Abstract
Background:
The operation theater (OT) complex is a costly component of a hospital budget expenditure. This area of hospital activity requires maximum utilization to ensure optimum cost benefit. To achieve a high level of utilization in the OT, it is necessary to efficiently coordinate number of activities and personnel.
Methods:
This study was conducted in a 1000-bedded tertiary care teaching hospital in rural maharashtra over aperiod of two months. The OT complex consists of eight major OTs. Normal working hours for routine scheduled cases on all working days except Sundays and public holidays.
Results:
Total study period consisted of 96 working days. There were a total of eight OT tables of various specialties, and parameters were observed during the routine hours excluding Sundays and holidays. The total procedure time was maximum for ENT followed by orthopedics and least for obstetrics. Room turnover time was maximum for obstetrics followed by general and oncosurgery. Case delays were maximum in general surgery and least for ophthalmology. The most common reason for delay in starting the operation table was patient getting shifted late from the ward and administrative causes. The most prominent reasons for cancellation were lack of operating room time followed by medical reasons of the patient.
Conclusion:
We concluded that most of the causes of delays and cancellations of surgeries were avoidable with proper preoperative planning and optimization of patients and resources and good communication between surgeon anesthesiologists and the nursing staff.
Keywords: Cancellations, operation theatre, rescheduling of surgeries, utilization
INTRODUCTION
The operation theater (OT) complex is a costly component of a hospital budget expenditure. This area of hospital activity requires maximum utilization to ensure optimum cost benefit. In any hospital, OT is said to be the source of primary revenue generation with around 50%–60% of revenue generated only with this area. To achieve a high level of utilization in the OT, it is necessary to efficiently coordinate a number of activities and personnel.[1] It is, therefore, desirable to optimize the efficiency of these assets. Unanticipated cancellation of scheduled operations at the last minute, even on the morning of surgery is of concern. Late cancellation of scheduled operations is a major cause of inefficient use of operating room time and a waste of resources. It is also potentially stressful with depressing effects and costly to the patient in terms of working days lost and disruption of daily life.[1,2,3]
OT is that specialized facility of the hospital where lifesaving or life-improving procedures are carried out on the human body by invasive methods under strict aseptic conditions in a controlled environment by specially trained personnel to promote healing and cure with maximum safety, comfort, and economy.[4] The efficiency of OTs can be measured in a variety of ways. Essentially, it tends to be defined in terms of ability to translate available time into earnings.[5,6,7] Utilization is a simple and adequate measure of the efficiency of a theater, because of its ability to generate revenue rises as the time for which it is used increases. OT utilization is defined by Donham et al. as the quotient of hours of OT time actually used during elective resource hours and the total number of elective resource hours available.[8] Utilization of the OT time has always been a priority area for hospital administrators.
In a study done by Lakshmi Bhaskar at a tertiary care teaching hospital over 2 years, the utilization of OT complexes was 72.51% which was found to be optimum. Most of the scheduled hours were utilized for elective surgeries and unscheduled hours for emergency surgeries.[9]
Stavrou et al. studied operating room utilization in a teaching hospital a total of 548 operations. The mean (standard deviation [SD]) time in minutes for anesthesia induction was 19 (9), for surgery preparation 13 (8), for surgery 115 (64), for recovery from anesthesia 12 (8), and for transfer to postoperative care unit/Intensive Care Unit (PACU/ICU) 12 (9). The time spent in each step presented an ascending escalation pattern proportional to the surgical impact (P = 0.000), which was less pronounced in the transfer to PACU/ICU (P = 0.006).[10]
Similar study conducted by Vinukondaiah et al. had the OT functional for 279 days during the year of the study, and 1773 cases were operated (6.3 cases per day). The total operating time utilized was 91.5%. The major reasons for cancellation of a total of 310 cases were lack of operating time (65.2%), emergency surgery during the elective list (13.9%), and preoperative lack of fitness (1 1.3%). Among all the lists, 43.6% started late and 63.6% of lists finished well before the scheduled closing time.[1]
Garg et al. conducted a prospective study on cancellation of cases on the day of surgery. 1590 patients were scheduled for elective surgical procedures in 458 operation rooms. About 30.3% of patients were canceled on the day of surgery. Of these, 59.7% were cancelled due to lack of availability of theater time, 10.8% were canceled because of medical reasons, and 16.2% did not turn up on the day of surgery. In 5.4% of patients, surgery was canceled by surgeons due to a change in the surgical plan, 3.7% were canceled because of administrative reasons, and 4.2% of patients were postponed because of miscellaneous reasons. The authors concluded that most of the reasons were avoidable with previous planning and coordination.[11]
Therefore, this short study was conducted in a tertiary care rural hospital prospectively over a period of 2 months to study the OT utilization time and the most common causes of postponement and rescheduling of surgeries in the routine scheduled operative list.
