistic regression model
| Variable | OR | 95% CI | p-Value | Standardized estimates |
|---|---|---|---|---|
| Cervical dilatation (continuous) | 0.76 | 0.70–0.82 | < 0.0001 | 0.342 |
| Maternal age (continuous) | 1.06 | 1.04–1.09 | < 0.0001 | 0.198 |
| 1st generation Turkish migrants * | 0.63 | 0.37–1.08 | 0.0951 | 0.075 |
| 1st generation Lebanese migrants * | 0.64 | 0.31–1.31 | 0.2229 | 0.054 |
| Oxytocic agent (yes) ** | 0.55 | 0.42–0.72 | < 0.0001 | 0.198 |
| BMI 25 to < 30 *** | 1.08 | 0.73–1.61 | 0.6911 | 0.022 |
| BMI ≥ 30 | 2.25 | 1.51–3.34 | < 0.0001 | 0.214 |
| Educational attainment (medium) **** | 0.78 | 0.40–1.54 | 0.4767 | 0.068 |
| Educational attainment (high) | 0.80 | 0.39–1.62 | 0.5333 | 0.062 |
References: * = non-immigrant women, ** = oxytocic agent (no), *** = BMI < 25, **** = Educational attainment (low)
In addition, standardized estimates show that higher cervical dilatation is the most relevant predictor of an emergency cesarean delivery, followed by a BMI of 30 or above (Table 3).
Sensitivity analysis: Results of analysis with complete data show no substantial differences compared with the results of the imputed data set. This demonstrates that results are only slightly sensitive on changes in the study population.
Discussion
At the time of admission to labor ward, a smaller proportion of Turkish migrant women was in the active phase of labor, compared to women of Lebanese origin and non-immigrant women. In the logistic regression analysis cervical dilatation was found to be the most relevant predictor of a cesarean delivery. Still, rates of cesarean deliveries were lower in women of Turkish and Lebanese origin than in non-immigrant women.
Early admission to delivery room before or in the latency phase (cervical dilatation of less than 4 cm) can lead to a mistaken diagnosis of failure to progress in labor [22]. This risk factor by now is well documented, but it continues to be observed in nulliparous women, even in the high-standard secondary and tertiary hospitals of Berlin/Germany participating in our study. Underlying may be expectations of observing a dilatation of 1 cm/hour, which are unreasonable for the actual, early stage of labor. This may lead to an overdiagnosis of dystocia and, subsequently, to an overuse of interventions aimed at accelerating labor progress – and ultimately to an emergency cesarean delivery [8, 10, 22, 23].
Cesarean deliveries are considered safe, but there are several risks associated with this procedure like infections, bleedings, allergic reactions to anesthetics, problems with the placenta in future deliveries or possible injuries to newborn.
A higher frequency of emergency cesarean deliveries among immigrants and ethnic minorities has been observed in several studies [24–27]; however, it tends to differ between sub-groups, according e.g. to country of origin or duration of stay [28]. A possible explanation could be an earlier admission of nulliparous immigrant women to labor ward, e.g. because of actual or expected communication problems. In our study, however, we did not find evidence for the hypothesis that 1st generation immigrant women would generally be admitted to labor ward at earlier stages of labor (as measured by cervical dilatation) than non-immigrant women. There is some evidence that this may be the case for Turkish, but not for Lebanese women: A larger proportion of Turkish nulliparous women is admitted to labor ward before the onset of the active phase, and the proportion of deliveries by vacuum extraction is twice as high as among Lebanese women. Nevertheless, crude cesarean delivery rates are considerably lower among women from Turkey and Lebanon compared to non-immigrant women. A lower chance of cesarean delivery remains visible in the logistic regression analysis but fails to reach statistical significance in our sample. Thus, the lower rates of cesarean delivery reported by David et al. [20] in the full data set of this study cannot be explained by later admission of 1st generation migrant women (at least not from Turkey and Lebanon) or by the immigrant status itself. Other factors not considered in this paper must therefore play a role, such as multiparity. The strengths of the study are the high participation rate (which makes selection bias unlikely) and the availability of detailed data from interviews and clinical documentation of perinatal variables. Sectio rates are lower than reported in the literature, which is attributable to the inclusion and exclusion criteria applied to this sample (see flowchart).