Aim
The aim of the study is to study the OT utilization time and most common causes of cancellations and rescheduling of surgeries.
METHODS
This study was conducted in a 1000-bedded tertiary care teaching hospital in western rural Maharashtra. The OT complex consists of eight major OTs. Normal working hours for routine scheduled cases are from 8.00 am to 4 pm on all working days except Sundays and public holidays. This study was conducted prospectively over a period of 2 months from November 1, 2017, to December 31, 2017. The observation was recorded only for scheduled routine cases which were scheduled on the list on the previous day till 8 pm. The last case taken-up under anesthesia was induced before 2 pm. The cases that were induced after 2 pm and emergency surgeries were excluded. Observations were not made on Sundays and gazetted holidays.
The following parameters were observed:
OT start time: the time the first case was shifted inside the OT. Any delay >10 min of the scheduled start time was noted down
Induction to incision time: the time when anesthesiologist attaches the first monitor to the patient to the time when the patient is handed over to the surgeons for scrubbing. Any delay >15 min, the reason was specified
Time of shifting patient outside the OT: time between surgical closure to the patient getting shifted outside the OT. Any delay >15 min had the reason noted down
Table turnover time: time between previous patient getting shifted out to the next patient being wheeled inside the OT. Any delay >15 min, the reason was noted.
If any case gets canceled or rescheduled, the reason was noted down.
The most common causes of delays in various timings and rescheduling of surgeries were studied and analyzed.
Statistical analysis
This was done by IBM SPSS (International Business Machines; Statistical Package for the Social Sciences) statistics for windows version 20.0 (IBM Corp, Armonk, NY). One-way ANOVA for statistical analysis of parametric data whereas for non parametric data Chi square test was conducted.
RESULTS
Each of the eight OT tables was observed for 6 days (total 96 days). The available resource hours summed up to 480 min/day and 46,080 min in 96 days.
There were total eight OT tables of that three were allotted to general surgery (including oncosurgery), 1 for orthopedic and neurosurgery, 2 for obstetrics and gynecology, ENT – 1, and ophthalmology – 1.
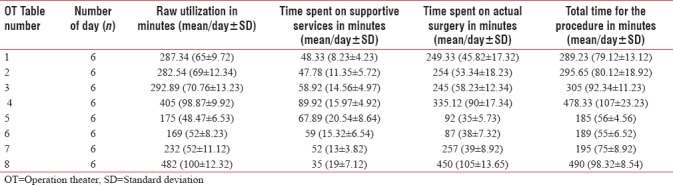
The total time for procedure was more in ENT, i.e., 490 min (98.32 ± 8.54) followed by orthopedics 478.33 min (107 ± 23.23), to be followed by surgery – 305 min (92.34 ± 11.23), 295.65 (80.12 ± 18.92), and 289.23 (79.12 ± 13.12) for each table, respectively. For ophthalmology, it was 195 min (75 ± 8.92), and for Obgyn, it was 189 min (55 ± 6.52) and 185 (56 ± 4.56) in both the theaters. This observed difference was statistically significant (one-way ANOVA, P < 0.05) [Table 1].
Table 1.