The main limitation is the sample size available for analysis due to exclusion criteria necessary to examine the study hypothesis. The cesarean delivery rates reported here are unlikely to be biased with regard to our study question. Exclusion criteria relate mainly to previous deliveries and different migration histories; the exclusion of women with elective cesarean deliveries is necessary because they are obviously not informative with regard to cervical dilatation. Moreover, given the heterogeneity of the immigrant population in Germany in terms of country of birth, migration background, and ethnicity, findings cannot be generalized to all immigrant women. Another limitation is that the sample is not representative for all German maternity hospitals; the way deliveries are organized may vary, thus incurring differing risks of emergency cesarean deliveries.
Turkish migrant women were more likely to have instrumental delivery compared to non-immigrant women, although cesarean delivery rates were certainly lower. This might suggest that other confounding factors help Turkish migrant women deliver instrumentally and may make the relationship between later admission and lower cesarean delivery rates in immigrant women obscure.
Conclusion
Advanced cervical dilatation at the time of admission to labor ward does not explain lower emergency cesarean delivery rates in Turkish and Lebanese migrant women, despite the fact that this is the strongest among the predictors for emergency cesarean delivery considered in this study: With early admission, the chance of cesarean delivery increases, irrespective of migrant status. Obesity (BMI ≥30 kg/m2) and later maternal age follow in second and third place.
Acknowledgements
Not applicable.
Funding
The original study was supported by Deutsche Forschungsgemeinschaft (DFG), grant number DA 1199/2–1. The funder played no role in study design, analysis and reporting. We acknowledge support for the Article Processing Charge by the Deutsche Forschungsgemeinschaft and the Open Access Publication Fund of Bielefeld University.
Availability of data and materials
Data are available upon request due to ethical restrictions. Interested researchers may submit requests to Mr. Heiko Wiese, Deputy Head of the Team Data Protection and Information Security, Charité University Medicine Berlin, for access to sensitive data. Contact: Virchowweg 20, Charitéplatz 1, 10,117 Berlin, Germany. E-mail: heiko.wiese@charite.de
Abbreviations
- BMI
Body mass index
- CI
Confidence interval
- CTG
Cardiotocography
- OR
Odds ratio
- S/P
Status post
Appendix
Authors’ contributions
Conceived and designed the experiments: MD TB OR SB WH. Performed the experiments: MD TB SB WH. Analyzed the data: JB OR MD TB. Contributed reagents/materials/analysis tools: EML JB OR. Wrote the paper: JB EML OR MD WH TB SB. All authors read and approved the final manuscript.
Ethics approval and consent to participate
The Charité Ethics Committee I, Berlin, approved the study (approval dated 18 February 2009; reference EA1/235/08) for the participating hospitals. Only anonymised data were processed. However, each person interviewed in the original study gave written informed consent for the two time points of interviews: on admission to the delivery room (T1) and on the second or third day postpartum in the maternity wards (T2).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Jürgen Breckenkamp, Email: juergen.breckenkamp@uni-bielefeld.de.
Eileen Marie Läcke, Email: eileen.laecke@uni-bielefeld.de.
Wolfgang Henrich, Email: wolfgang.henrich@charite.de.
Theda Borde, Email: theda.borde@ash-berlin.de.
Silke Brenne, Email: silke.brenne@med.ovgu.de.
Matthias David, Email: matthias.david@charite.de.
Oliver Razum, Email: oliver.razum@uni-bielefeld.de.
References
- 1.Menacker F, Declercq E, Macdorman MF. Cesarean delivery: background, trends, and epidemiology. Semin Perinatol. 2006;30(5):235–241. doi: 10.1053/j.semperi.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 2.Villar J, Valladares E, Wojdyla D, et al. Caesarean delivery rates and pregnancy outcomes: the 2005 WHO global survey on maternal and perinatal health in Latin America. Lancet. 2006;367(9525):1819–1829. doi: 10.1016/S0140-6736(06)68704-7. [DOI] [PubMed] [Google Scholar]
- 3.Lumbiganon P, Laopaiboon M, Gülmezoglu AM, et al. Method of delivery and pregnancy outcomes in Asia: the WHO global survey on maternal and perinatal health 2007-08. Lancet. 2010;375(9713):490–499. doi: 10.1016/S0140-6736(09)61870-5. [DOI] [PubMed] [Google Scholar]
- 4.Menacker F, Hamilton B. Recent trends in cesarean delivery in the United States. NCHS Data Brief. 2010;35:1–8. [PubMed] [Google Scholar]
- 5.Hure A, Powers J, Chojenta C, Loxton D. Rates and predictors of caesarean section for first and second births: a prospective cohort of Australian women. Matern Child Health J. 2017;21(5):1175–1184. doi: 10.1007/s10995-016-2216-5. [DOI] [PubMed] [Google Scholar]
- 6.Li HT, Luo S, Trasande L, et al. Geographic variations and temporal trends in cesarean delivery rates in China, 2008-2014. JAMA. 2017;317(1):69–76. doi: 10.1001/jama.2016.18663. [DOI] [PubMed] [Google Scholar]
- 7.Shabila NP. Rates and trends in cesarean sections between 2008 and 2012 in Iraq. BMC Pregnancy Childbirth. 2017;17(1):22. doi: 10.1186/s12884-016-1211-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Holmes P, Oppenheimer LW, Wen SW. The relationship between cervical dilatation at initial presentation in labour and subsequent intervention. BJOG. 2001;108(11):1120–1124. doi: 10.1111/j.1471-0528.2003.00265.x. [DOI] [PubMed] [Google Scholar]
- 9.Son GH, Kim JH, Kwon JY, Kim YH, Park YW. Risk factors for cesarean delivery after induction of labor in nulliparous women with an unfavorable cervix at or beyond 41 weeks of gestation. Gynecol Obstet Investig. 2013;76(4):254–259. doi: 10.1159/000350798. [DOI] [PubMed] [Google Scholar]
- 10.Kauffman E, Souter VL, Katon JG, Sitcov K. Cervical dilation on admission in term spontaneous labor and maternal and newborn outcomes. Obstet Gynecol. 2016;127(3):481–488. doi: 10.1097/AOG.0000000000001294. [DOI] [PubMed] [Google Scholar]
- 11.Mikolajczyk RT, Zhang J, Grewal J, Chan LC, Petersen A, Gross MM. Early versus late admission to labor affects labor Preogression and risk of cesarean section in nulliparous women. Front Med. 2016;26(3):1–7. doi: 10.3389/fmed.2016.00026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cheng YW, Shaffer BL, Bryant AS, Caughey AB. Length of the first stage of labor and associated perinatal outcomes in nulliparous women. Obstet Gynecol. 2010;116(5):1127–1135. doi: 10.1097/AOG.0b013e3181f5eaf0. [DOI] [PubMed] [Google Scholar]
- 13.Merry L, Small R, Blondel B, Gagnon AJ. International migration and caesarean birth: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2013;13:27. doi: 10.1186/1471-2393-13-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Merry L, Semenic S, Gyorkos TW, Fraser W, Gagnon AJ. Predictors of unplanned cesareans among low-risk migrant women from low- and middle-income countries living in Montreal, Canada. Birth. 2016;43(3):209–219. doi: 10.1111/birt.12234. [DOI] [PubMed] [Google Scholar]
- 15.Merten S, Wyss C, Ackermann-Liebrich U. Caesarean sections and breastfeeding initiation among migrants in Switzerland. Int J Public Health. 2007;52(4):210–222. doi: 10.1007/s00038-007-6035-8. [DOI] [PubMed] [Google Scholar]