Distribution as per the time spent on different parameters
The total room turnover time in minutes [Graph 1] (mean/day ± SD) was more in OT 5 and 6 (obstetrics and gynecology [Obgyn]) – 34.51 (6.5 ± 6.1) and 33.27 min (6.23 ± 3.54), respectively, followed by for OT no. 1, 2, and 3 (general and oncosurgery) – 27.12 min (7.23 ± 3.76), 26.17 min (8.17 ± 5.1), and 25.82 min (9.12 ± 3.24), respectively, followed by for OT no. 8 (ophthalmology) – 21 (7.1 ± 5.42), for OT no. 4 (orthopedic and neurosurgery), it was 19 min (6.71 ± 4.51) and least for OT no. 7 (ENT) – 13 (4.82 ± 2.92). This observed difference was statistically significant P < 0.05 (one-way ANOVA).
Graph 1.
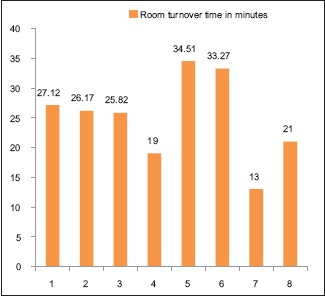
Distribution as per the Room turnover time for each operation theater
The number of delays among various OTs was more in general surgery theaters (OT no. 1, 2, and 3), i.e., 2 ± 1.21, 1.92 ± 1.41, and 1.82 ± 1.32, respectively, followed by for orthopedics (OT no. 4) 1 ± 1.54, for Obgyn (OT no 5 and 6), it was 0.94 ± 0.27 and 1 ± 0.98, respectively, and for ENT (OT no. 7) 1 ± 0.98 was least for ophthalmology (OT no. 8), i.e., 0.
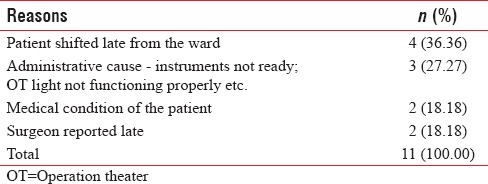
The reason for delays in starting the operation table was mostly patient shifted late from the ward (36.36%), followed by administrative causes such as instruments not ready and OT light not functioning properly (27.27%). This was followed by medical condition of the patient (18.18%) and operating surgeon reporting late (18.18%) [Table 2].
Table 2.
Distribution as per the reasons and the number of delays in starting the operation table
The cancellation percentage [Graph 2] was maximum in OT Tables 1–3 (general surgery), i.e., 27.27%, 23.68%, and 20.00%, respectively, followed by for OT no. 7 (ENT) was 23.94%, for OT no. 4 (orthopedic) was 11.36%, and for OT no. 5 and 6 (Obgyn) was 0.86 and 0.66, respectively. This observed difference was statistically significant (χ2 = 99.14, P < 0.0001).
Graph 2.
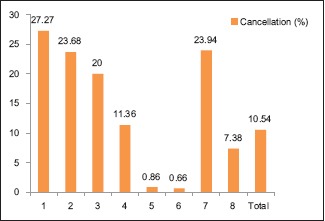
Distribution as per the various operation theater tables as per the cancellation of surgeries
Table 3.
Distribution of the patients as per the reasons of cancellation
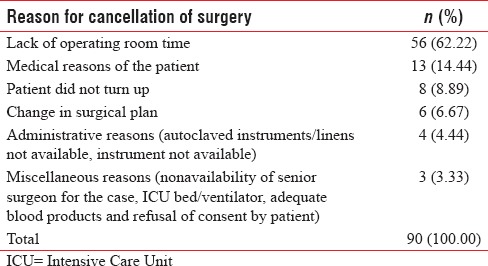
The most common causes of cancellations of surgical procedures were lack of operating room time (62.22%), followed by medical reasons of the patient (14.44%), patient did not turn up –8.89%, change in surgical plan (6.67%), administrative reasons such as autoclaved instruments/linens not available (4.44%), miscellaneous reasons such as nonavailability of senior surgeon for the case, ICU bed/ventilator, adequate blood products, and refusal of consent by patient (3.33%) [Graph 3].
Graph 3.
Distribution as per the reasons of cancellation
DISCUSSION
A properly structured OT is a vital and necessary part of any hospital. The theory of OT utilization is present in the surgical journalism as early as the late 1970s.[12,13,14] To satisfy patients, fulfill demands of surgeons and OT staff and to proof a well-functioning OT, an excellent management is needed. OT needs a great quantity of resource to maintain a working function in any hospital.[15] To increase the surgical management in any hospital it is essential that operation theatre time should be well utilised and managed.[16] Proper functioning of OT depends on a good hospital management, provision of multiple medical and surgical services such as equipment, drugs, time utilization, sterilization, and control of infections. Studies showed that the measurement of time utilization has always been of greater interest among researchers.[17,18]
In our study, there were a total of eight OT tables of that three were allotted to general surgery, one for orthopedic, two for Obgyn, one for ENT, and one for ophthalmology.
The total time for procedure in minutes (mean/day ± SD) was more in ENT, i.e., 490 (98.32 ± 8.54) followed by orthopedics 478.33 (107 ± 23.23), general and oncosurgery – 305 (92.34 ± 11.23), 295.65 (80.12 ± 18.92), and 289.23 (79.12 ± 13.12), respectively, for three surgical theaters, respectively. The total procedure time for ophthalmology was 195 (75 ± 8.92) and for Obgyn was 189 (55 ± 6.52) and 185 (56 ± 4.56), respectively, for its two allotted theaters.
Since ENT surgeries like thyroid surgeries and commando operations take longer time the total theatre utilisation time was maximum with ENT speciality whereas it was least with obstetrics since most of the surgeries are of shorter duration.
The room turnover time in minutes (mean/day ± SD) was in Obgyn 34.51 (6.5 ± 6.1) and 33.27 (6.23 ± 3.54) followed by for general and oncosurgery 27.12 (7.23 ± 3.76), 26.17 (8.17 ± 5.1), and 25.82 (9.12 ± 3.24) for the three allotted tables, respectively, followed by for ophthalmology – 21 (7.1 ± 5.42). For orthopedics, it was 19 (6.71 ± 4.51) and least for ENT – 13 (4.82 ± 2.92). This observed difference was statistically significant P < 0.05 (one-way ANOVA). The increased room turnover time in obstetric theater is mainly attributed to last moment reshuffling of scheduled cases to accommodate emergency cesarean sections and minor surgeries and haphazard scheduling of surgeries on the routine list.
Whereas the study by Talati et al. found the reason for variation in time spent on supportive services included, for example, time spent in positioning of patient for surgery or catheterization.[19] Other reasons included the patient's medical condition, for example, an increase or decrease in blood pressure on the table requiring time for stabilization. The case duration of surgeries conducted by various surgical specialties is different. In fact in the same specialty, each procedure requires different length of time. The time spent on supportive services, time spent on actual surgery, time between entry and exit of patient (raw utilization), and total time for the procedure (adjusted utilization) were significantly different among the 16 OT tables (P < 0.001), whereas the room turnover time was not significantly different among the various OT tables (P = 0.195).
The number of delays among various OTs was more in general surgery theaters, i.e., 2 ± 1.21, 1.92 ± 1.41, and 1.82 ± 1.32, respectively, followed by for orthopedics 1 ± 1.54, for Obgyn, it was 0.94 ± 0.27 and 1 ± 0.98, respectively, and for ENT, 1 ± 0.98 was least for ophthalmology, i.e., 0.
The reason for delays in starting the operation table was mostly patient shifted late from the ward (36.36%), followed by administrative causes such as instruments not ready and OT light not functioning properly (27.27%). This was followed by medical condition of the patient (18.18%) and operating surgeon reporting late (18.18%).
The study by Vinukondaiah et al. showed that 43.6% of the lists started later than the scheduled time. From these 43.6% delays, 80.4% of the time, the delay was due to late shifting of the patient to the OT and 17.1% of the time, the delay was due to an emergency surgery from the previous night continuing beyond 8.00 am. In the remaining 2.5% of time, the delay was because of miscellaneous causes.[1] In our study, there were delays on 15 occasions of 96 lists, i.e., 15.63%, and late shifting of the patient from the ward to the OT was the most common (44.66%) cause. In a study by Kumar and Sarma, none of the residents felt that there is a delay in the start of OT, yet the majority of the consultants and 35% of the nurses felt that OTs were starting late and the most common reason stated was delay in shifting of patients to OTs from wards.[20]
The cancellation percentage was maximum in general and oncosurgery, i.e., 27.27%, 23.68%, and 20%, respectively, for each table allotted to the specialty, followed by ophthalmology 23.94%. Cancellation percentage for orthopedic surgeries was 11.36%, and Obgyn was 0.86 and 0.66, respectively. This observed difference was statistically significant (χ2 = 99.14, P < 0.0001).