- 16.Roman H, Blondel B, Breart G, Goffinet F. Do risk factors for elective cesarean section differ from those of cesarean section during labor in low risk pregnancies? J Perinat Med. 2008;36(4):297–305. doi: 10.1515/JPM.2008.044. [DOI] [PubMed] [Google Scholar]
- 17.Vangen S, Stoltenberg C, Skrondal A, Magnus P, Stray-Pedersen B. Cesarean section among immigrants in Norway. Acta Obstet Gynecol Scand. 2000;79(7):553–558. doi: 10.1080/j.1600-0412.2000.079007553.x. [DOI] [PubMed] [Google Scholar]
- 18.Edmonds JK, Yehezkel R, Liao X, Moore Simas TA. Racial and ethnic differences in primary, unscheduled cesarean deliveries among low-risk primiparous women at an academic medical center: a retrospective cohort study. BMC Pregnancy Childbirth. 2013;168(13):1–7. doi: 10.1186/1471-2393-13-168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Getahun D, Strickland D, Lawrence JM, Fassett MJ, Koebnick C, Jacobsen SJ. Racial and ethnic disparities in the trends in primary cesarean delivery based on indications. Am J Obstet Gynecol. 2009;201(4):422.e1. doi: 10.1016/j.ajog.2009.07.062. [DOI] [PubMed] [Google Scholar]
- 20.David M, Borde T, Brenne S, Henrich W, Breckenkamp J, Razum O. Caesarean section frequency among immigrants, second- and third-generation women, and non-immigrants: prospective study in Berlin/Germany. PLoS One. 2015;10(5):e0127489. doi: 10.1371/journal.pone.0127489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.IVEware - imputation and variance estimation. University of Michigan, Ann Arbor, MI, USA. http://www.isr.umich.edu/software. Accessed 21 Oct 2017.
- 22.Neal JL, Lowe NK, Patrick TE, Cabbage LA, Corwin EJ. What is the slowest-yet-normal cervical dilation rate among nulliparous women with spontaneous labor onset? J Obstet Gynecol Neonatal Nurs. 2010;39(4):361–369. doi: 10.1111/j.1552-6909.2010.01154.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rahnama P, Ziaei S, Faghihzadeh S. Impact of early admission in labor on method of delivery. Int J Gynaecol Obstet. 2006;92(3):217–220. doi: 10.1016/j.ijgo.2005.12.016. [DOI] [PubMed] [Google Scholar]
- 24.Braveman P, Egerter S, Edmonston F, Verdon M. Racial/ethnic differences in the likelihood of caesarean delivery, California. Am J Public Health. 1995;85:625–630. doi: 10.2105/AJPH.85.5.625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Diani F, Zanconato G, Foschi F, Turinetto A, Franchi M. Management of the pregnant immigrant woman in the decade 1992-2001. J Obstet Gynacol. 2003;23(6):615–617. doi: 10.1080/01443610310001604367. [DOI] [PubMed] [Google Scholar]
- 26.Ibison JM. Ethnicity and mode of delivery in ‘low-risk’ first time mothers. East London, 1988-1997. Eur J Obstet Gynecol Reprod Biol. 2005;118(2):199–205. doi: 10.1016/j.ejogrb.2004.05.002. [DOI] [PubMed] [Google Scholar]
- 27.Dahlen HG, Schmied V, Dennis CL, Thomtom C. Rates of obstetric intervention during birth and selected maternal and perinatal outcomes for low risk women born in Australia compared to those born overseas. BMC Pregnancy Childbirth. 2013;13:100. doi: 10.1186/1471-2393-13-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sørbye IK, Daltweit AK, Sundby J, Stoltenberg C, Vangen S. Caesarean section by immigrants‘ length or residence in Norway; a population-based study. Eur J Pub Health. 2015;25(1):78–84. doi: 10.1093/eurpub/cku135. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available upon request due to ethical restrictions. Interested researchers may submit requests to Mr. Heiko Wiese, Deputy Head of the Team Data Protection and Information Security, Charité University Medicine Berlin, for access to sensitive data. Contact: Virchowweg 20, Charitéplatz 1, 10,117 Berlin, Germany. E-mail: heiko.wiese@charite.de