The most frequent cause of cancellation of surgery was found to be lack of operating room time in 62.22%, followed by medical reasons of the patient (14.44%). Patient not turning up for admission consisted of 8.89% cancellations while change in surgical plan contributed to 6.67%. Administrative reasons like instruments/linens not available emerged as the reason for 4.44% of total surgical cancellations. Other factors included miscellaneous reasons such as nonavailability of senior surgeon for the case, ICU bed/ventilator, adequate blood products, and refusal of consent by patient (3.33%).
Schofield et al. in their study at a major hospital in Australia reported 941 (11.9%) cancellations of 7913 theater sessions. The reasons included no bed available (18.9%), run out of theater time (16.1%), patient nonarrival (10.5%), patient unfit (9.2%), and canceled by patient or relative (8.2%). In our study, there were no cancellations because of unavailability of bed or by patient/relative. Nearly 4.1% of the cancellations were due to nonarrival of the patient and 8.2% due to lack of fitness.[2]
Another prospective study by Sanjay et al. they demonstrated that 14% of elective operations were canceled. Almost 51% of the cancellations were due to patient-related reasons, 34% were canceled for nonclinical reasons, and 15% were canceled for clinical reasons. The common reasons for cancellation were inconvenient appointment (18.5%), list overrunning (16%), and emergencies and trauma (9.4%).[21]
SUMMARISE
The total time for procedure was more for ENT followed by orthopedics, general and oncosurgery, ophthalmology, and obstetrics and gynecology in that order
The room turnover time was maximum obstetric theaters followed by for general and oncosurgery and least for ophthalmology
The total number of case delays was maximum in general and oncosurgeries followed by orthopedic, obstetrics and gynecology, ENT, and least for ophthalmology
The most common reason for delay in starting the operation table was patient getting shifted late from the ward, followed by administrative causes, medical condition of the patient, and operating surgeon reporting late
The cancellation percentage was maximum in general and oncosurgery and least for obstetrics
The most prominent reasons for cancellation were lack of operating room time, medical reasons of the patient, patient not getting admitted, last moment change in the surgical plan, administrative reasons such as nonavailability of linen and autoclaved instruments. Miscellaneous reasons such as nonavailability of senior surgeon, ICU bed, adequate blood products, and refusal of consent by patient also emerged as causes for cancellations of scheduled cases.
CONCLUSION
This study highlights that most causes of cancellations and delays of surgeries are avoidable, and efforts should be made to prevent cancellation of surgery by careful planning and utilization human and material resources. Delays in starting the OT table in the mornings cause considerable wastage of productive OT time and lead to cancellations of surgeries in the later part of the day which in turn hampers the daily OT utilization. Therefore, proper communication among surgeon, anesthesiologist, and nursing staff on the night before surgery can help in morning delays. Room turnover time can be improved by keeping a dedicated theater for emergency procedures can avoid rescheduling of cases due to last moment entry of emergency cases.
Adequate staffing and meticulous preanesthetic checkup and proper screening of patients preoperatively, proper arrangements for blood and blood products, ICU backup required instruments, and linen beforehand can go a long way in avoiding last moment cancellations.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Vinukondaiah K, Ananthakrishnan N, Ravishankar M. Audit of operation theatre utilization in general surgery. Natl Med J India. 2000;13:118–21. [PubMed] [Google Scholar]
- 2.Schofield WN, Rubin GL, Piza M, Lai YY, Sindhusake D, Fearnside MR, et al. Cancellation of operations on the day of intended surgery at a major Australian referral hospital. Med J Aust. 2005;182:612–5. doi: 10.5694/j.1326-5377.2005.tb06846.x. [DOI] [PubMed] [Google Scholar]
- 3.Wildner M, Bulstrode C, Spivey J, Carr A, Nugent I. Avoidable causes of cancellation in elective orthopaedic surgery. Health Trends. 1991;23:115–6. [PubMed] [Google Scholar]
- 4.Sonal S. Express Health Care: Streamlining. Occup Ther. 2008;2:12. [Google Scholar]
- 5.Sherman HD. Hospital efficiency measurement and evaluation. Empirical test of a new technique. Med Care. 1984;22:922–38. doi: 10.1097/00005650-198410000-00005. [DOI] [PubMed] [Google Scholar]
- 6.van As AB, Brey Z, Numanoglu A. Improving operating theatre efficiency in South Africa. S Afr Med J. 2011;101:444. 446, 448. [PubMed] [Google Scholar]
- 7.Macario A. Are your hospital operating rooms “efficient”? A scoring system with eight performance indicators. Anesthesiology. 2006;105:237–40. doi: 10.1097/00000542-200608000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Donham RT, Mazzei WJ, Jones RL. Columbus (OH): Association of Anesthesia Clinical Directors; 1996. Association of anesthesia clinical directors' procedural times glossary: Glossary of times used for scheduling and monitoring of diagnostic and therapeutic procedures. [Google Scholar]
- 9.Lakshmi Bhaskar N, Satish Kumar SN. A study of utilization of operation theatres in a tertiary care teaching hospital, Hyderabad. Indian J Appl Res. 2015;5:427–9. [Google Scholar]
- 10.Stavrou G, Panidis S, Tsouskas J, Tsaousi G, Kotzampassi K. An audit of operating room time utilization in a teaching hospital: Is there a place for improvement? ISRN Surg 2014. 2014:431740. doi: 10.1155/2014/431740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Garg R, Bhalotra AR, Bhadoria P, Gupta N, Anand R. Reasons for cancellation of cases on the day of surgery-a prospective study. Indian J Anaesth. 2009;53:35–9. [PMC free article] [PubMed] [Google Scholar]
- 12.Magerlein JM, Martin JB. Surgical demand scheduling: A review. Health Serv Res. 1978;13:418–33. [PMC free article] [PubMed] [Google Scholar]
- 13.Quayle SN. Efficient costing and budgeting in the operating theatre. Natnews. 1978;15:11–4. [PubMed] [Google Scholar]
- 14.Faiz O, Tekkis P, McGuire A, Papagrigoriadis S, Rennie J, Leather A, et al. Is theatre utilization a valid performance indicator for NHS operating theatres? BMC Health Serv Res. 2008;8:28. doi: 10.1186/1472-6963-8-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shah J, Ansari A, Bhattacharyya J. Cancellation of urologyoperations. Clin Gov J. 2006;11:128–33. [Google Scholar]
- 16.Kumar R, Sarma R. Operation room utilization at AIIMS, a prospective study. J Acad Hosp Adm. 2003;15:1–6. [Google Scholar]
- 17.Dexter F, Abouleish AE, Epstein RH, Whitten CW, Lubarsky DA. Use of operating room information system data to predict the impact of reducing turnover times on staffing costs. Anesth Analg. 2003;97:1119–26. doi: 10.1213/01.ANE.0000082520.68800.79. [DOI] [PubMed] [Google Scholar]
- 18.Tyler DC, Pasquariello CA, Chen CH. Determining optimum operating room utilization. Anesth Analg. 2003;96:1114–21. doi: 10.1213/01.ANE.0000050561.41552.A6. [DOI] [PubMed] [Google Scholar]
- 19.Talati S, Gupta AK, Kumar A, Malhotra SK, Jain A. An analysis of time utilization and cancellations of scheduled cases in the main operation theater complex of a tertiary care teaching institute of North India. J Postgrad Med. 2015;61:3–8. doi: 10.4103/0022-3859.147009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kumar R, Sarma RK. Operation room utilization at AIIMS, a prospective study. J Acad Hosp Adm. 2003;15:1–6. [Google Scholar]
- 21.Sanjay P, Dodds A, Miller E, Arumugam PJ, Woodward A. Cancelled elective operations: An observational study from a district general hospital. J Health Organ Manag. 2007;21:54–8. doi: 10.1108/14777260710732268. [DOI] [PubMed] [Google Scholar]


